Abstract
Background
Children and adolescents who have experienced trauma are at high risk of developing post‐traumatic stress disorder (PTSD) and other negative emotional, behavioural and mental health outcomes, all of which are associated with high personal and health costs. A wide range of psychological treatments are used to prevent negative outcomes associated with trauma in children and adolescents.
Objectives
To assess the effects of psychological therapies in preventing PTSD and associated negative emotional, behavioural and mental health outcomes in children and adolescents who have undergone a traumatic event.
Search methods
We searched the Cochrane Common Mental Disorders Group's Specialised Register to 29 May 2015. This register contains reports of relevant randomised controlled trials from The Cochrane Library (all years), EMBASE (1974 to date), MEDLINE (1950 to date) and PsycINFO (1967 to date). We also checked reference lists of relevant studies and reviews. We did not restrict the searches by date, language or publication status.
Selection criteria
All randomised controlled trials of psychological therapies compared with a control such as treatment as usual, waiting list or no treatment, pharmacological therapy or other treatments in children or adolescents who had undergone a traumatic event.
Data collection and analysis
Two members of the review group independently extracted data. We calculated odds ratios for binary outcomes and standardised mean differences for continuous outcomes using a random‐effects model. We analysed data as short‐term (up to and including one month after therapy), medium‐term (one month to one year after therapy) and long‐term (one year or longer).
Main results
Investigators included 6201 participants in the 51 included trials. Twenty studies included only children, two included only preschool children and ten only adolescents; all others included both children and adolescents. Participants were exposed to sexual abuse in 12 trials, to war or community violence in ten, to physical trauma and natural disaster in six each and to interpersonal violence in three; participants had suffered a life‐threatening illness and had been physically abused or maltreated in one trial each. Participants in remaining trials were exposed to a range of traumas.
Most trials compared a psychological therapy with a control such as treatment as usual, wait list or no treatment. Seventeen trials used cognitive‐behavioural therapy (CBT); four used family therapy; three required debriefing; two trials each used eye movement desensitisation and reprocessing (EMDR), narrative therapy, psychoeducation and supportive therapy; and one trial each provided exposure and CBT plus narrative therapy. Eight trials compared CBT with supportive therapy, two compared CBT with EMDR and one trial each compared CBT with psychodynamic therapy, exposure plus supportive therapy with supportive therapy alone and narrative therapy plus CBT versus CBT alone. Four trials compared individual delivery of psychological therapy to a group model of the same therapy, and one compared CBT for children versus CBT for both mothers and children.
The likelihood of being diagnosed with PTSD in children and adolescents who received a psychological therapy was significantly reduced compared to those who received no treatment, treatment as usual or were on a waiting list for up to a month following treatment (odds ratio (OR) 0.51, 95% confidence interval (CI) 0.34 to 0.77; number needed to treat for an additional beneficial outcome (NNTB) 6.25, 95% CI 3.70 to 16.67; five studies; 874 participants). However the overall quality of evidence for the diagnosis of PTSD was rated as very low. PTSD symptoms were also significantly reduced for a month after therapy (standardised mean difference (SMD) ‐0.42, 95% CI ‐0.61 to ‐0.24; 15 studies; 2051 participants) and the quality of evidence was rated as low. These effects of psychological therapies were not apparent over the longer term.
CBT was found to be no more or less effective than EMDR and supportive therapy in reducing diagnosis of PTSD in the short term (OR 0.74, 95% CI 0.29 to 1.91; 2 studies; 160 participants), however this was considered very low quality evidence. For reduction of PTSD symptoms in the short term, there was a small effect favouring CBT over EMDR, play therapy and supportive therapies (SMD ‐0.24, 95% CI ‐0.42 to ‐0.05; 7 studies; 466 participants). The quality of evidence for this outcome was rated as moderate.
We did not identify any studies that compared pharmacological therapies with psychological therapies.
Authors' conclusions
The meta‐analyses in this review provide some evidence for the effectiveness of psychological therapies in prevention of PTSD and reduction of symptoms in children and adolescents exposed to trauma for up to a month. However, our confidence in these findings is limited by the quality of the included studies and by substantial heterogeneity between studies. Much more evidence is needed to demonstrate the relative effectiveness of different psychological therapies for children exposed to trauma, particularly over the longer term. High‐quality studies should be conducted to compare these therapies.
Plain language summary
Psychological therapies for preventing post‐traumatic stress disorder in children and adolescents
Why is this review important?
Children and adolescents who have experienced trauma are at high risk of developing post‐traumatic stress disorder (PTSD) and negative psychological and social outcomes.
Who will be interested in this review?
Children and adolescents who have undergone trauma and their families and caregivers will be interested in this review, along with healthcare professionals, particularly those working in mental health services for children and adolescents.
What questions does this review aim to answer?
• What are the effects of psychological therapies in preventing PTSD and other negative emotional, behavioural and mental health outcomes in children and adolescents exposed to a traumatic event?
• Which psychological therapies are most effective?
• Are psychological therapies more effective than pharmacological therapies or other treatments?
Which studies were included in the review?
Review authors searched databases to May 2015 to find all relevant trials. To be included in the review, studies had to be randomised controlled trials and had to include both children and adolescents exposed to trauma.
We included 51 trials with a total of 6201 participants. Participants had been exposed to sexual abuse in 12 trials, to war or community violence in ten, to physical trauma and natural disaster in six each and to interpersonal violence in three. In one trial each, participants had suffered a life‐threatening illness or had been physically abused or maltreated. Participants in the remaining trials were exposed to a range of traumas.
Most trials compared psychological therapy with a control condition such as treatment as usual, waiting list or no treatment; others compared different psychological therapies.
A total of 43 studies reported outcomes recorded within the first month after treatment; 27 studies reported outcomes from one month up to a year, and eight reported data for a year or longer after treatment.
What does evidence presented in the review tell us?
Children and adolescents receiving psychological therapies were less likely to be diagnosed with PTSD and had fewer symptoms of PTSD up to a month after treatment compared with those who received no treatment, treatment as usual or were on a waiting list. Our confidence in these findings is limited as the overall quality of evidence was very low to low. There was no evidence for the effectiveness of psychological therapies beyond one month. There was moderate quality evidence that cognitive‐behavioural therapy (CBT) might be more effective in reducing symptoms of PTSD compared to other psychological therapies for up to a month. Adverse effects were not reported. There were no studies which compared psychological therapies to drug treatments.
What should happen next?
Researchers should conduct high‐quality trials to further evaluate the effectiveness of psychological therapies for children and adolescents exposed to trauma. These trials should be designed to ensure that participants and their families are not aware of whether they are receiving psychological therapy, particularly when measures are completed by participants or their parents. In addition, efforts should be made to ensure high rates of follow‐up beyond one month after completion of therapy.
In addition, studies should compare different types of psychological therapy to give a better indication of whether children and adolescents exposed to different types of trauma are more or less likely to respond to these therapies.
Summary of findings
Summary of findings for the main comparison. Psychological therapies versus wait list, treatment as usual or no treatment for children and adolescents exposed to trauma (short‐term).
| Patient or population: children and adolescents exposed to trauma Setting: three hospitals and fourteen community/outpatient settings (including eight schools, a trauma clinic, child support services, foster care and youth support services) in the US (6), Australia (2), Democratic Republic of Congo (2), Israel (2), the Palestinian territories (2), Bosnia(1), Canada (1), and Indonesia (1). Intervention: all psychological therapies Comparison: control (short‐term) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with control (short‐term) | Risk with all psychotherapies | |||||
| PTSD diagnosis | Study population | OR 0.51 (0.34 to 0.77) | 874 (5 studies) | ⊕⊝⊝⊝ Very lowa,b,c | ||
| 367 per 1000 | 228 per 1000 (165 to 309) | |||||
| Moderate | ||||||
| 345 per 1000 | 212 per 1000 (152 to 288) | |||||
| PTSD total symptoms | Mean PTSD total symptoms in the intervention group 0.42 standard deviations undefined fewer (0.61 fewer to 0.24 fewer) | Moderate effect size | 2051 (15 studies) | ⊕⊕⊝⊝ Lowd,e | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and relative effect of the intervention (and its 95% CI) CI: confidence interval; OR: odds ratio; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect but may be substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aParticipants are likely to have been aware of whether they received the active or inactive intervention in all studies, and diagnosis was based on self reported measures in 2 studies bSignificant difference between the 2 psychological therapies included in this analysis (i.e. CBT and family therapy) (I2 = 69%) cOnly 3 included studies with a relatively small overall sample number of 352
dParticipants were likely to have been aware of whether they received active or inactive intervention in all but one study, and scores were based on self reported measures in 10 studies
eSubstantial heterogeneity between different types of psychological therapy (I2 = 71%)
Summary of findings 2. CBT versus other psychological therapies for children and adolescents exposed to trauma (short‐term).
| Patient or population: children and adolescents exposed to trauma Setting: All seven studies were done in community or outpatient settings including child trauma (2) or psychiatric (2) services, child support services (1), domestic violence service (1) and school (1) in the US (4), Netherlands (2), and Iran (1). Intervention: CBT Comparison: other psychological therapies (short‐term) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Numer of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with other therapies (short‐term) | Risk with CBT | |||||
| PTSD diagnosis | Study population | OR 0.74 (0.29 to 1.91) | 160 (2 studies) | ⊕⊝⊝⊝ Very lowa,b | ||
| 141 per 1000 | 108 per 1000 (45 to 239) | |||||
| Moderate | ||||||
| 111 per 1000 | 85 per 1000 (35 to 193) | |||||
| PTSD total symptoms | Mean PTSD total symptoms in the intervention group 0.24 standard deviations undefined fewer (0.42 fewer to 0.05 fewer) | Small effect size | 466 (7 studies) | ⊕⊕⊕⊝ Moderatec | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and relative effect of the intervention (and its 95% CI) CI: confidence interval; OR: odds ratio; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of effect but may be substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aParticipants are likely to have been aware of whether they received active or inactive intervention in both studies, and diagnosis was based on self reported measures in both bOnly 2 included studies with a relatively small overall sample number of 287
cParticipants are likely to have been aware of whether they received active or inactive intervention in all studies, and scores were based on self reported measures in 4 studies
Background
Description of the condition
Children and adolescents exposed to trauma are at high risk of post‐traumatic stress disorder (PTSD) and other negative emotional, behavioural and mental health outcomes. Although estimates of the prevalence of PTSD in children and adolescents who have experienced trauma vary, most studies have reported prevalence of 30% to 40% (AACAP 1998; Fletcher 2003; McNally 1996; Saigh 1996), and a meta‐analysis of 34 studies of 2697 children and adolescents exposed to traumatic events (Fletcher 2003) reported an overall prevalence of 36%. The prevalence of PTSD appears to vary with several factors, such as type of trauma, frequency and severity of exposure and time since the traumatic event (Carr 2004; Donnelly 2002; Fletcher 2003; Foy 1996; Yule 2001). Multiple studies have identified co‐morbidities between PTSD and other psychiatric disorders, including depression and anxiety disorders, externalising disorders, substance use and suicidal ideation (AACAP 1998; APA 2000; Donnelly 2002; Perrin 2000).
Characteristic symptoms of PTSD include re‐experiencing the trauma (such as recurrent memories or nightmares), avoiding stimuli associated with the trauma and increased arousal and reactivity (APA 2000; WHO 1990). According to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM‐IV‐TR) criteria for a PTSD diagnosis, symptoms must be present for at least a month and must cause clinically significant distress or impairment in social, occupational or other important areas of function (APA 2000). Types of traumatic events that may cause PTSD include natural and man‐made disasters, war, physical or sexual abuse, violence to self or others, exposure to suicidal acts, serious injury and life‐threatening illness such as cancer or severe burns (AACAP 1998; APA 2000; Parry‐Jones 1995).
Description of the intervention
For children who have been exposed to trauma, psychological therapies are intended to prevent the onset of trauma‐related symptoms or PTSD (Forman‐Hoffman 2013). Although a range of psychological therapies are used with people exposed to trauma (see How the intervention might work), most therapies are based on one or more common elements. These may include psychoeducational elements, which may help traumatised children or adolescents to normalise PTSD reactions; psychodynamic elements, which can help them to process the trauma emotionally and gain a better understanding of its meaning to them; exposure elements, which can desensitise them to trauma‐related memories; cognitive‐behavioural elements, which help them rethink assumptions and reactions to the traumatic event; and coping elements or skills, such as problem solving, safety planning and anxiety management (AACAP 2010; Carr 2004; Robertson 2004; Sones 2011). Inclusion of parents may enhance the effectiveness of these therapies with children and adolescents by improving parental recognition of trauma symptoms and enhancing their ability to help with their child's emotional distress and to manage related behaviour problems (AACAP 2010). Psychological therapies may be targeted to the individual or may be group‐based, and the frequency and duration of treatment may vary widely.
How the intervention might work
Several trauma‐specific and generic psychological therapeutic approaches have been used to prevent negative outcomes among children and adolescents who have undergone trauma. Cognitive‐behavioural therapy (CBT) challenges the distorted, negative thinking patterns associated with the trauma to help people develop more adaptive cognitions and behaviours (Robertson 2004; Sones 2011). Exposure therapy is used to help people overcome symptoms by exposing them to specific or non‐specific cues or memories related to the trauma (Neuner 2004; Robertson 2004). Because the fragmentation and distortion of memories and cognitions associated with trauma are thought to prevent symptom resolution, narrative therapy can be used to help someone reconstruct a consistent narrative about the trauma (Neuner 2004). Therapists work with individuals in psychodynamic psychotherapy to help them develop a better understanding of their responses to the trauma and how it impacts their feelings, behaviours and relationships (AACAP 2010; BluePages 2012; Foa 1997). In eye movement desensitisation and reprocessing (EMDR), the individual focuses on a disturbing image, memory, emotion or cognition associated with the trauma, while the therapist initiates rapid voluntary eye movements (Bryant 2001; Robertson 2004). Other therapies include supportive therapy, whereby counsellors give support, listen to people and help them talk over their problems (BluePages 2012); debriefing, which allows emotional processing or ventilation by encouraging recollection, ventilation and reworking of the traumatic event (Rose 2002); and family therapy, which can reduce psychological symptoms by focusing on improving family communication and functioning (Henken 2007).
Why it is important to do this review
Although a Cochrane review has been conducted to examine the effectiveness of psychological interventions for children and adolescents diagnosed with PTSD (Gillies 2012), no Cochrane reviews have studied available psychological therapies for prevention of PTSD in children and adolescents exposed to trauma. Therefore, we have prepared this Cochrane review to address the remaining need for a systematic review of the effectiveness of psychological therapies for prevention of PTSD and other negative outcomes in children and adolescents who have undergone trauma.
Objectives
To assess the effects of psychological therapies in preventing PTSD and associated negative emotional, behavioural and mental health outcomes in children and adolescents who have undergone a traumatic event.
Methods
Criteria for considering studies for this review
Types of studies
All relevant randomised and quasi‐randomised controlled trials. Quasi‐randomised studies included studies that used allocation methods with no apparent association with participant characteristics. For example, we could include studies that allocated participants on the basis of the last numeral of the medical identifier number or the last numeral of the date of birth.
All cross‐over trials and cluster‐randomised trials were eligible for inclusion.
Types of participants
Participant characteristics
We included studies of children or adolescents, boys and girls, up to and including 18 years of age, who had been exposed to a traumatic event. Trauma is defined as an event in which the child or adolescent experienced, witnessed or was confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others, and response involved intense fear, helplessness or horror, which in children may be expressed as disorganised or agitated behaviour (APA 2000). Trauma may include natural or man‐made disaster, physical or sexual abuse, war, violence and life‐threatening injury.
The primary criterion of exposure to trauma differentiates this review, which focuses on the effectiveness of psychological therapies in prevention of PTSD, from the previously published review on psychological therapies as treatment for children and adolescents with PTSD (Gillies 2012).
Diagnosis
Although the inclusion criterion for this review was exposure to trauma, participants in some identified studies may have been diagnosed with PTSD or might have had baseline symptom scores that were above validated cut‐off scores for PTSD. Therefore, for this review we included studies if less than 50% of participants in both groups had baseline symptom scores above validated cut‐offs, or were diagnosed with PTSD using validated methods. When 50% or more of participants received a diagnosis of PTSD or had baseline scores above validated cut‐off scores, these were considered treatment studies and included in Gillies 2012 or, if newly identified, will be included in updates of Gillies 2012.
Co‐morbidities
We included studies of participants with any co‐morbidity.
Setting
We placed no restriction on the setting of studies.
Subset data
If children and adolescents were randomised separately, and if data for children or adolescents were reported as a subset of data in a study that included adults, we would have included these data.
Types of interventions
Experimental interventions
Major categories of psychological therapies included CBT (including both cognitive and behavioural components), exposure therapy, family therapy, EMDR, narrative therapy, psychodynamic therapy (including play therapy), psychoeducation, immediate post‐trauma interventions such as debriefing and psychological first aid and supportive therapy (including non‐directive counselling). Therapies had to be used primarily with the child or adolescent and could be delivered in any format including individual or group therapies but could also include parents or could have parents attend parallel sessions.
Comparator interventions
Control (treatment as usual, waiting list controls or no treatment).
Another psychological therapy.
Pharmacological therapy.
Types of outcome measures
Reports of the following outcomes were not required for studies to be considered for inclusion in this review. If it was apparent that these outcomes had not been measured (rather than had not been reported) upon review of these studies, we excluded them and provided the reasons for exclusion.
Primary outcomes
1. Diagnosis of post‐traumatic stress disorder determined by accepted clinical diagnostic criteria such as International Classification of Diseases, Revision 10 (ICD‐10), or DSM‐IV‐TR.
2. Symptoms of PTSD measured on scales based on diagnostic criteria such as ICD‐10 or DSM‐IV‐TR with published reliability and validity (e.g. Children's PTSD Inventory) (Saigh 2000).
Secondary outcomes
3. Severity or incidence of anxiety symptoms (e.g. State‐Trait Anxiety Inventory for Children) (Spielberger 1973).
4. Severity or incidence of depressive symptoms (e.g. Children's Depression Inventory) (Kovacs 1992).
5. Severity or incidence of behavioural problems (e.g. Child Behavior Checklist) (Achenbach 1983).
6. Function (e.g. Children's Global Assessment Scale) (Schaffer 1983).
7. Quality of life (e.g. Pediatric Quality of Life Inventory, version 4.0) (Varni 2001).
8. Any adverse events including self harm or suicidal behaviour.
9. Cost.
10. Loss to follow‐up.
Outcome scales
We included outcome data only if the scale or questionnaire was reported to be valid and reliable in a peer‐reviewed journal. If useable data for a particular outcome were collected from different sources (i.e. PTSD symptoms reported by child and parent in Celano 1996, Danielson 2012, Jaberghaderi 2004, Kemp 2010 and Schottelkorb 2012), we used data that showed the highest response rates. If follow‐up was the same for all raters, we used clinician scales in preference because these were based on clinician interview with child and parent, which is considered by expert groups as the most valid form of assessment (AACAP 1998).
Timing of outcome assessment
Data were analysed as short‐term (up to and including one month following completion of therapy), medium‐term (between one month and one year following therapy) and long‐term (one year or longer).
Hierarchy of outcome measures
If two or more sets of data were available for any of these periods, we used the first data set. For example, if follow‐up data were reported at three months and six months, we used data for the three‐month follow‐up period.
Search methods for identification of studies
Cochrane Common Mental Disorders Group's Specialised Register (CCMDCTR)
The Cochrane Common Mental Disorders Group maintains a specialised register of randomized controlled trials, the CCMDCTR. This register contains over 40,000 reference records (reports of RCTs) for anxiety disorders, depression, bipolar disorder, eating disorders, self‐harm and other mental disorders within the scope of this Group. The CCMDCTR is a partially studies based register with >50% of reference records tagged to c12,500 individually PICO coded study records. Reports of trials for inclusion in the register are collated from (weekly) generic searches of Medline (1950‐), Embase (1974‐) and PsycINFO (1967‐), quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL) and review specific searches of additional databases. Reports of trials are also sourced from international trial registries, drug companies, the hand‐searching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses. Details of CCMD's core search strategies (used to identify RCTs) can be found on the Group's website with an example of the core Medline search displayed in Appendix 1.
Electronic searches
1. Cochrane Specialised Register
CCDMDCTR ‐ Studies Register
We searched the studies register (to 29‐May‐2015) using the following terms.
Diagnosis = ("post‐traumatic stress disorders" or "acute stress disorder" or stress) and Age‐Group = (child or adolescent) and Intervention = (counsel* or *therapy or intervention or training or *education).
CCDMDCTR ‐ References Register
We searched the References Register (to 29‐May‐2015) using a more sensitive set of free‐text terms to identify additional untagged/uncoded references.
Title/Abstract/Keywords = (PTSD or “post trauma*” or post‐trauma* or posttrauma* or trauma* or stress) and (adolesc* or preadolesc* or pre‐adolesc* or boy* or girl* or child* or infant* or juvenil* or minors or school* or pediatri* or paediatri* or pubescen* or puberty or student* or teen* or young or youth* or school* or high‐school or “high school” or college or undergrad*).
2. Interntional Trial Registers
We searched ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform (ICTRP) to 29‐May‐2015
Searching other resources
We checked reference lists of relevant studies and reviews for additional references to potentially relevant studies. We included non‐English language studies.
Data collection and analysis
Selection of studies
Two review authors checked the results of database searches to exclude references that clearly were not relevant to the review. These review authors then assessed titles and/or abstracts of the remaining studies, as well as studies identified by other methods, to determine eligibility for the review. We resolved disagreements regarding selection of studies through consensus or, if necessary, by consultation with a third member of the review team. When doubt remained, we obtained and reviewed the full‐text article. When further clarification by study authors was needed for a decision, we made all reasonable attempts to contact them.
Data extraction and management
Members of the review team developed and piloted a data extraction form. Two members of the review group independently extracted methodological and outcome data from each study. Each pair then compared results to identify differences. If identified, we resolved differences by consensus or by referral to a third member of the review team. When further clarification or missing data were needed from study authors, we made all reasonable attempts to contact them.
Extracted data included information about participants, including inclusion criteria, exclusion criteria and number, age, ethnicity and gender; details of study setting and information on trauma exposure and symptoms; information on interventions, including major components of each therapy as described by study authors, whether treatment was manualised and length, frequency and format of sessions; the professional background of therapists, any intervention training received and supervision or fidelity; and outcomes, including which measures were used, who rated them and when they were measured. These study characteristics are reported in the Characteristics of included studies tables, with details provided by study authors.
The three main planned comparisons were:
psychological therapies versus control (wait list, treatment as usual, no treatment);
psychological therapies versus other psychological therapies; and
psychological therapies versus pharmacological therapies.
We organised data under the following categories of psychological therapies.
Cognitive‐behavioural therapy (CBT).
Eye movement desensitisation and reprocessing (EMDR).
Exposure‐based therapy.
Family therapy.
Narrative therapy.
Post‐trauma interventions (including debriefing and psychological first aid).
Psychodynamic psychotherapy (including play therapy).
Psychoeducation.
Supportive therapy (including non‐directive counselling).
Assessment of risk of bias in included studies
We independently assessed trials as having 'low', 'high' or 'unclear' risk of bias according to the following quality criteria (Higgins 2008).
Adequate sequence generation (selection bias).
Allocation concealment (selection bias).
Blinding of participants (performance bias).
Blinding of outcome assessment (detection bias).
Incomplete outcome data (attrition bias).
Free of selective reporting (selective reporting).
Free of any other bias.
When disagreement arose about whether a trial fulfilled particular quality criteria, we resolved differences by consensus or by referral to a third member of the review team.
As little is available to inform levels of attrition that are acceptable, it is difficult to make an objective judgement about the level of attrition bias; therefore, we considered two factors: percentage loss to follow‐up and use of imputed data; the latter was treated as a positive factor against attrition bias. Therefore, we considered attrition of less than 5% as associated with low risk of bias, whether completer or imputed data were reported. If attrition was between 5% and 15%, it was considered to involved unclear risk of bias if completer data were reported, and low risk if imputed data were reported. if attrition was greater than 15% up to 30%, completer data were considered to show high risk, and imputed data as unclear risk; if attrition was greater than 30%, both were considered to show high risk of attrition bias. If loss to follow‐up was greater than 50% in either group, we did not include study data. We investigated potential differences between groups in loss to follow‐up by performing meta‐analysis.
Measures of treatment effect
Dichotomous data
For binary outcomes, we calculated the odds ratio (OR) and the 95% confidence interval (95% CI) by using a random‐effects model.
Continuous data
We calculated the standardised mean difference (SMD) and the 95% CI of continuous outcomes by using a random‐effects model. SMDs were used to pool continuous outcomes when different measures were used. However, to ensure consistency of reporting in this review, we used SMDs throughout.
To calculate SMDs, we needed means and standard deviations (SDs). If SDs were not reported, we calculated them from reported measures of variance such as standard errors or 95% CIs, if possible.
Skewed data
As a meta‐analysis is based on assumptions of normality, we checked all continuous data for skew before inclusion. For a scale that starts from zero, we considered a standard deviation that is more than half the mean to show strong evidence of a skewed distribution (Higgins 2008). Therefore, if the standard deviation was greater than the mean for both groups, we did not include these data in a meta‐analysis and reported them separately.
Unit of analysis issues
Cross‐over trials
We identified no cross‐over trials. If we had found these, we would have used only first interval data, as the likelihood of a carryover effect is high when psychological therapy is provided.
Cluster‐randomised trials
We intended to correct data for cluster‐randomised trials for paired analysis; however, as intracluster correlations were not available for these trials, we conducted sensitivity analyses to identify whether inclusion of these trials had affected meta‐analytical findings.
Studies with multiple treatment groups
If a study included multiple treatment arms that described different comparisons, we would have analysed these separately. For example, if a three‐armed trial incorporated narrative therapy, supportive therapy and a control treatment arm, we would use these data in comparisons of narrative therapy versus control, supportive therapy versus control and narrative therapy versus supportive therapy. However, no studies in this review reported multiple treatment arms.
Dealing with missing data
We used intention‐to‐treat data and imputed values such as last observation carried forward when these were reported. We conducted sensitivity analyses to test for effects of loss to follow‐up on the stability of results.
Assessment of heterogeneity
We used a Mantel‐Haenszel Chi2 statistic test and I2 analysis to test for heterogeneity.
Based on the recommendations of Higgins 2008 (9.5.2), we interpreted heterogeneity by using the following values of I2.
0% to 40%: might not be important.
30% to 60%: may represent moderate heterogeneity.
50% to 90%: may represent substantial heterogeneity.
75% to 100%: shows considerable heterogeneity.
Assessment of reporting biases
We entered primary outcome data from all included studies into a funnel plot (trial effect against trial size) to investigate the possibility of publication bias (Egger 1997).
Data synthesis
We collected data for all follow‐up periods as long as loss to follow‐up did not exceed 50% for either group. We analysed data as short‐term (up to and including one month following completion of therapy), medium‐term (between one month and one year following therapy) and long‐term (one year or longer). If two or more more sets of useable data were provided for any of these periods, we used the first data set.
When studies reported data for more than one group (e.g. Tol 2012, which reported data for boys and girls separately), we calculated pooled means and standard deviations and used them in the meta‐analysis.
In meta‐analyses of psychological therapies versus control, we used studies that compared an added psychological therapy versus another psychological therapy (i.e. Berliner 1996, which compared exposure plus supportive therapy versus supportive therapy only, and Deblinger 2011, which compared narrative therapy plus CBT versus CBT) when the additional psychological therapy was considered the control intervention. We investigated effects of psychological therapies as controls in the sensitivity analysis for active versus inactive controls (Analysis 11.1; Analysis 11.2).
11.1. Analysis.

Comparison 11 Sensitivity analysis: type of control, Outcome 1 PTSD diagnosis.
11.2. Analysis.

