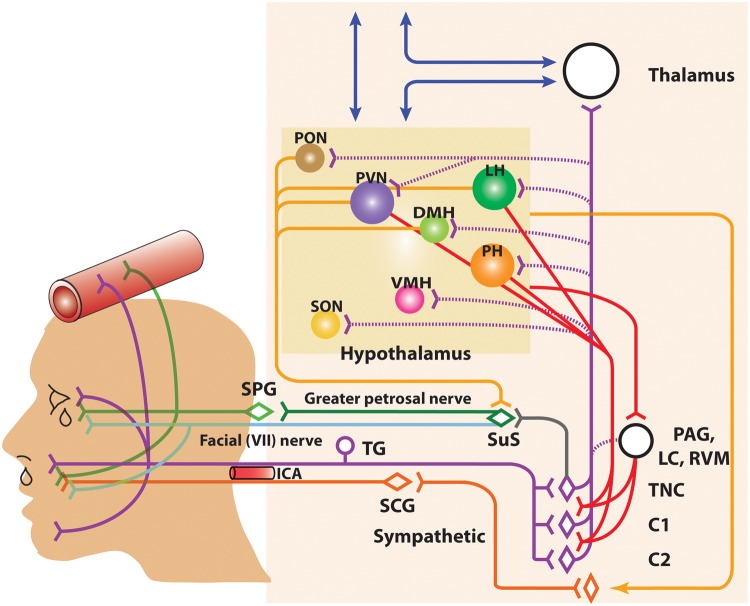
Figure 2.
Anatomy of the neurovascular pathways that constitute the trigeminal-autonomic reflex. Schematic representation of neurovascular pathways of the trigeminal-autonomic reflex involved in cranial autonomic symptoms in migraine and cluster headache. They are thought to result, in part, from activation of the trigeminal-autonomic reflex; a reflex connection from the trigeminal nucleus caudalis (TNC; grey neuron), via the superior salivatory nucleus (SuS; green diamond), which provides an autonomic parasympathetic projection to the cranial vasculature. This is predominantly through the greater petrosal nerve (green neuron) and its relay with the sphenopalatine ganglion (SPG), but also via the facial (VIIth cranial) nerve (sky blue neuron). Descending projections from hypothalamic nuclei (red and yellow neurons) including the posterior (PH), paraventricular (PVN), lateral (LH), dorsomedial (DMH) and pre-optic hypothalamic nuclei (PON), to the TCC (red projections) and SuS (yellow projections) neurons, and the sympathetic nervous system (yellow projections), are thought to modulate and control both trigeminovascular nociceptive transmission (purple network of neurons) and parasympathetic (green)/sympathetic (orange) autonomic projections to the cranial vasculature that result indirectly or directly, respectively, in cranial autonomic symptoms ipsilateral to head pain. A third-order sympathetic nerve lesion (orange projection), in part mediated by internal carotid artery (ICA) vasodilation, is thought to result in Horner’s syndrome (see text for full description). VMH: ventromedial hypothalamus; SON: supra-optic nerve: TG: trigeminal ganglion: SPG: sphenopalatine ganglion; SCG: superior cervical ganglion: PAG: periaqueductal gray; LC: locus coeruleus; RVM: rostral ventromedial medulla.