Abstract
Background
The introduction of video laryngoscopy (VL) may impact emergency medicine (EM) residents' intubation practices.
Methods
We analyzed 14,313 intubations from 11 EM training sites, July 1, 2002, to December 31, 2012, assessing the likelihood of first‐attempt success and likelihood of having a second attempt, by rank and device. We determined whether direct laryngoscopy (DL) first‐attempt success decreased as VL became more prevalent using a logistic regression model with proportion of encounters initiated with VL at that center in the prior 90 and 365 days as predictors of DL first‐attempt success.
Results
First‐attempt success by PGY‐1s was 71% (95% confidence interval [CI] = 63% to 78%); PGY‐2s, 82% (95% CI = 78% to 86%); and PGY‐3+, 89% (95% CI = 85% to 92%). Residents' first‐attempt success rate was higher with the C‐MAC video laryngoscope (C‐MAC) versus DL, 92% versus 84% (risk difference [RD] = 8%, 95% CI = 4% to 11%), but there was no statistical difference between the GlideScope video laryngoscope (GVL) and DL, 80% versus 84% (RD = −4%, 95% CI = −10% to 1%). PGY‐1s were more likely to have a second intubation attempt after first‐attempt failure with VL versus DL: 32% versus 18% (RD = 14%, 95% CI = 5% to 23%). DL first‐attempt success rates did not decrease as VL became more prevalent.
Conclusions
First‐attempt success increases with training. Interns are more likely to have a second attempt when using VL. The C‐MAC may be associated with increased first‐attempt success for EM residents compared with DL or GVL. The increasing prevalence of VL is not accompanied by a decrease in DL success.
Airway management is a fundamental component of emergency medicine (EM) resident training, and most academic emergency department (ED) intubations are performed by EM resident trainees.1 The largest report of resident intubations showed that trainees can safely perform endotracheal intubations.1 This conclusion was made before the advent of video laryngoscopy (VL). The clinical learning environment has evolved and VL is increasingly utilized in community and academic EDs.2, 3
Some reports suggest that VL is superior to direct laryngoscopy (DL) with respect to first‐attempt success, obtaining an optimal view of the airway and limiting esophageal intubations.4, 5, 6 VL may increase attending physician comfort when working with residents and the screen provides an opportunity to teach intubation skills in a way that cannot be done with DL. By also visualizing the airway, an attending may be more comfortable with a resident performing a second attempt if he or she fails on the initial try. This is important for developing procedural skills and building confidence. However, it is also possible that physicians learning how to intubate with VL may rely on the screen instead of directly visualizing the airway, impairing the development of DL skills, which are important because video devices can be compromised by blood or secretions in the airway. Given the increasing frequency with which EM residents learn to intubate using VL, surveillance of resident performance is important for patient safety and pedagogy.
Objectives
We evaluate the impact of VL on the clinical learning environment of EM residents by investigating three objectives. First, we compare the likelihood of first‐attempt success of EM resident intubations performed with DL and VL. Second, we report the likelihood that a resident will have an opportunity to attempt an intubation a second time, after failing to secure the airway on the first attempt. Finally, we explore the concern that DL skills may diminish as VL becomes more prevalent. For the first two objectives, we analyze standard geometry C‐MAC versus hyperangulated GlideScope intubations separately, because the hyperangulated blade of the GlideScope might impair first‐attempt success by making tube passage more difficult.
Methods
Study Design
This is a secondary analysis of a prospective multicenter cohort study of ED intubations. Institutional review board approval was obtained by all participating centers.
Setting
The National Emergency Airway Registry is an international network of academic and community hospitals. Each center was responsible for ensuring compliance, defined as data entry on 90% or more of ED intubations, confirmed by comparison of captured patient data with institutional coding for intubation procedures. After intubation, the operator recorded intubation details on a standardized intubation form accessed at www.near.edu, using a center‐specific log‐in and password. Data were entered with a custom‐designed Web‐based data entry tool and imported directly into a relational data base (Microsoft Access version 11.0) at the coordinating center. Compliance plans and criteria have been published previously.7
Selection of Participants
This report represents intubation data collected from July 1, 2002, to December 31, 2012. We excluded encounters at sites without an EM training program or outside of North America and intubations initially attempted by a non‐EM provider. We excluded any intubation attempt that was not performed with DL (either the Macintosh or the Miller blade), the C‐MAC, or the GlideScope (Figure 1).