Comparison 11 Sensitivity analysis: type of control, Outcome 2 PTSD total symptoms.
When cluster‐randomised trials were identified, we would have made appropriate corrections for the cluster design if appropriate data had been reported, and these data were incorporated into the meta‐analyses. However, data that could be used to make these corrections were not reported.
Subgroup analysis and investigation of heterogeneity
We explored whether clinical differences between studies may have resulted in different estimates of effectiveness through subgroup analyses. These included
type of therapy: CBT, debriefing, EMDR, family therapy, narrative therapy, psychoeducation, supportive therapy;
type of trauma: sexual abuse, maltreatment, physical trauma, life‐threatening illness, interpersonal violence, community violence or war, natural disaster. For studies that included participants who had experienced a range of traumas, if most experienced a particular type of trauma (e.g. Berkowitz 2011, in which most participants experienced physical trauma), we analysed them under this category;
therapy mode: individual versus group, child versus mother, child therapy;
type of control: active control (e.g. treatment as usual, which included elements of psychological therapy, or compared a particular psychological therapy as an adjunct to another therapy) or inactive control (e.g. no treatment, wait list, craft group); and
inclusion of symptoms as part of the inclusion criteria compared with symptom levels not defined.
Sensitivity analysis
We conducted sensitivity analysis for loss to follow‐up using best‐case and worst‐case analyses of the primary binary outcome ‐ improvement. For the best‐case analysis, we considered all participants lost to follow‐up to have improved, and for the worst‐case analysis, we considered participants lost to follow‐up to be not improved. Studies that did not report loss to follow‐up could not be included in this analysis.
We also carried out sensitivity analyses based on whether studies were rated as having low, unclear or high risk of selection, performance, detection and attrition bias. In addition, we assessed whether including data from cluster‐randomised trials had an effect on the analysis.
Therefore, sensitivity analyses were performed as follows.
Best‐case versus worst‐case analysis.
Selection bias: low versus unclear versus high risk.
Performance bias: low versus unclear versus high risk.
Detection bias: low versus unclear versus high risk.
Attrition bias: low versus unclear versus high risk.
Cluster versus individually randomised trials.
'Summary of findings' tables
We created 'Summary of findings' tables for primary outcomes, PTSD and symptoms for all psychological therapies compared with control, and for CBT compared with other psychological therapies in the short‐term. We used the five GRADE (Grades of Recommendation, Assessment, Development and Evaluation Working Group) considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of evidence for each outcome, and to draw conclusions about quality of evidence within the text of the review.
Results
Description of studies
Results of the search
From 172 study records, we identified 116 studies for review (see Figure 1 for Search flow diagram), included 51 studies (88 citations) with a total of 6201 participants (see Characteristics of included studies) and excluded 46 studies (59 records) (Characteristics of excluded studies). We have not yet assessed 14 studies, three because they require translation and the remainder because data were not available at the time of writing the review (Characteristics of studies awaiting classification); we also identified five ongoing studies (Characteristics of ongoing studies).
1.
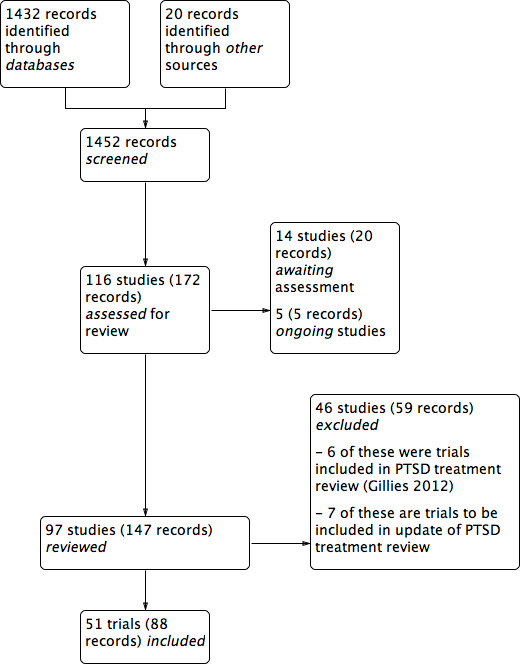
PRISMA study flow diagram.
Included studies
See Characteristics of included studies.
Ten included studies were cluster‐randomised controlled trials. Berger 2009, Berger 2012, Berliner 1996, Qouta 2012 and Shechtman 2010 randomised classes; Tol 2008, Tol 2012 and Tol 2014 randomised schools; Barron 2013 randomised counsellors; and Overbeek 2013 randomised children and family therapists. All other included studies randomised participants to interventions.
Settings
Most (27) included trials were done in the United States (Baker 1985; Berkowitz 2011; Berliner 1996; Carbonell 1999; Carrion 2013; Celano 1996; Chapman 2001; Chemtob 2002; Cohen 1996; Cohen 2005; Cohen 2011; Danielson 2012; Deblinger 1996; Deblinger 2001; Deblinger 2011; Dominguez 2001; Glodich 2000; Kazak 2004; Lieberman 2005; Pace 2013; Raider 2008; Salloum 2008; Salloum 2012; Shirk 2014; Stein 2003; Taussig 2010); three in the the Democratic Republic of Congo (O'Callaghan 2013; O'Callaghan 2014; McMullen 2013); two each were carried out in Australia (Cox 2010; Kemp 2010),Israel (Berger 2012; Shechtman 2010), the Netherlands (Diehle 2014; Overbeek 2013), Palestine (Barron 2013; Qouta 2012), Sri Lanka (Berger 2009; Tol 2012) and the UK (Stallard 2006; Trowell 2002). One study each was done in Bosnia (Layne 2008), Burundi (Tol 2014), Canada (Farkas 2010), Indonesia (Tol 2008), Iran (Jaberghaderi 2004), Jordan (Damra 2014), Peru (Church 2012), Sierra Leone (Betancourt 2014) and Switzerland (Zehnder 2010).
Participants
Included studies consisted of 6201 participants, and the number in each trial ranged from 16 (Church 2012; Jaberghaderi 2004) to 482 (Qouta 2012).
Ages of participants ranged from two to 24 years. Twenty trials included children only (Berliner 1996; Carbonell 1999; Celano 1996; Chemtob 2002; Damra 2014; Deblinger 1996; Deblinger 2001; Deblinger 2011; Jaberghaderi 2004; Kemp 2010; Overbeek 2013; Qouta 2012; Salloum 2008; Salloum 2012; Schottelkorb 2012; Stein 2003; Taussig 2010; Tol 2008; Tol 2012; Tol 2014), and 18 trials included both children and adolescents (Barron 2013; Berger 2009; Berkowitz 2011; Carrion 2013; Chapman 2001; Church 2012; Cohen 2005; Cohen 2011; Cox 2010; Diehle 2014; Dominguez 2001; Kazak 2004; O'Callaghan 2013; O'Callaghan 2014; Shechtman 2010; Stallard 2006; Trowell 2002; Zehnder 2010). Nine trials included only adolescents (Baker 1985; Berger 2012; Danielson 2012; Farkas 2010; Glodich 2000; Layne 2008; Pace 2013; Raider 2008; Shirk 2014) and two preschool children only (Cohen 1996; Lieberman 2005). Betancourt 2014 included adolescents and young adults, but because the mean age of participants was 18 years, we included this study.
In 12 trials, the targeted trauma was sexual abuse (Baker 1985; Berliner 1996; Celano 1996; Cohen 1996; Cohen 2005; Danielson 2012; Deblinger 1996; Deblinger 2001; Deblinger 2011; Dominguez 2001; Jaberghaderi 2004; Trowell 2002). Participants were exposed to war or community violence in ten trials (Betancourt 2014; Glodich 2000; Layne 2008; O'Callaghan 2014; McMullen 2013; Qouta 2012; Stein 2003; Tol 2008; Tol 2012; Tol 2014); physical trauma (Berkowitz 2011; Chapman 2001; Cox 2010; Kemp 2010; Stallard 2006; Zehnder 2010) and natural disaster in six trials each (Barron 2013; Berger 2009; Berger 2012; Chemtob 2002; Salloum 2008; Salloum 2012); and interpersonal violence in three (Cohen 2011; Lieberman 2005; Overbeek 2013); and had suffered a life‐threatening illness (Kazak 2004), had been physically abused (Damra 2014) or were maltreated (Taussig 2010) in one trial each. Participants in the remaining trials were exposed to a range of traumas (Carbonell 1999; Carrion 2013; Church 2012; Diehle 2014; Farkas 2010; O'Callaghan 2013; Pace 2013; Raider 2008; Schottelkorb 2012; Shechtman 2010; Shirk 2014). Participants were frequently exposed to more than one type of trauma in most trials.
Fifteen studies included participants on the basis of some measure of post‐trauma symptoms or reported baseline symptoms. To be included, participants needed a score of at least 12 on the Post‐Traumatic Stress Disorder Index (PTSD‐I) in Chapman 2001, a score of at least 7 on the Weekly Behaviour Report in Cohen 1996, at least one post‐traumatic symptom in Berkowitz 2011, significant symptoms in Cohen 2005, at least five symptoms with one from each cluster in Cohen 2011 and Deblinger 2011, clinical symptoms of PTSD in Damra 2014, at least three symptoms including at least one re‐experiencing or avoidance symptom in Deblinger 1996 and full or partial PTSD (although 5/32 had no diagnosis of PTSD) in Diehle 2014, or they had to be one of 10 students with the highest Children's Revised Impact of Events Scale (CRIES) scores in each class in Barron 2013. Mean baseline Post‐Traumatic Stress Disorder Reaction Index (PTSD‐RI) item scores were 0.68 in the therapies group and 0.77 in the control group in Betancourt 2014, PTSD‐RI total scores ranged from 22.70 to 25.80 in Carrion 2013, and mean Impact of Events Scale (IES) score was 34.2 in Church 2012. A ‘chart diagnosis’ was recorded for 81% of participants in Berliner 1996, and 88% met self reported Diagnostic and Statistical Manual, Fourth Edition (DSM‐IV) criteria for PTSD in Chemtob 2002.
Interventions
Most included trials compared a psychological therapy versus control (i.e. wait list, treatment as usual or no treatment). The psychological therapy was categorised predominantly as CBT in 17 trials (Barron 2013; Berger 2009; Berger 2012; Betancourt 2014; Carrion 2013; Damra 2014; Deblinger 1996; Layne 2008; O'Callaghan 2013; McMullen 2013; Pace 2013; Qouta 2012; Shirk 2014; Stein 2003; Tol 2008; Tol 2012; Tol 2014); as family therapy in four trials (Danielson 2012; Kazak 2004; Lieberman 2005; Raider 2008); as debriefing (Chapman 2001; Stallard 2006; Zehnder 2010) and psychoeducation/skills training (Cox 2010; Glodich 2000; O'Callaghan 2014) in three trials each; as narrative therapy (Carbonell 1999; Salloum 2012), supportive therapy (Shechtman 2010; Taussig 2010) and EMDR (Farkas 2010; Kemp 2010) in two trials each; and as exposure (Church 2012) or CBT plus narrative therapy (O'Callaghan 2013) in one trial each. Although these trials were broadly categorised under these therapies, several psychotherapeutic elements were common to a range of therapies. In particular, psychoeducation and coping skills were common to most interventions.
Among trials that compared one form of therapy versus another, eight compared CBT with supportive therapy (Berkowitz 2011; Celano 1996; Cohen 1996; Cohen 2005; Cohen 2011; Deblinger 2001; Dominguez 2001; Overbeek 2013), two compared CBT with EMDR (Diehle 2014; Jaberghaderi 2004) and one compared CBT with psychodynamic therapy (Schottelkorb 2012). Berliner 1996 compared exposure plus supportive therapy with supportive therapy only, and Deblinger 2011 compared narrative therapy plus CBT with CBT alone.
Five trials compared different models of delivery for psychological therapies. Four trials compared individual delivery of a psychological therapy versus group delivery of the same therapy (Baker 1985; Chemtob 2002; Salloum 2008; Trowell 2002), and Deblinger 1996 compared CBT for children only versus CBT for both mothers and children.
Three trials used a single intervention session (Chapman 2001; Stallard 2006; Zehnder 2010), and the remaining trials used between four and 40 therapy sessions but most commonly 10 to 15 sessions of 45 minutes to two hours, usually on a weekly basis. Interventions were delivered in a group setting in 20 trials (Barron 2013; Berger 2009; Berger 2012; Berliner 1996; Betancourt 2014; Carbonell 1999; Deblinger 2001; Glodich 2000; Kazak 2004; Layne 2008; O'Callaghan 2013; O'Callaghan 2014; Overbeek 2013; Pace 2013; Qouta 2012; Shechtman 2010; Stein 2003; Tol 2008; Tol 2012; Tol 2014).
Eleven trials were based on individual sessions with children (Carrion 2013; Chapman 2001; Church 2012; Diehle 2014; Dominguez 2001; Farkas 2010; Jaberghaderi 2004; Kemp 2010; Schottelkorb 2012; Shirk 2014; Stallard 2006), eight used a combination of individual and group delivery modes (Baker 1985; Chemtob 2002; McMullen 2013; Raider 2008; Salloum 2008; Salloum 2012; Taussig 2010; Trowell 2002) and one used a Web‐based intervention (Cox 2010). All other therapies involved parents or caregivers. Most of these were individual sessions that included parents for at least part of the therapy (Berkowitz 2011; Celano 1996; Cohen 1996; Deblinger 2011; Lieberman 2005; Zehnder 2010) or run in parallel with child and parent (Cohen 2005; Damra 2014) or consisted of both joint and parallel sessions (Cohen 2011; Danielson 2012; Deblinger 1996). Overbeek 2013 ran parallel group sessions for children and parents, and Qouta 2012 ran groups that included both.
Outcomes
Children and adolescents were diagnosed with PTSD on the basis of the Anxiety Disorder Interview Schedule for DSM‐IV (ADIS‐P; Diehle 2014), the Clinician Administered PostTraumatic Stress Disorder Scale for Children (Stallard 2006), the Diagnostic Interview Schedule for Children (Farkas 2010), the Semi Structured Interview for Diagnostic Classification (Lieberman 2005) and the Kiddie Schedule for Affective Disorders and Schizophrenia for school‐aged children ‐ Epidemiologic version (K‐SADS‐E; Deblinger 1996). They were also considered to have PTSD if they had a score of 3 or higher on one item of the University of California, Los Angeles (UCLA) PTSD Index (Berger 2009; Berger 2012), a total score of 38 or higher on the UCLA PTSD Index (Salloum 2008; Salloum 2012) or a score of 17 or higher on the intrusion/avoidance subscales of the Children's Revised Impact of Events Scale (CRIES)‐13 (Barron 2013).
The most frequently used measure for PTSD symptoms was the UCLA PTSD Index (Berger 2009; Betancourt 2014; Carrion 2013; Chapman 2001; Cohen 2011; Danielson 2012; Kazak 2004; Layne 2008; McMullen 2013; O'Callaghan 2013; Salloum 2008; Salloum 2012; Schottelkorb 2012) or the earlier version, the Child Post‐Traumatic Stress Reaction Index (Kemp 2010; Shechtman 2010), followed by the Trauma Symptom Checklist for Children (Berkowitz 2011; Cohen 2005; Cox 2010; Farkas 2010; Overbeek 2013; Raider 2008; Taussig 2010) or the Trauma Symptom Checklist for Young Children (Overbeek 2013); the Impact of Events Scale ‐ Revised (Church 2012; Cox 2010; Glodich 2000; Kazak 2004) or the earlier Impact of Traumatic Events Scale (Dominguez 2001; Kemp 2010; Stallard 2006); the K‐SADS‐E (Deblinger 1996; Deblinger 2001) and the K‐SADS ‐ Present and Lifetime (PL) version (Deblinger 2011; Shirk 2014; Trowell 2002); and the Child PTSD Symptoms Scale (Stein 2003; Tol 2008; Tol 2012; Tol 2014). Trauma symptoms were also measured by the CRIES‐13 (Barron 2013; Celano 1996; Diehle 2014; Qouta 2012) or revised version (CRIES‐8; O'Callaghan 2013); the Clinician Administered PTSD Scale (CAPS‐CA; Diehle 2014; Zehnder 2010); the Child Report of Post‐Traumatic Symptoms and the Parent Report of Post‐Traumatic Symptoms (Jaberghaderi 2004; Schottelkorb 2012); the Kauai Recovery Index (Chemtob 2002); Post‐Traumatic Stress Symptoms in Children (PTSS‐C; Damra 2014); and the Semi Structured Interview for Diagnostic Classification 0 to 3 (Lieberman 2005).
For depression, most used the Children's Depression Inventory (Berliner 1996; Carrion 2013; Cohen 2005; Cohen 2011; Damra 2014; Danielson 2012; Deblinger 1996; Deblinger 2011; Dominguez 2001; Overbeek 2013; Stein 2003; Zehnder 2010), followed by the Depression Self Rating Scale (Barron 2013; Layne 2008; Qouta 2012; Stallard 2006; Tol 2008; Tol 2012; Tol 2014). Other trials used the Beck Depression Inventory (Berger 2009; Shirk 2014); the Birleson Depression Inventory (Stallard 2006); the Children’s Depression Scale (Kemp 2010); the Institute for Personality and Ability Testing Depression Scale (Baker 1985); the Mood and Feelings Questionnaire (Salloum 2008; Salloum 2012); Orvaschel's PTSD scale (Trowell 2002); the Trauma Symptom Checklist for Children‐A (TSCC‐A; Cox 2010; Farkas 2010); and the Quick Inventory of Depressive Symptomatology (Pace 2013). Depression was diagnosed by a score of 29 or higher on the Mood and Feelings Questionnaire in Salloum 2008 and Salloum 2012 or on the K‐SADS‐PL (Shirk 2014).
The scales most frequently used to measure anxiety were the Revised Children's Manifest Anxiety Scale (Berliner 1996; Carrion 2013; Kazak 2004; Shechtman 2010; Stallard 2006), the State‐Trait Anxiety Inventory for Children (Cohen 2005; Deblinger 1996; Kemp 2010); the Screen for Child Anxiety Related Emotional Disorders (SCARED; Berger 2012; Cohen 2011; Tol 2008; Tol 2012); and the Trauma Symptom Checklist for Children (Berkowitz 2011; Cox 2010; Farkas 2010). Anxiety was also measured with the Institute for Personality and Ability Testing Anxiety Scale (Baker 1985); the Revised Child Anxiety and Depression Scale (Diehle 2014); the Multidimensional Anxiety Scale for Children (Deblinger 2011); and the State‐Trait Anxiety Inventory (Pace 2013).
Most trials measured behaviour with the Child Behavior Checklist (Berliner 1996; Celano 1996; Cohen 1996; Cohen 2005; Deblinger 1996; Deblinger 2001; Deblinger 2011; Farkas 2010; Kemp 2010; Lieberman 2005; Overbeek 2013; Salloum 2012; Shirk 2014; Zehnder 2010). Other measures of behaviour included the Strengths and Difficulties Questionnaire (SDQ; Barron 2013; Diehle 2014; Stallard 2006; Tol 2012); the Behavioral Assessment System for Children (BASC‐2; Danielson 2012); the Children’s Aggression Scale for Parents (Tol 2008); internalising and externalising items from the Oxford Measure of Psychosocial Adjustment (Betancourt 2014); the Teacher’s Report Form (Overbeek 2013); the Teacher‐Child Rating Scale (Stein 2003); the Youth Self‐Report (Glodich 2000; Raider 2008); and the African Youth Psychosocial Assessment (McMullen 2013; O'Callaghan 2013; O'Callaghan 2014).
Psychosocial function was measured by the Children's Global Assessment Scale (Celano 1996); the Kiddie Global Assessment Scale (Trowell 2002); the Pediatric Symptom Checklist (Stein 2003); and the Word Health Organization (WHO) Disability Adjustment Scale (Betancourt 2014). Functional impairment was measured by the Child Diagnostic Interview Schedule in Berger 2012 and by a scale developed by study authors in Tol 2008, Tol 2012 and Tol 2014.
Quality of life was measured by the Life Satisfaction Survey in Taussig 2010.
Cost in Great Britain pounds was reported in Trowell 2002.
Most studies (42) reported outcomes recorded within the first month after treatment; 27 studies reported outcomes from one month up to a year, and eight reported data for a year or longer after completion of treatment.
Data that could not be added to the meta‐analysis
Data from six studies could not be used because loss to follow‐up was greater than 50% for at least one group. Data included post‐treatment function in Celano 1996, PTSD symptoms and behaviour at three and 12 months in Deblinger 1996, symptoms of PTSD and depression at four months in Layne 2008 and all post‐treatment outcomes in Carrion 2013. Other than behaviour post treatment in Cohen 1996, loss to follow‐up was greater than 50% in the supportive therapy group at six and 12 months in Cohen 1996 and for all intervals in Cohen 2005.
Data from three studies could not be used in meta‐analyses because the required data were not reported and could not be calculated or obtained from study authors. Sample numbers were not clear in Chemtob 2002, and outcomes were reported as the intercept and the slope of a growth curve in Dominguez 2001; no variance was given in Chapman 2001.
Data from two studies could not be used in meta‐analyses because they showed substantial evidence of skew. Standard deviations were greater than mean PTSD scores for all groups in Deblinger 2001 and greater than all PTSD subscores in Cox 2010.
Data from three studies (Church 2012; Damra 2014; McMullen 2013) are reported separately (Table 3; Table 4; Table 5) because the effect size in all studies was several times higher than the overall estimate and contributed from 45% to 90% heterogeneity if they were added to meta‐analyses.
1. Data from Church 2012.
| Outcome | Group | n | Mean | SD |
| PTSD symptoms One month |
Exposure therapy | 8 | 3.38 | 2.60 |
| Control | 8 | 31.38 | 3.84 | |
| Avoidance One month |
Exposure therapy | 8 | 2.88 | 2.62 |
| Control | 8 | 20.25 | 2.38 | |
| Intrusion One month |
Exposure therapy | 8 | 0.50 | 0.50 |
| Control | 8 | 11.13 | 2.93 |
2. Data from Damra 2014.
| Outcome | Group | n | Mean | SD |
| PTSD symptoms Post therapy |
TF‐CBT | 9 | 13.00 | 1.12 |
| Control | 9 | 24.20 | 1.54 | |
| PTSD symptoms 4 months |
TF‐CBT | 9 | 11.88 | 1.96 |
| Control | 9 | 23.98 | 1.47 |
3. Data from McMullen 2013.
| Outcome | Group | n | Mean | SD |
| PTSD symptoms Post therapy |
TF‐CBT | 24 | 10.6 | 4.5 |
| Control | 24 | 34.8 | 11.6 | |
| Conduct Problems Post therapy |
TF‐CBT | 24 | 0.7 | 0.9 |
| Control | 24 | 7.1 | 7.0 |
Excluded studies
See Characteristics of excluded studies.
We excluded 46 studies, but six of these (Catani 2009; Cohen 2004; Ertl 2011; King 2000; Ruf 2010; Schauer 2008) were included in the Cochrane review on psychological therapies for treatment of PTSD in children and adolescents (Gillies 2012), and seven will be reviewed in the update (Chen 2014; Jacob 2014; Jensen 2014; Murray 2015; Rosner 2014; Ruf 2012; Soltanifar 2012).
We obtained full copies of the remaining 33 studies, as it was not clear from the available title or abstract whether they would meet the inclusion criteria. We excluded most because allocation was not randomised (Burke 1988; Ehntholt 2005; Gellman 2001; Goenjian 1997; Jeffres 2004; Kenardy 2008; Krueger 2013; Pfeffer 2002; Shooshtary 2008; Thabet 2005; Wang 2011; Wolmer 2011a; Wolmer 2011b) or study participants were not screened for exposure to trauma (Berger 2007; Bolton 2007; Cooley‐Strickland 2011; Gelkopf 2009; Hardin 2002; Jordans 2010; Rubin 2001; Wang 2011). Less than 50% of participants in the intervention group were randomised in Scheeringa 2011, the average age of participants was 19 years in Schaal 2009, no comparison group was included in Goenjian 1997 and Shelby 1995, the intervention was not a psychological therapy in Kassam‐Adams 2011 and Phipps 2012 and was used with mothers only in Dybdahl 2001 and follow‐up was only 10% in Saxe 2012 and 25% in the control group in Pfeffer 2002. Data were not reported and could not be obtained for Ensink 2004 and McWhirter 2011, and no data for the control group could be obtained for Kataoka 2003. Lyshak‐Stelzer 2007 was an interim publication of a trial that had already reported very high loss to follow‐up.
Studies awaiting classification
Fourteen studies are awaiting assessment (see Characteristics of studies awaiting classification). We have not yet assessed three randomised controlled trials (RCTs) as translations of these findings are not yet available (Mahmoudi‐Gharaei 2006; Narimani 2013,Shen 2012). The remainder have not been assessed as data were not available at the time of writing this review.
In contrast to our included studies, which were mostly done in the United States, the studies awaiting assessment were conducted in African countries including Burundi (Crombach 2012), Northern Uganda (Elbert 2009); and South Africa (Elbert 2013), Australia (Ooi 2010), China (Shen 2012; Zang 2013), Iran (Mahmoudi‐Gharaei 2006; Narimani 2013), Sweden (Hultmann 2012), Switzerland (Kramer 2014), and the UK (Jessiman 2013), with three in the United States (Kassam‐Adams 2016; Rowe 2013; Ruggiero 2015).
Participants had been affected by natural disasters (Mahmoudi‐Gharaei 2006; Rowe 2013; Shen 2012; Zang 2013); by war (Elbert 2009; Ooi 2010); by interpersonal abuse (Jessiman 2013; Hultmann 2012); by physical illness or injury (Kramer 2014;Ruggiero 2015;Kassam‐Adams 2016); unspecified traumatic events (Elbert 2009; Narimani 2013); or were violent offenders who had been exposed to traumatic stress (Elbert 2013).
Controls were compared to CBT (Hultmann 2012; Ooi 2010; Mahmoudi‐Gharaei 2006; Narimani 2013); guided narrative technique (Crombach 2012; Elbert 2009; Elbert 2013; Zang 2013); 'Letting the Future in' for children affected by sexual abuse (Jessiman 2013); a debriefing, psychoeducation and coping intervention (Kramer 2014); and expressive group counselling (Shen 2012). Controls were also compared to two web‐based interventions, ‘Coping Coach’ (Kassam‐Adams 2016) and ‘Bounce Back’ (Ruggiero 2015). The other studies compared different psychological therapies: Elbert 2013 compared FORNET, a narrative exposure therapy, to CBT; and Rowe 2013 compared group‐based CBT to family therapy. Mahmoudi‐Gharaei 2006 compared CBT to CBT plus art and sport interventions, and an art and sport intervention alone.
Ongoing studies
We identified five ongoing RCTs (see Characteristics of ongoing studies). These are being conducted in Kenya or Tanzania (Dorsey 2012), Australia (Sansom‐Daly 2012), the Netherlands (Roos 2013) and the United States (Belcher 2009; Toth 2011).
Participants had one or both parents die (Dorsey 2012); were exposed to neglect (Belcher 2009) or maltreatment (Toth 2011); had recently completed cancer treatment (Sansom‐Daly 2012); or had been exposed to a single traumatic event (Roos 2013).
Interventions compared with controls in ongoing trials include trauma‐focused CBT (Dorsey 2012) and family‐based therapy (Belcher 2009). Three ongoing trials are comparing different psychological therapies: 'Recapture Life’, an online group‐based CBT, is being compared with online supportive therapy (Sansom‐Daly 2012); EMDR to cognitive‐behavioural writing therapy (Roos 2013); and interpersonal therapy to enhanced care (Toth 2011).
Risk of bias in included studies
For graphical representations of the overall risk of bias in included trials, see Figure 2 and Figure 3.
2.
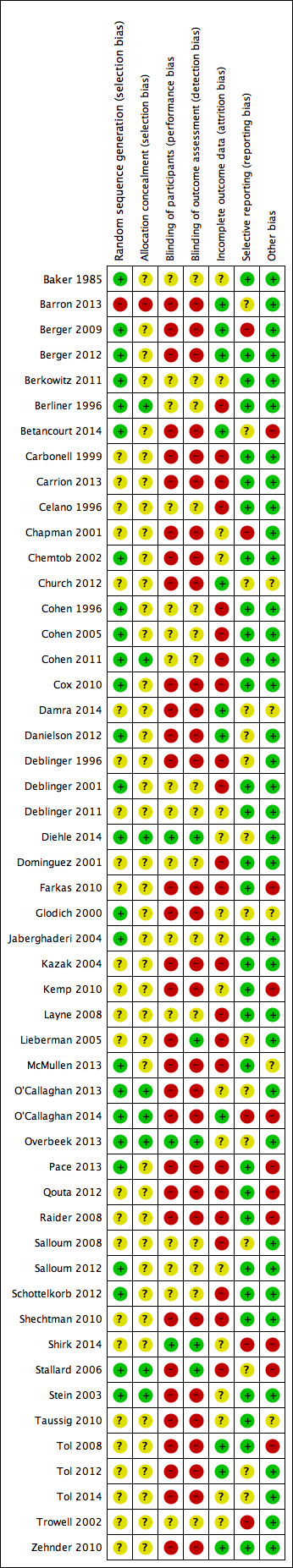
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Barron 2013 was considered to have high risk of selection bias because even though counsellors were randomised, they then identified participant classes. The generation of a randomisation sequence was described and was considered to lead to low risk of bias in 25 trials (Baker 1985; Berger 2009; Berger 2012; Berkowitz 2011; Berliner 1996; Betancourt 2014; Chemtob 2002; Cohen 1996; Cohen 2005; Cohen 2011; Cox 2010; Danielson 2012; Deblinger 2001; Diehle 2014; Glodich 2000; Jaberghaderi 2004; McMullen 2013; O'Callaghan 2013; O'Callaghan 2014; Overbeek 2013; Pace 2013; Salloum 2012; Schottelkorb 2012; Stallard 2006; Stein 2003) and to unclear risk in the remainder.
Barron 2013 was also considered at high risk because of allocation concealment based on selection of participant classes. Eight included trials (Berliner 1996; Cohen 2011; Diehle 2014; O'Callaghan 2013; O'Callaghan 2014; Overbeek 2013; Stallard 2006; Stein 2003) were considered to have low risk. Allocation concealment was not described in the remaining 42 trials, which therefore were rated as having unclear risk.
Blinding
Participants were likely to be aware of whether they had been assigned to an intervention group or a control group in 32 trials (Barron 2013; Berger 2009; Berger 2012; Betancourt 2014; Carbonell 1999; Carrion 2013; Chapman 2001; Chemtob 2002; Church 2012; Cox 2010; Damra 2014; Danielson 2012; Deblinger 1996; Farkas 2010; Glodich 2000; Kazak 2004; Kemp 2010; Lieberman 2005; McMullen 2013; O'Callaghan 2013; O'Callaghan 2014; Pace 2013; Qouta 2012; Raider 2008; Shechtman 2010; Stallard 2006; Stein 2003; Taussig 2010; Tol 2008; Tol 2012; Tol 2014; Zehnder 2010); therefore, these were rated as having high risk of performance bias. Participants in both groups received therapy in Diehle 2014, Overbeek 2013 and Shirk 2014, and these studies were rated as having low risk. All other trials were rated as having unclear risk of performance bias.
Primary outcomes were self reported in most studies (30) in which participants were probably aware of whether they received an intervention; these studies were rated as having high risk of detection bias (Barron 2013; Berger 2009; Berger 2012; Betancourt 2014; Carbonell 1999; Carrion 2013; Chapman 2001; Chemtob 2002; Church 2012; Cox 2010; Damra 2014; Danielson 2012; Deblinger 1996; Farkas 2010; Glodich 2000; Kazak 2004; Kemp 2010; McMullen 2013; O'Callaghan 2013; O'Callaghan 2014; Pace 2013; Qouta 2012; Raider 2008; Shechtman 2010; Stein 2003; Taussig 2010; Tol 2008; Tol 2012; Tol 2014; Zehnder 2010). Trials were rated as having low risk of bias when blinded assessment of primary outcomes was described (Lieberman 2005; Shirk 2014; Stallard 2006), and when studies that used self reported primary measures provided therapy to both groups (Diehle 2014; Overbeek 2013). Risk was rated as unclear in the remaining 15 studies.
Incomplete outcome data
Risk of attrition bias was low in 10 studies. Berger 2009, Berger 2012, Church 2012 and Damra 2014 reported no apparent loss to follow‐up, and loss to follow‐up was less than 5% in Tol 2012 and Zehnder 2010. Loss to follow‐up in Betancourt 2014, Danielson 2012, O'Callaghan 2014 and Tol 2008 was between 5% and 15%, but imputed values were used to account for missing data.
Other trials that reported completer data were rated as having unclear risk of bias if loss to follow‐up was between 5% and 15% (Barron 2013; Glodich 2000; Jaberghaderi 2004; Kemp 2010; O'Callaghan 2013; Salloum 2012; Stein 2003; Taussig 2010). If loss to follow‐up was between 15% and 25% but imputed values were used to account for missing data, the risk was considered unclear (Berkowitz 2011; Cohen 2005; Cohen 2011; Cox 2010; Deblinger 2011; Diehle 2014; Overbeek 2013; Shirk 2014; Trowell 2002). In addition, if loss to follow‐up was not reported (Baker 1985; Chapman 2001; Chemtob 2002; Tol 2014), studies were rated as having unclear risk.
We considered 18 trials to have high risk of attrition bias because incomplete outcome data were reported and attrition rates were greater than 15% (i.e. Berliner 1996; Carbonell 1999; Celano 1996; Cohen 1996; Deblinger 1996; Deblinger 2001; Dominguez 2001; Farkas 2010; Layne 2008; Lieberman 2005; McMullen 2013; Pace 2013; Qouta 2012; Raider 2008; Salloum 2008; Schottelkorb 2012; Shechtman 2010; Stallard 2006). We also rated Kazak 2004 as having high risk of attrition bias even though imputed results were reported, because loss to follow‐up was differentially higher in the intervention group than in the control group (38% versus 7%). Studies that used imputed data but reported loss to follow‐up greater than 30% were also considered to have high risk of bias (Berliner 1996; Cohen 2005; Cohen 2011; Cox 2010; Diehle 2014; Farkas 2010).
Selective reporting
The primary outcome of PTSD symptoms were not reported in four trials (Berger 2009; Chapman 2001; Diehle 2014; Shirk 2014), which therefore were rated as having high risk of reporting bias. Studies that did not report secondary outcomes such as Trowell 2002, which did not report depression, anxiety and hyperarousal; Stallard 2006 did not report parent SDQ scores; and O'Callaghan 2014, which did not report function, were rated as having unclear risk of bias. It was not clear whether all outcomes were reported in Barron 2013, Church 2012, Damra 2014, Danielson 2012, Deblinger 1996, Glodich 2000, Lieberman 2005, O'Callaghan 2013, Overbeek 2013, Salloum 2008, Tol 2012 and Tol 2014, which therefore were rated as having unclear risk of bias. All other trials appeared to report all outcomes and were rated as having low risk of reporting bias.
Other potential sources of bias
We rated eight studies as having high risk of other bias because they reported a baseline imbalance in the primary outcome of a PTSD diagnosis, post‐trauma symptoms or exposure to trauma. The baseline diagnosis of PTSD in the usual care group was twice as high as in the intervention group (61% versus 30%) in Shirk 2014, and was 53% higher in Stallard 2006 (35.5% versus 23.2%). Baseline symptom scores were significantly higher in the wait list group in Kemp 2010 (34.6 versus 22.3) and 10% higher in Betancourt 2014. Wait list participants in Tol 2008 were twice as likely to be displaced (75%) compared with those in the intervention group (37%). More participants in the intervention group had a baseline diagnosis of PTSD in Farkas 2010 (37% versus 19%) and clinically significant symptoms in Qouta 2012 (64% versus 43%). Baseline PTSD symptoms were also higher in the treatment group in both Farkas 2010 (6.4 versus 3.7) and Qouta 2012 (32.8 versus 27.8). Participants who had undergone sexual abuse accounted for 19% of those in the intervention group compared with only 4% in the wait list group in Pace 2013, and neglect was 52.0% in the wait list group and 29.6% in the intervention group.
We considered three studies to have unclear risk of other potential bias because they were less likely to have a direct effect on primary outcomes. Participants in the intervention group in Taussig 2010 were more likely to have undergone physical abuse and maternal neglect and to have a mother with a criminal history, although their scores for IQ, coping and social support were higher. Baseline conduct scores were approximately 17% higher in the intervention group in O'Callaghan 2014. In Shirk 2014, therapists in the intervention group had a total of 38 years of clinical experience compared with seven years among those in the usual care group, and intervention therapists received 'more targeted and frequent' case supervision. Raider 2008 referred to five participants who dropped out in the early sessions of group therapy but did not appear to be included among the 23 randomised participants. In Glodich 2000, data from a student who joined the treatment group after randomisation were included. Church 2012 and Damra 2014 were also considered to have unclear risk of additional bias because potential differences between groups were not investigated.
We considered all other trials to have low risk because no other bias was apparent.
Effects of interventions
Outcomes collected over these trials included diagnosis of PTSD, PTSD symptoms (total scores and subscores for arousal, avoidance and intrusion), anxiety (total, state and trait), depression, behaviour (total, internalising and externalising), function, quality of life, cost and loss to follow‐up.
Comparison 1. All psychological therapies versus controls
Primary outcomes
1. Diagnosis of PTSD
Across all trials that compared a psychological therapy versus a control, a significantly smaller proportion of children and adolescents who received therapy interventions had been diagnosed with PTSD at the end of the study in the short term (odds ratio (OR) 0.51, 95% confidence interval (CI) 0.34 to 0.77; 874 participants; five studies; I2 = 22%; number needed to treat for an additional beneficial outcome (NNTB) 9, 95% CI 6 to 20; Analysis 1.1), but not in the medium (OR 0.66, 95% CI 0.26 to 1.69; 742 participants; four studies; I2 = 70%; Analysis 2.1) or long term (OR 0.56, 95% CI 0.09 to 3.62; 64 participants; one study; Analysis 3.1).
1.1. Analysis.
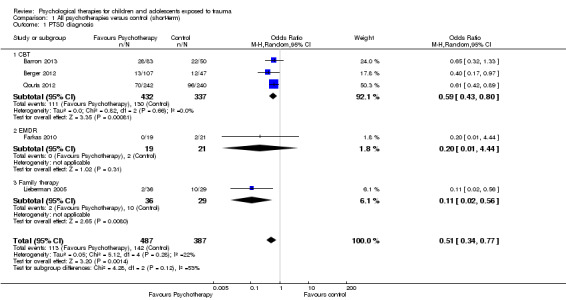
Comparison 1 All psychotherapies versus control (short‐term), Outcome 1 PTSD diagnosis.
2.1. Analysis.
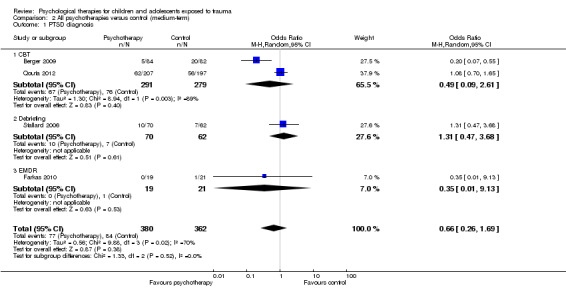
Comparison 2 All psychotherapies versus control (medium‐term), Outcome 1 PTSD diagnosis.
3.1. Analysis.

Comparison 3 All psychotherapies versus control (long‐term), Outcome 1 PTSD diagnosis.
2. PTSD symptoms
Scores for PTSD symptoms were significantly lower in the psychological therapy group in the short term (standardised mean difference (SMD) ‐0.42, 95% CI ‐0.61 to ‐0.24; 2051 participants; 17 studies; high heterogeneity at I2 = 71%; Analysis 1.2) than in the medium (SMD ‐0.17, 95% CI ‐0.38 to 0.05; 2337 participants; 13 studies; I2 = 83%; Analysis 2.2) or long term (SMD 0.17, 95% CI ‐0.28 to 0.62; 141 participants; two studies; I2 = 44%; Analysis 3.2). Church 2012 and Damra 2014 also reported significant improvement in overall trauma symptoms, but because these differences were approximately 20 times greater than in the other included studies, data were included in the meta‐analysis but did not contribute to the overall estimate.
1.2. Analysis.
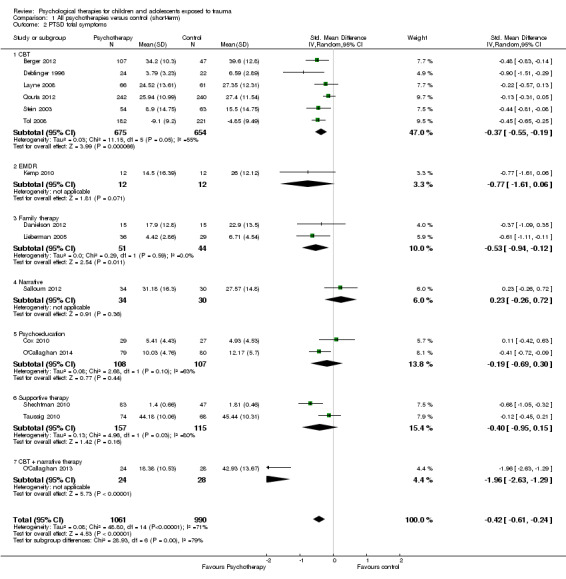
Comparison 1 All psychotherapies versus control (short‐term), Outcome 2 PTSD total symptoms.
2.2. Analysis.
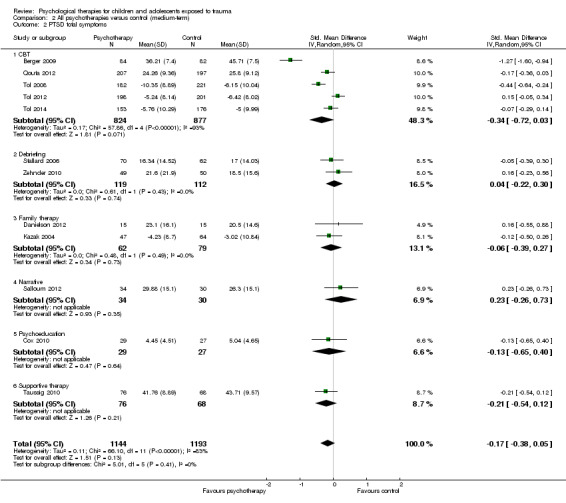
Comparison 2 All psychotherapies versus control (medium‐term), Outcome 2 PTSD total symptoms.
3.2. Analysis.

Comparison 3 All psychotherapies versus control (long‐term), Outcome 2 PTSD total symptoms.
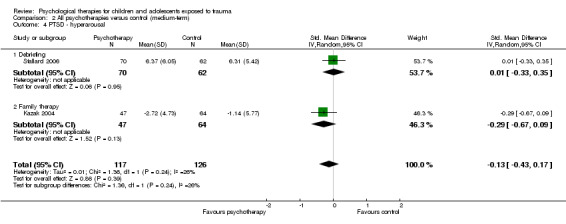
Investigators reported no differences between psychological therapy and control for any of the PTSD domains of avoidance, hyperarousal and intrusion in the short (Analysis 1.3; Analysis 1.4; Analysis 1.5) or medium term (Analysis 2.3; Analysis 2.4; Analysis 2.5). Long‐term PTSD domain data were not reported.
1.3. Analysis.
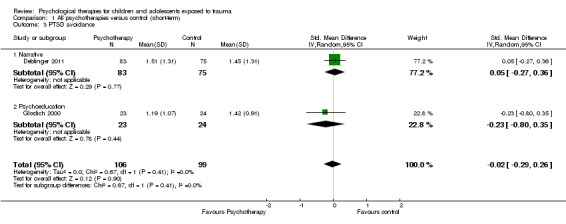
Comparison 1 All psychotherapies versus control (short‐term), Outcome 3 PTSD avoidance.
1.4. Analysis.

Comparison 1 All psychotherapies versus control (short‐term), Outcome 4 PTSD hyperarousal.
1.5. Analysis.
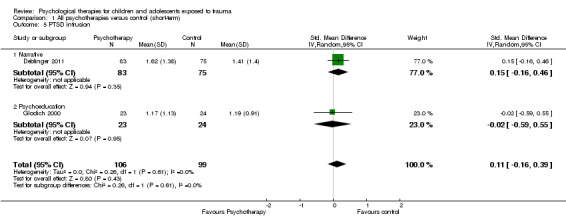
Comparison 1 All psychotherapies versus control (short‐term), Outcome 5 PTSD intrusion.
2.3. Analysis.

Comparison 2 All psychotherapies versus control (medium‐term), Outcome 3 PTSD ‐ avoidance.
2.4. Analysis.
Comparison 2 All psychotherapies versus control (medium‐term), Outcome 4 PTSD ‐ hyperarousal.
2.5. Analysis.

Comparison 2 All psychotherapies versus control (medium‐term), Outcome 5 PTSD ‐ intrusion.
Secondary outcomes
3. Anxiety
Scores for anxiety symptoms were not significantly different in the psychological therapy groups compared with the control groups in the short term (SMD ‐0.13, 95% CI ‐0.26 to 0.00; 959 participants; seven studies; I2 = 3%; Analysis 1.6), medium term (SMD ‐0.10, 95% CI ‐0.20 to 0.00; 1470 participants; seven studies; I2 = 0%; Analysis 2.6) or long term (SMD ‐0.12, 95% CI ‐0.41 to 0.18; 176 participants; two studies; I2 = 0%; Analysis 3.3). State anxiety was significantly less in the therapy groups in the short (SMD ‐0.64, 95% CI ‐1.12 to ‐0.16; 70 participants; two studies; I2 = 0%; Analysis 1.7) and medium term (SMD ‐0.71, 95% CI ‐1.31 to ‐0.12; 46 participants; one study; Analysis 2.7). Trait anxiety was not different in the short term (Analysis 1.8) but was significantly less in the medium term (SMD ‐0.45, 95% CI ‐0.85 to ‐0.05; 101 participants; two studies; I2 = 0%; Analysis 2.8). State anxiety and trait anxiety were not reported in the long term.
1.6. Analysis.
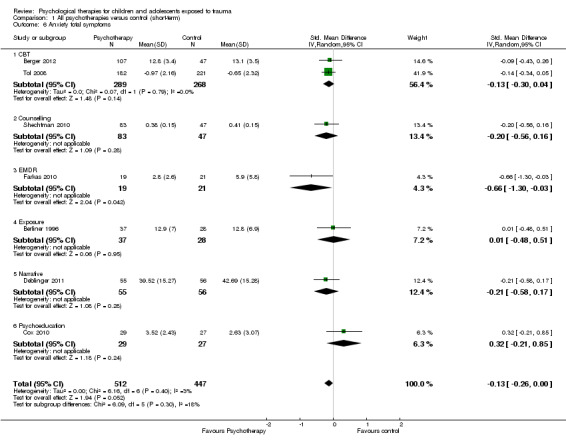
Comparison 1 All psychotherapies versus control (short‐term), Outcome 6 Anxiety total symptoms.
2.6. Analysis.
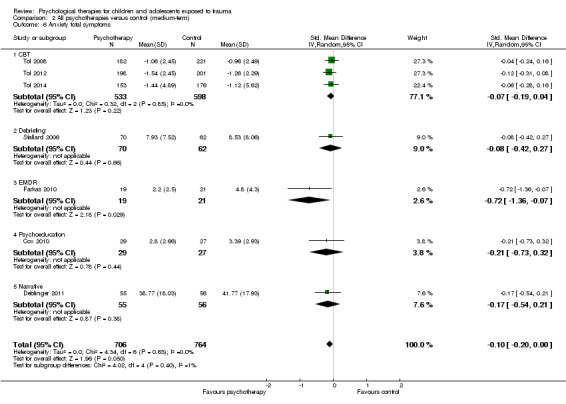
Comparison 2 All psychotherapies versus control (medium‐term), Outcome 6 Anxiety total symptoms.
3.3. Analysis.
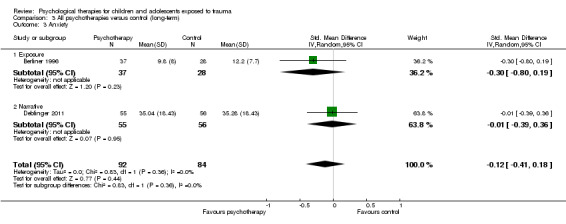
Comparison 3 All psychotherapies versus control (long‐term), Outcome 3 Anxiety.
1.7. Analysis.
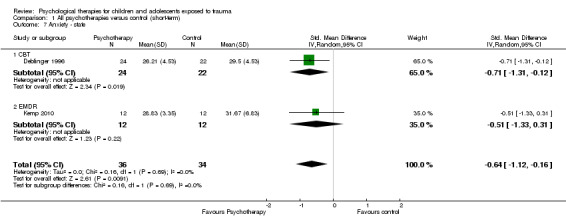
Comparison 1 All psychotherapies versus control (short‐term), Outcome 7 Anxiety ‐ state.
2.7. Analysis.
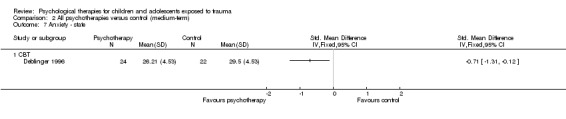
Comparison 2 All psychotherapies versus control (medium‐term), Outcome 7 Anxiety ‐ state.
1.8. Analysis.

Comparison 1 All psychotherapies versus control (short‐term), Outcome 8 Anxiety ‐ trait.
2.8. Analysis.

