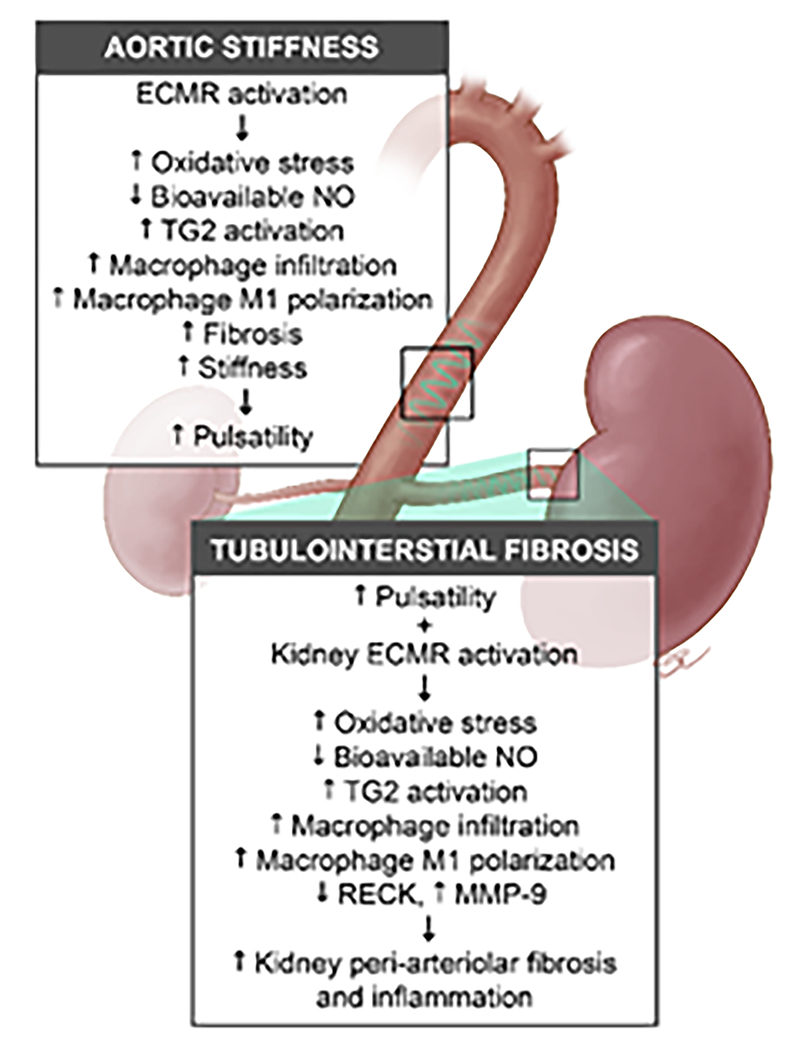
Figure 6: Hypothetical model showing the contribution of the endothelial mineralocorticoid receptor to central aortic stiffening and kidney tubulointerstitial fibrosis.
Activation of the endothelial cell mineralocorticoid receptor (ECMR) in the aorta contributes to reductions in bioavailable nitric oxide (NO), enhanced oxidant, and inflammatory pathways that lead to central aortic perivascular fibrosis and stiffening. The increased central aortic stiffness contributes to an excessive pulsatile wave (e.g., pulsatility) that in combination with kidney ECMR activation, leads to reductions in endothelial NO synthase and bioavailable NO with downstream activation of oxidant and inflammatory pathways in the kidney. The net result in the kidney is endothelial regulation of macrophage infiltration and M1 polarization, disruption of extracellular adhesion through cross-linking enzymes like transglutaminase 2, and matrix metalloproteinase (MMP-9). These changes result in peri-arteriolar inflammation, fibrosis, stiffness and downstream tubulointerstitial fibrosis.