Figure 1.
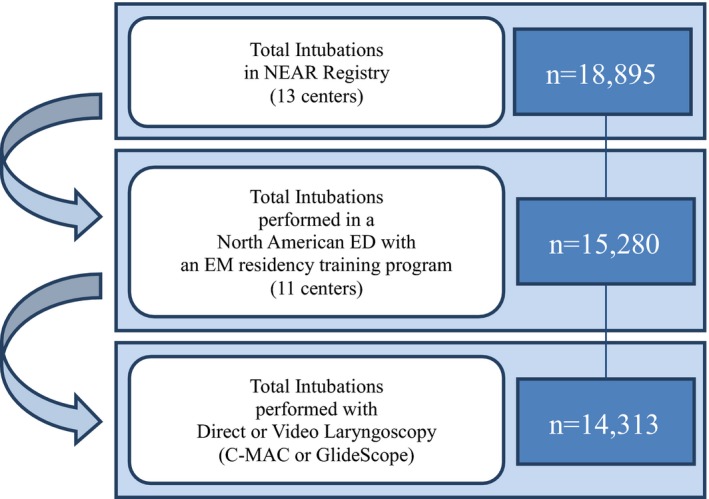
Inclusion criteria and enrollment strategy. NEAR = National Emergency Airway Registry.
Methods of Measurement
Data collected included the type of laryngoscope chosen to perform the intubation, level of training and specialty of the operator, number of attempts, and success or failure.7 If a resident performed an intubation with a video laryngoscope, but did not use the video screen, we categorized this intubation as DL. EM residents who classified themselves as PGY‐4 or PGY‐5 were included with the PGY‐3 residents in a group called “PGY‐3+.”
Data Analysis
Success on the first attempt was calculated for each device and rank. We report the proportion of failed intubations for which the same operator was given a second attempt at securing the airway after failing on first attempt. We present univariate descriptive data as proportions and compare proportions with risk differences (RDs) with 95% confidence intervals (95%CIs). We round RDs to the nearest integer. Finally, we investigated whether DL first‐attempt success decreased as VL became more prevalent, via logistic regression with the following predictors: proportion of encounters with VL at that center in the prior 90 or 365 days, calendar year, and rank. All analyses were adjusted for clustering by center. We performed all analyses with SAS (version 9.4).
Results
Of 18 reporting sites, five were excluded for failing to comply with minimal enrollment requirements (capture of ≥90% of all intubations at the site). Another two were excluded for not having an EM residency program (Figure 1). In the remaining 11 sites, there were 15,280 encounters recorded from July 2002 through December 2012. A total of 14,313 encounters (13,605 adult and 708 pediatric) met inclusion criteria (Figure 1). The majority of excluded intubations were those performed by anesthesiologists or other non‐EM providers or with flexible fiberoptics. EM trainees were the primary operator for 13,183 (92%) of these encounters.
Direct laryngoscopy was the most common initial device, used in 88% of cases (95% CI = 80% to 97%). A C‐MAC was chosen as the first device in 1,088 cases (8%; 95% CI = 0% to 15%) and the GlideScope in 575 cases (4%; 95% CI = 2% to 6%).
Figure 2 demonstrates success on first and multiple attempts, by level of training. First‐attempt success by PGY‐1s was 71% (95% CI = 63% to 78%); PGY‐2s, 82% (95% CI = 78% to 86%); PGY‐3+, 89% (95% CI = 85% to 92%); and attendings 88% (95% CI = 86% to 89%).
Figure 2.