Comparison 2 All psychotherapies versus control (medium‐term), Outcome 8 Anxiety ‐ trait.
4. Depression
Scores for depression symptoms were not significantly lower in the psychological therapy group in the short term (SMD ‐0.13, 95% CI ‐0.30 to 0.04; 1569 participants; 13 studies; I2 = 52%; Analysis 1.9), medium term (SMD ‐0.07, 95% CI ‐0.22 to 0.07; 2191 participants; 13 studies; I2 = 55%; Analysis 2.9) or long term (SMD ‐0.12, 95% CI ‐0.41 to 0.18; 176 participants; two studies; I2 = 0%; Analysis 3.4).
1.9. Analysis.
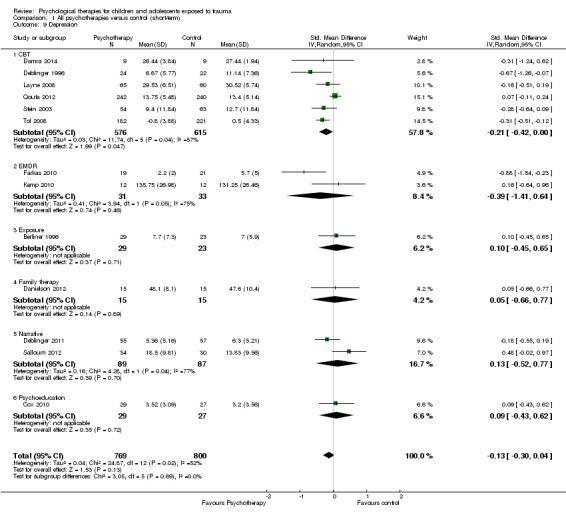
Comparison 1 All psychotherapies versus control (short‐term), Outcome 9 Depression.
2.9. Analysis.

Comparison 2 All psychotherapies versus control (medium‐term), Outcome 9 Depression.
3.4. Analysis.
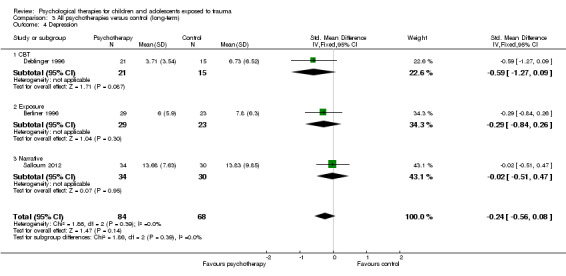
Comparison 3 All psychotherapies versus control (long‐term), Outcome 4 Depression.
5. Behaviour
Total behaviour scores were not significantly lower in the psychological therapy group in the short (SMD ‐0.04, 95% CI ‐0.51 to 0.42; 166 participants; three studies; I2 = 51%; Analysis 1.10), medium (SMD ‐0.20, 95% CI ‐0.43 to 0.04; 281 participants; three studies; I2 = 0%; Analysis 2.10) or long term (SMD 0.39, 95% CI ‐0.07 to 0.85; 77 participants; one study; Analysis 3.5).
1.10. Analysis.
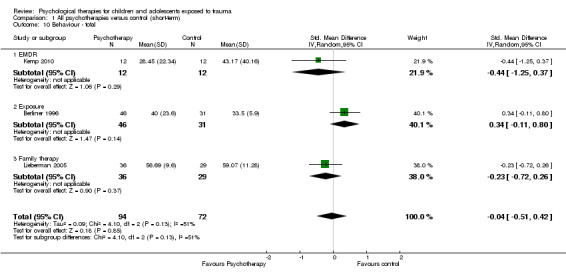
Comparison 1 All psychotherapies versus control (short‐term), Outcome 10 Behaviour ‐ total.
2.10. Analysis.
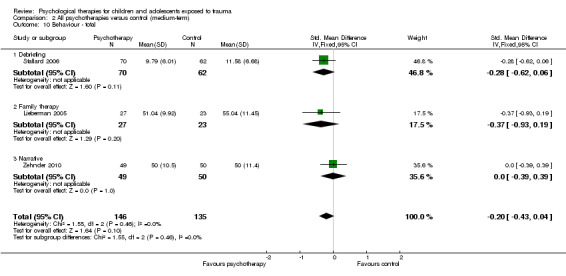
Comparison 2 All psychotherapies versus control (medium‐term), Outcome 10 Behaviour ‐ total.
3.5. Analysis.

Comparison 3 All psychotherapies versus control (long‐term), Outcome 5 Behaviour ‐ total.
Scores for internalising behaviour were not different in the short (SMD ‐0.04, 95% CI ‐0.20 to 0.13; 719 participants; 10 studies; I2 = 16%; Analysis 1.11), medium (SMD 0.01, 95% CI ‐0.25 to 0.28; 291 participants; four studies; I2 = 16%; Analysis 2.11) or long term (SMD 0.04, 95% CI ‐0.51 to 0.59; 141 participants; two studies; I2 = 63%; Analysis 3.6). Researchers reported no differences between groups in externalising behaviour in the short (SMD ‐0.10, 95% CI ‐0.33 to 0.14; 1174 participants; 12 studies; I2 = 68%; Analysis 1.12), medium (SMD ‐0.11, 95% CI ‐0.38 to 0.17; 206 participants; two studies; I2 = 0%; Analysis 2.12) or long term (SMD 0.28, 95% CI ‐0.05 to 0.60; 298 participants; three studies; I2 = 46%; Analysis 3.7).
1.11. Analysis.
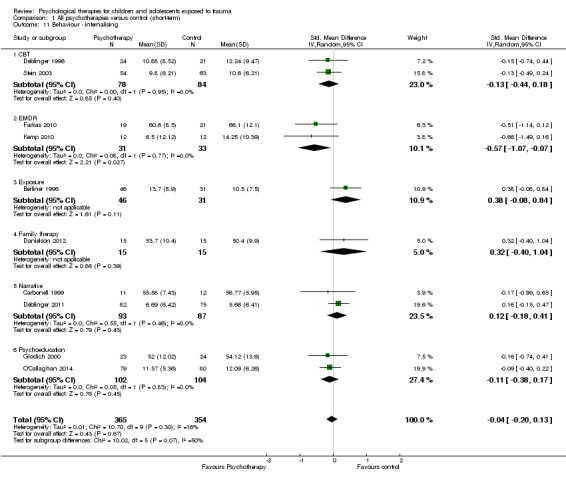
Comparison 1 All psychotherapies versus control (short‐term), Outcome 11 Behaviour ‐ internalising.
2.11. Analysis.

Comparison 2 All psychotherapies versus control (medium‐term), Outcome 11 Behaviour ‐ internalising.
3.6. Analysis.

Comparison 3 All psychotherapies versus control (long‐term), Outcome 6 Behaviour ‐ internalising.
1.12. Analysis.
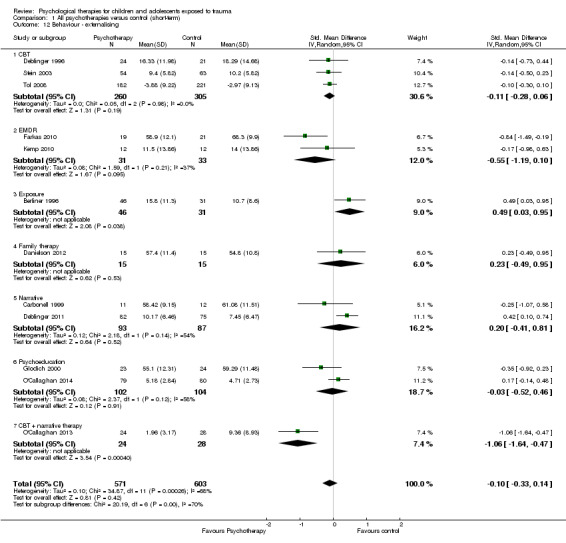
Comparison 1 All psychotherapies versus control (short‐term), Outcome 12 Behaviour ‐ externalising.
2.12. Analysis.
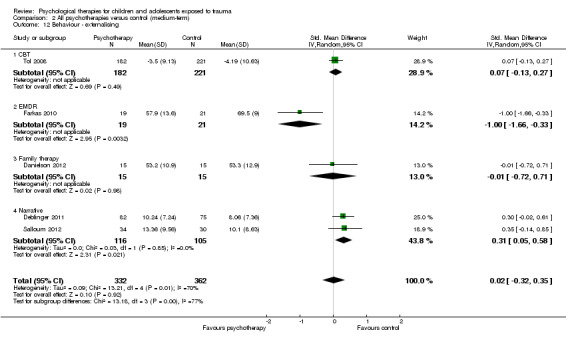
Comparison 2 All psychotherapies versus control (medium‐term), Outcome 12 Behaviour ‐ externalising.
3.7. Analysis.
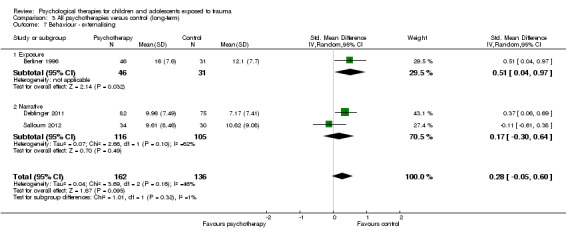
Comparison 3 All psychotherapies versus control (long‐term), Outcome 7 Behaviour ‐ externalising.
6. Functional impairment
Function was significantly improved in the group receiving psychological therapy in the short (SMD ‐0.41, 95% CI ‐0.59 to ‐0.24; 557 participants; two studies; I2 = 0%; Analysis 1.13) and medium term (SMD ‐0.46, 95% CI ‐0.88 to ‐0.05; three studies; I2 = 88%; Analysis 2.13). No study reported long‐term function scores.
1.13. Analysis.
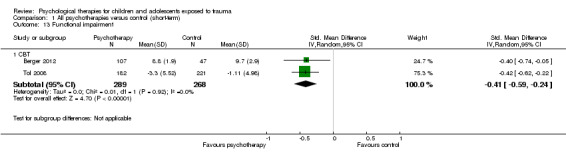
Comparison 1 All psychotherapies versus control (short‐term), Outcome 13 Functional impairment.
2.13. Analysis.
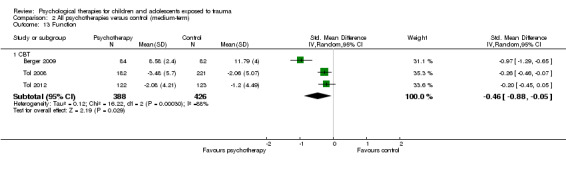
Comparison 2 All psychotherapies versus control (medium‐term), Outcome 13 Function.
7. Quality of life
Investigators reported no differences between groups in quality of life measures in the short (SMD 0.03, 95% CI ‐0.30 to 0.36; 144 participants; one study; Analysis 1.14) and medium term (SMD 0.13, 95% CI ‐0.19 to 0.46; 144 participants; one study; Analysis 2.14). Long‐term quality of life was not reported.
1.14. Analysis.

Comparison 1 All psychotherapies versus control (short‐term), Outcome 14 Quality of life.
2.14. Analysis.
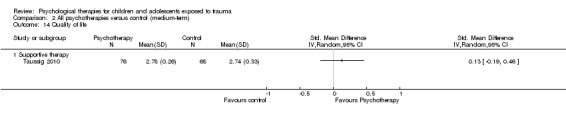
Comparison 2 All psychotherapies versus control (medium‐term), Outcome 14 Quality of life.
8. Adverse events
Researchers provided no adverse events data.
9. Cost
Researchers provided no cost data.
10. Loss to follow‐up
Among all trials that compared a psychological therapy versus a control, investigators reported no differences in the proportions of children and adolescents lost to follow‐up in the short term (risk ratio (RR) 0.98, 95% CI 0.69 to 1.39; 3872 participants; 26 studies; I2 = 59%; Analysis 1.15), medium term (OR 1.00, 95% CI 0.82 to 1.21; 3663 participants; 20 studies; I2 = 71%; Analysis 2.15) or long term (SMD 0.28, 95% CI ‐0.05 to 0.60; 298 participants; three studies; I2 = 46%; Analysis 3.7).
1.15. Analysis.
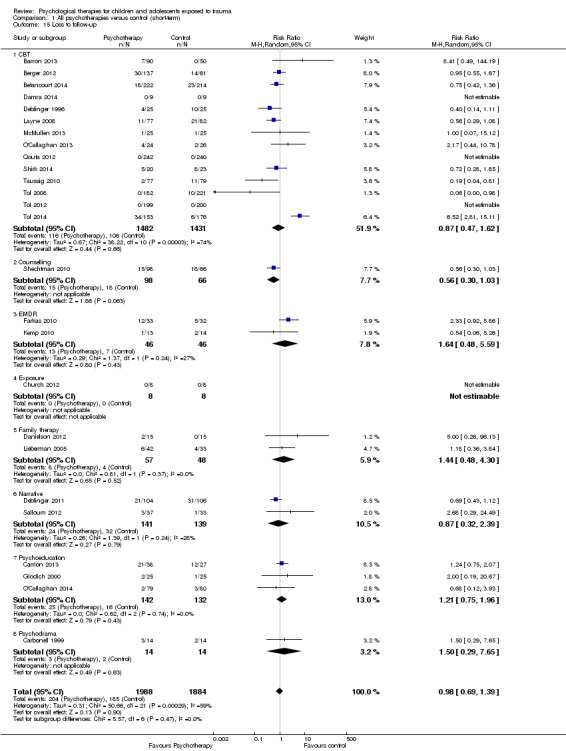
Comparison 1 All psychotherapies versus control (short‐term), Outcome 15 Loss to follow‐up.
2.15. Analysis.

Comparison 2 All psychotherapies versus control (medium‐term), Outcome 15 Loss to follow‐up.
Subgroup analyses of psychological therapies
Primary outcomes
Diagnosis of PTSD
We noted no significant differences between the therapy subgroups of CBT, EMDR and family therapy in PTSD diagnosis in the short (Analysis 1.1), medium (Analysis 2.1) or long term (Analysis 3.1).
PTSD symptoms
In the short term, we observed significant differences between therapy subgroups in effects on symptoms of PTSD (P value < 0.0001; Analysis 1.2). With CBT (SMD ‐0.37, 95% CI ‐0.55 to ‐0.19; 1329 participants; seven studies; I2 = 55%), family therapy (SMD ‐0.53, 95% CI ‐0.94 to ‐0.12; 95 participants; two studies; I2 = 0%) and CBT plus narrative therapy (SMD ‐1.96, 95% CI ‐2.63 to ‐1.29; 52 participants; one study), all symptom scores were improved compared with control, and we noted no differences in scores when EMDR, psychoeducation and narrative, supportive and exposure therapies were compared with controls. We found no differences between therapy subgroups in the medium term (Analysis 2.2) and observed that none of the therapies (CBT, debriefing, family therapy, narrative therapy, psychoeducation and supportive therapy) were significantly different from controls. We observed no differences between the two single trials that compared exposure therapy versus control and narrative therapy versus control in the long term (Analysis 2.3), and no subgroup differences for any of the PTSD domains of avoidance (Analysis 1.3; Analysis 2.3), hyperarousal (Analysis 1.4; Analysis 2.4) and intrusion (Analysis 1.5; Analysis 2.5) in the short or medium term; we found no long‐term data.
Secondary outcomes
Anxiety
We found no significant differences between therapy groups when comparing anxiety scores with those of a control group in the short (Analysis 1.6), medium (Analysis 2.6) or long term (Analysis 3.3), nor did we note differences between therapy groups in state (Analysis 1.7; Analysis 2.7) or trait anxiety (Analysis 1.8; Analysis 2.8), which was reported in the short and medium term.
Depression
We found no significant differences between therapy subgroups for the outcome of depression in the short (Analysis 1.9), medium (Analysis 2.9) or long term (Analysis 3.4).
Behaviour
Although we noted no differences between therapy subgroups for total (Analysis 1.10; Analysis 2.10) or internalising behaviour (Analysis 1.11; Analysis 2.11; Analysis 3.6) scores, we observed a significant difference for externalising behaviour scores in the short term (P value = 0.004; Analysis 1.12). Externalising behaviours were significantly greater in the therapy groups in the single trials that compared exposure therapy versus control (SMD 0.49, 95% CI 0.03 to 0.95; 77 participants; Analysis 1.12) and fewer in the trial that compared CBT plus narrative therapy versus control (SMD ‐1.06, 95% CI ‐1.64 to ‐0.47; 52 participants; Analysis 1.12).
Function
Function was reported only in trials that compared CBT versus control in the short (Analysis 1.13) and medium term (Analysis 2.13).
Quality of life
Only one trial of supportive therapy compared with control reported quality of life in the short (Analysis 1.14) and medium term (Analysis 2.14).
Adverse events
No data were reported.
Cost
No data were reported.
Loss to follow‐up
We found no differences between therapy subgroups in loss to follow‐up in the short (Analysis 1.15), medium (Analysis 2.15) or long term (Analysis 3.8).
3.8. Analysis.

Comparison 3 All psychotherapies versus control (long‐term), Outcome 8 Loss to follow‐up.
Comparison 2. Psychological therapies versus other psychological therapies
We were able to compare CBT with other pooled therapies for the primary outcomes only. We report these results below; thereafter, we report the results subgrouped by comparator.
CBT versus other psychological therapies
Primary outcomes
1. Diagnosis of PTSD
CBT was found to be no more or less effective than EMDR and supportive therapy in reducing diagnosis of PTSD in the short term (OR 0.74, 95% CI 0.29 to 1.91; 2 studies, 160 participants; Analysis 4.1). The quality of the evidence was very low.
4.1. Analysis.

Comparison 4 CBT versus other therapies (short‐term), Outcome 1 PTSD diagnosis.
2. PTSD symptoms
For reduction of PTSD symptoms in the short term, there was a small effect favouring CBT over EMDR, play therapy and supportive therapies (SMD ‐0.24, 95% CI ‐0.42 to ‐0.05, 7 studies, 466 participants; Analysis 4.2). The quality of the evidence was moderate.
4.2. Analysis.
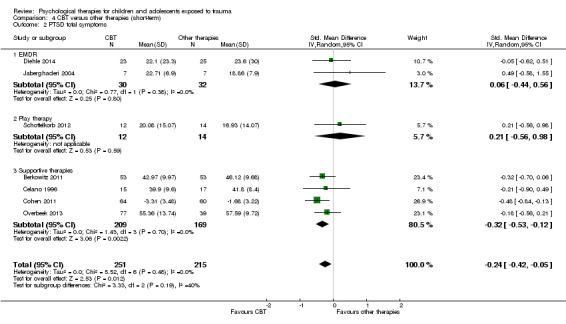
Comparison 4 CBT versus other therapies (short‐term), Outcome 2 PTSD total symptoms.
CBT versus EMDR
One study compared CBT versus EMDR, and all reported outcomes were short term.
Primary outcomes
1. Diagnosis of PTSD
No data were reported.
2. PTSD symptoms
Scores for PTSD symptoms were not significantly different when CBT was compared with EMDR (SMD 0.06, 95% CI ‐0.44 to 0.56; 62 participants; two studies; I2 = 0%; Analysis 4.2).
Secondary outcomes
3. Anxiety
No data were reported.
4. Depression
No data were reported.
5. Behaviour
Total behaviour scores were not significantly different between groups (SMD ‐0.44, 95% CI ‐1.50 to 0.63; 14 participants; one study; Analysis 4.8).
4.8. Analysis.

Comparison 4 CBT versus other therapies (short‐term), Outcome 8 Behaviour ‐ total.
6. Function
No data were reported.
7. Quality of life
No data were reported.
8. Adverse events
No data were reported.
9. Cost
No data were reported.
10. Loss to follow‐up
We observed no differences in loss to follow‐up at the end of the study (OR 0.76, 95% CI 0.23 to 2.52; 64 participants; two studies; I2 = 0%; Analysis 4.12).
4.12. Analysis.
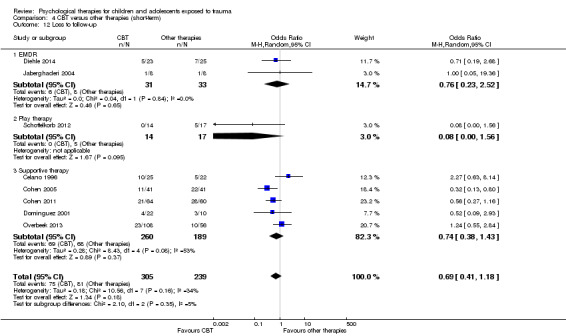
Comparison 4 CBT versus other therapies (short‐term), Outcome 12 Loss to follow‐up.
CBT versus psychodynamic therapy
The one study that compared CBT versus psychodynamic therapy reported only short‐term outcomes.
Primary outcomes
1. Diagnosis of PTSD
No data were reported.
2. PTSD symptoms
PTSD symptom scores were not significantly different between groups (SMD 0.21, 95% CI ‐0.56 to 0.98; 26 participants; Analysis 5.1).
5.1. Analysis.
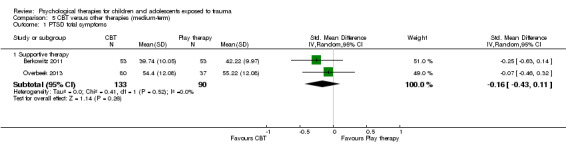
Comparison 5 CBT versus other therapies (medium‐term), Outcome 1 PTSD total symptoms.
Secondary outcomes
3. Anxiety
No data were reported.
4. Depression
No data were reported.
5. Behaviour
No data were reported.
6. Function
No data were reported.
7. Quality of life
No data were reported.
8. Adverse events
No data were reported.
9. Cost
No data were reported.
10. Loss to follow‐up
We noted no differences in the proportions of children and adolescents lost to follow‐up at the end of the study (OR 0.08, 95% CI 0.00 to 1.56; 31 participants; Analysis 4.12).
CBT versus supportive therapy
Four trials compared CBT versus supportive therapy.
Primary outcomes
1. Diagnosis of PTSD
We found no differences in the proportions of children and adolescents diagnosed with PTSD in the short term (OR 0.71, 95% CI 0.26 to 1.95; 124 participants; one study; Analysis 4.1) when CBT was compared with supportive therapy. The diagnosis of PTSD was not reported in the medium or long term.
2. PTSD symptoms
Scores for PTSD symptoms were significantly lower in the CBT group in the short term (SMD ‐0.32, 95% CI ‐0.53 to ‐0.12; 378 participants; four studies; I2 = 0%; Analysis 4.2) but not in the medium term (SMD ‐0.16, 95% CI ‐0.43 to 0.11; 223 participants; two studies; I2 = 0%; Analysis 5.1).
Short‐term scores for PTSD avoidance (SMD ‐0.40, 95% CI ‐0.76 to ‐0.05; 124 participants; Analysis 4.3) and hyperarousal (SMD ‐0.52, 95% CI ‐0.87 to ‐0.16; 124 participants; Analysis 4.4) were also significantly lower in the CBT group, although we found no differences in intrusion (Analysis 4.5).
4.3. Analysis.

Comparison 4 CBT versus other therapies (short‐term), Outcome 3 PTSD avoidance.
4.4. Analysis.
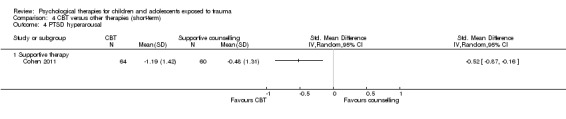
Comparison 4 CBT versus other therapies (short‐term), Outcome 4 PTSD hyperarousal.
4.5. Analysis.
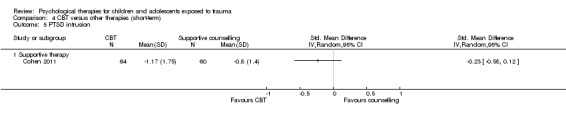
Comparison 4 CBT versus other therapies (short‐term), Outcome 5 PTSD intrusion.
Secondary outcomes
3. Anxiety
Anxiety symptoms were significantly lower in the CBT group in the short (SMD ‐0.48, 95% CI ‐0.74 to ‐0.22; 230 participants; two studies; I2 = 0%) but not the medium term (Analysis 4.6).
4.6. Analysis.
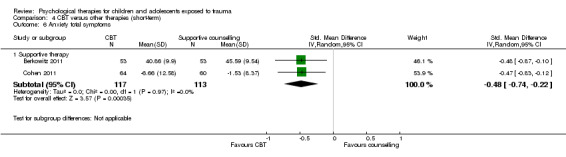
Comparison 4 CBT versus other therapies (short‐term), Outcome 6 Anxiety total symptoms.
4. Depression
We found no differences in depression symptoms in the short or medium term (Analysis 4.7).
4.7. Analysis.
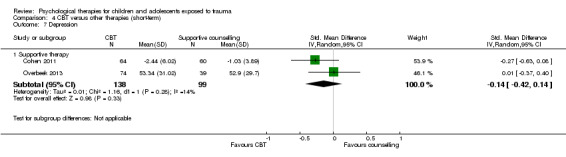
Comparison 4 CBT versus other therapies (short‐term), Outcome 7 Depression.
5. Behaviour
We noted no differences between CBT and supportive therapy groups in total behaviour scores (Analysis 4.8) nor in scores for internalising (Analysis 4.9) or externalising behaviour (Analysis 4.10) at any interval.
4.9. Analysis.
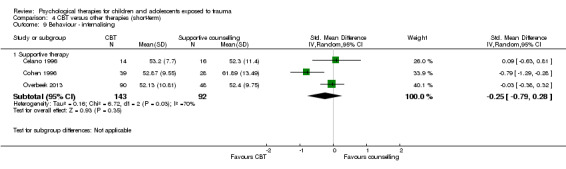
Comparison 4 CBT versus other therapies (short‐term), Outcome 9 Behaviour ‐ internalising.
4.10. Analysis.
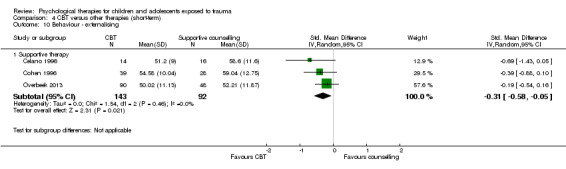
Comparison 4 CBT versus other therapies (short‐term), Outcome 10 Behaviour ‐ externalising.
6. Function
Function was reported by only one trial in the short term. We found no differences between groups (Analysis 4.11).
4.11. Analysis.
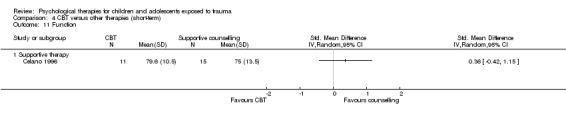
Comparison 4 CBT versus other therapies (short‐term), Outcome 11 Function.
7. Quality of life
No data were reported.
8. Adverse events
No data were reported.
9. Cost
No data were reported.
10. Loss to follow‐up
We noted no differences between trials that compared CBT versus supportive therapy in short‐, medium‐ or long‐term loss to follow‐up (Analysis 4.12).
Comparison 3. Psychological therapies versus pharmacological therapies
We identified no trials that compared psychological therapies versus pharmacological therapies.
Subgroup analyses
Group versus individual therapy
Three trials compared delivery of psychological therapies in group and individual modes.
No data were reported for diagnosis of PTSD.
Total PTSD symptom scores were not different when group therapy was compared with individual therapy (Analysis 7.1). These scores were reported in the short term only.
7.1. Analysis.
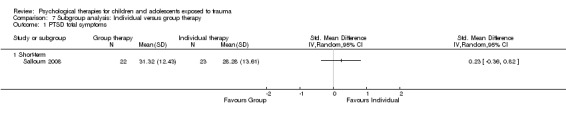
Comparison 7 Subgroup analysis: Individual versus group therapy, Outcome 1 PTSD total symptoms.
Child versus child and parent therapy
Deblinger 1996 reported data for CBT therapy for children only and data for CBT for children and mothers.
No data were reported for diagnosis of PTSD.
We did not find any difference in symptoms of PTSD when CBT for children was compared to CBT for children and mothers (Analysis 8.1).
8.1. Analysis.
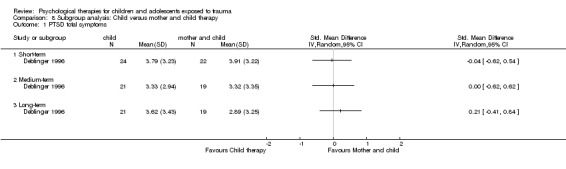
Comparison 8 Subgroup analysis: Child versus mother and child therapy, Outcome 1 PTSD total symptoms.
Type of trauma
We compared types of trauma including sexual abuse, maltreatment, physical trauma, life‐threatening illness, domestic violence, community violence and war and natural disaster in subgroup analyses.
Effects of psychological therapies on PTSD diagnosis were significantly different when participants exposed to different types of trauma were compared (P value = 0.007; Analysis 9.1). Intervention effects were significantly better compared with those of controls in children and adolescents exposed to community violence (OR 0.59, 95% CI 0.43 to 0.80; 769 participants; three studies; I2 = 0%), interpersonal violence (OR 0.11, 95% CI 0.02 to 0.56; 65 participants; one study) and natural disaster (OR 0.16, 95% CI 0.06 to 0.45; 166 participants; one study), but not in participants who had undergone physical trauma.
9.1. Analysis.
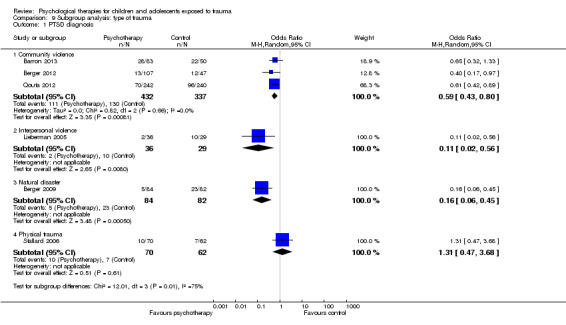
Comparison 9 Subgroup analysis: type of trauma, Outcome 1 PTSD diagnosis.
Effects on PTSD symptom scores were also significantly different between subgroups who had undergone different types of trauma (P value < 0.00001; Analysis 9.2). Scores were significantly improved for children and adolescents who had undergone sexual abuse (SMD ‐0.67, 95% CI ‐1.18 to ‐0.16; 76 participants; two studies; I2 = 16%) or were exposed to interpersonal violence (SMD ‐0.61, 95% CI ‐1.11 to ‐0.11; 65 participants; one study), natural disaster (SMD ‐1.27, 95% CI ‐1.60 to ‐0.94; 166 participants; one study) or community violence (SMD ‐0.24, 95% CI ‐0.41 to ‐0.06; 2170 participants; eight studies; I2 = 73%), although the latter subgroup was highly heterogeneous (I2 = 73%). We noted no differences between therapy and control groups among children and adolescents who had been maltreated or had undergone physical trauma or life‐threatening illness.
9.2. Analysis.

Comparison 9 Subgroup analysis: type of trauma, Outcome 2 PTSD total symptoms.
Types of control
We performed a subgroup analysis of active controls (e.g. treatment as usual, which included elements of psychological therapy, or psychological therapy as control, which is used in combination with another therapy in the intervention group) versus an inactive control (e.g. no treatment, wait list, craft group). We found no differences for diagnosis of PTSD (Analysis 11.1) or PTSD symptom scores (Analysis 11.2) when comparing active and inactive control subgroups.
Symptomatic inclusion criteria
We compared studies that included symptoms of PTSD or anxiety as well as exposure to trauma as the inclusion criteria versus studies in which symptoms were not part of the inclusion criteria. We found no significant differences between these subgroups for outcomes of PTSD diagnosis (Analysis 10.1) or symptoms (Analysis 10.2).
10.1. Analysis.
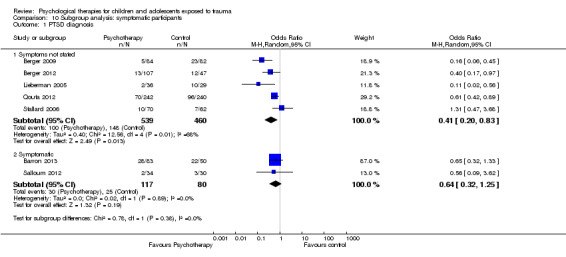
Comparison 10 Subgroup analysis: symptomatic participants, Outcome 1 PTSD diagnosis.
10.2. Analysis.
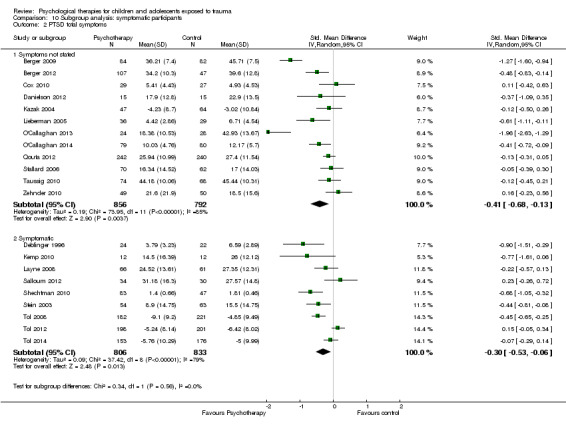
Comparison 10 Subgroup analysis: symptomatic participants, Outcome 2 PTSD total symptoms.
Sensitivity analyses
We performed all sensitivity analyses for the primary outcomes of a diagnosis of PTSD and symptoms of PTSD when a psychological therapy was compared with control.
Best‐case/Worst‐case analysis
We found no significant differences between best‐case and worst‐case analyses (Analysis 12.1).
12.1. Analysis.
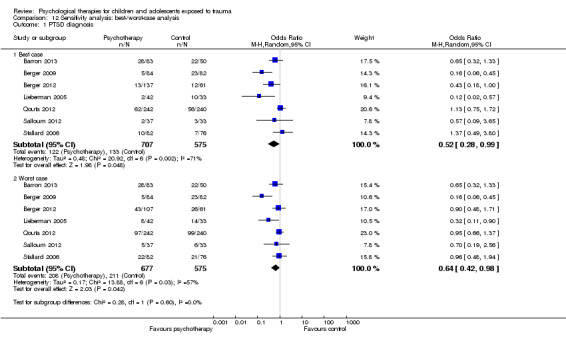
Comparison 12 Sensitivity analysis: best‐/worst‐case analysis, Outcome 1 PTSD diagnosis.
Selection bias
For the outcome of PTSD diagnosis, we found no significant differences between the four trials rated as having low risk of selection bias compared with the single trials rated as having unclear and high risk of bias (Analysis 17.1). We noted no differences between low and unclear risk trials for PTSD symptoms (Analysis 17.2). We rated no trials reporting PTSD symptoms as having high risk of selection bias.
17.1. Analysis.
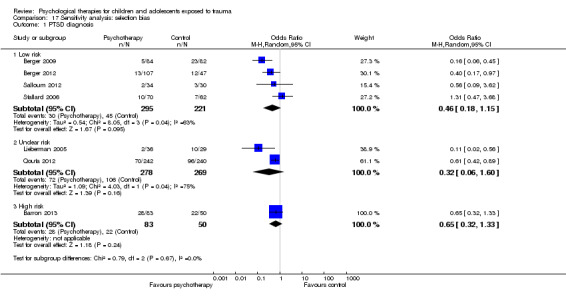
Comparison 17 Sensitivity analysis: selection bias, Outcome 1 PTSD diagnosis.
17.2. Analysis.
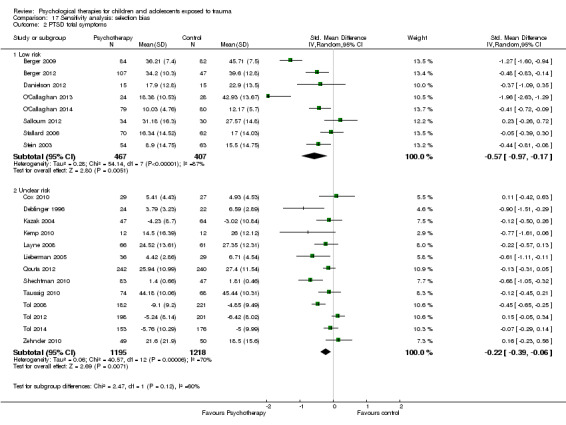
Comparison 17 Sensitivity analysis: selection bias, Outcome 2 PTSD total symptoms.
Performance bias
We found no significant differences in the diagnosis of PTSD when we compared the one trial rated as having unclear risk of performance bias versus the five trials rated as having high risk (Analysis 14.1). However, we noted significant differences between subgroups for symptoms of PTSD (one trial with unclear risk versus 17 trials with high risk; P value = 0.02; Analysis 14.2). We rated no trials as having low risk of performance bias.
14.1. Analysis.
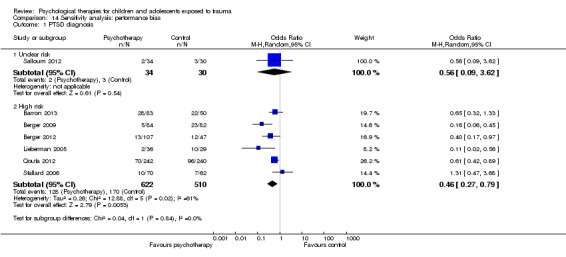
Comparison 14 Sensitivity analysis: performance bias, Outcome 1 PTSD diagnosis.
14.2. Analysis.
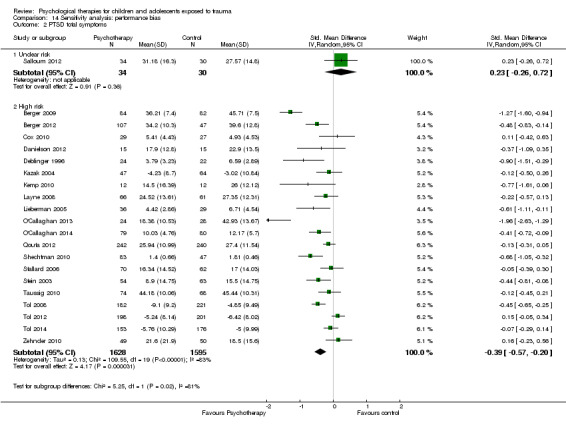
Comparison 14 Sensitivity analysis: performance bias, Outcome 2 PTSD total symptoms.
Detection bias
We found no significant differences between trials rated as having low, unclear or high risk of detection bias for the diagnosis of PTSD (Analysis 15.1) or for symptoms of PTSD (Analysis 15.2).
15.1. Analysis.
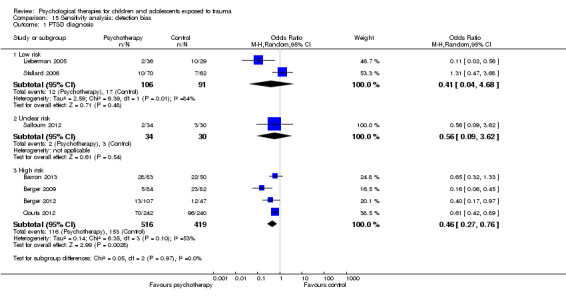
Comparison 15 Sensitivity analysis: detection bias, Outcome 1 PTSD diagnosis.
15.2. Analysis.
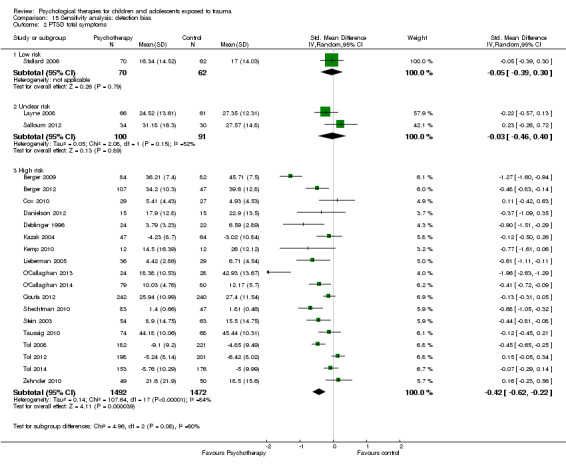
Comparison 15 Sensitivity analysis: detection bias, Outcome 2 PTSD total symptoms.
Attrition bias
We noted significant differences between trials rated as having low, unclear and high risk of attrition bias for the diagnosis of PTSD (Analysis 16.1); however, both low‐ and high‐risk studies resulted in a significant reduction in the diagnosis or PTSD. We found no differences between studies rated as having low, unclear or high risk of attrition bias for symptoms of PTSD (Analysis 16.2).
16.1. Analysis.

Comparison 16 Sensitivity analysis: attrition bias, Outcome 1 PTSD diagnosis.
16.2. Analysis.

Comparison 16 Sensitivity analysis: attrition bias, Outcome 2 PTSD total symptoms.
Cluster‐randomised versus individually randomised trials
We found no significant differences between cluster‐randomised and individually randomised trials for the outcomes of PTSD diagnosis (Analysis 13.1) and symptoms (Analysis 13.2).
13.1. Analysis.
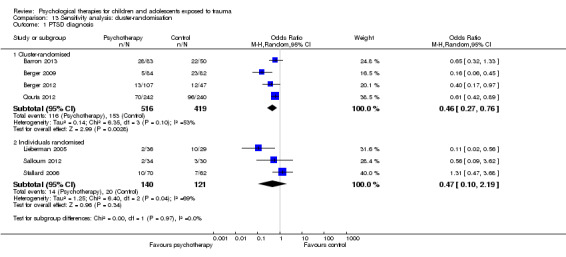
Comparison 13 Sensitivity analysis: cluster‐randomisation, Outcome 1 PTSD diagnosis.
13.2. Analysis.
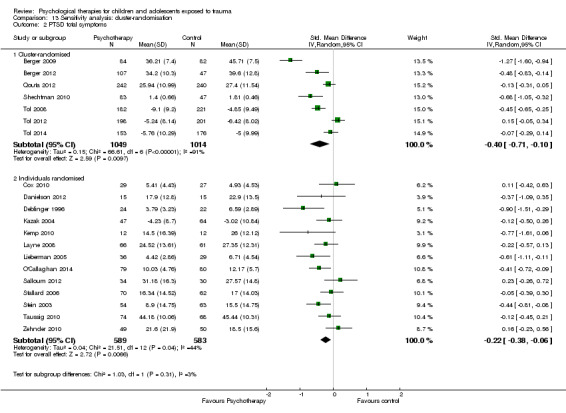
Comparison 13 Sensitivity analysis: cluster‐randomisation, Outcome 2 PTSD total symptoms.
Assessment of reporting bias
We created a funnel plot for the primary outcome of PTSD symptoms using data provided by the 15 trials reporting these data in the short term (Figure 4). We noted no asymmetry in the funnel plot.
4.

Funnel plot of comparison: 1 All psychotherapies versus control (short‐term), outcome: 1.2 PTSD total symptoms.
Discussion
Summary of main results
The likelihood of being diagnosed with post‐traumatic stress disorder (PTSD) and PTSD symptoms were significantly reduced in children and adolescents who received a psychological therapy compared to those who received treatment as usual, no treatment, or were on a wait list for up to a month following treatment. The GRADE quality of evidence for PTSD symptoms was rated low because participants probably were aware of whether they received the intervention and because high levels of heterogeneity between studies (see Table 1). The evidence for diagnosis of PTSD was further limited by small study and participant numbers and therefore rated as very low (see Table 1). The effects of psychological therapies were not apparent over the longer term.
Cognitive‐behavioural therapy (CBT) was found to be no more or less effective than eye movement desensitisation and reprocessing (EMDR) and supportive therapy in reducing diagnosis of PTSD in the short term, although there was evidence favouring CBT over EMDR, play therapy and supportive therapies in reducing symptoms of PTSD for up to a month after treatment. The GRADE quality of evidence for the role of CBT in preventing PTSD diagnosis was rated very low because of lack of blinding and small sample and study numbers. Evidence for the greater effectiveness of CBT in decreasing symptoms of PTSD was rated moderate quality (see Table 2).
We did not identify any studies that compared pharmacological therapies to psychological therapies.
Overall completeness and applicability of evidence
Evidence indicates that psychological therapies were effective in preventing the development of PTSD and related symptoms across a range of psychotherapeutic approaches in the short term. Although evidence for the effectiveness of CBT was better, apparent lack of effect with other therapies may be due to lack of data.
Significant benefit from psychological therapies was evident only for up to one month following completion of treatment. Data were insufficient to permit conclusions about the effects of psychological therapies lasting longer than a month after therapy. However, lack of long‐term effects may be due in part to the small number of studies reporting data past one month and the lower rates of follow‐up for those that did so.
Difficulty is associated with conclusions about the applicability of evidence across different types of trauma, as significant differences between trials of children and adolescents with different types of trauma were reported, and generally only one study reported results for each type of trauma.
Although we noted differences in inclusion criteria in that some studies specifically included symptoms (although not a full diagnosis) of PTSD, we found no apparent differences in findings between these studies and those that did not require a predefined level of symptoms as part of the inclusion criteria.
We had intended to include only studies of children and adolescents who had been exposed to trauma within the previous year; however, time since trauma was not an inclusion criterion for any included study, and time since trauma was rarely reported. Therefore, time since trauma may also account for heterogeneity across studies.
Although evidence suggests that psychological therapies were effective in preventing the onset of PTSD and PTSD symptoms in the short term, the quality of studies comparing psychological therapies versus control was relatively low. Few studies compared psychological therapies versus other psychological therapies, and none compared psychological therapies versus pharmacological therapies or other treatments.
Quality of the evidence
Overall, risk of allocation, detection and attrition bias in included trials was unclear because inadequate details were provided by study authors to permit a judgement. Most trials were considered to have high risk of performance bias, and most were considered to have low risk of reporting bias. Marked heterogeneity was evident in several analyses. We conducted several exploratory analyses to identify sources of heterogeneity and noted differences between types of therapy and types of trauma; additional data are needed before conclusions can be drawn about the effectiveness of different therapies and the types of trauma for which they are effective. We identified no differences between trials that used active and inactive controls, but the inactive control subgroup itself was highly heterogeneous. Although we found significant differences between trials rated as having low and unclear risk of selection bias, we noted only one trial determined to have low risk and none determined to have high risk. Performance bias due to the predominance of child‐ or parent‐rated measures may have resulted in an overestimation of effects, but these findings are based on limited data. Although we found differences between risk categories in bias due to attrition, we did not note this effect with symptoms of PTSD. We found no evidence of publication bias when preparing this review. When effects of psychological therapies were apparent, GRADE ratings of the quality of evidence were very low to moderate as the result of study limitations of non‐blinded outcome measurement, lack of consistency across studies in effect size and imprecision due to small numbers of included studies and relatively small sample sizes.
Potential biases in the review process
Data generated from these included trials had some limitations. Most trials were very small, often including fewer than 100 participants and in some cases fewer than 20. Therefore, negative findings with many of these analyses may well be due to lack of power. In addition, most trials reported only short‐term outcomes. Another limitation was that large portions of the continuous data reported in these trials were skewed, and this limited the useability of data.
We used a large range of tools to measure continuous outcomes in this review (more than 20 for PTSD), making integration and interpretation of data difficult. As in the narrative review by Forman‐Hoffman 2013 of interventions for children exposed to non‐relational traumatic events, trials did not replicate interventions, short‐term interventions were reported and most were self reported outcomes.
Agreements and disagreements with other studies or reviews
Findings of this review are in line with those of Cochrane reviews that found good evidence for the effectiveness of CBT in the treatment of adults with PTSD (Bisson 2013) and acute traumatic stress symptoms (Roberts 2010) and in the prevention of adverse consequences of child sexual abuse (MacDonald 2012). In addition, a systematic review by Leenarts 2013 concluded that CBT yielded the best evidence of effectiveness among psychological therapies for children who had been maltreated, and Kramer 2011 concluded from a meta‐analysis of psychological interventions within one month following trauma that interventions should include psychoeducation, coping skills and exposure.
Authors' conclusions
Implications for practice.
Although we found some evidence for the effectiveness of psychological therapies, particularly CBT, in preventing the onset of PTSD and decreasing PTSD symptoms in children and adolescents for up to a month after treatment, the quality of this evidence was very low to moderate, and effects were not apparent in the longer term. In addition, the level of improvement appears to be considerably lower in children exposed to trauma compared with those diagnosed with PTSD (Gillies 2012), in whom improvement was seen for up to 12 months following therapy.
Implications for research.
More evidence is needed to evaluate the effectiveness of psychological therapies longer than one month after treatment. Much more evidence is needed to demonstrate the relative effectiveness of psychological therapies for children and adolescents exposed to trauma.
Future trials should aim to be double‐blind by attempting to ensure that participants and their families are not aware of who is receiving an active intervention. This can be achieved by a two‐factor design whereby two combined therapies are compared with one of those therapies as a control. In addition to achieving more effective blinding of participants and parents, this design is more ethical in that both groups receive treatment. Measures completed by blinded observers such as clinicians, in addition to measures completed by participants or their families, should also be included. Efforts should be made to ensure high rates of follow‐up in the longer term (i.e. longer than one month after therapy). In addition, data from future studies should describe the types of trauma to which children and adolescents are exposed and the time between trauma exposure and therapy. This would be best achieved by making individual participant data available for meta‐analysis.
What's new
| Date | Event | Description |
|---|---|---|
| 2 November 2008 | Amended | Protocol converted to new review format |
Acknowledgements
Pam Withey (Rogers) and Charles Meekings, co‐authors of the protocol for the original review (Gillies 2007).
CRG Funding Acknowledgement: The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Common Mental Disorders Group.
Disclaimer: The views and opinions expressed herein are those of the review authors and do not necessarily reflect those of the NIHR, the NHS or the Department of Health.
Appendices
Appendix 1. Cochrane Specialised Register ‐ core MEDLINE search strategy
Core search strategy used to inform the Cochrane Common Mental Disorders Group's specialised register: OVID Medline A weekly search alert based on condition + RCT filter only 1. [MeSH Headings]: eating disorders/ or anorexia nervosa/ or binge‐eating disorder/ or bulimia nervosa/ or female athlete triad syndrome/ or pica/ or hyperphagia/ or bulimia/ or self‐injurious behavior/ or self mutilation/ or suicide/ or suicidal ideation/ or suicide, attempted/ or mood disorders/ or affective disorders, psychotic/ or bipolar disorder/ or cyclothymic disorder/ or depressive disorder/ or depression, postpartum/ or depressive disorder, major/ or depressive disorder, treatment‐resistant/ or dysthymic disorder/ or seasonal affective disorder/ or neurotic disorders/ or depression/ or adjustment disorders/ or exp antidepressive agents/ or anxiety disorders/ or agoraphobia/ or neurocirculatory asthenia/ or obsessive‐compulsive disorder/ or obsessive hoarding/ or panic disorder/ or phobic disorders/ or stress disorders, traumatic/ or combat disorders/ or stress disorders, post‐traumatic/ or stress disorders, traumatic, acute/ or anxiety/ or anxiety, castration/ or koro/ or anxiety, separation/ or panic/ or exp anti‐anxiety agents/ or somatoform disorders/ or body dysmorphic disorders/ or conversion disorder/ or hypochondriasis/ or neurasthenia/ or hysteria/ or munchausen syndrome by proxy/ or munchausen syndrome/ or fatigue syndrome, chronic/ or obsessive behavior/ or compulsive behavior/ or behavior, addictive/ or impulse control disorders/ or firesetting behavior/ or gambling/ or trichotillomania/ or stress, psychological/ or burnout, professional/ or sexual dysfunctions, psychological/ or vaginismus/ or Anhedonia/ or Affective Symptoms/ or *Mental Disorders/
2. [Title/ Author Keywords]: (eating disorder* or anorexia nervosa or bulimi* or binge eat* or (self adj (injur* or mutilat*)) or suicide* or suicidal or parasuicid* or mood disorder* or affective disorder* or bipolar i or bipolar ii or (bipolar and (affective or disorder*)) or mania or manic or cyclothymic* or depression or depressive or dysthymi* or neurotic or neurosis or adjustment disorder* or antidepress* or anxiety disorder* or agoraphobia or obsess* or compulsi* or panic or phobi* or ptsd or posttrauma* or post trauma* or combat or somatoform or somati#ation or medical* unexplained or body dysmorphi* or conversion disorder or hypochondria* or neurastheni* or hysteria or munchausen or chronic fatigue* or gambling or trichotillomania or vaginismus or anhedoni* or affective symptoms or mental disorder* or mental health).ti,kf.
3. [RCT filter]: (controlled clinical trial.pt. or randomized controlled trial.pt. or (randomi#ed or randomi#ation).ab,ti. or randomly.ab. or (random* adj3 (administ* or allocat* or assign* or class* or control* or determine* or divide* or distribut* or expose* or fashion or number* or place* or recruit* or subsitut* or treat*)).ab. or placebo*.ab,ti. or drug therapy.fs. or trial.ab,ti. or groups.ab. or (control* adj3 (trial* or study or studies)).ab,ti. or ((singl* or doubl* or tripl* or trebl*) adj3 (blind* or mask* or dummy*)).mp. or clinical trial, phase ii/ or clinical trial, phase iii/ or clinical trial, phase iv/ or randomized controlled trial/ or pragmatic clinical trial/ or (quasi adj (experimental or random*)).ti,ab. or ((waitlist* or wait* list* or treatment as usual or TAU) adj3 (control or group)).ab.)
4. (1 and 2 and 3)
Records are screened for reports of RCTs within the scope of the Cochrane Common Mental Disorders Group. Secondary reports of RCTs are tagged to the appropriate study record. Similar weekly search alerts are also conducted on OVID EMBASE and PsycINFO, using relevant subject headings (controlled vocabularies) and search syntax, appropriate to each resource.
Data and analyses
Comparison 1. All psychotherapies versus control (short‐term).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD diagnosis | 5 | 874 | Odds Ratio (M‐H, Random, 95% CI) | 0.51 [0.34, 0.77] |
| 1.1 CBT | 3 | 769 | Odds Ratio (M‐H, Random, 95% CI) | 0.59 [0.43, 0.80] |
| 1.2 EMDR | 1 | 40 | Odds Ratio (M‐H, Random, 95% CI) | 0.2 [0.01, 4.44] |
| 1.3 Family therapy | 1 | 65 | Odds Ratio (M‐H, Random, 95% CI) | 0.11 [0.02, 0.56] |
| 2 PTSD total symptoms | 15 | 2051 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐0.61, ‐0.24] |
| 2.1 CBT | 6 | 1329 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.55, ‐0.19] |
| 2.2 EMDR | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐1.61, 0.06] |
| 2.3 Family therapy | 2 | 95 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.94, ‐0.12] |
| 2.4 Narrative | 1 | 64 | Std. Mean Difference (IV, Random, 95% CI) | 0.23 [‐0.26, 0.72] |
| 2.5 Psychoeducation | 2 | 215 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.69, 0.30] |
| 2.6 Supportive therapy | 2 | 272 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.95, 0.15] |
| 2.7 CBT + narrative therapy | 1 | 52 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.96 [‐2.63, ‐1.29] |
| 3 PTSD avoidance | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.29, 0.26] |
| 3.1 Narrative | 1 | 158 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.27, 0.36] |
| 3.2 Psychoeducation | 1 | 47 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.80, 0.35] |
| 4 PTSD hyperarousal | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.22, 0.32] |
| 4.1 Narrative | 1 | 158 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.21, 0.41] |
| 4.2 Psychoeducation | 1 | 47 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.70, 0.45] |
| 5 PTSD intrusion | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.16, 0.39] |
| 5.1 Narrative | 1 | 158 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.16, 0.46] |
| 5.2 Psychoeducation | 1 | 47 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.59, 0.55] |
| 6 Anxiety total symptoms | 7 | 959 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.26, 0.00] |
| 6.1 CBT | 2 | 557 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.30, 0.04] |
| 6.2 Counselling | 1 | 130 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.56, 0.16] |
| 6.3 EMDR | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.30, ‐0.03] |
| 6.4 Exposure | 1 | 65 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.48, 0.51] |
| 6.5 Narrative | 1 | 111 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.58, 0.17] |
| 6.6 Psychoeducation | 1 | 56 | Std. Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.21, 0.85] |
| 7 Anxiety ‐ state | 2 | 70 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.12, ‐0.16] |
| 7.1 CBT | 1 | 46 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.31, ‐0.12] |
| 7.2 EMDR | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.33, 0.31] |
| 8 Anxiety ‐ trait | 2 | 70 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.81, 0.14] |
| 8.1 CBT | 1 | 46 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.94, 0.22] |
| 8.2 EMDR | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐1.10, 0.51] |
| 9 Depression | 13 | 1569 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.30, 0.04] |
| 9.1 CBT | 6 | 1191 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.42, ‐0.00] |
| 9.2 EMDR | 2 | 64 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐1.41, 0.64] |
| 9.3 Exposure | 1 | 52 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.45, 0.65] |
| 9.4 Family therapy | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.66, 0.77] |
| 9.5 Narrative | 2 | 176 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.52, 0.77] |
| 9.6 Psychoeducation | 1 | 56 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.43, 0.62] |
| 10 Behaviour ‐ total | 3 | 166 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.51, 0.42] |
| 10.1 EMDR | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐1.25, 0.37] |
| 10.2 Exposure | 1 | 77 | Std. Mean Difference (IV, Random, 95% CI) | 0.34 [‐0.11, 0.80] |
| 10.3 Family therapy | 1 | 65 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.72, 0.26] |
| 11 Behaviour ‐ internalising | 10 | 719 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.20, 0.13] |
| 11.1 CBT | 2 | 162 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.44, 0.18] |
| 11.2 EMDR | 2 | 64 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐1.07, ‐0.07] |
| 11.3 Exposure | 1 | 77 | Std. Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.08, 0.84] |
| 11.4 Family therapy | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.40, 1.04] |
| 11.5 Narrative | 2 | 180 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.18, 0.41] |
| 11.6 Psychoeducation | 2 | 206 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.38, 0.17] |
| 12 Behaviour ‐ externalising | 12 | 1174 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.33, 0.14] |
| 12.1 CBT | 3 | 565 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.28, 0.06] |
| 12.2 EMDR | 2 | 64 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐1.19, 0.10] |
| 12.3 Exposure | 1 | 77 | Std. Mean Difference (IV, Random, 95% CI) | 0.49 [0.03, 0.95] |
| 12.4 Family therapy | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | 0.23 [‐0.49, 0.95] |
| 12.5 Narrative | 2 | 180 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.41, 0.81] |
| 12.6 Psychoeducation | 2 | 206 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.52, 0.46] |
| 12.7 CBT + narrative therapy | 1 | 52 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.06 [‐1.64, ‐0.47] |
| 13 Functional impairment | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 CBT | 2 | 557 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.59, ‐0.24] |
| 14 Quality of life | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Supportive therapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Loss to follow‐up | 26 | 3872 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.69, 1.39] |
| 15.1 CBT | 14 | 2913 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.47, 1.62] |
| 15.2 Counselling | 1 | 164 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.30, 1.03] |
| 15.3 EMDR | 2 | 92 | Risk Ratio (M‐H, Random, 95% CI) | 1.64 [0.48, 5.59] |
| 15.4 Exposure | 1 | 16 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.5 Family therapy | 2 | 105 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.48, 4.30] |
| 15.6 Narrative | 2 | 280 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.32, 2.39] |
| 15.7 Psychoeducation | 3 | 274 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.75, 1.96] |
| 15.8 Psychodrama | 1 | 28 | Risk Ratio (M‐H, Random, 95% CI) | 1.5 [0.29, 7.65] |
Comparison 2. All psychotherapies versus control (medium‐term).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD diagnosis | 4 | 742 | Odds Ratio (M‐H, Random, 95% CI) | 0.66 [0.26, 1.69] |
| 1.1 CBT | 2 | 570 | Odds Ratio (M‐H, Random, 95% CI) | 0.49 [0.09, 2.61] |
| 1.2 Debriefing | 1 | 132 | Odds Ratio (M‐H, Random, 95% CI) | 1.31 [0.47, 3.68] |
| 1.3 EMDR | 1 | 40 | Odds Ratio (M‐H, Random, 95% CI) | 0.35 [0.01, 9.13] |
| 2 PTSD total symptoms | 12 | 2337 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.38, 0.05] |
| 2.1 CBT | 5 | 1701 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.72, 0.03] |
| 2.2 Debriefing | 2 | 231 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.22, 0.30] |
| 2.3 Family therapy | 2 | 141 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.39, 0.27] |
| 2.4 Narrative | 1 | 64 | Std. Mean Difference (IV, Random, 95% CI) | 0.23 [‐0.26, 0.73] |
| 2.5 Psychoeducation | 1 | 56 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.65, 0.40] |
| 2.6 Supportive therapy | 1 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.54, 0.12] |
| 3 PTSD ‐ avoidance | 2 | 243 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.22, 0.29] |
| 3.1 Debriefing | 1 | 132 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.08 [‐0.42, 0.26] |
| 3.2 Family therapy | 1 | 111 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.18 [‐0.20, 0.55] |
| 4 PTSD ‐ hyperarousal | 2 | 243 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.43, 0.17] |
| 4.1 Debriefing | 1 | 132 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.33, 0.35] |
| 4.2 Family therapy | 1 | 111 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.67, 0.09] |
| 5 PTSD ‐ intrusion | 2 | 243 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.29, 0.21] |
| 5.1 Debriefing | 1 | 132 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.39, 0.29] |
| 5.2 Family therapy | 1 | 111 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.40, 0.35] |
| 6 Anxiety total symptoms | 7 | 1470 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.20, 0.00] |
| 6.1 CBT | 3 | 1131 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.19, 0.04] |
| 6.2 Debriefing | 1 | 132 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.42, 0.27] |
| 6.3 EMDR | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.72 [‐1.36, ‐0.07] |
| 6.4 Psychoeducation | 1 | 56 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.73, 0.32] |
| 6.5 Narrative | 1 | 111 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.54, 0.21] |
| 7 Anxiety ‐ state | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 CBT | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Anxiety ‐ trait | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 CBT | 2 | 101 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.45 [‐0.85, ‐0.05] |
| 9 Depression | 13 | 2191 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.22, 0.07] |
| 9.1 CBT | 8 | 1810 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.31, 0.07] |
| 9.2 Debriefing | 2 | 231 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.38, 0.14] |
| 9.3 Family therapy | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | 0.34 [‐0.38, 1.06] |
| 9.4 Narrative | 1 | 64 | Std. Mean Difference (IV, Random, 95% CI) | 0.34 [‐0.15, 0.84] |
| 9.5 Psychoeducation | 1 | 56 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.67, 0.38] |
| 10 Behaviour ‐ total | 3 | 281 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.43, 0.04] |
| 10.1 Debriefing | 1 | 132 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐0.62, 0.06] |
| 10.2 Family therapy | 1 | 50 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.37 [‐0.93, 0.19] |
| 10.3 Narrative | 1 | 99 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.39, 0.39] |
| 11 Behaviour ‐ internalising | 4 | 291 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.25, 0.28] |
| 11.1 EMDR | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.13, 0.14] |
| 11.2 Family therapy | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.72, 0.72] |
| 11.3 Narrative | 2 | 221 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.13, 0.40] |
| 12 Behaviour ‐ externalising | 5 | 694 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.32, 0.35] |
| 12.1 CBT | 1 | 403 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.13, 0.27] |
| 12.2 EMDR | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | 1.00 [‐1.66, ‐0.33] |
| 12.3 Family therapy | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.72, 0.71] |
| 12.4 Narrative | 2 | 221 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [0.05, 0.58] |
| 13 Function | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 CBT | 3 | 814 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.88, ‐0.05] |
| 14 Quality of life | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Supportive therapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Loss to follow‐up | 20 | 3663 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.82, 1.21] |
| 15.1 CBT | 11 | 2856 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.81, 1.27] |
| 15.2 Counselling | 1 | 23 | Odds Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.32, 152.95] |
| 15.3 Debriefing | 1 | 158 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.33, 1.76] |
| 15.4 EMDR | 1 | 65 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.41 [0.52, 3.84] |
| 15.5 Family therapy | 1 | 75 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.48, 3.39] |
| 15.6 Narrative | 2 | 171 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.16, 2.99] |
| 15.7 Psychoeducation | 2 | 244 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.40, 1.47] |
| 15.8 Other | 1 | 71 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.29, 2.73] |
Comparison 3. All psychotherapies versus control (long‐term).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD diagnosis | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Narrative | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PTSD total symptoms | 2 | 141 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.28, 0.62] |
| 2.1 Exposure | 1 | 77 | Std. Mean Difference (IV, Random, 95% CI) | 0.39 [‐0.07, 0.85] |
| 2.2 Narrative | 1 | 64 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.56, 0.42] |
| 3 Anxiety | 2 | 176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.41, 0.18] |
| 3.1 Exposure | 1 | 65 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.80, 0.19] |
| 3.2 Narrative | 1 | 111 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.39, 0.36] |
| 4 Depression | 3 | 152 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.24 [‐0.56, 0.08] |
| 4.1 CBT | 1 | 36 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.59 [‐1.27, 0.09] |
| 4.2 Exposure | 1 | 52 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.29 [‐0.84, 0.26] |
| 4.3 Narrative | 1 | 64 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.51, 0.47] |
| 5 Behaviour ‐ total | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Exposure | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Behaviour ‐ internalising | 2 | 141 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.51, 0.59] |
| 6.1 Exposure | 1 | 77 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [‐0.15, 0.77] |
| 6.2 Narrative | 1 | 64 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.75, 0.24] |
| 7 Behaviour ‐ externalising | 3 | 298 | Std. Mean Difference (IV, Random, 95% CI) | 0.28 [‐0.05, 0.60] |
| 7.1 Exposure | 1 | 77 | Std. Mean Difference (IV, Random, 95% CI) | 0.51 [0.04, 0.97] |
| 7.2 Narrative | 2 | 221 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.30, 0.64] |
| 8 Loss to follow‐up | 2 | 120 | Odds Ratio (M‐H, Random, 95% CI) | 0.45 [0.15, 1.32] |
| 8.1 CBT | 1 | 50 | Odds Ratio (M‐H, Random, 95% CI) | 0.29 [0.08, 1.09] |
| 8.2 Narrative | 1 | 70 | Odds Ratio (M‐H, Random, 95% CI) | 0.88 [0.17, 4.71] |
Comparison 4. CBT versus other therapies (short‐term).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD diagnosis | 2 | 160 | Odds Ratio (M‐H, Random, 95% CI) | 0.74 [0.29, 1.91] |
| 1.1 EMDR | 1 | 36 | Odds Ratio (M‐H, Random, 95% CI) | 1.0 [0.06, 17.33] |
| 1.2 Supportive therapy | 1 | 124 | Odds Ratio (M‐H, Random, 95% CI) | 0.71 [0.26, 1.95] |
| 2 PTSD total symptoms | 7 | 466 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.42, ‐0.05] |
| 2.1 EMDR | 2 | 62 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.44, 0.56] |
| 2.2 Play therapy | 1 | 26 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.56, 0.98] |
| 2.3 Supportive therapies | 4 | 378 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.53, ‐0.12] |
| 3 PTSD avoidance | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Supportive therapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 PTSD hyperarousal | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Supportive therapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 PTSD intrusion | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Supportive therapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Anxiety total symptoms | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Supportive therapy | 2 | 230 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.74, ‐0.22] |
| 7 Depression | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Supportive therapy | 2 | 237 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.42, 0.14] |
| 8 Behaviour ‐ total | 3 | 182 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.27, 0.31] |
| 8.1 EMDR | 1 | 14 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐1.50, 0.63] |
| 8.2 Supportive therapy | 2 | 168 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.25, 0.36] |
| 9 Behaviour ‐ internalising | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 Supportive therapy | 3 | 235 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.79, 0.28] |
| 10 Behaviour ‐ externalising | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 Supportive therapy | 3 | 235 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.58, ‐0.05] |
| 11 Function | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Supportive therapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Loss to follow‐up | 8 | 544 | Odds Ratio (M‐H, Random, 95% CI) | 0.69 [0.41, 1.18] |
| 12.1 EMDR | 2 | 64 | Odds Ratio (M‐H, Random, 95% CI) | 0.76 [0.23, 2.52] |
| 12.2 Play therapy | 1 | 31 | Odds Ratio (M‐H, Random, 95% CI) | 0.08 [0.00, 1.56] |
| 12.3 Supportive therapy | 5 | 449 | Odds Ratio (M‐H, Random, 95% CI) | 0.74 [0.38, 1.43] |
Comparison 5. CBT versus other therapies (medium‐term).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD total symptoms | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Supportive therapy | 2 | 223 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.43, 0.11] |
| 2 Anxiety total symptoms | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Supportive therapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Depression | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Supportive therapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Behaviour ‐ total | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Supportive therapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Behaviour ‐ internalising | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Supportive therapy | 2 | 178 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.36, 0.26] |
| 6 Behaviour ‐ externalising | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Supportive therapy | 2 | 178 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.37, 0.25] |
| 7 Loss to follow‐up | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 Supportive therapy | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
5.2. Analysis.
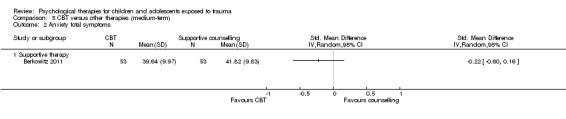
Comparison 5 CBT versus other therapies (medium‐term), Outcome 2 Anxiety total symptoms.
5.3. Analysis.
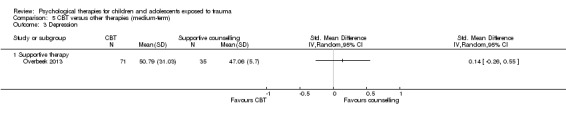
Comparison 5 CBT versus other therapies (medium‐term), Outcome 3 Depression.
5.4. Analysis.
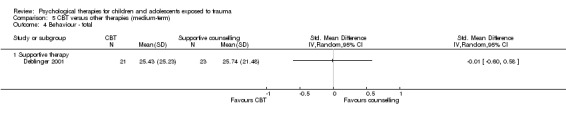
Comparison 5 CBT versus other therapies (medium‐term), Outcome 4 Behaviour ‐ total.
5.5. Analysis.

Comparison 5 CBT versus other therapies (medium‐term), Outcome 5 Behaviour ‐ internalising.
5.6. Analysis.

Comparison 5 CBT versus other therapies (medium‐term), Outcome 6 Behaviour ‐ externalising.
5.7. Analysis.

Comparison 5 CBT versus other therapies (medium‐term), Outcome 7 Loss to follow‐up.
Comparison 6. CBT versus other therapies (long‐term).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Behaviour ‐ internalising | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Supportive therapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Behaviour ‐ externalising | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Supportive therapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Loss to follow‐up | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Supportive therapy | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
6.1. Analysis.

Comparison 6 CBT versus other therapies (long‐term), Outcome 1 Behaviour ‐ internalising.
6.2. Analysis.
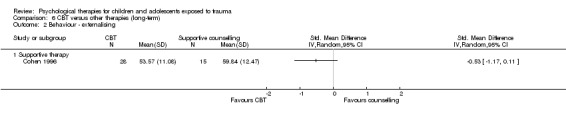
Comparison 6 CBT versus other therapies (long‐term), Outcome 2 Behaviour ‐ externalising.
6.3. Analysis.