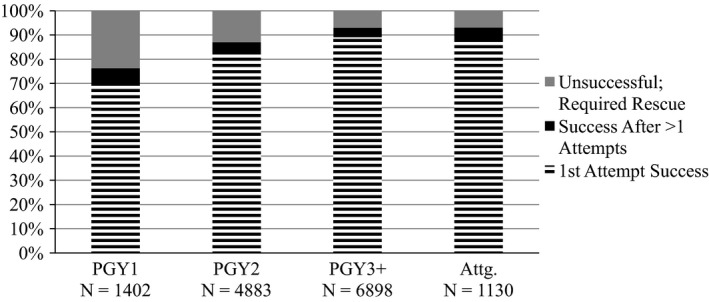
Initial intubations by emergency physicians: success on first and multiple attempts by level of training. *”Intubations” refers to any attempt at passing an endotracheal tube through a glottic opening via either DL, C‐MAC, or GVL. “Success after > 1 attempts” refers to an intubation encounter in which an operator is successful only after two or more attempts. “Unsuccessful; required rescue” refers to an intubation encounter in which an operator is unable to successfully intubate on any number of attempts and a second operator then performs an intubation attempt. DL = direct laryngoscopy; GVL = GlideScope video laryngoscope.
Table 1 compares rates of first‐attempt success for VL versus DL. There was no statistically significant difference at any level. Table 2 compares rates of first‐attempt success for intubations performed with a C‐MAC versus DL. Both PGY‐1s and PGY‐3s had a statistically significant advantage when using C‐MAC versus DL. However, first‐attempt success was no higher with the GlideScope than with DL (Table 3).
Table 1.
First‐attempt Success: VL Versus DL
| Rank | All (n) | Video (n) | Direct (n) | RD between Video and Direct (95% CI) |
|---|---|---|---|---|
| PGY‐1 | 71% (1,402) | 81% (148) | 70% (1,254) | 12% (0% to 23%) |
| PGY‐2 | 82% (4,883) | 86% (628) | 82% (4,255) | 5% (−6% to 15%) |
| PGY‐3+ | 89% (6,898) | 90% (828) | 89% (6,070) | 1% (−4% to 6%) |
| All residents | 84% (13,183) | 88% (1,604) | 84% (11,579) | 4% (−3% to 10%) |
| Attending | 88% (1,130) | 86% (59) | 88% (1,071) | −1% (−20% to 17%) |
First‐attempt success is listed as a percent. “n” refers to the number of attempted intubations for a given subset. “PGY‐3+” refers to PGY‐3–5 residents. “All” refers to intubations performed with either DL or VL. “Video” refers to an intubation performed with either C‐MAC VL or GlideScope VL.
DL = direct laryngoscopy; RD = risk difference; VL = video laryngoscopy.
Table 2.
First‐attempt Success: C‐MAC VL Versus DL
| Rank | C‐MAC (n) | Direct (n) | RD (95% CI) |
|---|---|---|---|
| PGY‐1 | 86% (94) | 70% (1,254) | 17% (4% to 29%) |
| PGY‐2 | 90% (405) | 82% (4,255) | 9% (−1% to 18%) |
| PGY‐3+ | 93% (553) | 89% (6,070) | 5% (3% to 6%) |
| All residents | 92% (1,052) | 84% (11,579) | 8% (4% to 11%) |
| Attending | 89% (36) | 88% (1,071) | 1% (−11% to 14%) |
First‐attempt success is listed as a percent. “n” refers to the number of attempted intubations for a given subset. “PGY‐3+” refers to PGY‐3–5 residents.
DL = direct laryngoscopy; VL = video laryngoscopy.
Table 3.
First‐attempt Success: GlideScope VL Versus DL
| Rank | GlideScope (n) | Direct (n) | RD (95% CI) |
|---|---|---|---|
| PGY‐1 | 72% (54) | 70% (1,254) | 3% (−2% to 8%) |
| PGY‐2 | 79% (223) | 82% (4,255) | −3% (−8% to 2%) |
| PGY‐3+ | 82% (275) | 89% (6,070) | −6% (−16% to 3%) |
| All residents | 80% (552) | 84% (11,579) | −4% (−10% to 1%) |
| Attending | 83% (23) | 88% (1,071) | −5% (−40% to 30%) |
First‐attempt success is listed as a percent. “n” refers to the number of attempted intubations for a given subset. “PGY‐3+” refers to PGY‐3–5 residents.
DL = direct laryngoscopy; RD = risk difference; VL = video laryngoscopy.
We also report the proportion of failed intubations for which a trainee had a second opportunity to perform an intubation, and compare VL with DL (Table 4). PGY‐1s were more likely to have a second opportunity to secure the airway after failing on first attempt when the first attempt was performed with VL versus DL (32% vs. 18%, RD = 14%, 95% CI = 5% to 23%). There was no difference for PGY‐2 or PGY‐3+ residents.