Comparison 6 CBT versus other therapies (long‐term), Outcome 3 Loss to follow‐up.
Comparison 7. Subgroup analysis: Individual versus group therapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD total symptoms | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Short‐term | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 8. Subgroup analysis: Child versus mother and child therapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD total symptoms | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Short‐term | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Medium‐term | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Long‐term | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 9. Subgroup analysis: type of trauma.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD diagnosis | 6 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Community violence | 3 | 769 | Odds Ratio (M‐H, Random, 95% CI) | 0.59 [0.43, 0.80] |
| 1.2 Interpersonal violence | 1 | 65 | Odds Ratio (M‐H, Random, 95% CI) | 0.11 [0.02, 0.56] |
| 1.3 Natural disaster | 1 | 166 | Odds Ratio (M‐H, Random, 95% CI) | 0.16 [0.06, 0.45] |
| 1.4 Physical trauma | 1 | 132 | Odds Ratio (M‐H, Random, 95% CI) | 1.31 [0.47, 3.68] |
| 2 PTSD total symptoms | 18 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Community violence | 8 | 2170 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.41, ‐0.06] |
| 2.2 Interpersonal violence | 1 | 65 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.11, ‐0.11] |
| 2.3 Life‐threatening illness | 1 | 111 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.50, 0.26] |
| 2.4 Maltreatment | 1 | 142 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.45, 0.21] |
| 2.5 Natural disaster | 1 | 166 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.27 [‐1.60, ‐0.94] |
| 2.6 Physical trauma | 4 | 311 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.29, 0.26] |
| 2.7 Sexual abuse | 2 | 76 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.18, ‐0.16] |
Comparison 10. Subgroup analysis: symptomatic participants.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD diagnosis | 7 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Symptoms not stated | 5 | 999 | Odds Ratio (M‐H, Random, 95% CI) | 0.41 [0.20, 0.83] |
| 1.2 Symptomatic | 2 | 197 | Odds Ratio (M‐H, Random, 95% CI) | 0.64 [0.32, 1.25] |
| 2 PTSD total symptoms | 21 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Symptoms not stated | 12 | 1648 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.68, ‐0.13] |
| 2.2 Symptomatic | 9 | 1639 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.53, ‐0.06] |
Comparison 11. Sensitivity analysis: type of control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD diagnosis | 7 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Inactive control | 5 | 1067 | Odds Ratio (M‐H, Random, 95% CI) | 0.53 [0.32, 0.88] |
| 1.2 Active control | 2 | 129 | Odds Ratio (M‐H, Random, 95% CI) | 0.23 [0.05, 1.14] |
| 2 PTSD total symptoms | 21 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Inactive control | 15 | 2856 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.61, ‐0.19] |
| 2.2 Active control | 6 | 431 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.58, 0.09] |
Comparison 12. Sensitivity analysis: best‐/worst‐case analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD diagnosis | 7 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Best case | 7 | 1282 | Odds Ratio (M‐H, Random, 95% CI) | 0.52 [0.28, 0.99] |
| 1.2 Worst case | 7 | 1252 | Odds Ratio (M‐H, Random, 95% CI) | 0.64 [0.42, 0.98] |
Comparison 13. Sensitivity analysis: cluster‐randomisation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD diagnosis | 7 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Cluster‐randomised | 4 | 935 | Odds Ratio (M‐H, Random, 95% CI) | 0.46 [0.27, 0.76] |
| 1.2 Individuals randomised | 3 | 261 | Odds Ratio (M‐H, Random, 95% CI) | 0.47 [0.10, 2.19] |
| 2 PTSD total symptoms | 20 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Cluster‐randomised | 7 | 2063 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.71, ‐0.10] |
| 2.2 Individuals randomised | 13 | 1172 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.38, ‐0.06] |
Comparison 14. Sensitivity analysis: performance bias.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD diagnosis | 7 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Unclear risk | 1 | 64 | Odds Ratio (M‐H, Random, 95% CI) | 0.56 [0.09, 3.62] |
| 1.2 High risk | 6 | 1132 | Odds Ratio (M‐H, Random, 95% CI) | 0.46 [0.27, 0.79] |
| 2 PTSD total symptoms | 21 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Unclear risk | 1 | 64 | Std. Mean Difference (IV, Random, 95% CI) | 0.23 [‐0.26, 0.72] |
| 2.2 High risk | 20 | 3223 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐0.57, ‐0.20] |
Comparison 15. Sensitivity analysis: detection bias.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD diagnosis | 7 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Low risk | 2 | 197 | Odds Ratio (M‐H, Random, 95% CI) | 0.41 [0.04, 4.68] |
| 1.2 Unclear risk | 1 | 64 | Odds Ratio (M‐H, Random, 95% CI) | 0.56 [0.09, 3.62] |
| 1.3 High risk | 4 | 935 | Odds Ratio (M‐H, Random, 95% CI) | 0.46 [0.27, 0.76] |
| 2 PTSD total symptoms | 21 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Low risk | 1 | 132 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.39, 0.30] |
| 2.2 Unclear risk | 2 | 191 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.46, 0.40] |
| 2.3 High risk | 18 | 2964 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐0.62, ‐0.22] |
Comparison 16. Sensitivity analysis: attrition bias.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD diagnosis | 7 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Low risk | 2 | 320 | Odds Ratio (M‐H, Random, 95% CI) | 0.27 [0.11, 0.65] |
| 1.2 Unclear risk | 3 | 329 | Odds Ratio (M‐H, Random, 95% CI) | 0.79 [0.45, 1.38] |
| 1.3 High risk | 2 | 547 | Odds Ratio (M‐H, Random, 95% CI) | 0.32 [0.06, 1.60] |
| 2 PTSD total symptoms | 21 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Low risk | 7 | 1410 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.75, ‐0.01] |
| 2.2 Unclear risk | 9 | 1046 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.67, ‐0.05] |
| 2.3 High risk | 5 | 831 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.53, ‐0.06] |
Comparison 17. Sensitivity analysis: selection bias.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PTSD diagnosis | 7 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Low risk | 4 | 516 | Odds Ratio (M‐H, Random, 95% CI) | 0.46 [0.18, 1.15] |
| 1.2 Unclear risk | 2 | 547 | Odds Ratio (M‐H, Random, 95% CI) | 0.32 [0.06, 1.60] |
| 1.3 High risk | 1 | 133 | Odds Ratio (M‐H, Random, 95% CI) | 0.65 [0.32, 1.33] |
| 2 PTSD total symptoms | 21 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Low risk | 8 | 874 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐0.97, ‐0.17] |
| 2.2 Unclear risk | 13 | 2413 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.39, ‐0.06] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Baker 1985.
| Methods | Randomised trial of individual vs group therapy | |
| Participants |
Included (n = 39) Adolescent females 13 to 17 years of age who had suffered contact sexual abuse validated by child protective services. Ethnicity: white 31, black 8. The girls were in the process of court proceedings or investigative procedures; 9 completed the court process during treatment Excluded Not reported Setting Counselling centre in a rural county in Delaware, USA |
|
| Interventions |
Both therapies Therapists were instructed to use Rogerian techniques in both individual and group therapies. Therapists were given a list of topics to be introduced for discussion, including associated emotions and life changes, assertiveness and coping, family roles, support systems and resources, communication, court preparation and social concerns Individual therapy (n = 15) Individual therapy sessions of 1 hour were conducted for 10 weeks Group therapy (n = 24) Group therapy allowed sharing of experiences and information and provided feedback from other victims. Group sessions of 1 ½ hours were run with a maximum of 8 participants over 6 weeks Therapists All held master's level degrees in counselling disciplines, had received training in treatment of sexual abuse and were skilled in Rogerian techniques. Therapists were also provided with examples of Rogerian techniques (restatement, reflection of meaning, reflection of feeling, congruence, acceptance and reinforcement of positive feelings). Each of the 3 therapists led 1 group and saw 5 girls individually |
|
| Outcomes |
Depression Scale: Institute for Personality and Ability Testing Depression Scale Rater: adolescent Anxiety Scale: Institute for Personality and Ability Testing Anxiety Scale Rater: adolescent When Post therapy |
|
| Notes | Depression and anxiety were in the normal range at pretest for both groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment was achieved by having participants draw 1 slip of paper at a time from a box until all were assigned |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Participants could not be blinded, but both groups received a psychological therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessment could not be blinded, as all measures were self report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up was not reported |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other apparent bias |
Barron 2013.
| Methods | Cluster‐randomised trial of teaching recovery technique vs wait list | |
| Participants |
Included (n = 140) The 10 students with the highest CRIES‐13 scores in each class of 11‐ to 14‐year‐olds. Female: 60. Mean age: 11.08 (range 11 to 14) years. Ethnicity: all Palestinian Excluded Students with incomplete pretest data Setting Nablus, Palestine; selected because of high levels of ongoing violence |
|
| Interventions |
Teaching recovery technique (n = 90) This cognitive‐behavioural programme includes 5 sessions that focus on normalising trauma and strategies for intrusive memories, hyperarousal and avoidance symptoms of PTSD. The fifth session focuses on children’s response to loss. Sessions were delivered over 5 consecutive weeks. Each session lasted 1 hour and 30 minutes. Two counsellors were present during programme delivery ‐ one to present and the other to observe Wait list (n = 50) The wait list received the usual school health education curriculum (health and social issues) Therapists Counsellors received 3 days of training in programme delivery provided by 2 expert trainers from the Children and War Foundation, covering programme values, content and processes Programme fidelity was assessed by 18 observers who completed a fidelity questionnaire Observers reported that 60% of objectives were achieved and 74% of guidelines were followed |
|
| Outcomes |
Diagnosis Scale: score ≥ 17 on the Children’s Revised Impact of Events Scale (CRIES‐13) Rater: child/adolescent Trauma symptoms Scale: CRIES‐13 Rater: child/adolescent Depression Scale: Depression Self‐Rating Scale for Children Rater: child/adolescent Behaviour Scale: Strength and Difficulties Questionnaire Rater: child/adolescent When Two weeks after intervention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Counsellors trained in the intervention were randomly allocated to groups by the principal researcher, who 'blindly selected' their names from a container; however, counsellors then ‘identified’ classes |
| Allocation concealment (selection bias) | High risk | See above |
| Blinding of participants (performance bias | High risk | Participants were probably aware of whether they were in the active or wait list group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | 'Questionnaires were translated to Arabic and then blind back‐translated to English from Arabic', but all measures were self reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up 5% |
| Selective reporting (reporting bias) | Unclear risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other apparent bias |
Berger 2009.
| Methods | Cluster‐randomised trial of ERASE Stress Sri Lanka group therapy vs wait list | |
| Participants |
Included (n = 166) Children 9 to 14 years of age exposed to the 2004 tsunami Female: 73. Trauma exposure: physically hurt during the tsunami 139, knew someone close who had died during the tsunami 100, exposed to another major traumatic incident 148 Excluded Not reported Setting School in a small town that suffered a direct hit from the tsunami in Welligama Sri Lanka, 2006 |
|
| Interventions |
Group therapy (n = 84) Twelve weekly 90‐minute sessions of 12 to 16 participants (grouped by age and gender for the older 2 groups). Key components: CBT, psychoeducation, meditation, bioenergetic exercises, coping skills, narrative techniques including art therapy, planning for the future Wait list control (n = 82) Children in this group attended a religious class Therapists Teacher training was given to all 12 homeroom teachers over 3 days. Each teacher was responsible for 1 class only |
|
| Outcomes |
Diagnosis Scale: score ≥ 3 on 1 item of the UCLA PTSD Index (17‐item) Rater: child Trauma symptoms Scale: UCLA PTSD Index Rater: child Depression Scale: Beck Depression Inventory (7‐item) Rater: child Functional problems Scale: Child Diagnostic Interview Schedule (7‐item) Rater: clinician When At 3‐month follow‐up |
|
| Notes | So they could be added to the meta‐analysis of function, functional impairment scores were converted to negative values | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | One class in each of the 6 age groups were randomised by coin toss to group therapy or wait list control |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in the active or wait list group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Although 'volunteers blinded to the experimental condition administered questionnaires', all measures were self reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up: "we had no dropouts among those who completed the questionnaires. There were no missing data" |
| Selective reporting (reporting bias) | High risk | Only diagnosis was reported |
| Other bias | Low risk | No other bias was apparent |
Berger 2012.
| Methods | Cluster‐randomised trial of ERASE‐Stress vs wait list | |
| Participants |
Included (n = 154) 7th and 8th grade students from the largest Jewish governmental religious school in Sderot whose parents had participated in a psychoeducation session and had given informed consent. Females: 83 (53.9%). Age: mean 12.8 (range 11 to 13) years. 96% had been exposed to missile attacks Excluded Setting The largest Jewish governmental religious school with approximately 1200 students in Sderot, a town in Southern Israel exposed to ongoing and intense war‐related threat from daily rocket attacks and mortar shelling, 2007 to 2008 |
|
| Interventions |
ERASE‐Stress (n = 107) Covered cognitive‐behavioural techniques; psychoeducation on types and impact of stress, normative and non‐normative reactions; connections between sensations, thoughts and feelings; identification of personal resources and enhancement of coping strategies, affect modulation, emotional awareness, positive self talk and self affirmation techniques; and modalities to express feelings. The intervention consisted of 16 weekly 90‐minute classroom sessions. All sessions included homework review, warm‐up introduction, experiential exercises, psychoeducational material, learned skills and a closure exercise, followed by a new homework assignment Two major adaptations were made to the original ERASE Stress programme, extending the programme from 12 to 16 sessions. These included religious and spiritual practices, affect modulation strategies, self affirmations, a practice session on combating fears and additional social skills Wait list (n = 47) Homeroom teachers of wait list classes were instructed to delay the intervention for the following year Therapists Sessions were given in weekly social study classes traditionally taught by homeroom teachers All 6 seventh and eighth grade homeroom teachers participated in eight 3‐hour training sessions Fidelity assessments were done to ensure that the manual was followed. Teachers were aware that trainers would come and observe interventions but did not know when |
|
| Outcomes |
Diagnosis Scale: UCLA PTSD‐I (17‐item) Rater: child/adolescent Trauma symptoms Scale: UCLA PTSD‐I (17‐item) Rater: child/adolescent Anxiety Scale: Screen for Child Anxiety‐Related Emotional Disorders (7‐item) Rater: child/adolescent Functional impairment Scale: Child Diagnostic Interview Schedule (4‐item) Rater: child/adolescent When At 1 month after training |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘we randomly (by picking paper slips out of a bag) assigned four of the six seventh and eighth grade classes (two in each grade level) to the experimental EES and two classes (one class for each grade level) to the waiting list (WL) condition’ |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in the active or wait list group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | ‘Clinicians blinded to the experimental condition assisted students when necessary’, but all measures were self reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were followed up |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Berkowitz 2011.
| Methods | Block‐randomised trial of child and family traumatic stress intervention vs supportive therapy | |
| Participants |
Included (n = 106) Youth 7 to 17 years of age attending a paediatric emergency department and reporting ≥ 1 new distressing post‐traumatic stress symptom. Mean age: 12 years. Female: 52% Caucasian 32%, African American 37%, Hispanic 22%, multi‐ethnic 7%, other ethnicities 2%. Trauma exposure: motor vehicle accident 24%, sexual abuse 18%, witnessing violence 19%, physical assaults 21%, injuries 8%, threats of violence 5% Excluded Receiving counselling or mental health treatment, developmental delay, psychotic or bipolar disorder, caregiver or participant did not speak English Setting Trauma Section of the Yale Child Study Center, USA, 2006 to 2009 |
|
| Interventions |
Child and family traumatic stress intervention (n = 53) Four sessions involving child and caregiver used cognitive, behavioural and psychoeducational techniques. Identification of trauma responses, behavioural skills and communication between caregiver and child included Control (n = 53) Four sessions over 4 weeks involving child and caregiver included psychoeducation, relaxation training, coping strategies and supportive therapy Therapists Master's and doctoral level clinicians. Fidelity checked and weekly supervision provided |
|
| Outcomes |
Trauma symptoms Scale: Trauma Symptom Checklist for Children (54‐item) Rater: child/adolescent Anxiety Scale: Trauma Symptom Checklist for Children Rater: child/adolescent When Post therapy and at 3‐month follow‐up |
|
| Notes | Standard deviations calculated from standard errors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block‐randomised (block size of 10) using number containers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Participants could not be blinded, but both groups received psychological therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessment could not be blinded, as all measures were self report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Analysis appears to be based on 'last observation carried forward', but loss to follow‐up was relatively high: post therapy 25%, 3 months 27% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Berliner 1996.
| Methods | Cluster‐randomised trial of stress inoculation training, gradual exposure and standard group therapy vs standard group therapy only | |
| Participants |
Included (n = 154) Child:ren 4 to 13 years of age reporting sexual abuse that child protection services or law enforcement professionals had substantiated or did not consider unfounded. Female 90%. Caucasian 73%. The index assault was rape in 49%; 75% were serially assaulted. The chart diagnosis was PTSD in 81% Excluded Those who did not complete a minimum 8 of 10 sessions Setting Two sexual assault clinics in a major metropolitan area, USA |
|
| Interventions |
Stress inoculation training/Gradual exposure/Standard group therapy (n = 48) Experimental interventions were stress inoculation training and gradual exposure, in addition to standard group therapy Standard group therapy only (n = 32) The 10 sessions over 10 weeks covered feelings, family and friends, disclosure impact, self esteem and sexual abuse, body awareness and sexuality and prevention and termination Therapists Both treatment protocols were manualised. Therapists were trained in both protocols. Therapists completed a checklist describing the components covered in each session. Sessions were audiotaped and reviewed by the project co‐ordinator. As a result of these procedures, treatment integrity was excellent and was consistent with the written manuals |
|
| Outcomes |
Behaviour Scale: Child Behavior Checklist (134‐item) Rater: parent Anxiety Scale: Revised Children’s Manifest Anxiety Scale (37‐item) Rater: child Depression Scale: Children’s Depression Inventory (27‐item) Rater: child When Post therapy and at 1‐ and 2‐year follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Groups (stratified for age and gender) were randomly assigned to the treatment or comparison condition by a random number table |
| Allocation concealment (selection bias) | Low risk | Therapists and other staff were blind to the random assignment schedule and were not informed of the condition of the group they would be running until all children were referred |
| Blinding of participants (performance bias | Unclear risk | Participants could not be blinded, but both groups received a psychological therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessment could not be blinded, as all measures were self reported or parent reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up was high (48%), and only results for those completing were reported |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Betancourt 2014.
| Methods | Randomised trial of a group psychosocial Intervention vs wait list control for war‐affected youth | |
| Participants |
Included (n = 436) Multi‐symptomatic war‐affected youth 15 to 24 years of age recruited through outreach centres and by referral from workers at youth‐serving agencies, religious leaders and community elders; wanted to continue education; psychological distress and impairment in daily functioning. Mean age 18 years. Female: 199. Type of trauma: separated from caregiver as the result of war 237: 54%; friend/family member died because of war: 219 (50%); exposure to armed conflict: 73 (17%); member of armed forces: 23 (5%). Mean UCLA PTSD‐RI: treatment 0.68; control 0.77 Excluded Active suicidality or psychosis Setting Six community‐based sites, Sierra Leone, 2012 to 2013 |
|
| Interventions |
Youth Readiness Intervention (n = 222) Based on stabilisation and skills‐focused, including elements from CBT and interpersonal therapy, to address symptoms and impairments related to emotion dysregulation, risky behaviour and functional impairments, including interpersonal deficits. Core components included psychoeducation, self regulation and relaxation, cognitive restructuring, behavioural activation, communication and interpersonal skills and sequential problem solving. Ten group sessions (mean, 6.3) with an average of 9 participants per group Wait list control (n = 214) Length of wait list unclear; it appears that both groups were randomised to EducAid intervention at 3 months Therapists Four male and 4 female counsellors who had a bachelor’s degree or diploma in social work completed intensive 2‐week training and achieved a high level of competency in the YRI after training. A senior local mental health worker provided weekly supervision, and clinical psychologists provided weekly phone supervision |
|
| Outcomes |
PTSD symptoms Scale: UCLA PTSD‐RI Rater: child/adolescent Behaviour Scale: internalising and externalising items from the Oxford Measure of Psychosocial Adjustment (28‐item) Rater: child/adolescent Functional impairment Scale: functional impairment ‐ WHO Disability Adjustment Scale Rater: child/adolescent When Post treatment and at 6‐month follow‐up |
|
| Notes | After post‐treatment follow‐up, both groups were randomised to receive or not receive an educational intervention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified by gender and age; sequence generated in STATA |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants (performance bias | High risk | Wait list control |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | ‘assessors were blinded', but outcomes were child/adolescent‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Imputation data were used; loss to follow‐up at end of treatment was 9.6%; at 6 months, 14.9% |
| Selective reporting (reporting bias) | Unclear risk | All data were reported |
| Other bias | High risk | PTSD scores were 10% higher in control group at baseline |
Carbonell 1999.
| Methods | Randomised trial of a psychodrama group vs wait list | |
| Participants |
Included (n = 28) Girls who were referred to a large school‐based mental health programme at the beginning of sixth grade by their teachers or parents for trauma‐related problems. Girls were screened for at least 7 of 10 listed traumatic experiences. Ages: 11 to 13 years; Latinas 14/26 who completed the intervention, African American 11, Haitian 1 Excluded Not reported Setting Middle school in an urban neighbourhood identified as having a high rate of community violence, poverty and social problems, USA |
|
| Interventions |
Psychodrama group (n = 14) Psychodrama groups met for 20 weeks with the principal investigator. Groups covered 3 phases. The warm‐up phase introduced acting out feelings and learning to identify and share emotions. During the action phase, each child was helped to show or tell what had happened to him or her, and in the sharing phase, participants talked about their feelings during the action phase Wait list control (n = 14) The wait list control group could participate in an arts and crafts group over 20 weeks Therapists The therapist was a social worker 'well trained in psychodrama techniques and had extensive experience in group work and school‐based services' |
|
| Outcomes |
Behaviour Scale: Youth Self‐Report (112‐item): withdrawn, aggressive subscales Rater: child When Post therapy |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in the active or wait list group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessment could not be blinded, as the only measure was self reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data reported for completing participants; 18% loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Carrion 2013.
| Methods | Randomised trial of Stanford cue‐centred treatment vs wait list in children chronically exposed to violence | |
| Participants |
Included (n = 65) Individuals 8 to 17 years of age with a history of exposure to violence but no current exposure to perpetrators of violence and with a non‐abusing caretaker willing to participate. Mean age: 11.56 years. Female: 40%. Ethnicity: African American 50.7%, Hispanic/Latino 40.0%, Pacific Islander 1.5%, mixed ethnicity 7.7%. Type of trauma: All participants reported exposure to ≥ 2 traumatic events. The most common traumas were separation/loss (75.0%), witnessing violence (61.5%), homicide (51.9%), physical abuse (25.0%) and bullying (25.0%). Mean PTSD‐RI scores were 22.70 in the treatment group and 25.80 in the wait list group Excluded Significant medical illness, diagnosis of autism or schizophrenia, history of mental retardation or IQ < 70, substance dependency, lack of proficiency in English Setting 13 urban low‐income schools, USA, 2009 to 11 |
|
| Interventions |
Stanford cue‐centred treatment (n = 38) The primary goal is to empower the child through knowledge of trauma exposure and current affective, cognitive, behavioural or physiological responses. Children and parents learn about how adaptive responses become maladaptive, how to cope with rather than avoid ongoing stress and the importance of verbalising their life experiences. Also included skills training in how to reduce physical symptoms of anxiety, modify cognitive distortions and facilitate emotional expression. The manual also contained pictorial representations to assist the youth with understanding concepts. Therapy was delivered in 15 weekly individual sessions of approximately 50 minutes Two licensed therapists (PhD and MFT) with experience in the treatment of childhood trauma were trained in the cue‐centred treatment protocol over 3 months. Therapists received weekly supervision on the manual, phone consultation and case conferences. Fidelity to the treatment protocol in 25% of randomly selected audiotapes of sessions was assessed by 2 independent research assistants, who rated it as 91.2% Wait list (n = 27) Received cue‐centred treatment 3 months after randomisation |
|
| Outcomes |
PTSD symptoms Scale: UCLA PTSD‐RI for DSM‐IV (48‐item) Rater: child/adolescent Scale: UCLA PTSD‐RI for DSM‐IV (48‐item) Rater: parent Depression Scale: CDI (27‐item) Rater: child/adolescent Anxiety Scale: RCMAS (37‐item) Rater: child/adolescent When Post treatment |
|
| Notes | Because loss to follow‐up was greater than 55% overall, only loss to follow‐up data are used in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants (performance bias | High risk | Wait list control |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Self report measures used |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 55.4% lost to follow‐up (63% treatment and 44.4% wait list) |
| Selective reporting (reporting bias) | Low risk | Protocol was not identified, but major measures were reported |
| Other bias | Low risk | No other biases were identified |
Celano 1996.
| Methods | Randomised trial of Recovering from Abuse Program vs supportive therapy | |
| Participants |
Included (n = 47) Girls 8 to 13 years of age who had experienced sexual abuse within the previous 3 years and had received no previous treatment and their non‐offending female caretaker. Mean age: 10.5 years; African American 75%, Caucasian 22%, Hispanic 3%. Abuse was substantiated by child protection authorities and had been disclosed within 1 to 26 months Excluded Children and/or female caretakers with mental retardation, psychosis or drug addiction Setting Outpatient Child Psychiatry clinic, USA |
|
| Interventions |
Recovering From Abuse Program (RAP) (n = 25) A structured programme over 8 weekly 1‐hour sessions that used developmentally appropriate cognitive‐behavioural and metaphoric techniques. Issues covered were blame and stigmatisation, feelings of betrayal, traumatic sexualisation, feelings of powerlessness and anxiety and assertiveness skills. Two or 3 sessions were joint sessions with child and caretaker; remaining sessions were split individually between child and caretaker Supportive therapy (n = 22) Eight weekly 1‐hour sessions, primarily covering support education and discussion of child's symptoms, feelings and thoughts. Topics most frequently discussed with children in TAU were abuse‐related symptoms/feelings, other family issues, school issues, mother‐child communication, peer relationships and self esteem issues. Two or 3 sessions were joint sessions with child and caretaker; remaining sessions were split individually between child and caretaker Therapists Therapists for both interventions were 18 female psychiatrists, psychologists, social workers, nurses and trainees in psychiatry and psychology with prior education and experience in psychotherapy with children. RAP therapists participated in a 3‐hour training session and received weekly supervision in the manualised programme. Trainees providing TAU received 7 weekly supervision sessions highlighting clinical issues relevant to child sexual abuse. Professional clinicians participated in monthly group supervision sessions |
|
| Outcomes |
PTSD symptoms Scale: Revised Children's Impact of Traumatic Events Scale (CITES‐R; 77‐item): symptom subscale Rater: child Behaviour Scale: Child Behavior Checklist (CBCL): internalising, externalising Rater: parent Function Scale: Children's Global Assessment Scale (C‐GAS) Rater: psychiatrist When Post therapy |
|
| Notes | CBCL PTSD subscale scores were also reported, but because these data were skewed, CITES‐R data were used Loss to follow‐up was greater than 40% in the therapy group post therapy for the outcome of function |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Participants could not be blinded, but both groups received a psychological therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessment of the C‐GAS was blinded, but the other 2 measures were self reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completer analysis reported. Loss to follow‐up: 32% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Chapman 2001.
| Methods | Randomised trial of Chapman art therapy vs standard hospital care | |
| Participants |
Included (n = 58) Children 7 to 17 years of age admitted for ≥ 24 hours to a level 1 trauma centre and scoring ≥ 12 on the PTSD‐I Scale. Mean age: 10.7 years. Female: 29%, Ethnicity: white 35%, black 29%, Asian 24%, Hispanic 12% Excluded Children with burns, head injuries or injuries resulting from child abuse; non‐English‐speaking children or caregivers Setting: level 1 trauma centre at a large urban hospital, USA |
|
| Interventions |
Chapman art therapy (n = 31) A brief, trauma resolution method of approximately 1 hour designed to provide an opportunity for the child to sequentially relate and cognitively comprehend his or her medical trauma in a 1‐to‐1 session at the child's bedside Standard hospital care (n = 27) Therapists One of 2 art therapists |
|
| Outcomes |
PTSD symptoms Scale: UCLA PTSD Index Rater: child/adolescent and parent When At 1 week after injury and at 1 month and 6 months after discharge |
|
| Notes | No means or variance values were reported. The only data were shown graphically; it appears that only scores for avoidance were reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in the active or standard hospital care group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessment could not be blinded, as the only measure was self reported or parent reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up not reported |
| Selective reporting (reporting bias) | High risk | Only the subscore for PTSD avoidance was available. Six‐month follow‐up data were not reported |
| Other bias | Low risk | No other bias was apparent |
Chemtob 2002.
| Methods | Randomised trial of individual therapy vs group therapy or wait list | |
| Participants |
Included (n = 248) Children in grades 2 to 6 who met criteria for disaster exposure measured by a score at or above the 94th percentile for trauma symptom severity on the Kauai Recovery Index. Age: 6 to 12 years (mean, 8.2 years). Female: 61.4%. Hawaiian or part‐Hawaiian 30.1%; white 24.9%; Filipino 19.7%; Japanese 9.2%. 88% met DSM‐IV criteria for self reported PTSD Excluded Not reported Setting Ten elementary public schools on a Hawaiian island 2 years after a major hurricane, 1995 to 1996 |
|
| Interventions |
Individual therapy Therapists were provided a standard box of art and play materials, and therapy was guided by treatment manuals. The 4 weekly sessions covered safety and helplessness, loss, mobilising competence, issues of anger and ending and going forward. Themes were explored through a combination of play, expressive art and talk Group therapy As for individual therapy, except that co‐operative play and discussion were used in group sessions of 4 to 8 children Therapists Therapists were 3 school counsellors and 1 social worker experienced at working with children in schools who received 4 ½ days of training and 3 hours of supervision each week |
|
| Outcomes |
PTSD symptoms Scale: Kauai Recovery Index (24‐item) Rater: child When At 1 and 12 months |
|
| Notes | Sample numbers were not reported, and these data could not be obtained from study authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | SPSS used to generate randomisation sequence. Randomised to 1 of 3 cohorts, then randomised to group or individual treatments |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they had been allocated to individual or group therapy or wait list |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessment could not be blinded, as the only measure was self reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up not clear |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Church 2012.
| Methods | Randomised trial of Emotional Freedom Technique vs no treatment | |
| Participants |
Included (n = 16) Males 12 to 17 years of age who were removed by court order to a residential facility because of physical, psychological or sexual abuse, parental abandonment or negligence and could understand the instructions on the Impact of Events Scale. Average age: 13.7 years. All participants scored in the moderate clinical range on the IES Total, with an average score of 34.2 Excluded Organic or neurological conditions, prior clinical psychiatric diagnoses, concurrent pharmacological treatment Setting Residential facility in Trujillo, Peru |
|
| Interventions |
Emotional Freedom Technique (n = 8) The Emotional Freedom Technique (EFT) is an exposure‐based therapy in which participants pair the memory of a highly traumatic event with a statement of self acceptance while tapping prescribed acupuncture points. The therapist asks the child to recall the most troubling specific incident of abuse as though it were a movie, give the movie a title and rate the level of distress associated with the trauma (subjective units of distress scale of 0 to 10). EFT was repeated until the distress level was at or near 0 over a single 1‐hour session Mean number of EFT was 2.47 (range, 2 to 4) Control (n = 8) No treatment Therapists Investigators providing therapy were trained with 'other psychologists in EFT'. Clinical supervisors monitored fidelity to the EFT manual |
|
| Outcomes |
Trauma symptoms Scale: Impact of Events Scale (15‐item) ‐ intrusion, avoidance, total Rater: child/adolescent When At 1 month |
|
| Notes | Data were not added to meta‐analyses because the effect sizes were several times higher than the overall estimate and contributed substantial heterogeneity | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in the active or no treatment group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | 'Data [were] scored, offsite and blind, by a biostatistician', but data were collected by a therapy supervisor and measures were self reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Only 1 outcome measure was reported |
| Other bias | Unclear risk | Potential differences between groups were not investigated |
Cohen 1996.
| Methods | Randomised trial of CBT vs supportive therapy | |
| Participants |
Included (n = 86) Preschool children who had been sexually abused, with the most recent episode of sexual abuse reported within the previous 6 months with minimal symptoms defined as a Weekly Behavior Report score > 7 or any sexually inappropriate behavior reported on the Child Sexual Behavior Inventory. Mean age: 4.7 years. Female: 58%. Caucasian 54%, African American 42%, other 4%. Trauma: 25% abused once, 26% abused 2 to 5 times Excluded Children with mental retardation, pervasive developmental disorder, psychotic symptoms or serious mental illness or in short‐term care (< 12 months), or parents with a psychotic disorder or current substance abuse Setting Children were referred to the Center for Traumatic Stress in Children and Adolescents, Pittsburgh, USA |
|
| Interventions |
Cognitive‐behavioural therapy for sexually abused preschool children (CBT‐SAP) (n = 39 completing treatment) A short‐term treatment model for sexually abused preschool children and their parents over 12 weekly sessions of 40 to 50 minutes with the child and 50 minutes with the parent. Specific issues addressed with the child were safety and assertiveness, ambivalence towards the perpetrator, behaviours, fears and anxiety. Interventions included cognitive reframing, thought stopping, positive imagery and contingency programmes. Issues addressed with parents included ambivalence to the perpetrator and their belief in the abuse, attributions, management of their fear and anxiety, their own history of abuse, feelings towards the child, legal issues and emotional support and behavioural management for the child Non‐directive supportive therapy (NST) (n = 28 completing treatment) Support from an understanding and concerned professional over 12 weekly sessions of 40 to 50 minutes with the child and 50 minutes with the parent designed to reduce isolation, loneliness, hopelessness and anxiety; improve understanding of their feelings; and validate these feelings. The therapist did not make interpretations or offer directive advice but could help identify alternatives through non‐directive suggestions Therapists Both therapists were master’s level clinicians who had worked with sexually abused children for several years. Two therapists were trained in both treatments before the study began. Detailed treatment manuals were provided for both therapies. Weekly individual supervision was provided. All treatment sessions were audiotaped, and scores for compliance with the treatment model were rated as greater than 90% |
|
| Outcomes |
Behaviour Scale: Child Behavior Checklist Rater: parent When Post therapy and at 6‐ and 12‐month follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Children and their parents were randomised by Efron's biased coin toss to ensure the 2 groups were balanced in terms of perpetrator, type of abuse, gender and age |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Participants could not be blinded, but both groups received a psychological therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessment could not be blinded, as all measures were self reported or parent reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Overall loss to follow‐up at the end of treatment was 22% and 50% at 6 and 12 months and was > 50% for the supportive therapy group at 6 and 12 months |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Cohen 2005.
| Methods | Randomised trial of sexual abuse‐specific CBT vs non‐directive supportive therapy | |
| Participants |
Included (n = 82) Females 8 to 15 years of age who had experienced validated contact sexual abuse by someone ≥ 5 years older within the previous 6 months, had significant symptoms related to the abuse and had a non‐offending parent or primary caregiver able to participate in treatment. Participants were referred from a variety of sources. Mean age: 11 years. Female: 69%. Caucasian 60%, African American 37%, bi‐racial 2%, Hispanic 1%. Trauma exposure: 54% of participants experienced anal and/or vaginal intercourse, 33% were abused more than 10 times, and, for most, the abuse was accompanied by use of threatened or actual force Excluded Children with mental retardation, pervasive developmental disorder, active psychosis or substance abuse or serious medical illness, or whose caretaker was not long‐term (≥ 12 months) or had active psychosis or substance abuse Settting Urban outpatient child psychiatric programme specialising in the treatment of traumatic stress in children, USA |
|
| Interventions |
Sexual abuse‐specific CBT (n = 41) CBT methods with the child focused on depression, anxiety and behavioural difficulties and with the parent focused on parental emotional distress, enhanced support for the child and management of behavioural difficulties. Major components for the child included identification of feelings, stress inoculation techniques, gradual exposure exercises, cognitive processing of the abuse, education about healthy sexuality and safety skill building. Parental components paralleled those for the child, with the addition of building parenting management skills. Each of the 12 weekly sessions consisted of 45 minutes with the child and 45 minutes with the parent Non‐directive supportive therapy (n = 41) Therapists did not provide specific suggestions or directive advice but encouraged exploration of alternative attributions, behaviours and feelings. Issues were addressed as they were raised by child or parent. Interventions provided a high degree of non‐judgmental empathy and support; encouraged identification, clarification and acceptance of upsetting feelings; and re‐established trust and positive interpersonal expectations. Each of the 12 weekly sessions consisted of 45 minutes with the child and 45 minutes with the parent Both therapies Appropriate referrals to non‐therapeutic ancillary care were made when indicated, and mothers in either group with a DSM‐III‐R diagnosis were also offered a referral for individual therapy Therapists Both therapists had received a master's level degree in clinical social work and were trained and experienced in both models. Halfway through the programme, therapists swapped to the other treatment model. Both therapies were manualised. Therapists received weekly supervision, and sessions were audiotaped and audited weekly to ensure adherence, which was rated at > 90% |
|
| Outcomes |
Trauma‐related symptoms Scale:Trauma Symptom Checklist for Children (54‐item) Rater: child/adolescent Depression Scale: Children’s Depression Inventory (27‐item) Rater: child/adolescent Anxiety Scale: State‐Trait Anxiety Inventory for Children TSCC Rater: child/adolescent Behaviour Scale: Child Behavior Checklist Rater: parent When Post therapy and at 6‐ and 12‐month follow‐up |
|
| Notes | Because loss to follow‐up was greater than 54% in the supportive therapy group, only loss to follow‐up data were used in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number series generated by computer |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Participants could not be blinded, but both groups received a psychological therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessment could not be blinded, as all measures were child reported or parent reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Last observation carried forward was used to account for missing data, but loss to follow‐up was greater than 54% for the NST group at all intervals and was high overall: post therapy 40%, 6 months 44%, 12 months 52% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Cohen 2011.
| Methods | Randomised trial of trauma‐focused CBT vs child‐centred therapy | |
| Participants |
Included (n = 124) Children of mothers attending a community women’s health service in the United States, 7 to 14 years of age with ≥ 5 interpersonal violence (IPV)‐related PTSD symptoms, including ≥ 1 symptom from each of the 3 clusters, who were fluent in English and had an English‐speaking mother who was a direct victim of IPV. Mean age: 9.64 years. Female: 63. Ethnicity: white 69, black 41, bi‐racial 14. Only 14.5% no longer had contact with the perpetrator Excluded Significant development disorder, IQ < 80, serious psychotic symptoms in parent or child, living in an IPV shelter Settting Community women's centre for victims of interpersonal violence, Pittsburgh, USA, 2004 to 2009 |
|
| Interventions |
Trauma‐focused CBT (n = 64) Develops a narrative of the child’s experiences, corrects maladaptive cognitions and includes mastery of trauma reminders. Treatment included psychoeducation about trauma, how to develop individualised relaxation skills, expression and modulation of upsetting feelings and development of cognitive coping skills. Some of the session time was given to joint child‐parent sessions in which the child was encouraged to discuss his or her IPV experience and safety plans. Child and parent each attended eight 45‐minute individual therapy sessions. The same therapist saw child and parent Child‐centred therapy (n = 60) Aimed at establishing an empowering and trusting relationship between therapist and client by encouraging the child and parent to direct the content of their own treatment. The therapist provided active listening, reflection, accurate empathy, encouragement to talk about feelings and belief in the client’s ability to develop positive coping strategies. Child and parent each attended eight 45‐minute individual therapy sessions. The same therapist saw child and parent Therapists Three master's‐level social workers providing child therapy at the Women’s Center and Shelter were trained in the TF‐CBT model and in distinctions between TF‐CBT and Child‐centred therapy models. Workers were supervised and adherence to therapy was checked, with a blinded rating of 25% of randomly selected sessions and ratings greater than 90%. A manual that differentiated the 2 therapies was also available |
|
| Outcomes |
PTSD symptoms Scale: Schedule for Affective Disorders and Schizophrenia for School Age Children ‐ Present and Lifetime version (K‐SADS‐PL) Scores: change from baseline in total scores and in avoidance, hyperarousal and re‐experiencing subscores Rater: Trained research co‐ordinators interviewed child and parent Scale: UCLA PTSD Reaction Index Rater: child Depression Scale: Children’s Depression Inventory Rater: child Anxiety Scale: Screen for Child Anxiety‐Related Emotional Disorders (SCARED) Rater: child Behaviour Scale: Child Behavior Checklist Rater: parent When Post therapy |
|
| Notes | K‐SADS‐PL data were used for PTSD symptoms | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment to treatment by computer‐generated random number series. However, 24 received the same treatment as the randomised sibling |
| Allocation concealment (selection bias) | Low risk | Randomisation lists were locked in therapists’ offices |
| Blinding of participants (performance bias | Unclear risk | Participants could not be blinded, but both groups received a psychological therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Two project co‐ordinators blinded to treatment assignment were trained in administration of the K‐SADS‐PL, but all other measures were child‐reported or parent report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Last observation carried forward was used to account for missing data, but loss to follow‐up was 40% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Cox 2010.
| Methods | Randomised trial of a Web‐based psychoeducation intervention vs no treatment | |
| Participants |
Included (n = 85) Children between 7 and 16 years of age recruited from paediatric surgical wards over 12 months, hospitalised overnight, who had acquired an accidental or unintentional injury including mild traumatic brain injury, with family Internet access. Mean age: 10.90 years. Female: 26. Type of injury: 41 falls, 13 sports, 12 MVA, 6 burns, 13 other. Mean injury severity score, 7 Excluded Parents' or child’s English was inadequate for completion of questionnaires, child had acquired a moderate to severe head injury, injury was the result of suspected intentional trauma Setting Children’s hospital in Queensland, Australia, 2007 |
|
| Interventions |
Web‐based intervention (n = 44) Consisted of a booklet for parents containing information regarding common child reactions, their likely time course and how parents can best assist their child’s emotional recovery, as well as a Website for children. Both aimed to normalise and relieve trauma reactions and incorporated practical tools based on cognitive‐behavioural and resiliency strategies including relaxation, coping skills, problem solving, identification of strengths and reflections on trauma Control group (n = 41) Assessed at each interval |
|
| Outcomes |
PTSD symptoms Scale: Trauma Symptom Checklist for Children‐A (TSCC‐A; 44‐item) Rater: child/adolescent Scale: Impact of Events Scale‐Revised (IES‐R; 22‐item): intrusion, avoidance and hyperarousal Rater: parent Depression Scale: TSCC‐A: depression Rater: child/adolescent Anxiety Scale: TSCC‐A: anxiety Rater: child/adolescent When Post intervention (4 to 6 weeks) and at 6 months post injury |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number generator in Microsoft Excel |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they had been allocated to treatment or no treatment groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessments could not be blinded, as all were self reported or parent reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Analysis was based on last observation carried forward, but loss to follow‐up was 34% post therapy and 31% at 6 months |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Damra 2014.
| Methods | Randomised trial of trauma‐focused CBT vs no treatment in children who had been physically abused | |
| Participants |
Included (n = 18) Physically abused children who were referred by local community organisations and other local child protection institutes. Mean age: 11.3 years. Female: 0. Types of trauma: All had undergone physical abuse (most within 4 to 6 months before therapy) and had clinical symptoms of PTSD and depression for ≥ 5 weeks before. treatment. Mean PTSS‐C: TF‐CBT 23.66, control 24.55 (moderate to severe range) Excluded Not stated Setting Child care unit at Institute for Family Health (Jordan 2012) |
|
| Interventions |
Trauma‐focused CBT (n = 9) Trauma‐related cognitions and feelings, along with skills training. Parents also received ‘Better Parenting Skills Education’. Ten sessions of 60 minutes (90 minutes for 2 Better Parenting sessions) for children and parents over 2 weeks Therapists Two qualified and accredited registered child counsellors who had previous experience working with abused children and had attended 6 days of TF‐CBT training. Counsellors were supervised for every session and via meetings or email. Sessions were directly monitored by the supervisor Control (n = 9) No treatment |
|
| Outcomes |
PTSD symptoms Scale: Post‐Traumatic Stress Symptoms in Children (PTSS‐C; 30‐item) Rater: child/adolescent Depression Scale: Children’s Depression Inventory (27‐item) Rater: child/adolescent When Post treatment and at 4‐month follow‐up |
|
| Notes | PTSD symptom data were not added to meta‐analyses because the effect sizes were several times higher than the overall estimate and contributed substantial heterogeneity | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants (performance bias | High risk | Control group appears to have been given no treatment |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Self report measures were used, and participants probably realised whether or not they were receiving treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Follow‐up appears to have been 100% |
| Selective reporting (reporting bias) | Unclear risk | Protocol not identified |
| Other bias | Unclear risk | Comparison between groups not explored |
Danielson 2012.
| Methods | Randomised trial of family therapy vs treatment as usual | |
| Participants |
Included (n = 30) Treatment‐seeking adolescents who could recollect ≥ 1 childhood unwanted/forced contact sexual abuse. Mean age: 14.8 years. Female: 88%. African American 46%, white 37.5%, Native American 4.2%, bi‐racial 8.3% and Hispanic 4%. Age at first/only abuse: 4 to 15 years. Mean time since most recent assault: 3.7 years; 23 reported other traumatic events Excluded Adolescents with mental retardation Setting Therapy was delivered through the outpatient clinic and by an outreach programme at an urban clinic specialising in treatment of trauma in the USA |
|
| Interventions |
Risk reduction through family therapy (RRFT) (n =15) RRFT was developed to reduce the risk of substance use, other high‐risk behaviours and trauma‐related psychopathology in adolescents who had experienced child sexual abuse. RRFT was built upon the principles and interventions applied in multi‐system therapy (MST) and trauma‐focused cognitive‐behavioural therapy (TF‐CBT). The protocol has 7 components: psychoeducation, coping, family communication, substance abuse, PTSD, healthy dating and sexual decision making and re‐victimisation risk reduction. Strategic family therapy is utilised to help the family define problems and work together to find solutions. Weekly sessions of 60 to 90 minutes with the therapist were held, with adolescents and caregivers individually and as a family. The order of and time spent on each component was determined by the needs of each youth and family. A mean of 23 sessions were completed Treatment as usual (TAU) (n =15) No single treatment emerged as consistently delivered across youth and families assigned to the TAU group. The mean number of sessions was 13 Therapists Participants in both groups were treated by clinical psychology graduate students completing a predoctoral internship. RRFT adherence was assessed by review of randomly selected audiotaped sessions (2 per client per month), weekly individual supervision by the treatment developer (a licenced clinical psychologist) and an RRFT adherence checklist completed by therapists immediately after completion of each session. TAU therapists were supervised by other licenced psychologists in the clinic |
|
| Outcomes |
Trauma symptoms Scale: UCLA PTSD Index Rater: adolescent, parent Depression Scale: CDI Rater: adolescent Behaviour Scale: Behavioral Assessment System for Children (BASC‐2) Rater: adolescent, parent When Post therapy and at 3‐ and 6‐month follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned by computerised block randomisation |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they had been allocated to treatment or no treatment groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessment could not be blinded, as all were self‐reported or parent report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Post therapy, 7% were lost to follow‐up, but imputed data appear to have been used, and none were lost to follow‐up at 3 months |
| Selective reporting (reporting bias) | Unclear risk | Parent‐rated BASC‐2 scores were not reported |
| Other bias | Low risk | No other bias was apparent |
Deblinger 1996.
| Methods | Randomised trial of CBT for child only, CBT for non‐offending mother only, CBT for non‐offending mother and child and standard community care | |
| Participants |
Included (n = 100) Children 7 to 13 years of age who had contact sexual abuse substantiated by the Division of Youth and Family Services or the prosecutor’s office with ≥ 3 symptoms of PTSD, including ≥ 1 avoidance or re‐experiencing symptom. Mean age: 9.8 years. Female: 83%. Caucasian 72%, African American 20%, Hispanic 6%, other 2%. Time since last abuse: ≤ 6 months 66%, 6 months to 2 years 16%, > 2 years 18% Excluded Children with severe developmental delay, psychosis, ongoing unsupervised contact with perpetrator, danger to self or others or mother unwilling to take part Setting Centre for Children's Support, USA |
|
| Interventions |
CBT therapies (child only n = 25, mother only n = 25, combined n = 25) Therapies with the child focused on coping skills training, gradual exposure and processing, education and prevention skills training. Parent therapy concentrated on education, coping, communication, modelling, gradual exposure and behaviour management skills. Individual treatment sessions were 12 weekly treatments of 45 minutes each and 90 minutes for the combined child and parent group Control group (n = 25) Participants were given information about their children’s symptom patterns and were strongly encouraged to seek therapy Therapists Mental health therapists were intensively trained in the CBT intervention, including 1 pilot case. Treatment was manualised, and therapists were supervised weekly and monitored for adherence/fidelity |
|
| Outcomes |
PTSD diagnosis Assessment: Schedule for Affective Disorders and Schizophrenia for School‐Aged Children (K‐SADS‐E) (DSM‐III‐R criteria) Rater: clinician PTSD symptoms Scale: K‐SADS‐E Rater: clinician Depression Scale: Child Depression Inventory (27‐item) Rater: child Anxiety Scale: State/Trait Anxiety Inventory for Children: state, trait (20‐item) Rater: child Behaviour Scale: Child Behavior Checklist: internalising, externalising (118 behaviour problem items) Rater: parent When Post therapy and at 3‐, 6‐, 12‐ and 24‐month follow‐up |
|
| Notes | Loss to follow‐up was greater than 40% in the control group for PTSD and behaviour at 3 and 12 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they had been allocated to treatment or no treatment groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Most measures were based on child or parent report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completer analysis reported, and follow‐up data reported only for those who were available at all 4 measurement intervals; loss to follow‐up 23% |
| Selective reporting (reporting bias) | Unclear risk | All outcomes were reported at all intervals, except anxiety and behaviour, which were reported only post therapy |
| Other bias | Low risk | No other bias was apparent |
Deblinger 2001.
| Methods | Randomised trial of a CBT group vs a supportive therapy group | |
| Participants |
Included (n = 44) Children 2 to 8 years of age referred to the Regional Child Abuse Diagnostic and Treatment Centre. All had credible disclosures of sexual abuse. Mean age: 5.45 years. Female: 27. Ethnicity: white 28, black 1, Hispanic 1, other 6 Excluded Children with, or children of parents with, psychotic disorders, severe developmental delay and/or behaviours that were dangerous to themselves or others Setting Regional Child Abuse Diagnostic and Treatment Centre, USA |
|
| Interventions |
CBT (21 completers) Therapy consisted of 11 weekly sessions of 1 hour and 45 minutes with children and parents individually and 15 minutes for a joint parent and child activity. Sessions utilised an interactive format and a workbook. Parent sessions assisted parents to cope with their emotions, so they could support their children, provide education about communication skills and teach behaviour management skills. The main objectives were to help children communicate and cope with their feelings, identify okay and not okay touches and learn abuse response skills. An additional 15 minutes was used for a combined mother/child activity Supportive therapy (23 completers) The main objectives of supportive therapy with children were the same as with the CBT group but used a didactic approach. Parent sessions were based on self help models and were less structured than CBT sessions for parents. Eleven weekly sessions of 1 hour and 45 minutes of counselling were provided for children and parents Both Therapists for both groups were checked for adherence and were supervised weekly |
|
| Outcomes |
PTSD symptoms Scale: Schedule for Affective Disorders and Schizophrenia for School‐Age Children ‐ Epidemiologic version (K‐SADS‐E) Rater: parent Behaviour Scale: Child Behavior Checklist Rater: parent When Post therapy and at 3‐month follow‐up |
|
| Notes | PTSD symptom scores were skewed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly determined by computer programme |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Both groups received a psychological therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Both measures were based on parent report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data were reported for completing participants, and loss to follow‐up was 30% at all intervals |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Deblinger 2011.
| Methods | Randomised trial of trauma narrative therapy + trauma‐focused CBT vs trauma‐focused CBT | |
| Participants |
Included (n = 210) Children 4 to 11 years of age referred for verified contact sexual abuse with ≥ 5 PTSD symptoms, including 1 from each cluster. Mean age: 7.7 years. Female: 96/158 at follow‐up. Caucasian 103, African American 22, Hispanic 11, other 22 Excluded Children with an IQ < 70, with continued unsupervised face‐to‐face contact with perpetrator or with parent who had a serious medical or mental health illness that would impact participation Setting New Jersey and Pennsylvania, USA |
|
| Interventions |
Trauma‐focused narrative therapy + CBT (n = 104) As for CBT + children, were encouraged to develop a detailed trauma narrative about the sexual abuse, which they processed and reviewed with the caregiver and therapist Trauma‐focused CBT (n = 106) Included psychoeducation and parenting, relaxation, affective modulation, cognitive coping, in vivo exposure, enhanced safety and future development, delivered as 8 or 16 weekly conjoint parent/child sessions of 90 minutes each. Mean number of sessions attended: 7.36 and 13.92, respectively Therapists Therapists had graduate degrees in psychology, clinical social work or a related field with ≥ 3 years of clinical experience. They were supervised weekly, and adherence to inclusion or non‐inclusion of trauma narrative was checked |
|
| Outcomes |
PTSD symptoms Scale: Schedule for Affective Disorders and Schizophrenia for School‐Age Children ‐ Present and Lifetime version (K‐SADS‐PL) Rater: clinician administered individually to child and parent Depression Scale: Children's Depression Inventory (27‐item) Rater: child Anxiety Scale: Multidimensional Anxiety Scale for Children (39‐item) Rater: child Behaviour Scale: Child Behavior Checklist (120‐item) Rater: parent rating When Post therapy and at 6‐ and 12‐month follow‐up |
|
| Notes | Data for 8‐ and 16‐week groups were pooled | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Children were randomised to groups, but 17 siblings were allocated to the same intervention as the first randomised sibling |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Both groups were given a psychological therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | 'The project coordinator who was blind to assignment conducted assessments'; however, most scales were child‐reported or parent report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ITT analysis was used, but follow‐up means and SDs were reported. Loss to follow‐up: 25% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Diehle 2014.
| Methods | Parallel RCT of trauma‐focused CBT vs EMDR in children and adolescents recruited from a trauma centre | |
| Participants |
Included (n = 48) Between 8 and 18 years of age; command of the Dutch language; exposure to ≥ 1 single traumatic event; last traumatic event occurred ≥ 4 weeks before the first measurement; partial or full PTSD. Mean age: 13 years. Female: 30. Majority were Dutch (77%): 46% with Dutch mothers and 33% with Dutch fathers. Types of trauma: accidents 23%, sexual assaults 17%, threats (with weapon) 13%, kidnapping 10%, serious illness 7%, other 30%. Exposure to domestic violence 44%, sexual assault 39%, multiple‐event trauma 17%. Seven children in the TF‐CBT condition were diagnosed with PTSD on the ADIS‐P: 6 fulfilled a partial diagnosis and 4 had no PTSD. EMDR condition: 9 children in the EMDR group fulfilled a PTSD diagnosis, 5 fulfilled a partial diagnosis and 1 had no diagnosis (Note: This accounts for only 32 participants) Excluded Children showing clinical signs of psychotic disorder, substance use disorder, pervasive developmental disorder (e.g. autism) or acute suicidality Setting Department of Child and Adolescent Psychiatry Trauma Centre, The Netherlands, 2009 to 2012 |
|
| Interventions |
Trauma‐focused CBT (n = 23) The following components were included in this programme: psychoeducation, relaxation, affective expression and regulation, cognitive coping, gradual exposure through creation of child’s trauma narrative, parent management skills, conjoint child/parent session, enhanced future safety and development. Children worked on their trauma narrative in sessions 4, 5 and 6 and shared the narrative with their parents in session 7 Parents were invited to also join sessions 1, 2, 3 and 8 or spent 15 minutes of a session alone with the therapist Therapy was delivered over 8 weekly sessions of 60 minutes but could be terminated earlier if all modules were administered, the child’s score on the CRIES‐13 was < 10 and the child and parent agreed EMDR (n = 25) The main components of this protocol include the following: psychoeducation about the trauma and therapy, preparation of the target memory, desensitisation of the memory, identification and processing of body sensations, re‐evaluation of the target. Desensitisation of the memory started in session 3 and was pursued until session 7. Children were asked to keep the target image in mind while simultaneously concentrating on the distracting stimulus (typically following the finger of the therapist). After episodes of 30 minutes, the child was asked to report what he or she had just experienced. This was repeatedly done until the target did not induce distress in the child. Parents were invited to join 15 minutes of each session, or to spend this time alone with the therapist. Therapy was delivered over 8 weekly sessions of 60 minutes Therapists Eight experienced CBT therapists were trained in both TF‐CBT and EMDR before the study. Four were EMDR practitioners, and 2 had competed advanced training. Supervision was provided weekly by an expert on EMDR for children and experts on TF‐CBT. Therapists filled out protocol‐specific checklists and recorded each session on video. A random selection of 25% of all videos was evaluated by therapists for treatment integrity (not clear which therapists). Treatment integrity was scored as 75% for EMDR and 73% for TF‐CBT |
|
| Outcomes |
PTSD diagnosis Scale: ADIS‐P PTSD (47‐item) Rater: parent PTSD symptoms Scale: improvement on CAPS‐CA Rater: clinician Scale: CRIES‐13 Rater: child/adolescent Behaviour Scale: SDQ domains Rater: parent Anxiety Scale: Revised Child Anxiety and Depression Scale Rater: child/adolescent and parent When Post treatment |
|
| Notes |
Starting date: 1 June 2009 Completion date: proposed completion December 2009 Contact information: Dr. R.J.L. Lindauer Academic Medical Center (AMC), Medical Research B.V. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “A methodologist prepared the randomization list” |
| Allocation concealment (selection bias) | Low risk | "The researcher managing the randomization list directly communicated the assigned condition to the therapist” |
| Blinding of participants (performance bias | Low risk | Participants were not blinded, but both groups received therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “Assessors were blinded to the allocated treatment condition of the children” |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | “Multiple imputation” was used; overall loss to follow‐up was 25%, but 68% were lost to follow‐up for measures other than PTSD symptoms in the EMDR group |
| Selective reporting (reporting bias) | Unclear risk | CRIES‐13 scores not reported |
| Other bias | Low risk | No other biases were identified |
Dominguez 2001.
| Methods | Randomised trial of CBT or supportive therapy | |
| Participants |
Included (n = 32) Sexually abused children and adolescents 6 to 17 years of age referred to a Victims' Resource Institute. Mean age: 10 years. Female: 19. Caucasian 48%, Hispanic 40%, African American 8%, other 4% Excluded Children and adolescents with mental retardation, brain damage, psychotic or autistic behaviour, learning disabilities, perpetrators of violence or gang members, substance abusers and conduct‐disordered children Setting University of Houston, USA |
|
| Interventions |
CBT (n = 22) Participants were taught to normalise their responses and skills to manage their affective, cognitive and behavioural responses to the traumatic event, and to identify and address deficits in interpersonal function. Therapy was based on 20 weekly sessions but could vary depending on participant need Supportive therapy (n = 10) The goal of therapy was to identify and encourage the participant's use of existing coping behaviours and to reflect on and validate their experiences and emotional reactions. A central component was the therapeutic relationship based on genuineness, unconditional positive regard for the participant and accurate empathic understanding. Therapy was based on 20 weekly sessions but could vary depending on need Therapists Therapists were 10 'upper level' graduate students in clinical psychology supervised weekly by PhD‐level clinical psychologists. Both therapies were manualised and all progress notes checked for use of CBT elements in CBT group and non‐use of CBT in supportive therapy group. CBT elements were used in 86% of CBT sessions and in 57% of supportive therapy sessions |
|
| Outcomes |
PTSD symptoms Scale: Impact of Event Scale‐Revised: avoidance and intrusion (15‐item) Rater: clinician Depression Scale: Children's Depression Inventory (27‐item) Rater: clinician When Every second week during treatment |
|
| Notes | Only slope and intercept of outcome growth curves were reported. No significant differences were noted between the 2 treatments | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Participants could not be blinded, but all participants received a psychological therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Clinician‐rated outcomes were used, but blinding of assessment was not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completer analysis reported. Loss to follow‐up: 22% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Farkas 2010.
| Methods | Randomised trial of motivation‐adaptive skills‐trauma resolution + EMDR vs wait list | |
| Participants |
Included (n = 65) Traumatised adolescents with conduct problems in Youth Protective Services reporting traumatic events with high impact on the Lifetime Incidence of Traumatic Events questionnaire. Participants were French‐speaking and 13 to 17 years of age; 25 were female. Participants were exposed to a mean 4.4 types of trauma Excluded Adolescents with psychosis, suicidal or mentally retarded Setting Youth Protective Services in Quebec, Canada, 2005 to 2006 |
|
| Interventions |
Motivation ‐ Adaptive Skills ‐ Trauma Resolution (MASTR) + EMDR (n = 33) Consisted of 12 weekly individual sessions. Sessions 1 to 4 aimed to establish rapport, assess history, identify goals, visualise a positive future and develop a case formulation and treatment plan. Sessions 5 to 8 covered self management skills, avoidance of high‐risk situations and imaginal rehearsal of behavioural choices. Sessions 9 to 12 were devoted to trauma resolution by EMDR. A manualised EMDR protocol with minor age‐appropriate modifications was used. Participants in the MASTR‐EMDR group continued to receive other types of therapy. Participants attended a mean 11 sessions over 8 months Wait list control (n = 32) Among the wait list group, 57% received another form of therapy and attended a mean 17 sessions over 8 months Therapists EMDR was provided by 2 licenced master's‐level therapists who together had 30 years of experience working with youth, had completed EMDR training and received ongoing supervision from the developer of MASTR. Treatment fidelity (of a random selection of 30% of sessions) was assessed as 94% |
|
| Outcomes |
PTSD diagnosis Scale: Diagnostic Interview Schedule for Children Rater: not clear, appear to have been research assistants PTSD symptoms Scale: Trauma Symptom Checklist for Children (TSCC; 54‐item) Rater: adolescent Anxiety Scale: TSCC Rater: adolescent Depression Scale: Child Behavior Checklist (118‐item) Rater: parent When Post therapy and at 3 months |
|
| Notes | Although participants in the MASTR‐EMDR group continued to receive other types of therapy, this was not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in the wait list or therapy group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Research assistants were not 'consistently blind to the treatment condition', and measures were self reported or parent reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only data available for the 40 participants assessed post treatment and at 3 months follow‐up were reported (loss to follow‐up: EMDR 42%, control 34%) |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | High risk | Twice as many males (48% vs 26%) were included; more came from low‐income families in the control group (75% vs 41%). Nearly twice as many had received a diagnosis of PTSD (37% vs 19%), and PTSD symptoms were greater (6.4 vs 3.7) in the treatment group |
Glodich 2000.
| Methods | Randomised trial of psychoeducation vs wait list | |
| Participants |
Included (n = 50) High school students 14 to 18 years of age who had experienced and/or witnessed violent events that were significantly stressful and/or traumatic. Mean age: 16.1 years. Female: 30. Caucasian 20, Hispanic 10, African American 8. Overall trauma exposure scores for traumatic violence and physical or verbal abuse were moderate but for indirect violence were high Excluded Students in the behavioural disorders class, those with ≥ 5 absences in a semester, those who could not behave appropriately (angry, anxious or impulsive) during the initial interview Setting High school in USA, 1998 |
|
| Interventions |
Group psychoeducation (n = 25) Group intervention was designed to provide education about the effects of trauma and violence and the connection of these effects to re‐enactment and risk‐taking behaviours. Key topics over the 8 weekly 70‐minute sessions were prevalence of violence and trauma, violence‐related trauma and PTSD, defences, avoiding further trauma and violence, re‐exposure, re‐enactment, combating helplessness and the role of family in combating helplessness Wait list control (n = 25) Therapists It was not reported whether the protocol was manualised, whether supervision occurred and whether fidelity/adherence was checked |
|
| Outcomes |
PTSD symptoms Scale: Impact of Event Scale‐Revised (22‐item) Rater: adolescent Behaviour Scale: Youth Self‐Report (112 behavioural items) Rater: adolescent When Post therapy |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Each student was assigned by a randomly generated number and was successively placed into 1 of 2 treatment groups or wait list |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Quite probable that participants were aware of whether they were in the wait list or therapy group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not reported, but measures were self reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Completer analysis reported; loss to follow‐up was 6% |
| Selective reporting (reporting bias) | Unclear risk | All outcomes appear to have been reported |
| Other bias | Unclear risk | Data from a student who joined the treatment group after randomisation were included |
Jaberghaderi 2004.
| Methods | Randomised trial of EMDR vs CBT | |
| Participants |
Included (n = 16) Sixth grade girls 12 to 13 years of age from an urban school in Iran who reported contact sexual abuse occurring ≥ 6 months previously Excluded Girls subjected to ongoing abuse Setting University clinic, Iran |
|
| Interventions |
CBT (n = 8) Sessions focused on skill development and exposure and were limited to 45 minutes, with a maximum 12 and a minimum 10 sessions. Treatment was terminated earlier if the Subjective Units of Distress score was between 0 and 2 and abuse‐related anxiety symptoms were 25% or less. Homework followed all sessions (a total of 10 to 15 hours) and included checklists, drawings and listening to tapes of the exposure narrative. Parents attended a psychoeducation session within the first 2 weeks EMDR (n = 8) Focus on the identified trauma memory was not as strict as with the CBT group. The EMDR therapist was allowed to treat spontaneous trauma memories that arose during work with the index trauma but was not allowed to systematically work through all trauma memories. The maximum 12 sessions (with no minimum) were limited to 45 minutes each, but most lasted approximately 30 minutes. Homework was minimal and was limited to drawing a ‘safe place’ on 1 occasion. Treatment was terminated earlier if the Subjective Units of Distress score was 0 to 2 and positive self statements were 6 or 7 on a 7‐point scale related to the abuse. Parents attended a psychoeducation session within the first 2 weeks Therapists Each treatment was manualised. Therapists were clinical psychologists experienced in working with children and trained in the respective therapies |
|
| Outcomes |
PTSD symptoms Scale: Child Report of Post‐Traumatic Symptoms (26‐item) Rater: child Scale: Parent Report of Post‐Traumatic Symptoms (32‐item) Rater: parent When Post therapy |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by picking names out of a hat |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Blinding was not possible, but both groups received a psychological therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Child‐ and parent‐reported outcomes were used |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Completer analysis reported. Loss to follow‐up: 13% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Kazak 2004.
| Methods | Randomised trial of Surviving Cancer Competently Program or wait list | |
| Participants |
Included (n = 150) Adolescent survivors of childhood cancer 11 to 19 years of age who had completed treatment within the previous 1 to 10 years and their families. Female: 51%. Ethnicity: white 85%, black 9%, Hispanic 5%, Asian 1% Excluded Adolescents who had relapsed, had mental retardation, lacked fluency in English or lived more than 150 miles from the hospital Setting Children's Hospital, Philadelphia, USA |
|
| Interventions |
Surviving Cancer Competently Program (n = 76) A manualised family group programme integrating CBT and family therapy principles over 1 day. The 4 sessions covered 'How Cancer Has Affected Me and My Family', 'Coping Skills', 'Getting on With Life' and 'Family Health and Our Future' Wait list control (n = 74) Therapists Therapists included psychologists, nurses and social workers who were given 12 hours of training. Treatment adherence was assessed as 96% across sessions |
|
| Outcomes |
PTSD symptoms Scale: Impact of Events Scale ‐ Revised (22‐item) Rater: child/adolescent Scale: UCLA PTSD Reaction Index (20‐item) Rater: child/adolescent Anxiety Scale: Revised Children's Manifest Anxiety Scale (RCMAS; 37‐item) Rater: child/adolescent When At 3 to 5 months after therapy |
|
| Notes | Sample sizes for the RCMAS were not clear SDs were calculated from 95% CIs |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stratified randomisation by age group (11 to 14 and 15 to 18 years) and gender, but no other details given |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Quite probable participants were aware of whether they were in the wait list or therapy group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All measures were self reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Imputed values were given, but loss to follow‐up was 38% in the intervention group compared with 7% in the wait list control group; overall loss to follow‐up was 26% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Kemp 2010.
| Methods | Randomised trial of EMDR vs wait list | |
| Participants |
Included (n = 27) Children 6 to 12 years of age admitted to a hospital emergency department after a motor vehicle accident, and scoring ≥ 12 on the Child Post‐Traumatic Stress – Reaction Index, or with ≥ 2 DSM‐IV criteria for PTSD. Mean age: 8.93 years. Female: 12. Mean time since accident: 8.35 months Excluded Children taking psychotropic medication; those with a concurrent psychological condition, with history of sexual or physical abuse or neglect, with head injury with persistent associated neurological dysfunction or scoring < 12 on the Glasgow Coma Scale Setting Not reported, Australian study |
|
| Interventions |
EMDR (n = 14) Four 60‐minute sessions over 6 weeks included client history and assessment, engagement and orientation to EMDR, assessment of target traumatic memory and desensitisation, instillation, body scan and closure Wait list control (n = 13) Received EMDR after 6 weeks Therapist All sessions were delivered by the same doctoral level psychologist, who had received advanced EMDR training. Fidelity was rated as acceptable to highly acceptable by an experienced child clinical psychologist with advanced EMDR training |
|
| Outcomes |
PTSD symptoms Scale: Child Post‐Traumatic Stress ‐ Reaction Index Rater: child, parent Scale: Impact of Events Scale (IES) Rater: parent Anxiety Scale: State Trait Anxiety Inventory Rater: child Depression Scale: Children’s Depression Scale Rater: child Behavioural problems Scale: Child Behavior Checklist Rater: parent When Post therapy and at 3 and 12 months, but the wait list group received therapy after 6 weeks; therefore, only post‐treatment data can be used |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Quite probable participants were aware of whether they were in the therapy or wait list group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All measures were self reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up was 11% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | High risk | More females were included (9 vs 3) and IES scores (34.64 vs 22.33) were significantly higher in the wait list group |
Layne 2008.
| Methods | Randomised trial of a classroom‐based psychoeducation and skills intervention with or without an additional trauma and grief component | |
| Participants |
Included (n = 159) War‐exposed adolescents in year 1 to 3 of high school who had undergone significant trauma exposure, reporting significant current distress and functional impairment. Mean age: 15.9 years. Females: 82. 73% had experienced a direct life threat Excluded Students with signs of psychosis, disruptive behavioural or substance abuse problems; those who represented a risk to themselves or others; those unable to participate in groups Setting Ten secondary schools in postwar central Bosnia, 2000 to 2001 |
|
| Interventions |
Trauma and grief‐focused component therapy + psychoeducation and skills intervention (n = 77) Included a trauma and grief‐focused group, which provided trauma and grief processing in addition to psychoeducation and skills intervention. Specific features of the intervention included psychoeducation about reactions to trauma; enhanced coping; trauma and grief processing; building of social support skills; enhanced problem solving; understanding of links between behaviour and trauma; and reappraisal of traumatic expectations. Groups of 6 to 10 participants met for 60 to 90 minutes over 17 to 20 weeks Psychoeducation and skills intervention (n = 82) Classroom intervention that included psychoeducation, skills for managing reminders of trauma and loss and other coping skills taken from selected modules of the trauma and grief component therapy for adolescents. Number of sessions not clear Therapists The 2 therapies were based on different modules of the manualised Trauma and Grief Focused Component Therapy. Treatment was implemented by 16 school counsellors, who received supervision every 2 to 4 weeks |
|
| Outcomes |
PTSD symptoms Scale: UCLA PTSD Reaction Index (17‐item) Rater: adolescents Depression Scale: Depression Self‐Rating Scale (18‐item) Rater: adolescents When Post therapy and at 4 months |
|
| Notes | Loss to follow‐up was greater than 40% for therapy and control groups at 4 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Counsellors at each school pulled the names of eligible students out of a box |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Participants were not blinded; both received a psychological therapy, and 1 was classroom‐based |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | All measures were self reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data were reported for completing participants, and risk was high to follow‐up at both intervals: post therapy 20%; 4 months 38% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Lieberman 2005.
| Methods | Randomised trial of child/parent psychotherapy or case management | |
| Participants |
Included (n = 75) Preschool children 3 to 5 years of age who had been exposed to marital violence but still were not living with the perpetrator. Mean age: 4.1 years. Female: 39. Ethnicity: mixed 38.7%, Latino 28%, African American 14.7%, white 9.3%, Asian 6.7%, other 2.6% Excluded Children with mental retardation or autism spectrum disorder, or who had mothers who had abused the child, had current substance abuse, were homeless or had mental retardation or psychosis Setting Appears to have been a general hospital in the USA |
|
| Interventions |
Child/parent psychotherapy (n = 42) Targeted maladaptive behaviours, supported appropriate interactions and guided child and mother in creating a joint narrative of traumatic events in weekly mother and child sessions of 60 minutes over 50 weeks. This was guided by child/parent interactions and the child's play with developmentally appropriate toys selected to elicit trauma play and to foster social interaction Case management (n = 33) Mothers received assessment feedback and information on mental health clinics and were connected to the clinic of their choice. They received a monthly call, usually of 30 minutes, from their case manager, whom they could also contact as needed. Face‐to‐face meetings were scheduled when indicated Therapists Psychotherapy clinicians had master's or PhD qualifications in clinical psychology, and treatment fidelity was monitored through weekly supervision. The case manager was an experienced PhD level clinician |
|
| Outcomes |
PTSD diagnosis Criteria: semi‐structured Interview for Diagnostic Classification Rater: clinician PTSD symptoms Scale: semi‐structured Interview for Diagnostic Classification Rater: clinician Behaviour Scale: Child Behavior Checklist Rater: parent When Post therapy and at 6 months |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in the active or control group |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Risk of bias for assessing PTSD seems low, as 'every effort was made to keep assessors blind to group assignment'; however, parents completing behavioural scores probably were aware of group assignment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completer analysis reported; although loss to follow‐up post therapy was moderate (13%), it was high at 6 months (33%) |
| Selective reporting (reporting bias) | Unclear risk | 6‐Month PTSD scores were not reported |
| Other bias | Low risk | No other bias was apparent |
McMullen 2013.
| Methods | Parallel single‐blind RCT of group‐based trauma‐focused CBT compared with wait list in former child soldiers and other war‐affected children in the Democratic Republic of Congo | |
| Participants |
Included: male former child soldiers and war‐affected 'street boys' 13 to 17 years of age, screened for symptoms of psychological distress in eastern Democratic Republic of Congo (n = 58) Excluded: those who psychosis, had not experienced traumatic war events, or were unable to speak Swahili, French or English |
|
| Interventions |
Trauma‐focused CBT (n = 25) 15 sessions of a manualised, culturally adapted, group‐based, trauma‐focused cognitive‐behavioural intervention that includes psychoeducation, relaxation, affect modulation, cognitive processing and construction of a trauma narrative Wait list control (n = 25) After treatment and post testing of the intervention group, wait list controls begin the intervention Therapists Delivered by the first and second authors and two experienced Congolese counsellors. Daily training and evaluation sessions were held with these facilitators to ensure fidelity. |
|
| Outcomes |
Trauma symptoms Scale: UCLA‐PTSD Revised Index Rater: adolescent Behaviour Scale: antisocial behaviour measured with the African Youth Psychosocial Assessment Rater: adolescent Combined anxiety‐depression subscale: Scale: antisocial behaviour measured with the African Youth Psychosocial Assessment Rater: adolescent When Post therapy and 3 months follow‐up |
|
| Notes | Data were not added to meta‐analyses because the effect sizes were several times higher than the overall estimate and contributed substantial heterogeneity | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were ranked on a list according to their UCLA‐PTSD RI Total score and then randomly allocated, by the first author, to either TF‐CBT intervention group or wait‐list control group using a matched dyad sequence from a computer randomisation program (www.random.org) generated by the third author (off site). |
| Allocation concealment (selection bias) | Unclear risk | No described |
| Blinding of participants (performance bias | High risk | Outcomes were self‐reported and participants are likely to have know they were in the intervention group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcomes were self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 3 month outcome data could not be reported because all participants in the control group were lost to follow up |
| Selective reporting (reporting bias) | Low risk | All outcomes listed in the protocol were reported |
| Other bias | Unclear risk | No other apparent biases |
O'Callaghan 2013.
| Methods | Randomised trial of trauma‐focused CBT + trauma narrative vs wait list | |
| Participants |
Included (n = 52) War‐affected girls 12 to 17 years of age who had witnessed or had personal experience of rape, sexual abuse or inappropriate sexual touch attending vocational training sponsored by World Vision. Mean age: 16.02 years. Mean number of traumatic events: 12 Excluded Intellectual disability, psychosis, severe emotional and behavioural problems that prevented group participation Setting Urban setting, Beni, Democratic Republic of Congo, 2006 to 2007 |
|
| Interventions |
Trauma‐focused CBT + trauma narrative (n = 24) Intervention group received a 15‐session, manualised, culturally modified TF‐CBT. It included the following modules: introduction, stress management, feelings, cognitive coping, trauma narratives, identification of and changes to inaccurate or unhelpful cognitions. All modules were group‐based, with the exception of trauma narratives, which were covered in 3 individual sessions. Intervention finished with a graduation ceremony also attended by parents/guardians, community leaders and other representatives. Sessions ran for 2 hours per day, 3 days per week for 5 weeks. Average attendance was 13.19 sessions Three caregiver sessions took place for parents/guardians of girls in the intervention group. Caregiver attendance ranged from 82% to 100% Wait list (n = 28) No details Therapists Intervention facilitators were social workers employed by World Vision. Daily pre‐therapy and post‐therapy meetings took place with facilitators and lead authors to ensure that module content was understood. The lead researcher monitored each session to ensure treatment integrity |
|
| Outcomes |
Trauma symptoms Scale: UCLA PTSD Reaction Index (22‐item) Rater: child/adolescent Depression/anxiety Scale: African Youth Psychological Assessment Instrument (40‐item) ‐ internalising and externalising Rater: child/adolescent Behaviour Scale: African Youth Psychological Assessment Instrument (40‐item) ‐ internalising and externalising Rater: child/adolescent When Post therapy |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were listed in order of their UCLA‐PTSD‐RI score, then were randomly assigned by a computer‐generated random sequence of numbers from the top of the list. The random sequence was supplied by an off‐site investigator |
| Allocation concealment (selection bias) | Low risk | 'Treatment allocation was concealed from those responsible for participant enrolment and ensuring that the person responsible for assigned participants had met none of the participants before the group allocation' |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in the active or control group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not stated, but self report measures were used |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up: 11.5% |