Table 4.
Opportunity to Intubate a Second Time, After First‐attempt Failure: VL Versus DL
| Rank | Video (n) | Direct (n) | RD (95%CI) |
|---|---|---|---|
| PGY‐1 | 32% (28) | 18% (382) | 14% (5% to 23%) |
| PGY‐2 | 44% (86) | 27% (777) | 17% (−2% to 35%) |
| PGY‐3+ | 30% (86) | 38% (695) | −8% (−32% to 17%) |
| All residents | 37% (200) | 29% (1,854) | 7% (−12% to 26%) |
“PGY‐3+” refers to PGY3–5 residents. “n” refers to the number of recorded intubations with first‐attempt failure for a given subset. “Video” refers to an intubation performed with either C‐MAC VL or GlideScope VL.
DL = direct laryngoscopy; RD = risk difference; VL = video laryngoscopy.
We examined the relationship between trainees' first‐attempt success with DL and the proportion of intubations performed with VL at each site, using a multivariable logistic regression model with the following predictors: proportion of encounters with VL at that center in the prior 90 or 365 days, calendar year, and rank (Figure 3). If increasing use of VL caused a decrement in DL skills, we would expect these regression lines to have a negative slope (i.e., an odds ratio [OR] < 1). Instead, a positive slope was observed, suggesting that increasing use of VL did not decrease DL first‐attempt success. The OR for first‐attempt success when the prior 90 days' proportion of video intubations was used as the predictor was 1.24 (95% CI = 1.08 to 1.43; Figure 3) and 1.28 when the prior 365 days' proportion was used (95% CI = 1.06 to 1.54). For both models, Stukel's test of linearity indicated a good fit, with a chi‐square p‐value > 0.50.
Figure 3.
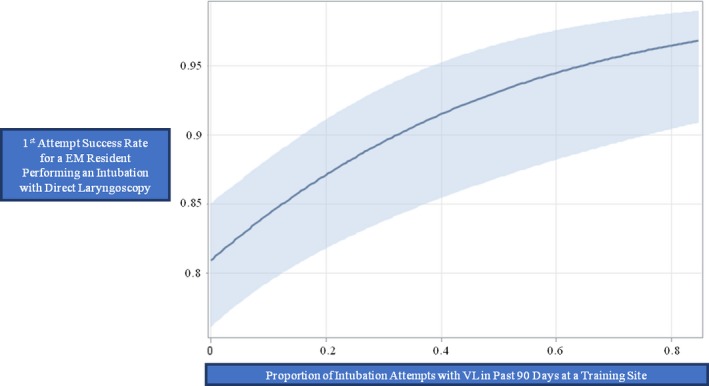
Relationship between prevalence of VL at an individual training site and DL first‐attempt success, via logistic regression with the following predictors: proportion of encounters with VL at that center in the prior 90 days, calendar year, and rank. The odds ratio for first‐attempt success when the prior 90 days' proportion of video intubations was used as the predictor was 1.24. DL = direct laryngoscopy; VL = video laryngoscope.
Discussion
We report on 14,313 ED intubations from 11 North American EM training centers. EM residents performed 92% (13,183) of intubations. To our knowledge, this is the largest sample of North American EM resident intubations to date.
The last publication from this registry evaluating EM resident intubation data reported on 7,498 ED intubations. These were performed almost exclusively with DL and residents were successful on first attempt 85% of the time.1 In our study, we found residents to be successful on first attempt when intubating with DL 84% of the time.
We demonstrate improvement in first‐attempt success rates with increasing years of residency training. Previous analysis reported a similar trend.1, 7 This has been shown for GlideScope intubations in a small sample of EM residents.8 Our study is the first, however, to report an increase in first‐attempt success with each year of training for both GlideScope and C‐MAC.