| Selective reporting (reporting bias) | Unclear risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other differences were identified |
O'Callaghan 2014.
| Methods | Parallel randomised double‐blind trial of trauma‐focused CBT vs control for children and adolescents affected by war | |
| Participants |
Included (n = 160) War‐affected children and young people 7 to 18 years of age who witnessed a violent event involving a direct threat to life, or at risk of abduction or attack by armed groups and able to attend a 3‐week intervention. Mean age: 13.42 years. Female: 72. Types of trauma: 81% had a family member killed in the conflict, 77% had a family member who had been abducted and 22% had themselves been abducted; 99% reported that they were in fear of attack by the Lord's Resistance Army. Mean score: 11.85 on the CRIES‐8; 26/159 had a score ≥ 17 on the CRIES‐8 Excluded Children and young people with psychosis, mental retardation, inability to understand Swahili, severe emotional and behavioural problems that made group participation impossible Setting Villages of Kiliwa and Li‐May in northeastern Democratic Republic of Congo, with combined population < 1000 in 2012 |
|
| Interventions |
"Chuo Cha Maisha" group‐based trauma‐focused CBT (n = 79) Included effective communication and conflict resolution and contributed to community, psychoeducation, relaxation training and mobile cinema screenings that modelled how abducted children can be welcomed back into the community. Effective parenting was also covered for parents. Participants and caregivers attended 8 gender‐based groups over 3 weeks. Session attendance was 88% for participants and 84% for caregivers Therapists Three male and 3 female local lay facilitators were given a copy of the intervention manual and met with the lead researcher for 3 hours beforehand to discuss preparations for the programme and needed modifications. Lead researcher provided on‐site supervision during sessions and ensured that each module was covered Wait list (n = 80) Received intervention after intervention group had completed the programme |
|
| Outcomes |
PTSD symptoms Scale: CRIES‐8 (8‐item) Behaviours ‐ internalising, externalising, conduct, prosocial Scale: African Youth Psychosocial Assessment Instrument (AYPA) Rater: child/adolescent and parent for conduct When Post treatment |
|
| Notes | NCT01509872 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated stratified random sequence run off‐site by 1 of the study authors |
| Allocation concealment (selection bias) | Low risk | Lead author allocated participants on the basis of randomised sequence |
| Blinding of participants (performance bias | High risk | Participants would have known whether or not they were receiving treatment |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | “assessed by blinded interviewers”, but PTSD symptoms were reported by participants and parents |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing values were replaced by using regression estimates; loss to follow‐up: 1.9% post treatment; 13.8% at 3 months; 3‐month control data were not reported |
| Selective reporting (reporting bias) | High risk | Daily function (Youth Daily Task Functioning Questionnaire), family function (an 8‐item family function questionnaire) and community function (AYPA) measures were also proposed in the protocol but were not reported |
| Other bias | High risk | Conduct scores (both self reported and parent reported) were approximately 17% higher in the intervention group |
Overbeek 2013.
| Methods | Multi‐centre cluster‐randomised controlled trial of a trauma‐focused psychoeducational intervention compared with supportive therapy in children exposed to interparental violence | |
| Participants |
Included (n = 164) Children 6 to 12 years of age who experienced psychological and/or physical interparental violence, who were referred to the programme by agencies such as the police and child protection agencies. Mean age: 9.22 years. Female: 44.5% (69). Mean length of abusive relationship: 10.87 years Excluded Children and parents with intellectual, psychiatric or behavioural problems that prevent participation in groups Setting Eight organisations in 7 cities in The Netherlands, 2009 to 2012 |
|
| Interventions |
En nu ik! (’It’s my turn now!’) (n = 108) Focused on how to differentiate and express emotions; increasing feelings of emotional security, learning how to cope with feelings and problems in a non‐violent way, developing a trauma narrative, improving parent/child interaction and psychoeducation, processing interparental violence experiences. Nine sessions of 90 minutes were provided for a maximum of 8 children, and 9 parallel sessions for the non‐violent custodial parent Therapists Therapists for parallel sessions usually included a mental health professional and a social worker who had received 1 day of training in the manualised intervention and participated in ≥ 3 peer supervision meetings. 69% of sessions were rated as having no or few deviations Jij hoort erbij ("You belong") (n = 56) Comparable with intervention on non‐specific factors by offering positive attention, positive expectations, recreation, distraction, warmth and empathy of the therapist, as well as social support among group participants. Also 9 sessions of 90 minutes for a maximum of 8 children, and 9 parallel sessions for the custodial parent Therapists Parallel sessions were provided by a mental health professional along with a mental health professional in training or a social worker. Therapists followed a manual for every session and participated in ≥ 3 peer supervision meetings. 78% of sessions were rated as having no or few deviations |
|
| Outcomes |
PTSD symptoms Scale: Trauma Symptom Checklist for Young Children (TSCYC; 90‐item) Rater: parent Scale: Trauma Symptom Checklist for Children (TSCC; 54‐item) Rater: children ≥ 7.5 years of age Behaviour Scale: CBCL (119‐item) Rater: parent Scale: Teacher Report Form (133‐item) Rater: teacher Depression Scale: CDI (27‐item) Rater: children ≥ 7.5 years of age When At 1 week and 6 months after completion of the programme |
|
| Notes | Netherlands Trial register: NTR 3064 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “An independent researcher will make the allocation schedule with a computerized random number generator”. Therapists were randomised in blocks of 3 (2:1 intervention:control) |
| Allocation concealment (selection bias) | Low risk | “Concealed random allocation” |
| Blinding of participants (performance bias | Low risk | Parents and children were blind to group allocation until 2 weeks before the start of the programme; both programmes were presented as useful |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | ‘The researchers coding the observation tasks and analyzing the data will be blind to the group condition of parents and children, as well as assessment’ |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The ‘last value carried forward will be applied’ for missing data. Loss to follow‐up: 20.1% |
| Selective reporting (reporting bias) | Unclear risk | All outcomes listed in protocol were reported |
| Other bias | Low risk | No other bias was identified |
Pace 2013.
| Methods | Randomised trial of cognitive‐based compassion training vs wait list | |
| Participants |
Included (n = 71) Adolescents in the Georgia foster care system with a documented history of trauma and neglect Mean age: 14.7 years. Female: 31. Ethnicity: African American 74%, Caucasian 13%, multi‐racial 7%, Asian 4%. Mean number of psychiatric diagnoses: 1.74. Trauma was neglect 40.20%, physical abuse 25.07%, sexual abuse 11.66% Excluded Adolescents taking medications known to influence immune and endocrine functioning, including corticosteroids and non‐steroidal anti‐inflammatory compounds; medical illness including cancer, cardiovascular disease, diabetes and autoimmune disorders, schizophrenia, bipolar I disorder, eating disorders and major depression severe enough to require hospitalisation Setting Georgia State foster care system, USA, 2010 |
|
| Interventions |
Cognitive‐based compassion training (n = 37) Participants in the cognitive‐based compassion training (CBCT) group attended classes of 1 hour twice a week for 6 weeks. CBCT is a secular, analytical meditation‐based programme derived from Tibetan Buddhist mind‐training. The goal of CBCT is to challenge unexamined assumptions regarding feelings and actions toward others, with a focus on generating spontaneous empathy and compassion for the self as well as others Wait list (n = 34) Control group was on a 6‐week wait list Therapists Not described |
|
| Outcomes |
Depression Scale: Quick Inventory of Depressive Symptomatology Rater: child/adolescent Anxiety Scale: State‐Trait Anxiety Inventory Rater: child/adolescent When Post therapy |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Participants were evenly randomized by a list of random numbers, generated by computer' |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in the active or control group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not stated, but self report measures were used |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: 22.5% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | High risk | Percentage of participants who had undergone sexual abuse was much higher in the intervention group than in the control group (18.52% vs 4.00%), and neglect was much higher in the control group (52.00% vs 29.63%) |
Qouta 2012.
| Methods | Cluster‐randomised trial of teaching recovery techniques vs wait list in 10‐ to 13‐year‐old boys and girls in heavily bombarded areas | |
| Participants |
Included (n = 482) Children in 5th and 6th grades from 2 randomly selected schools in heavily bombarded areas. Mean age: 11.29 years. Female: 49.4%. 86% lived in urban areas, 12% in refugee camps, 3% in villages; 49% had unemployed fathers. Clinically significant post‐traumatic stress symptoms: 64% intervention group, 43% control group Excluded Not stated Setting Schools in heavily bombarded areas in North Gaza and Gaza City, Palestine, after the Gaza War in 2008 to 2009 |
|
| Interventions |
Teaching Recovery Techniques (n = 242) The Teaching Recovery programme was modified to suit a war situation. It incorporated trauma‐related psychoeducation, CBT methods, coping skills training and creative‐expressive elements such as dream work and drawing. Problem solving, storytelling and role play techniques were also applied Four groups of 15 children were also attended by family members. Two weekly sessions of 2 hours over 4 weeks Four psychologists (2 male and 2 female) were trained in Teaching Recovery Techniques and had weekly preparatory and supervisory meetings with the primary author. Supervision covered case consultation, therapeutic elements, guidance through role playing and review of field diaries and sessions Wait list (n = 240) After 6 months, the control group was provided the same intervention for 1 month |
|
| Outcomes |
PTSD symptoms Scale: CRIES (13‐item) Rater: child/adolescent Depression Scale: Depression Self‐Rating Scale (18‐item) Rater: child/adolescent Behaviour Scale: SDQ Rater: child/adolescent When Post treatment and at 6‐month follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Four schools were randomly sampled from a Ministry of Education list. Two girls’ and two boys’ classes were randomly sampled at each of the 4 schools. Classes were randomly allocated (stratified by gender) to intervention and control groups |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants (performance bias | High risk | “Children, families, teachers, and research assistants were not aware of the intervention status of children at the baseline”, but it is likely they would have known whether they received treatment, once the study started |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcomes were self reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up between post treatment and 6 months: 16.2% |
| Selective reporting (reporting bias) | Low risk | Alll outcomes appear to have been reported |
| Other bias | High risk | Clinically significant symptoms were significantly greater in the intervention group (64% vs 43%) |
Raider 2008.
| Methods | Randomised trial of structured sensory therapy (SITCAP‐ART) vs wait list | |
| Participants |
Included (n = 23) Traumatised adjudicated adolescents in residential treatment. Two‐thirds of research participants were between 16 and 17 years of age, 9 of 20 who completed were female, 17 were white. Eleven had been diagnosed with PTSD, and 4 with traumatic or complicated grief Setting Multi‐county Attention Center, Ohio, USA |
|
| Interventions |
Structured Sensory Therapy (n =13) SITCAP‐ART is structured trauma treatment that uses a series of drawing tasks and treatment‐specific questions targeting the major sensations experienced in a traumatic event, so that traumatic memories are experienced at a sensory level and are reactivated in a safe environment to be moderated and tolerated with a sense of power and a feeling of safety. It consisted of 10 to 11 sessions of 1 hour and 15 minutes. Seven were group sessions with 6 participants. One session was held for individual debriefing, 1 for individual processing and 1 was a parent and adolescent session. Sessions covered identification of PTSD reactions; revisiting the trauma; normalisation of reactions; and helping parents respond to the child's reactions and resolve their own reactions Wait list (n = 10) Therapist The therapist completed a fidelity checklist for each session, which was rated as 98.5% overall |
|
| Outcomes |
Trauma symptoms Scale: Trauma Symptom Checklist for Children Rater: adolescent Behaviour Scale: Youth Self‐Report Rater: adolescent When Post therapy |
|
| Notes | Once they had received treatment, only pooled outcome data from the treatment group and the wait list group were reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably would have been aware of whether they were in the active or wait list group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All outcomes were self reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: 13% reported (p 176) but 5 reported to have dropped out in 'the early sessions of the group therapy' (22%; p 181) |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | High risk | Five additional participants were reported to have dropped out in 'the early sessions of the group therapy', but their data were not reported |
Salloum 2008.
| Methods | Randomised trial of individual vs group delivery of the Project LAST intervention | |
| Participants |
Included (n = 56) School children 7 to 12 years of age who were grieving ≥ 1 month after death or moderate PTSD symptoms (≥ 25 on the UCLA PTSD Index) due to death or related to Hurricane Katrina, and clinically appropriate for group participation. Female: 21. African American: 51. Thirty‐seven reported someone close to them had died, 14 had witnessed domestic violence, 12 witnessed a shooting or stabbing, 3 had experienced abuse. Eight children had received or were receiving mental health treatment Excluded Actively suicidal, loss within last month Setting School or after school programmes at 3 schools in New Orleans after Hurricane Katrina, January to May 2006 |
|
| Interventions |
Individual sessions (n = 28) Project LAST is a manualised intervention developed specifically for 7‐ to 12‐year‐olds experiencing grief and trauma due to death, disaster and/or violence. It has 3 overlapping phases: resilience and safety; restorative retelling; and reconnecting. It combines techniques from CBT and narrative therapy. Individual sessions were 1 hour each week over 10 weeks, and 1 parent session covered psychoeducation and support strategies Children attended a mean of 8.36 sessions Group sessions (n = 28) The Project LAST intervention was delivered through 9 weekly sessions for 5 to 6 children and 1 individual “pullout” session for the child. Children attended a mean of 7.82 sessions. Therapists All clinicians were master’s level social workers. To ensure fidelity, clinicians met with a consulting clinical social worker and the developer of the LAST intervention. Adherence for individual treatment was 98% and for the group intervention 100% |
|
| Outcomes |
PTSD diagnosis Scale: Score ≥ 38 on the UCLA PTSD Index Rater: child PTSD symptoms Scale: UCLA PTSD Index (22‐item) Rater: child Depression diagnosis Scale: Score ≥ 29 on the Mood and Feelings Questionnaire Rater: child Depression symptoms Scale: Mood and Feelings Questionnaire (33 items) Rater: child When Post therapy and at 3‐week follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Participants would have been aware of whether they were allocated to individual or group therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Observers were blinded, but all measures were self reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data were reported for those available at 3 weeks. Loss to follow‐up: 20% |
| Selective reporting (reporting bias) | Unclear risk | Clinically significant PTSD and depression were not reported by group, but symptom scores were given |
| Other bias | Low risk | No other bias was apparent |
Salloum 2012.
| Methods | Randomised trial of a grief and trauma intervention with and without narrative processing | |
| Participants |
Included (n = 72) Children who had experienced potentially traumatic events with a score ≥ 25 on the UCLA PTSD Index. Mean age: 9.6 years. Female: 31. All were African American. Sixty‐seven had been exposed to Hurricane Katrina. Most reported exposure to acts of violence including a beating (84.3%), a shooting (40%) or a dead body (31.4%), and 51.5% reported ≥ 3 exposures to violence Excluded Suicidal ideation, or not considered 'clinically appropriate' for group participation Setting Four elementary schools in New Orleans, after Hurricane Katrina, 2008 to 2009 |
|
| Interventions |
Grief and trauma intervention plus narrative processing (n = 37) This intervention was developed originally for children who had lost someone close through murder or had witnessed community violence. It combines techniques from CBT and narrative therapy over the 3 overlapping phases of resilience and safety; restorative retelling; and reconnecting. Children were instructed to share their stories, which were compiled in a book, with a caring adult. Therapy was delivered through 10 weekly group sessions and 1 individual session of 50 minutes to 1 hour plus a parent meeting that consisted predominantly of psychoeducation Grief and trauma intervention (n = 33) This was similar to the grief and trauma Intervention plus narrative processing, except that it did not include restorative storytelling or positive memories of the deceased. Children constructed a Coping Book, which they were instructed to share with a caring adult Therapists Therapists were 10 master's level social workers, 2 social work interns and 1 doctoral level psychologist. All received 3 days of training in the intervention they were using and were supervised twice a week. Fidelity checklists were completed after each session: 96% for the narrative intervention, 92% for grief and trauma |
|
| Outcomes |
PTSD diagnosis Scale: Score ≥ 38 on the UCLA PTSD Index Rater: child PTSD symptoms Scale: UCLA PTSD Index (22‐item) Rater: child Depression diagnosis Scale: Score ≥ 29 on the Mood and Feelings Questionnaire Rater: child Depression symptoms Scale: Mood and Feelings Questionnaire (33‐item) Rater: child Behaviour Scale: Child Behavior Checklist Rater: parent When Post therapy and at 3 and 12 months |
|
| Notes | Two Hispanic children, both of whom were randomised to the narrative processing group, were omitted from the final analysis, as all other participants were African American | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'using Excel randomization' |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Blinding not possible, but both groups received psychological therapies |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was stated that assessments were conducted by blinded personnel, but all measures were reported by child or parent |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Last observation carried forward analysis was used, but means and SDs were reported for those followed up at all intervals. Loss to follow‐up: 11% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Schottelkorb 2012.
| Methods | Randomised trial of trauma‐focused CBT vs child‐centred play therapy | |
| Participants |
Included (n = 31) Elementary school students 6 to 13 years of age who met full or partial criteria for PTSD on the UCLA PTSD Index, or had a clinical score on the Post‐Traumatic Symptoms Parent Report. Mean age: 9.16 years. Female: 45.5%. Their backgrounds covered 15 countries from Africa, Asia, Europe and the Middle East. Fifteen scored in the full PTSD range on the UCLA PTSD Index and Parent Report Excluded Children were excluded if they participated in counselling outside of this study Setting Three elementary schools in northwestern USA. All participating schools had more than average numbers of students who were English language learners |
|
| Interventions |
Trauma‐focused CBT (n = 17) Treatment was tailored to specific needs of refugee children, including information and education about trauma in general and refugee trauma in particular. Children participated in twice‐weekly 30‐minute sessions over 12 weeks, with an average of 17 completed sessions. Therapists met with parents twice on average Child‐centred play therapy (n = 14) Children attended 30‐minute sessions twice weekly for 12 weeks in the school. The playroom was additionally equipped with multi‐cultural dolls, musical instruments, play food and other toys reflective of the cultural backgrounds of the children. Children completed an average of 17 sessions, and therapists met with parents an average of 3 times Therapists All therapists were second‐ or third‐year graduate students in a master's level counsellor education programme. Face‐to‐face supervision of at least 1 hour was provided for every 10 hours of clinical work. All TF‐CBT therapists were trained and supervised by a doctoral level licenced professional counsellor, counsellor educator and certified TF‐CBT therapist. All CCPT therapists were trained and supervised by a doctoral level licenced professional counsellor, counsellor educator and registered play therapist supervisor. Supervisors for both therapies rated videotapes of each therapist's treatment sessions for adherence to treatment manuals; these were rated as excellent overall |
|
| Outcomes |
PTSD symptoms Scale: UCLA PTSD Index for DSM‐IV Rater: clinician PTSD symptoms Scale: Parent Report of Post‐Traumatic Symptoms (32‐item) Rater: parent When Post therapy |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Using a computer‐generated random numbers table' |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Blinding was not possible, but both groups received a psychological therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: 16% |
| Selective reporting (reporting bias) | Low risk | Al outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Shechtman 2010.
| Methods | Cluster‐randomised trial of group trauma therapy vs wait list | |
| Participants |
Included (n = 164) Elementary school students in Israel 9 to 14 years of age screened for post‐traumatic reactions with the Child Post‐Traumatic Stress Reaction Index (cutoff score 12). Female: 112 (68%). Most children were Jewish (82%), and all other participants were Arabic Excluded Not stated Setting Elementary and secondary schools in Israel, 2006 to 2007 |
|
| Interventions |
Group trauma therapy (n = 98) Treatment used activities and therapeutic games aimed at enhancing expression and exploration of feelings in a group context of mutual support over 10 sessions. Eighteen treatment groups were included: 5 for war‐related trauma, 7 for loss and divorce and 6 for mixed traumas Wait list (n = 66) Control children received treatment after the experimental group was terminated Therapists Therapists were 18 school counsellors who received training in the expressive‐supportive therapy modality over 56 hours and received group supervision . |
|
| Outcomes |
PTSD symptoms Scale: Child Post‐Traumatic Stress Reaction Index (20‐item) Rater: child/adolescent Anxiety Scale: Revised Children’s Manifest Anxiety Scale (37‐item) Rater: child/adolescent When Post therapy |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Cluster‐randomised by group, but how this was done was not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in the wait list control or active group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Observers were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: 17% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Shirk 2014.
| Methods | RCT of modified CBT vs usual care for referred adolescents with a depressive disorder and a history of interpersonal trauma | |
| Participants |
Included (n = 43) Adolescents referred for outpatient treatment who had been exposed to interpersonal trauma and met diagnostic criteria for a depressive disorder. Mean age: 15.48 years. Female: 36. Type of trauma: reported at least 1 incident of physical abuse (49%), witnessing family violence (58%), sexual abuse (67%) and verbal/emotional abuse (47%) in response to a highly structured screening interview. Diagnosis of PTSD: modified CBT group 30%, usual care group 61% Excluded Receiving concurrent psychological treatment for (1) depression, (2) attempted suicide within 3 months before intake, (3) engaged in self injurious behaviour that required hospitalisation or emergency room treatment within the previous 3 months, (4) met diagnostic criteria for bipolar disorder and/or substance dependence disorder, (5) presented with psychotic symptoms or intellectual deficit. None were receiving antidepressants Setting Two outpatient clinics of a large urban community mental health centre in an ethnically diverse urban city in the Rocky Mountains, USA |
|
| Interventions |
Modified CBT (n = 20) A CBT protocol for adolescent depression was modified to address cognitive deficits and distortions associated with interpersonal trauma. Core elements of the manualised therapy included mood monitoring, cognitive restructuring, relaxation training and interpersonal problem solving and mindfulness and explicitly addressed cognitions related to the experience of interpersonal trauma Therapy consisted of 12 weekly individual sessions, which were not time‐limited; however, the mean number of sessions attended was 5.33 Therapists Therapy was delivered by 1 male doctoral level psychologist with 28 years of clinical experience and 1 female master's level therapist with 10 years of experience. Therapists completed a 1‐day workshop and a practice case under supervision before the start of the trial Graduate‐level coders rated 86% of treatment elements delivered as specified in audio recordings of sessions Usual care (n = 23) Treatment strategies and procedures that therapists used regularly and believed to be effective for particular case formulations. Therapists described these as eclectic, although favouring client‐centred, psychodynamic and family approaches Usual care also consisted of weekly individual sessions, which were not time‐limited. The mean number of sessions attended was 6.22 Therapists Usual care therapists were 2 female doctoral level psychologists with 3 and 4 years of clinical experience. They were supervised by the clinic team leader; this included weekly group supervision and individual consultation on an as needed basis |
|
| Outcomes |
PTSD symptoms Scale: Disorders and Schizophrenia ‐ Present and Lifetime Version (K‐SADS‐LS) Rater: adolescent Depression Scale: Beck Depression Inventory (BDI‐II; 21‐item) Rater: adolescent Scale: K‐SADS‐LS (BDI‐II; 21‐item) Rater: adolescent Behaviour Scale: CBCL (118‐item) Rater: caregiver When BDI‐II was used during sessions 1, 4, 8 and 12 and at 16 weeks post treatment. K‐SADS‐PL and CBCL were rated post treatment |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Clinicians were assigned on the basis of clinic location, but randomisation was not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants (performance bias | Low risk | Both groups received individual therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | PTSD symptoms, behaviour and depression scales were completed by participants and caregivers |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Last observation carried forward (LOCF) was used for missing post‐treatment BDI‐II scores. Loss to follow‐up: 18.6% |
| Selective reporting (reporting bias) | High risk | Only BDI‐II depression scores for females were reported |
| Other bias | High risk | Percentage of participants with a baseline diagnosis of PTSD was twice as high (61%) in the control group as in the intervention group (30%). Therapists in the intervention group had 38 years of clinical experience between them as compared with 7 years in the usual care group. Also, intervention therapists received 'more targeted and frequent' case supervision |
Stallard 2006.
| Methods | Randomised trial of debriefing therapy vs control | |
| Participants |
Included (n = 158) Children and young people 7 to 18 years of age attending the A&E department after a road traffic accident. Mean age: 15 years. Female: 83 Excluded Children living outside the area, with significant learning disabilities, involved in > 1 incident Setting Hospital in the UK, 2000 to 2002 |
|
| Interventions |
Debriefing group (n = 82) A manualised series of standard prompts was used to guide the child through a structured debriefing process, including reconstruction of the accident in detail, helping the child identify thoughts about the trauma and discuss emotional reactions. Information was provided about common thoughts and feelings experienced by people who had undergone trauma as a way of normalising their reactions. Written information on coping with common problems was provided. The intervention was provided 4 weeks after the accident Control (n = 76) A series of prompt questions were used to engage the child in a discussion not focused on the accident Therapist Not reported |
|
| Outcomes |
PTSD diagnosis Scale: Clinician Administered Post‐Traumatic Stress Disorder Scale for Children Rater: clinician PTSD symptoms Scale: Impact of Events Scale Rater: child/adolescent Anxiety Scale: Revised Manifest Anxiety Scale Rater: child/adolescent Depression: Birleson Depression Inventory Rater: child/adolescent Behaviour Scale: Strengths and Difficulties Questionnaire (SDQ) Rater: child/adolescent and parent When At 8‐month follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised allocation stratified by gender |
| Allocation concealment (selection bias) | Low risk | Allocated by sequentially numbered sealed, opaque envelopes |
| Blinding of participants (performance bias | High risk | Participants may have been aware of whether they received an active treatment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for diagnosis, as "assessments were undertaken by a second researcher, who was blind to the child's status"; however, all other measures were self reported or parent reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completer analysis reported. Loss to follow‐up: 16% |
| Selective reporting (reporting bias) | Unclear risk | Data were not reported for parent SDQ |
| Other bias | High risk | Proportion of children diagnosed with PTSD at baseline was higher in the control group (35.5%) than in the experimental group (23.2%) |
Stein 2003.
| Methods | Randomised trial of a cognitive‐behavioural intervention for trauma vs wait list | |
| Participants |
Included (n = 126) Sixth grade students from 2 large middle schools who reported exposure to violence and had clinical symptoms of PTSD. Mean age: 11 years. Female: 56%. Mean number of violent events witnessed by students: 5.9 Excluded Children considered too disruptive to participate in group therapy Setting Two large middle schools in a socioeconomically disadvantaged, primarily Latino, area in the USA, 2001 to 2002 |
|
| Interventions |
Cognitive‐behavioural intervention for trauma in schools (n = 61) Consisted of 10 usually weekly sessions of 5 to 8 students per group delivered by psychiatric social workers. The intervention incorporated psychoeducation, exposure, relaxation training, games and worksheets and addressed symptoms of PTSD, depression and anxiety related to exposure to violence Wait list (n = 65) Students randomised to the wait list group completed the intervention 6 months after the intervention group had started Therapists Three psychiatric social workers working in mental health services who received 2 days of training in the manualised intervention with weekly supervision. Completion of required intervention elements in randomly selected audiotapes of sessions ranged from 67% to 100% |
|
| Outcomes |
PTSD symptoms Scale: Child PTSD Symptom Scale (17‐item) Rater: child Depression Scale: Child Depression Inventory minus suicidality item (26‐item) Rater: child Behaviour Scale: Teacher‐Child Rating Scale (6‐item) Rater: teacher Function Scale: Pediatric Symptom Checklist ‐ psychosocial dysfunction (33‐item) Rater: parent When At 2 weeks after treatment completion |
|
| Notes | SDs estimated from 95% CI of mean difference | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A central office was used for randomisation |
| Allocation concealment (selection bias) | Low risk | See sequence generation |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in the active or wait list group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Most outcomes were child reported or parent reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Completer analysis reported. Loss to follow‐up: 7% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
Taussig 2010.
| Methods | Stratified randomised trial of combined skills group training and individual mentoring vs control | |
| Participants |
Included (n = 156) Children 9 to 11 years of age who had been placed in foster care by court order because of maltreatment within the preceding year; currently resided within 35 minutes' drive to skills group sites; had lived with their current caregiver ≥ 3 weeks; demonstrated adequate proficiency in English Excluded None reported Setting Denver metropolitan area, 2002 to 2009 |
|
| Interventions |
Combined skills group training and individual mentoring (n = 77) Consisted of a manualised skills group and 30 weeks of 1‐on‐1 mentoring by graduate students in social work for each child. The skills group, which included 8 to 10 children and 2 facilitators, met for 1.5 hours over 30 weeks. Groups combined CBT skills with materials covering emotion recognition, perspective taking, problem solving, anger management, cultural identity, change and loss, healthy relationships, peer pressure, abuse prevention and future orientation. Mentors spent 2 to 4 hours a week with each child. The purpose of mentoring was to create empowering relationships with children, provide positive role models, ensure that children received appropriate services and support, help children generalise skills and promote a positive future orientation. Children attended a mean of 25.0 group sessions and 26.7 mentoring sessions Control (n = 79) Received assessment only Therapists The 2 facilitators were licenced clinicians and graduate student trainees. Mentors were graduate students in social work who received weekly individual and group supervision |
|
| Outcomes |
PTSD symptoms Scale: Trauma Symptom Checklist for Children Rater: child Quality of life Scale: Life Satisfaction Survey Rater: child When Post therapy and at 6 months |
|
| Notes | SDs calculated from SEs | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation was stratified by gender and county, followed by 'manually randomized, by cohort, in a single block'. No other details were provided. When multiple members of a sibling group were eligible, 1 sibling was randomly selected to participate in the randomised controlled trial |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably knew whether they were in the active or control group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | 'Interviewers were masked to participant group', but all outcomes were self reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Post‐therapy loss to follow‐up: 9%; loss to follow‐up at 6 months: 7% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Unclear risk | IQ, coping and social support scores were higher in the intervention group. Also, participants in the intervention group were more likely to have undergone physical abuse and maternal neglect and to have a mother with a criminal history |
Tol 2008.
| Methods | Cluster‐randomised trial of a group‐based CBT intervention vs wait list | |
| Participants |
Included (n = 403) Children attending randomly selected schools in violence‐affected communities were screened for exposure to ≥ 1 violent event, scored ≥ 12 on the PTSD scale and ≥ 5 on the anxiety scale Mean age: 9.94 years. Female: 196. Mean number of violent exposures: 3.9 Excluded Considered unable to function in a group setting, including aggression, mutism, mental retardation, substance abuse, dissociative disorders, unmedicated epilepsy, panic or phobic disorders, child psychosis Setting Fourteen schools in Central Sulawesi Indonesia, 2006 |
|
| Interventions |
Intervention (n = 182) Manualised, school‐based intervention that integrates CBT techniques over 15 sessions in 5 weeks to groups of approximately 15 children. Sessions included psychoeducation, trauma‐processing activities, cooperative play and creative/expressive elements Control (n = 221) Wait list control group Therapists Locally trained paraprofessionals who had been selected for their social skills and received 2 weeks of training. Adherence was rated as 90% |
|
| Outcomes |
PTSD symptoms Scale: Child Post‐Traumatic Stress Scale (17‐item) Rater: child Depression Scale: Depression Self‐Rating Scale (8‐item) Rater: child Anxiety Scale: Self‐Report for Anxiety‐Related Disorder (SCARED‐5; 5 items) Rater: child Behaviour Scale: Children’s Aggression Scale for Parents (33‐item) Rater: parent Function Scale: Functional impairment (10‐item) Rater: child, parent When At 1 week and 6 months |
|
| Notes | Functional impairment change scores were analysed as positive values to assess improvement in function | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in the active or wait list group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Observers were not blinded, but all measures were child reported or parent reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Last observation carried forward analysis was used. Loss to follow‐up was low: 1 week 3%, 6 months 9% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | High risk | Displacement was higher in the control group (75%) than in the intervention group (37%) |
Tol 2012.
| Methods | Cluster‐randomised trial of a school‐based mental health intervention vs wait list | |
| Participants |
Included (n = 399) Children in grades 4 through 7 were screened for war‐related risk factors, current psychological symptoms, affected school function and absence of protective factors using the Child Psychosocial Distress Screener (CPDS). Age ranged from 9 to 13 years (mean, 11.03). Boys: 61.4%; 81.0% were of the Hindu religion. Children were exposed to an average of 2 war‐related events Excluded None reported Setting Two divisions of the Jaffna District, northern Sri Lanka, 2007 to 2008 |
|
| Interventions |
School‐based mental health intervention (n = 199) The manualised intervention consisted of cognitive‐behavioural techniques, psychoeducation, coping and guided exposure to past traumatic events through drawing and creative expressive elements. It was delivered to groups of around 15 children in 15 sessions over 5 weeks Wait list control (n = 200) Therapists Interventionists were locally identified non‐specialised personnel who had received at least a high school diploma and were selected for their affinity and capacity to work with children. They were trained and supervised in implementing the manualised intervention for 1 year before the study |
|
| Outcomes |
PTSD symptoms Scale: Child PTSD Symptom Scale (17‐item) Rater: child Depression Scale: Depression Self Rating Scale (18‐item) Rater: child Anxiety Scale: Screen for Anxiety‐Related Disorders (5‐item) Rater: child Behaviour Scale: Strengths and Difficulties Questionnaire (25‐item) Rater: child Function Scale: Functional impairment scale developed by study authors (10‐item) Rater: child When At 1 week and 6 months |
|
| Notes | Data were reported for 201 participants in the wait list group at 3 months (123 boys and 78 girls), although the total was previously reported as 199 Data were pooled across genders for meta‐analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in the active or wait list group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Observers were blinded, but all measures were child reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up was reported at 1 week; loss to follow‐up was very small at 3 months (0.5%) |
| Selective reporting (reporting bias) | Unclear risk | Data from 1 week of follow‐up were not reported |
| Other bias | Low risk | No other bias was apparent |
Tol 2014.
| Methods | Cluster‐randomised trial of a classroom‐based CBT intervention vs wait list for children in war‐affected Burundi | |
| Participants |
Included (n = 329) Children screened for exposure to traumatic events, who scored above the standard cutoff on symptom checklists for PTSD (≥ 11)**, depression (≥ 15) or anxiety (≥ 5). Mean age 12.29 years. Female 48% (158). Mean number of traumatic events: intervention 4.6, wait list 4.1; mean PTSD symptom scores: intervention 15.62, wait list 16.30 Excluded Serious psychopathology and psychiatric disorders (mutism, retardation, psychotic symptoms) or incapability to function in a group (conduct disorders, harming others), as judged by local psychosocial counsellors Setting Random selection of schools in 2 northwestern provinces (Bubanza and Cibitoke) in Burundi, 2006 to 2007 |
|
| Interventions |
Classroom‐based CBT intervention (n = 153) Cognitive‐behavioural techniques including psychoeducation, coping skills and working with the trauma narrative, using creative expressive elements such as drawing, music, drama, dance, structured movement and cooperative games. The manualised intervention consisted of 15 sessions over 5 weeks with classroom‐based groups of around 15 children Therapists Locally identified non‐specialised facilitators were trained and supervised in the intervention for 1 year before the study. Facilitators had a minimum education level of a high school diploma and were selected for their affinity and capacity to work with children Wait list (n = 176) Provision of treatment after the research was completed |
|
| Outcomes |
PTSD symptoms Scale: Child Post‐Traumatic Symptom Scale (17‐item) Rater: child Depression Scale: Depression Self‐Rating Scale (18‐item) Rater: child Behaviour Scale: not reported but aggression scale was listed in the protocol Rater: not reported Function Scale: function impairment measure (9‐item) Rater: child When At 1 week and 3 months after treatment |
|
| Notes | **Criterion validity of the PTSD symptom checklist against a psychiatric diagnostic interview with the Schedule for Affective Disorders and Schizophrenia for School‐Age Children gave an optimum cutoff score for PTSD of 26 (sensitivity 0.71, specificity 0.83) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants (performance bias | High risk | Participants would have known whether they were in the intervention or wait list group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Measures were self reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Selective reporting (reporting bias) | Unclear risk | Aggression was not reported but was referred to in the protocol; anxiety was not used because of low values of Cronbach's alpha for the SCARED. One week follow‐up data were not reported for any outcome |
| Other bias | Low risk | None identified |
Trowell 2002.
| Methods | Randomised trial of individual vs group psychotherapy | |
| Participants |
Included (n = 75) Girls 6 to 14 years of age who had confirmed contact sexual abuse disclosed within the previous 2 years and experiencing emotional or behavioural disturbance that warranted treatment (n = 58). Mean age 10 years. Ethnicity: white 8, black Caribbean 7, mixed 5, Chinese 5, Mediterranean 4, unknown 2 Excluded Girls with severe developmental delay, psychosis, possibility of further abuse, hospitalisation at evaluation and 'other' clinical and legal issues Setting Two clinics in London: 1 tertiary and 1 community |
|
| Interventions |
Individual psychotherapy (n = 35 entered therapy) Comprised up to 30 weekly 50‐minute sessions. The first 5 were based on engagement, the next 25 on issues identified as relevant to the child and the final 10 on separation and ending Group psychotherapy (n = 36 entered therapy) Psychoeducational and psychotherapeutic. Participants attended up to 18 sessions Face‐to‐face contact time was comparable overall with individual sessions Therapists For both interventions, therapy was manualised and supervised. Therapists were trainee psychotherapists or experienced mental health professionals |
|
| Outcomes |
PTSD symptoms Scale: Schedule for Affective Disorders and Schizophrenia for School‐Age Children (K‐SADS, shortened version) Rater: clinician PTSD symptoms Scale: Orvaschel's PTSD scale (19‐item) Rater: clinician Function Scale: Kiddie Global Assessment Scale Rater: clinician Cost Scale: GBP When At 12 and 24 months |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | Unclear risk | Although all participants received therapy, they would have known whether they received individual or group treatment |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | All outcomes were clinician rated, but blinding was not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Last observation carried forward analyses were used, but completer data (means and SDs) were reported. Loss to follow‐up: 23% |
| Selective reporting (reporting bias) | High risk | Depression, anxiety and hyperarousal were not reported |
| Other bias | Low risk | No other bias was apparent |
Zehnder 2010.
| Methods | Stratified randomised trial of single‐session early psychological intervention for children after road traffic accidents vs standard care | |
| Participants |
Included (n = 101) Children or adolescents receiving inpatient or outpatient medical treatment after a road traffic accident, who were fluent in German Excluded Severe head injury (Glasgow Coma Scale > 11) or previous evidence of intellectual impairment Setting University Children’s Hospital in Zurich, Switzerland, 2004 to 2007 |
|
| Interventions |
Single‐session early psychological intervention (n = 51) The manualised intervention was provided to the child and ≥ 1 parent around 10 days after the child’s involvement in a road traffic accident. The psychologist used a series of standard prompts systematically to guide the child through a structured, 4‐step process, including detailed reconstruction of the accident and creation of a trauma narrative with drawings and toys used as aids, identification of accident‐related appraisals by asking children about trauma‐related thoughts and assistance modifying dysfunctional appraisals and psychoeducation on common stress reactions. The psychologist then discussed with the child and the parents helpful strategies for dealing with acute stress reactions, and parents were given advice on how to support their child, along with written information on post‐traumatic stress and a contact address Control (n = 50) Children of this group received standard medical care, including clinical diagnostics and comprehensive medical treatment. Psychological support was available but was not routinely provided Therapist The therapist was a psychologist. No other details were reported |