We cannot infer that the C‐MAC is a superior device for EM resident intubations due to our study limitations, but it is plausible that overall use of VL may allow residents to be more successful when an attending can share a view of the airway and provide real‐time feedback. Although our personal experience is that the mechanics of passing the endotracheal tube are different from an intubation performed with a Macintosh blade (either DL or C‐MAC), our study is not designed to directly compare the first pass success of the C‐MAC with the GlideScope. Mosier et al.9 however did compare ED intubations performed with either the C‐MAC or GlideScope and found no difference in first‐attempt success. Similar equipoise between the C‐MAC and DL has been shown in a retrospective study of pediatric ED intubations and a recent randomized trial of adult ED patients intubated with either the C‐MAC or the DL.10, 11 A trainee performed > 97% of the intubations in both studies and neither found a statistical difference in first intubation attempt success.10, 11
Our study also measured the likelihood that a resident who fails on first‐attempt intubation has a second attempt. We report that when an intern fails to successfully intubate on the first attempt, he or she is more likely to have a second opportunity to intubate that patient if the first attempt was performed with a video laryngoscope (Table 4). This was not true for the PGY‐2 or PGY‐3+ groups. We suspect that VL helps an attending determine whether first attempt failure was related to the intubating resident or a challenge intrinsic to the patient (e.g., anatomy). If the former, then perhaps an intern is more likely to have a second attempt after the attending provides feedback. If the challenge is intrinsic to the patient, then perhaps a more experienced resident would step in for a rescue intubation. To our knowledge, we are the first study to investigate the opportunity for an EM resident to try again after first attempt failure. This topic is important because it reflects a resident's learning opportunity to develop fine motor skills, adapt after failure, and build confidence.
Finally, we found no evidence for the theory that EM physicians may be losing DL skills in the setting of increasing utilization of VL. We found a positive association between the prevalence of VL and first‐attempt success with DL, while the opposite would be expected if training with VL caused a decrement in DL skills. It is possible that residents learning how to intubate predominantly with VL are visualizing airway anatomy in a way that enhanced comfort with the procedure and ability to identify anatomical structures. This may then allow the learner to identify the same structures more easily when intubating with DL. Future regression models incorporating providers' experience with airway management and patient characteristics will be better positioned to draw a conclusion about the relationship between VL prevalence and DL success.
Limitations
National Emergency Airway Registry is designed to monitor trends in airway management and provide performance expectations using a large, prospectively collected data. There are limitations to this design and analysis. Like all self‐reporting registries, NEAR is subject to possible recall bias and selective reporting of adverse events. During analysis, operators are deidentified, which should remove the desire to inflate performance through selective reporting. While we are unable to say with certainty that this did not occur, we do not know of any intentional errors. Compliance reporting and continuous monitoring across sites limit this potential impact.
Most intubations were performed at urban academic centers and may not reflect trends and practices at rural training sites. In our study period, most intubations (88%) in the registry were managed with DL. VL intubations were concentrated in the past 3 years.7 Although our sample is large, this concentration may limit our ability to capture an association between an increased prevalence of VL and decrease in DL success. We can extrapolate from this trend that the prevalence of VL has or may soon surpass DL. Our data may not match current practice at academic medical centers. Newer NEAR data are currently being collected but are incomplete. We believe that these data, however, reflect the period when VL was being introduced into practice. This provides a benchmark and context for future studies of ED intubation performance.
Center characteristics including annual volume have been reported previously.7 However, our analysis of first‐attempt success, second‐attempt opportunity, and regression model do not factor in patient characteristics (e.g., anatomy or indication for intubation) or provider differences (e.g., operator experience). We do not know if only one type of video laryngoscope was available at an individual site or if a particular laryngoscope was the typical device of choice for an anticipated difficulty airway. Despite our large sample size and adjustment for clustering by center, these confounders preclude us from drawing conclusions about device superiority or the relationship between the proportion of VL intubations at a training site and a resident's performance with DL.
Conclusions
In summary, we have presented data on 14,313 ED intubations, performed with either direct laryngoscopy or video laryngoscopy. This is the largest sample of EM resident intubations published to date and provides outcomes of first‐attempt success, the opportunity to try a second time after failure, and a model for the association between video laryngoscopy prevalence and direct laryngoscopy skills. Nearly all ED intubations (92%) at a hospital with an emergency medicine training program were performed by emergency medicine residents. This speaks to the acceptance across specialties that emergency intubations can be safely performed by emergency physicians. We found that interns and PGY‐3+ residents were more likely to intubate successfully on the first attempt when using C‐MAC versus direct laryngoscopy. Interns were more likely to have a second attempt at intubation after failing first attempt with a video laryngoscope versus direct laryngoscopy. We did not find evidence for the theory that the increasing use of video laryngoscopy is associated with a loss of direct laryngoscopy skills. These findings describe the clinical learning environment for emergency medicine residents and may provide national benchmarks for medical educators and residency program directors. Surveillance of resident intubation outcomes should be continued as video laryngoscopy overtakes direct laryngoscopy as the primary device with which emergency medicine physicians perform endotracheal intubation.
AEM Education and Training 2019;3:156–162
Presented at the Society for Academic Emergency Medicine Annual Meeting, Orlando, FL, May 2017.
The authors have no relevant financial information or potential conflicts to disclose.
Author contributions: DLM, JLB, JTM, SCC, MTS, AE, and DJP contributed to study design; CAB and DJP monitored data acquisition and compliance; DLM and DJP analyzed and interpreted the data; DLM drafted the manuscript; CAB, JLB, JM, SCC, MTS, AE, and DJP contributed to manuscript revisions; DJP, JLB, JTM, SCC, and MTS provided statistical expertise; and DJP and CAB provided acquisition of funding.
References
- 1. Sagarin MJ, Barton ED, Chng YM, Walls RM. Airway management by US and Canadian emergency department residents: a multicenter analysis of more than 6,000 endotracheal intubation attempts. Ann Emerg Med 2005;46:328–36. [DOI] [PubMed] [Google Scholar]
- 2. Swaminathan AK, Berkowitz R, Baker A, Spyres M. Do emergency medicine residents receive appropriate video laryngoscopy training? A survey to compare the utilization of video laryngoscopy devices in emergency medicine residency programs and community emergency departments. J Emerg Med 2015;48:613–9. [DOI] [PubMed] [Google Scholar]
- 3. Pallin DJ, Dwyer RC, Walls RM, Brown CA. Techniques and trends, success rates, and adverse events in emergency department pediatric intubations: a report from the National Emergency Airway Registry. Ann Emerg Med 2016;67:610–5. [DOI] [PubMed] [Google Scholar]
- 4. Sakles JC, Mosier JM, Chiu S, Cosentino M, Kalin L. A comparison of the C‐MAC video laryngoscope to the Macintosh direct laryngoscope for intubation in the emergency department. Ann Emerg Med 2012;60:739–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mosier JM, Stolz U, Chiu S, Sakles JC. Difficult airway management in the emergency department: GlideScope videolaryngoscopy compared to direct laryngoscopy. J Emerg Med 2012;42:629–34. [DOI] [PubMed] [Google Scholar]
- 6. Vassiliadis J, Tzannes A, Hitos K, Brimble J, Fogg T. Comparison of the C‐MAC video laryngoscope with direct Macintosh laryngoscope in the emergency department. Emerg Med Australas 2015;27:119–25. [DOI] [PubMed] [Google Scholar]
- 7. Brown CA 3rd, Bair AE, Pallin DJ, Walls RM. Techniques, success, and adverse events of emergency department adult intubations. Ann Emerg Med 2015;65:363–70. [DOI] [PubMed] [Google Scholar]
- 8. Sakles JC, Mosier J, Patanwala AE, Dicken J. Learning curves for direct laryngoscopy and GlideScope video laryngoscopy in an emergency medicine residency. West J Emerg Med 2014;15:930–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mosier J, Chiu S, Patanwala AE, Sakles JC. A comparison of the GlideScope video laryngoscope to the C‐MAC video laryngoscope for intubation in the emergency department. Ann Emerg Med 2013;61:414–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Eisenberg MA, Green‐Hopkins I, Werner H, Nagler J. Comparison between direct and video‐assisted laryngoscopy for intubations in a pediatric emergency department. Acad Emerg Med 2016;23:870–7. [DOI] [PubMed] [Google Scholar]
- 11. Driver BE, Prekker ME, Moore JC, Schick AL, Reardon RF, Miner JR. Direct versus video laryngoscopy using the C‐MAC for tracheal intubation in the emergency department, a randomized controlled trial. Acad Emerg Med 2016;23:433–9. [DOI] [PubMed] [Google Scholar]