|
| Outcomes |
PTSD symptoms Scale: Clinician‐Administered PTSD Scale for Children and Adolescents (CAPS‐CA) Rater: clinician Depression Scale: Children’s Depression Inventory (26‐item) Rater: child/adolescent Behaviour Scale: Child Behavior Checklist (120‐item) Rater: parent When At 2 and 6 months |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The randomisation list, stratified by gender, was generated by a computer programme |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias | High risk | Participants probably were aware of whether they were in an active or control group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not reported, but 2 of the 3 measures were child and parent reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT not used, but loss to follow‐up was small: 2 months 1%, 6 months 2% |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to have been reported |
| Other bias | Low risk | No other bias was apparent |
CDI: Children's Depression Inventory
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Berger 2007 | Not screened for trauma |
| Bolton 2007 | Screened for depression but not trauma |
| Burke 1988 | Not randomised; matched control |
| Catani 2009 | All participants had to meet criteria for PTSD to be included in this study; therefore, it was reviewed in Gillies 2012 |
| Chen 2014 | All participants had scores > 18 on the CRIES‐13, which was cited as 81% sensitivity and 77% specificity for PTSD ‐ to be reviewed in the update of Gillies 2012 |
| Cohen 2004 | All participants had to meet criteria for PTSD to be included in this study; therefore, it was reviewed in Gillies 2012 |
| Cooley‐Strickland 2011 | Exposure to trauma was not an inclusion criterion |
| Dybdahl 2001 | Intervention for mothers only |
| Ehntholt 2005 | Not randomised |
| Ensink 2004 | No data reported, and study authors could not be contacted |
| Ertl 2011 | All participants had to meet criteria for PTSD to be included in this study; therefore, it was reviewed in Gillies 2012 |
| Gelkopf 2009 | Exposure to trauma was not an inclusion criterion |
| Gellman 2001 | Not randomised; matched control |
| Goenjian 1997 | Pre‐post study |
| Graham‐Bermann 2013 | Partcipants were sequentially allocated to groups |
| Hardin 2002 | Not screened for trauma |
| Jacob 2014 | All participants had to meet criteria for PTSD; therefore, this study will be reviewed in the update of Gillies 2012 |
| Jeffres 2004 | Not randomised |
| Jensen 2014 | Included participants had scores ≥ 15 on the Child PTSD Symptom Scale, which is considered diagnostic of PTSD ‐ to be included in the update of Gillies 2012 |
| Jordans 2010 | Exposure to trauma was not an inclusion criterion |
| Kassam‐Adams 2011 | Randomised trial of stepped care versus usual care |
| Kataoka 2003 | Data for randomised controls not reported and could not be obtained |
| Kenardy 2008 | Case control study |
| King 2000 | All participants had to be diagnosed with PTSD to be included in this study; therefore, it was reviewed in Gillies 2012 |
| Krueger 2013 | Children were alternately allocated to trauma‐focused interpersonal therapy or CBT |
| Lyshak‐Stelzer 2007 | Interim analysis of the data (30/55 not LTFU – 86 randomised in total with 31 LTFU at this report) |
| McWhirter 2011 | Did not report included outcomes |
| Murray 2015 | Mean baseline trauma symptom item scores (PTSD‐RI 38‐item trauma symptom scale) were 1.88 in the TF‐CBT group and 1.75 in the TAU group ‐ to be reviewed in the update of Gillies 2012 |
| Pfeffer 2002 | Families were alternately allocated; loss to follow‐up was 75% in the no treatment group |
| Phipps 2012 | Intervention was not a psychological therapy |
| Rosner 2014 | Ongoing study of cognitive processing therapy versus usual care for treatment of adolescents and young adults with PTSD following abuse. To be reviewed in the update of Gillies 2012 |
| Rubin 2001 | Not screened for trauma |
| Ruf 2010 | All participants had to meet criteria for PTSD to be included in this study; therefore, it was reviewed in Gillies 2012 |
| Ruf 2012 | Study of Lifeline‐NET, short‐term narrative exposure therapy for refugees and asylum Seekers aged 16 to 60 years with PTSD. This will be reviewed in the update of Gillies 2012 |
| Saxe 2012 | Only 1 of 10 participants in the usual care group were followed up |
| Schaal 2009 | Average age of participants was 19 years |
| Schauer 2008 | All participants had to meet criteria for PTSD to be included in this study; therefore, it was reviewed in Gillies 2012 |
| Scheeringa 2011 | Less than 50% of the intervention group were randomised |
| Shelby 1995 | No comparison group |
| Shooshtary 2008 | Not randomised |
| Soltanifar 2012 | Study of attachment‐based play therapy compared to supportive therapy for children with developmental trauma disorder. This will be reviewed in the update of Gillies 2012 |
| Stronach 2012 | Both interventions working with mother, although directed at the parent/child interaction |
| Thabet 2005 | Not randomised |
| Wang 2011 | Not screened for trauma; case control study |
| Wolmer 2011a | Not randomised |
| Wolmer 2011b | Not randomised |
LTFU: Loss to follow‐up
Characteristics of studies awaiting assessment [ordered by study ID]
Crombach 2012.
| Methods | Randomised single‐blind trial of narrative exposure therapy for violent offenders versus no treatment for aggressive behaviour and symptoms of PTSD in former street children and vulnerable children in Burundi |
| Participants |
Included: male former street children and vulnerable children in Burundi 12 to 23 years of age who took part in an aid programme for reintegration into society and demonstrated positive emotions towards aggressive behavior (n = 42) Excluded: those with current substance dependence, those with use of antipsychotic drugs, chronically ill children |
| Interventions |
Narrative exposure therapy for violent offenders (NETvo): With the assistance of the therapist over 4 sessions, the client constructs a chronological narrative of his life with a focus on exposure to traumatic stress and perpetrated violent acts. Key components of the therapist's behaviour are empathic understanding, active listening, congruency and unconditional positive regard, while asking about emotions, cognitions, sensory information and physiological reactions, and linking these to an autobiographical context. Positive emotions and cognitions reported for violent acts are linked to the respective past. In the fifth session, plans and ideas for the future are developed to assist reintegration into society Control: no treatment |
| Outcomes |
Aggressive behavior: Appetitive Aggressions Scale for children and students
Trauma symptoms: UCLA Adolescent PTSD Index (Clinician‐Administered)
Depressive symptoms: Mini InternationaI Neuropsychiatric Interview for children (MINI‐KID)
Suicidal ideation: MINI‐KID
Function: Children's Global Assessment Scale; Strengths and Difficulties Questionnaire All measured at 6 months |
| Notes | Contact: Anselm Crombach, University of Konstanz Trial identifier: NCT01519193 |
Elbert 2009.
| Methods | Parallel single‐blind RCT comparing NET truth education, conflict resolution training and traditional methods for previously abducted and other vulnerable youths in Northern Uganda |
| Participants | Included: males and females 12 to 30 years of age (n = 600). Participants had to have a diagnosis of PTSD to be included in the individual NET trial, but all youths in the selected vocational training centres are eligible for inclusion in the trial of group interventions |
| Interventions |
NET truth education: individual narrative exposure and truth education in groups Conflict resolution and social competence skills; conflict resolution and social competence skills in groups Traditional methods: methods collected by local teachers to help vulnerable children and youths in Northern Uganda |
| Outcomes | Primary outcomes: PTSD symptoms and functional level at 6 and 12 months of follow‐up Secondary outcomes: aggression, reconciliation, reintegration, conflict and compromise behaviour at 6 and 12 months of follow‐up |
| Notes | Contact: Prof. Dr. Thomas Elbert, University of Konstanz Trial identifier: NCT00893750 |
Elbert 2013.
| Methods | Parallel RCT of FORNET versus CBT versus treatment as usual |
| Participants |
Included: 44 former young male offenders 10 to 30 years of age with high levels of aggression and exposed to traumatic stress in South Africa Excluded: participants with neurological or psychiatric disorders other than those resulting from exposure to trauma, including chronic psychosis or acute substance use |
| Interventions |
FORNET: a narrative exposure therapy adapted to forensic offender rehabilitation CBT Treatment as usual |
| Outcomes |
Primary outcome measures: change in PTSD symptom severity with the Post‐Traumatic Stress Disorder Scale ‐ Interview Secondary outcome measures: change in self committed violence with the Appetitive Aggression Scale Change in strength of suicidal ideation measured with the Mini InternationaI Neuropsychiatric Interview 6.0. Change in psychosocial functioning measured with the Work and Social Adjustment Scale Change in depression severity with the Patient Health Questionnaire‐9 All measured at 6 and 12 months post‐treatment follow‐up |
| Notes | Contact: Prof. Dr. Thomas Elbert, University of Konstanz Trial identifier: NCT02012738 |
Hultmann 2012.
| Methods | Parallel RCT of trauma‐focused CBT compared with treatment as usual treatment for children exposed or subjected to intimate partner violence or child abuse |
| Participants |
Included 1. Children and adolescents 5 to 17 years of age attending child psychiatric services exposed to intimate partner violence or child abuse as measured by the revised Conflict Tactics Scale 2 (CTS2) or child version (CTS‐C). 2. At least one item on CTS2 or CTS‐C positively checked on sexual abuse or at least three items checked on physical violence or at least five items checked on psychological abuse. Excluded: Child with IQ < 70 or pervasive developmental disorder; child or parent needs an interpreter to fulfil treatment; parent unable to take part in the treatment; child needs inpatient treatment. Setting Child psychiatric services, Sweden |
| Interventions |
Trauma‐focused CBT 10‐15 sessions of Individual trauma‐focused CBT Treatment as usual |
| Outcomes | Trauma symptoms, psychiatric symptoms, psychological well‐being at the end of treatment and one year from treatment |
| Notes | Contact: Ole Hultmann
Tel: +46 (0) 31 337 5170+46 (0) 31 337 5170 Trial identifier: ISRCTN58027256 (Retrospectively registered) |
Jessiman 2013.
| Methods | Randomised trial comparing the intervention 'Letting the Future In' with a wait list control for children affected by sexual abuse in the UK |
| Participants |
Included: children aged between 4‐17 years who have made a disclosure of sexual abuse and who have a safe carer who is willing to participate. Excluded: those with severe learning disability |
| Interventions |
Letting the Future In: Up to 24 sessions with a trained social worker or therapist. LTFI also emphasises work with the child’s safe carer, who may receive up to six individual sessions as well as joint sessions with the child. Wait list Offered therapy after 6 months |
| Outcomes | Trauma symptoms, victimisation, parenting stress at baseline and 3 and 12 months follow‐up |
| Notes | Contact: Tricia Jessiman
Tricia.Jessiman@bristol.ac.uk Trial identifier: ISRCTN65340805 |
Kassam‐Adams 2016.
| Methods | Randomised controlled trial of Coping Coach, a Web‐based preventive intervention to prevent or reduce symptoms of post‐traumatic stress after acute paediatric medical events compared with wait list |
| Participants | Included: children 8 to 12 years of age who had experienced a medical event, have access to Internet and telephone and have sufficient competency in English to complete measures and understand the intervention, Philadelphia, USA |
| Interventions |
Coping Coach: Children in the intervention condition will complete module 1. Feelings identification in the hospital and instructions on how to complete module 2. Appraisals and module 3. Avoidance online Wait list: After 12‐week assessment, children will receive instructions for completing the intervention |
| Outcomes | PTSD symptoms, coping, health‐related quality of life |
| Notes | Contact: Nancy Kassam‐Adams PhD, Center for Injury Research & Prevention, Children's Hospital of Philadelphia Trial identifier: NCT01653288 |
Kramer 2014.
| Methods | Parallel randomised single‐blind trial of brief early psychological intervention versus standard medical care for children and adolescents hospitalised for burns or road traffic accident injury |
| Participants |
Included: children and adolescents (2 to 16 years of age) hospitalised for burns or road traffic accident injury, with Glasgow Coma Scale (GCS) > 8, German speaking, with burn accident or road traffic accident, at high risk of developing PTSD in Zurich, Switzerland Excluded: those with > 2 weeks in the paediatric intensive care unit, with previous mental retardation |
| Interventions |
Intervention: age‐appropriate 2‐session intervention that includes detailed reconstruction of the accident, psychoeducation and discussion of helpful coping strategies. Both control and intervention groups are reassessed by blind raters at 3 and 6 months after the accident Standard medical care: not described |
| Outcomes | Post‐traumatic stress symptoms, depression, anxiety, behaviour, health‐related quality of life 3 and 6 months after the accident |
| Notes | Contact: Markus Landolt PhD, Psychosomatic and Psychiatry, University Children's Hospital Zurich Trial identifier: unknown |
Mahmoudi‐Gharaei 2006.
| Methods | RCT of group CBT with and without an art and sport intervention, art and sport alone and control for adolescents who survived the Bam earthquake |
| Participants |
Included (n = 200) Adolescents with PTSD symptoms who survived the Bam earthquake. Setting Iran |
| Interventions |
Group CBT: includes CBT with and without an art and sport intervention Control: no treatment or an art and sport intervention |
| Outcomes | PTSD symptoms |
| Notes | Contact: J Mahmoudi‐Gharaei, Hospital Tehran University of Medical Sciences.
Jmahmoudi@tums.ac.ir Trial identifier: unknown |
Narimani 2013.
| Methods | Randomised trial of cognitive processing therapy versus control |
| Participants |
Included (n = 60) Male students in first, second and third high school grades in Uromia who had experienced traumatic events Setting Iran |
| Interventions |
Cognitive processing therapy: holographic reprocessing Control |
| Outcomes | PTSD symptoms Anxiety Depression |
| Notes | Contact: Trial identifier: Status September 2016: Information about methods and data needed |
Ooi 2010.
| Methods | Cluster‐randomised non‐blinded trial of Teaching Recovery Techniques versus wait list in young migrants exposed to war‐related trauma |
| Participants |
Included males and females 11 to 17 years of age exposed to war‐related trauma before migrating to Australia, lived in Australia for less than 7 years, self reporting symptoms of PTSD Excluded diagnosis of PTSD, limited English, non‐accompanied humanitarian entrant, currently receiving psychological treatment for PTSD |
| Interventions |
Teaching Recovery Techniques (Smith et al., 2000): group‐based CBT aimed at educating children about their symptoms and teaching adaptive coping strategies, which include creation of self coping statements, relaxation and exposure strategies (manual and workbook available from www.childrenandwar.org). The intervention runs for 1 hour a week for 8 weeks and is facilitated by 2 trained facilitators Wait list: will not receive any intervention until the end of the trial |
| Outcomes | PTSD symptoms, depression, anxiety at baseline, post‐test and 3 months follow‐up |
| Notes | Contact: Dr Chew Ooi, School of Psychology Curtin University, chewsia@gmail.com Trial identifier: ACTRN12611000948998 (Retrospectively registered) Status September 2016: |
Rowe 2013.
| Methods | Parallel repeated‐measures intention‐to‐treat RCT of family therapy versus CBT |
| Participants |
Included: adolescents 13 to 17 years of age who met American Society for Addiction Medicine criteria for outpatient substance abuse treatment, at least mild trauma symptoms on the PTSD‐Reaction Index following Hurricane Katrina and not receiving other behavioural treatment Excluded: adolescents with mental retardation, pervasive developmental disorders, psychotic disorder or current suicidality |
| Interventions |
Multi‐dimensional family therapy (MDFT): a multi‐system family‐based approach designed to address the multiple developmental disruptions and symptoms that result from interaction of individual, family, peer and community risk factors Group CBT: peer group‐based CBT model based on established guidelines for CBT therapy for teen substance abuse by targeting cognitions about use and focusing on accompanying problem behaviours such as poor academic performance and limited social skills |
| Outcomes |
Trauma symptoms: revised PTSD‐RI School problems: based on school records Delinquency: court records and the National Youth Survey Self‐Report Delinquency Scale All measured 1 year before intake through 12‐month follow‐up |
| Notes | Contact: Cynthia Rowe, Research Associate Professor, University of Miami Trial identifier: NCT01859000 |
Ruggiero 2015.
| Methods | Parallel randomised double‐blind trial of a Web‐based intervention versus control for adolescents affected by natural disaster |
| Participants |
Included: adolescents 12 to 17 years of age residing in identified locations at the time of disaster who had home Internet connectivity and their primary caregiver, USA Excluded: those for whom primary caregiver was not available |
| Interventions |
Bounce Back Now: a Web‐based child, parenting and parent psychoeducation and self help Website Control: child and parent Web‐based assessment |
| Outcomes | Adolescent and parent mental health symptoms, parent/child conflict and relationship |
| Notes | Contact: Kenneth Ruggiero PhD, Medical University of South Carolina ruggierk@musc.edu. Trial identifier: NCT01606514 |
Shen 2012.
| Methods | Randomised trial of Expressive group counselling versus control |
| Participants |
Included (n = 120) Children who were 'affected by earthquake but had no grave psychic trauma' Setting China |
| Interventions |
Expressive group counselling (n = 60) Control (n = 60) |
| Outcomes |
Anxiety Scale: Social Anxiety Scale for Children Rater: child/adolescent When Post treatment |
| Notes | Contact: unknown Trial identifier: unknown |
Zang 2013.
| Methods | Parallel randomised single‐blind trial of guided narrative technique versus expressive writing instruction group for children affected by earthquake |
| Participants |
Included: children 9 to 14 years of age who had experienced the earthquake in Beichuan County, China, and did not attend other trauma‐focused interventions Excluded: children who cannot write |
| Interventions |
Guided narrative technique: writing instructions Control: expressive writing instruction group |
| Outcomes | PTSD, depression, anxiety, coping, social support, outlook scores |
| Notes | Contact: Yinyin Zang, Nigel Hunt, Nottingham University, zangyinyin@gmail.com nigel.hunt@nottingham.ac.uk Trial identifier: ChiCTR‐TRC‐12002940, ChiCTR‐TRC‐12002941 registered retrospectively |
Characteristics of ongoing studies [ordered by study ID]
Belcher 2009.
| Trial name or title | FamilyLive Feasibility and Effectiveness Study |
| Methods | Parallel RCT of FamilyLive versus standard mental health treatment in children exposed to neglect |
| Participants |
Included: children 5 to 17 years of age exposed to neglect, enrolled in treatment at the Kennedy Krieger Family Center, who continue to exhibit behavior dysregulation (CBCL > 60) and/or attachment difficulties after 3 months of standard mental health care treatments; and their parents who also have a history of neglect with or without trauma (n = 300), Baltimore, USA Excluded: children with cardiac arrhythmias, with endocrine disorders associated with heart rate irregularities, not able to co‐operate with or understand study procedures, Non‐English‐speaking children, hearing impaired, children in foster care |
| Interventions |
FamilyLive: an intervention for families with a history of intergenerational neglect and trauma exposure aimed at unresolved and untreated histories of neglect and disrupted attachment and providing support to improve parental self care, stress management, emotional regulation, self awareness and management of children's responses and behaviours Standard mental health treatment: standard trauma‐informed mental health treatment |
| Outcomes | Behaviour; post‐traumatic stress disorder symptoms; function at baseline, 3, 6 and 12 months |
| Starting date | February 2009 |
| Contact information | Contact: Harolyn M.E. Belcher, MD belcher@kennedykrieger.org |
| Notes | Trial identifier: NCT01524185 Status September 2016: active, not recruiting Estimated study completion: November 2021 |
Dorsey 2012.
| Trial name or title | Randomized Controlled Trial of Trauma‐Focused CBT in Tanzania and Kenya for Children Whose Parent Has Died |
| Methods | Parallel RCT of 12‐week trauma‐focused CBT group treatment for children and their guardians versus usual care |
| Participants | Included children 7 to 13 years of age living in Moshi, Tanzania, or Bungoma, Kenya, who have had 1 or both parents die since they were 3 years of age or older, those with symptoms of traumatic grief and/or traumatic stress, those living with an adult guardian willing to participate in 12 weekly group sessions Excluded children living in an institution |
| Interventions | Trauma‐focused CBT |
| Outcomes | PTSD, behaviour, traumatic grief, function, child/guardian relationship |
| Starting date | August 2012 |
| Contact information | Shannon Dorsey PhD, University of Washington Department of Psychology dorsey2@u.washington.edu |
| Notes | Trial identifier: NCT01822366 Status September 2016: This study is ongoing, but not recruiting participants Estimated study completion: December 2017 |
Roos 2013.
| Trial name or title | A Randomized Comparison of Eye Movement Desensitization and Reprocessing (EMDR) and Cognitive Behavioral Writing Therapy (CBWT) in Pediatric Post‐Traumatic Stress Disorder Following Single‐Incident Trauma |
| Methods | Parallel randomised single‐blind trial of EMDR versus cognitive‐behavioural writing therapy in children and adolescents following single‐incident trauma |
| Participants |
Included: children and adolescents between 8 and 18 years of age who have experienced a single traumatic event, have had 5 post‐traumatic stress symptoms after 1 month, with sufficient Dutch language, The Netherlands Excluded: those with acute psychiatric problems (suicidality, psychosis), IQ < 80 |
| Interventions | EMDR: requires the client to attend a distracting stimulus, typically the therapist’s fingers moving back and forth, while concentrating on the trauma memory. Treatment consists of (1) history taking and treatment planning, (2) explanation of and preparation for EMDR, (3) preparation of the target memory, (4) desensitisation of the memory, (5) guidance for the client to embrace a relevant positive belief regarding the event, (6) identification and processing of any residual disturbing body sensations, (7) closure of the session and (8) re‐evaluation A maximum of 6 sessions is permitted CBWT: The therapist helps the child to write a detailed account of his or her thoughts, feelings and behaviours during the traumatic event/s. The most important elements are psychoeducation, exposure, cognitive restructuring and promotion of adequate coping and social sharing A maximum of 6 sessions is permitted |
| Outcomes | PTSD symptoms, anxiety, depression, somatic and behavioural symptoms, quality of life, post‐traumatic cognitions, somatic symptoms, post‐traumatic growth |
| Starting date | October 2010 |
| Contact information | Carlijn de Roos Psychotrauma Centre for Children and Youth, MHI Rivierduinen |
| Notes | Trial identifier: NTR3870 Status September 2016: open for patient inclusion |
Sansom‐Daly 2012.
| Trial name or title | Online Group‐Based Cognitive‐Behavioural Therapy for Adolescents and Young Adults After Cancer Treatment |
| Methods | Cluster‐randomised single‐blind trial of Recapture Life, an online group‐based CBT, versus on‐line peer support and wait list for adolescents and young adults following cancer treatment |
| Participants | Included adolescents and young adults 15 to 25 years of age who had finished cancer treatment in the preceding 1 to 6 months, were able to read English and provide contact details of a trusted health professional and had access to the Internet in a private location, Australia Excluded those with insufficient English language skills to complete the intake interview, extremely severe depression and/or serious suicidal intent, symptoms of psychosis or substance abuse |
| Interventions | Recapture Life: Sessions focus on acquisition and application of cognitive‐behavioural skills, such as cognitive restructuring and problem solving to returning to normality after cancer treatment. Delivered over the Internet by a clinical psychologist in 6 weekly 90‐minute group sessions with a 1‐off 'booster' session 6 weeks afterwards Peer support group: gives young cancer survivors an open forum to discuss their experience and includes non‐directive counselling with no cognitive‐behavioural components Delivered over the Internet by a clinical psychologist in 6 weekly 90‐minute group sessions with a 1‐off 'booster' session 6 weeks afterwards Wait list |
| Outcomes | Quality of life, depression, anxiety, stress, family functioning, coping, cancer‐related identity |
| Starting date | 30 August 2010 |
| Contact information | Ursula M. Sansom‐Daly u.sansomdaly@gmail.com |
| Notes | Trial identifier: ACTRN12610000717055 Status September 2016: Recruiting Estimated study completion: |
Toth 2011.
| Trial name or title | Prevention of Depression in Maltreated and Non‐Maltreated Adolescents |
| Methods | Parallel randomised open trial of interpersonal therapy for adolescents versus enhanced care |
| Participants | Included: maltreated and non‐maltreated adolescent girls 13 to 15 years of age of low socioeconomic status (girls in the maltreated depressive symptom group will have Child Protection Service‐documented child maltreatment) who live in Rochester or surrounding counties, USA Excluded: those taking antidepressants or prescription medications for anxiety, receiving mental health treatment, actively suicidal, diagnosed with a severe mental disorder, abusing drugs or alcohol, compromised cognitive ability, pervasive developmental disorder, major physical or neurological disorder, non‐English speaking |
| Interventions | Interpersonal psychotherapy for adolescents: a manualised intervention for depression and prevention of depression that emphasises current interpersonal relationships, while focusing on immediate social context Enhanced care: consistent with care typically provided in community settings to treat and prevent depression |
| Outcomes | Depression |
| Starting date | July 2011 |
| Contact information | Sheree Toth University of Rochester 585‐275‐2991 |
| Notes | Trial identifier: http://grantome.com/grant/NIH/R01‐MH091070‐04 Status September 2016: Estimated study completion: May 2016 |
Differences between protocol and review
Trauma exposure
It was proposed for prevention studies that we include only trials in which children or adolescents had been exposed to a traumatic event within a year before initiation of therapy. However, as time since exposure to trauma was not an inclusion/exclusion criterion in any included trials, the review authors decided to include all studies that met all other inclusion criteria.
Quality criteria
We stated in the protocol the intention to collect the following quality criteria. We collected these, but we updated the headings for quality criteria for consistency with quality criteria headings provided in the 'Risk of bias' table.
Adequate allocation concealment and sequence generation.
Clear inclusion and exclusion criteria.
No potential confounding variables.
Intention‐to‐treat analysis.
< 25% loss to follow‐up.
Blinded outcome assessment.
Skewed data
In the protocol, it was stated that "if the standard deviation multiplied by two was greater than the mean it will not be added to the meta‐analysis", but this was updated to comply with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008) (i.e. for a scale that starts from zero, a standard deviation greater than half the mean suggests skew, but a standard deviation greater than the mean is considered strong evidence of a skewed distribution). Therefore, if the standard deviation was greater than the mean for both groups, these data were not included in a meta‐analysis.
Best‐case/Worst‐case analyses
It was initially proposed that in best‐case and worst‐case analyses of primary binary outcomes, early departure of people from the study was considered to have had a negative effect in the treatment group and no negative effect in the control group (worst‐case scenario), or no negative effect in the treatment group and a negative effect in the control group (best‐case scenario). However, we considered it more appropriate that people from both groups would have left for the same reason; therefore, for worst‐case, we have considered that all people lost to follow‐up had the negative outcome (i.e. a diagnosis of PTSD), and for best‐case analysis, all those lost to follow‐up were considered not diagnosed with PTSD.
Contributions of authors
Donna Gillies ‐ review co‐ordination, study selection, data extraction, data entry and analysis, writing of the review.
Licia Maiocchi ‐ data extraction, data analysis.
Abhishta P. Bhandari ‐ study selection, data extraction.
Fiona Taylor ‐ study selection, data extraction.
Carl Gray ‐ data extraction.
Louise O'Brien ‐ data extraction.
Sources of support
Internal sources
Sydney West Area Health Service, Australia.
The University of Western Sydney, Australia.
External sources
No sources of support supplied
Declarations of interest
None known.
New
References
References to studies included in this review
Baker 1985 {published data only}
- Baker CR. A comparison of individual and group therapy as treatment of sexually abused adolescent females. PhD dissertation, University of Maryland, USA, 1985.
Barron 2013 {published data only (unpublished sought but not used)}
- Barron, IG, Abdallah G, Smith P. Randomized control trial of a CBT trauma recovery program in Palestinian schools. Journal of Loss and Trauma 2013;18(4):306‐21. [Google Scholar]
Berger 2009 {published data only}
- Berger R, Gelkopf M. School‐based intervention for the treatment of tsunami‐related distress in children: a quasi‐randomized controlled trial. Psychotherapy and Psychosomatics 2009;78(6):364‐71. [DOI] [PubMed] [Google Scholar]
Berger 2012 {published data only}
- Berger R, Gelkopf M, Heineberg Y. A teacher‐delivered intervention for adolescents exposed to ongoing and intense traumatic war‐related stress: a quasi‐randomized controlled study. Journal of Adolescent Health 2012;51(5):453‐61. [DOI] [PubMed] [Google Scholar]
Berkowitz 2011 {published data only}
- Berkowitz SJ, Stover CS, Marans SR. The child and family traumatic stress intervention: secondary prevention for youth at risk of developing PTSD. Journal of Child Psychology and Psychiatry 2011;52(6):676‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goslin MC, Stover CS, Berkowitz SJ, Marans SR. Identifying youth at risk for difficulties following a traumatic event: pre‐event factors are associated with acute symptomatology. Journal of Traumatic Stress 2013;26:475‐82. [DOI] [PubMed] [Google Scholar]
Berliner 1996 {published data only}
- Berliner L, Saunders BE. Treating fear and anxiety in sexually abused children: results of a controlled 2‐year follow‐up study. Child Maltreatment 1996;1(4):294‐309. [Google Scholar]
Betancourt 2014 {published data only}
- Betancourt T. A Feasibility Trial of the Youth Readiness Intervention: A Group Psychosocial Intervention for War‐Affected Youth in Sierra Leone. ClinicalTrialsgov [wwwclinicaltrialsgov] 2012.
- Betancourt TS. A Feasibility Trial of the Youth Readiness Intervention: A Group Psychosocial Intervention for War‐Affected Youth in Sierra Leone. http://clinicaltrialsgov/show/NCT02128568 2014.
- Betancourt TS, McBain R, Newnham EA, Akinsulure‐Smith AM, Brennan RT, Weisz JR, et al. A behavioral intervention for war‐affected youth in Sierra Leone: a randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry 2014;53:1288‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carbonell 1999 {published data only}
- Carbonell DM, Parteleno‐Barehmi C. Psychodrama groups for girls coping with trauma. International Journal of Group Psychotherapy 1999;49(3):285‐306. [DOI] [PubMed] [Google Scholar]
Carrion 2013 {published data only}
- Carrion VG, Kletter H, Weems CF, Berry RR, Rettger JP. Cue‐centered treatment for youth exposed to interpersonal violence: a randomized controlled trial. Journal of Traumatic Stress 2013;26:654‐62. [DOI] [PubMed] [Google Scholar]
Celano 1996 {published data only}
- Celano M, Hazzard A, Webb C, McCall C. Treatment of traumagenic beliefs among sexually abused girls and their mothers: an evaluation study. Journal of Abnormal Child Psychology 1996;24(1):1‐17. [DOI] [PubMed] [Google Scholar]
Chapman 2001 {published data only}
- Chapman L, Morabito D, Ladakakos C, Schreier H, Knudson MM. The effectiveness of art therapy interventions in reducing post traumatic stress disorder (PTSD) symptoms in pediatric trauma patients. Art Therapy 2001;18(2):100‐4. [Google Scholar]
Chemtob 2002 {published data only}
- Chemtob CM, Nakashima JP, Hamada RS. Psychosocial intervention for post disaster trauma symptoms in elementary school children: a controlled community field study. Archives of Pediatrics & Adolescent Medicine 2002;156(3):211‐6. [DOI] [PubMed] [Google Scholar]
Church 2012 {published data only}
- Church D, Pina O, Reategu IC, Brooks A. Single‐session reduction of the intensity of traumatic memories in abused adolescents after EFT: a randomized controlled pilot study. Traumatology 2012;18(3):73‐9. [Google Scholar]
Cohen 1996 {published data only}
- Cohen JA, Mannarino AP. A treatment outcome study for sexually abused preschool children: initial findings.[erratum appears in J Am Acad Child Adolesc Psychiatry 1996 Jun;35(6):835]. Journal of the American Academy of Child & Adolescent Psychiatry 1996;35(1):42‐50. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. A treatment study for sexually abused preschool children: outcome during a one‐year follow‐up. Journal of the American Academy of Child & Adolescent Psychiatry 1997;36(9):1228‐35. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. Factors that mediate treatment outcome of sexually abused preschool children. Journal of the American Academy of Child & Adolescent Psychiatry 1996;35(10):1402‐10. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. Factors that mediate treatment outcome of sexually abused preschool children: six‐ and 12‐month follow‐up. Journal of the American Academy of Child & Adolescent Psychiatry 1998;37(1):44‐51. [DOI] [PubMed] [Google Scholar]
Cohen 2005 {published data only}
- Cohen JA, Mannarino AP. Interventions for sexually abused children: initial treatment outcome findings. Child Maltreatment 1998;3(1):17‐26. [Google Scholar]
- Cohen JA, Mannarino AP, Knudsen K. Treating sexually abused children: 1 year follow‐up of a randomized controlled trial. Child Abuse and Neglect 2005;29(2):135‐45. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Knudsen K. Treatment outcome for sexually abused children at one‐year follow‐up. 156th Annual Meeting of the American Psychiatric Association, May 17‐22, San Francisco CA. 2003, issue 107.
Cohen 2011 {published data only}
- Cohen JA, Mannarino AP, Iyengar S. Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence: a randomized controlled trial. Archives of Pediatrics and Adolescent Medicine 2011;165(1):16‐21. [DOI] [PubMed] [Google Scholar]
Cox 2010 {published data only}
- Cox CM, Kenardy JA, Hendrikz JK. A randomized controlled trial of a web‐based early intervention for children and their parents following unintentional injury. Journal of Pediatric Psychology 2010;35(6):581‐92. [DOI] [PubMed] [Google Scholar]
Damra 2014 {published data only}
- Damra JKM, Nassar YH, Ghabri TMF. Trauma‐focused cognitive behavioral therapy: cultural adaptations for application in Jordanian culture. Counselling Psychology Quarterly 2014;27:308‐23. [Google Scholar]
Danielson 2012 {published data only}
- Danielson CK, McCart MR, Walsh K, Arellano MA, White D, Resnick HS. Reducing substance use risk and mental health problems among sexually assaulted adolescents: a pilot randomized controlled trial. Journal of Family Psychology 2012;26(4):628‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deblinger 1996 {published data only}
- Deblinger E, Lippmann J, Steer R. Sexually abused children suffering posttraumatic stress symptoms: initial treatment outcome findings. Child Maltreatment 1996;1(4):310‐21. [Google Scholar]
- Deblinger E, Steer RA, Lippmann J. Two‐year follow‐up study of cognitive behavioral therapy for sexually abused children suffering post‐traumatic stress symptoms. Child Abuse and Neglect 1999;23(12):1371‐8. [DOI] [PubMed] [Google Scholar]
Deblinger 2001 {published data only}
- Deblinger E, Stauffer LB, Steer RA. Comparative efficacies of supportive and cognitive behavioral group therapies for young children who have been sexually abused and their nonoffending mothers. Child Maltreatment 2001;6(4):332‐43. [DOI] [PubMed] [Google Scholar]
Deblinger 2011 {published data only}
- Deblinger E, Mannarino AP, Cohen JA, Runyon MK, Steer RA. Trauma‐focused cognitive behavioral therapy for children: impact of the trauma narrative and treatment length. Depression and Anxiety 2011;28(1):67‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannarino AP, Cohen JA, Deblinger E, Runyon MK, Steer RA. Trauma‐focused cognitive‐behavioral therapy for children: sustained impact of treatment 6 and 12 months later. Child Maltreatment 2012;17(3):231‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Diehle 2014 {published data only}
- Diehle J, Opmeer BC, Boer F, Mannarino AP, Lindauer RJL. Trauma‐focused cognitive behavioral therapy or eye movement desensitization and reprocessing: what works in children with posttraumatic stress symptoms? A randomized controlled trial. European Child and Adolescent Psychiatry 2014;24(2):227‐36. [DOI] [PubMed] [Google Scholar]
- Lindauer RJL. Effects of Trauma Focused Cognitive Behavioural Therapy (TF‐CBT) and Eye Movement Desensitization and Reprocessing (EMDR) for Children With Posttraumatic Stress Symptoms After Emergency Care. http://www.trialregister.nl/trialreg/admin/rctview.asp?TC=1814.
Dominguez 2001 {published data only}
- Dominguez RZ. Evaluation of cognitive‐behavioral and supportive treatments for sexually abused children: analyzing the process of change using individual growth curve analyses. Dissertation Abstracts International. University of Houston, 2001:5370.
Farkas 2010 {published data only}
- Farkas L. The effects of Motivation‐Adaptive Skills‐Trauma Resolution (MASTR) ‐ Eye Movement Desensitization and Reprocessing (EMDR) on traumatized adolescents with conduct problems. Dissertation Abstracts International: Section B: The Sciences and Engineering 2010;71(1‐B):655. [Google Scholar]
Glodich 2000 {published data only}
- Glodich A. Psychoeducational groups for adolescents exposed to violence and abuse: assessing the effectiveness of increasing knowledge of trauma to avert reenactment and risk‐taking behaviors. Dissertation Abstracts International. Massachusetts, United States: Smith College School for Social Work, 2000; Vol. 60, issue 9‐A:3527. [AAT 9945613.]
Jaberghaderi 2004 {published data only}
- Jaberghaderi N, Greenwald R, Rubin A, Dalatabadi S, Zand SO. A comparison of CBT and EMDR for sexually‐abused Iranian girls. 18th Annual Meeting, International Society for Traumatic Stress Studies, November 7 ‐ 10, Baltimore, MD. 2002.
- Jaberghaderi N, Greenwald R, Rubin A, Zand Shahin O, Dolatabadi S. A comparison of CBT and EMDR for sexually‐abused Iranian girls. Clinical Psychology and Psychotherapy 2004;11(5):358‐68. [Google Scholar]
Kazak 2004 {published data only}
- Kazak A, Alderfer M, Streisand R, Simms S, Rourke M, Barakat L, et al. Family treatment of posttraumatic stress in childhood cancer survival. 19th Annual Meeting, International Society for Traumatic Stress Studies, October 29 ‐ November 1, Chicago, IL. 2003.
- Kazak AE, Alderfer MA, Streisand R, Simms S, Rourke MT, Barakat LP, et al. Treatment of posttraumatic stress symptoms in adolescent survivors of childhood cancer and their families: a randomized clinical trial. Journal of Family Psychology 2004;18(3):493‐504. [DOI] [PubMed] [Google Scholar]
Kemp 2010 {published data only}
- Kemp M, Drummond P, McDermott B. A wait‐list controlled pilot study of eye movement desensitization and reprocessing (EMDR) for children with post‐traumatic stress disorder (PTSD) symptoms from motor vehicle accidents. Clinical Child Psychology and Psychiatry 2010;15(1):5‐25. [DOI] [PubMed] [Google Scholar]
Layne 2008 {published data only}
- Layne CM, Saltzman WR, Poppleton L, Burlingame GM, Pasalic A, Durakovic E, et al. Effectiveness of a school‐based group psychotherapy program for war‐exposed adolescents: a randomized controlled trial [NCT00480480]. Journal of the American Academy of Child and Adolescent Psychiatry 2008;47(9):1048‐62. [DOI] [PubMed] [Google Scholar]
Lieberman 2005 {published data only}
- Ghosh Ippen C, Harris WW, Horn P, Lieberman AF. Traumatic and stressful events in early childhood: can treatment help those at highest risk?. Child Abuse and Neglect 2011;35(7):504‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman AF, Ghosh Ippen C, Horn P. Child‐parent psychotherapy: 6‐month follow‐up of a randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry 2006;45:913–8. [DOI] [PubMed] [Google Scholar]
- Lieberman AF, Horn P, Ippen CG. Toward evidence‐based treatment: child‐parent psychotherapy with preschoolers exposed to marital violence. Journal of the American Academy of Child and Adolescent Psychiatry 2005;44(12):1241‐8. [DOI] [PubMed] [Google Scholar]
McMullen 2013 {published data only}
- McMullen J. Randomized Control Trial of Group Intervention With Former War‐Affected Boys in the Democratic Republic of Congo. http://clinicaltrials.gov/show/NCT01494831.
- McMullen J, O'Callaghan P, Shannon C, Black A, Eakin J. Group trauma‐focused cognitive‐behavioural therapy with former child soldiers and other war‐affected boys in the DR Congo: a randomised controlled trial. Journal of Child Psychology and Psychiatry 2013;54(11):1231‐41. [DOI] [PubMed] [Google Scholar]
O'Callaghan 2013 {published data only}
- O'Callaghan P, McMullen J, Shannon C, Rafferty H, Black A. A randomized controlled trial of trauma‐focused cognitive behavioral therapy for sexually exploited, war‐affected congolese girls. Journal of the American Academy of Child and Adolescent Psychiatry 2013;52(4):359‐69. [DOI] [PubMed] [Google Scholar]
O'Callaghan 2014 {published data only}
- O'Callaghan P, Branham L, Shannon C, Betancourt TS, Dempster M, McMullen JA. Pilot study of a family focused, psychosocial intervention with war‐exposed youth at risk of attack and abduction in north‐eastern Democratic Republic of Congo. Child Abuse and Neglect 2014;38:1197‐207. [NCT01542398] [DOI] [PubMed] [Google Scholar]
- Shannon C. Is a Family‐Based, Life Skills Focused Intervention Effective in Reducing Psychological Distress and Stigma and Improving Inter‐personal Relations and Functioning Among Former LRA Abductees and Other War‐Affected Children in Their Community in Dungu, the Democratic Republic of Congo?. http://clinicaltrialsgov/show/NCT01542398 2012.
Overbeek 2013 {published and unpublished data}
- Overbeek MM, Schipper JC, Lamers‐Winkelman F, Schuengel C. Effectiveness of specific factors in community‐based intervention for child‐witnesses of interparental violence: a randomized trial. Child Abuse and Neglect 2013;37:1202‐14. [DOI] [PubMed] [Google Scholar]
- Overbeek MM, Schipper JC, Lamers‐Winkelman F, Schuengel C. Risk factors as moderators of recovery during and after interventions for children exposed to interparental violence. American Journal of Orthopsychiatry 2014;84:295‐306. [DOI] [PubMed] [Google Scholar]
- Overbeek MM, Schipper JC, Lamers‐Winkelman F, Schuengel C. The effectiveness of a trauma‐focused psycho‐educational secondary prevention program for children exposed to interparental violence: study protocol for a randomized controlled trial. Trials 2012;13:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pace 2013 {published data only}
- Pace T, Negi L, Donaldson‐Lavelle B, Ozawa‐de SB, Reddy S, Cole S, et al. Cognitively‐based compassion training reduces peripheral inflammation in adolescents in foster care with high rates of early life adversity [abstract]. BMC Complementary and Alternative Medicine 2012;12(Suppl 1):P175. [Google Scholar]
- Pace TW, Negi LT, Dodson‐Lavelle B, Ozawa‐de SB, Reddy SD, Cole SP, et al. Engagement with cognitively‐based compassion training is associated with reduced salivary C‐reactive protein from before to after training in foster care program adolescents. Psychoneuroendocrinology 2013;38(2):294‐9. [DOI] [PubMed] [Google Scholar]
- Pace TWW, Negi LT, Adame DD, Cole SP, Sivilli TI, Brown TD, et al. Effect of compassion meditation on neuroendocrine, innate immune and behavioral responses to psychosocial stress. Psychoneuroendocrinology 2009;34(1):87‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy SD, Negi LT, Dodson‐Lavelle B, Ozawa‐de Silva B, Pace TW, Cole SP, et al. Cognitive‐based compassion training: a promising prevention strategy for at‐risk adolescents. Journal of Child and Family Studies 2013;22(2):219‐30. [Google Scholar]
Qouta 2012 {published data only}
- Diab M, Punamaki R‐L, Palosaari E, Qouta SR. Can psychosocial intervention improve peer and sibling relations among war‐affected children? Impact and mediating analyses in a randomized controlled trial. Social Development 2014;23:215‐31. [Google Scholar]
- Punamaki R‐L, Peltonen K, Diab M, Qouta SR. Psychosocial interventions and emotion regulation among war‐affected children: randomized control trial effects. Traumatology 2014;20:241‐52. [Google Scholar]
- Qouta SR, Palosaari E, Diab M, Punamaki R‐L. Intervention effectiveness among war‐affected children: a cluster randomized controlled trial on improving mental health. Journal of Traumatic Stress 2012;25(3):288‐98. [DOI] [PubMed] [Google Scholar]
Raider 2008 {published data only}
- Raider M C, Steele W, Delillo‐Storey M, Jacobs J, Kuban C. Structured sensory therapy (SITCAP‐ART) for traumatized adjudicated adolescents in residential treatment. Residential Treatment for Children and Youth 2008;25(2):167‐85. [Google Scholar]
Salloum 2008 {published data only}
- Salloum A. Group therapy for children after homicide and violence: a pilot study. Research on Social Work Practice 2008;18(3):198‐211. [Google Scholar]
- Salloum A, Overstreet S. Evaluation of individual and group grief and trauma interventions for children post disaster. Journal of Clinical Child and Adolescent Psychology 2008;37(3):495‐507. [DOI] [PubMed] [Google Scholar]
Salloum 2012 {published data only}
- Salloum A, Overstreet S, Salloum A, Overstreet S. Grief and trauma intervention for children after disaster: exploring coping skills versus trauma narration. Behaviour Research and Therapy 2012;50(3):169‐79. [DOI] [PubMed] [Google Scholar]
Schottelkorb 2012 {published data only}
- Schottelkorb AA, Doumas DM, Garcia R. Treatment for childhood refugee trauma: a randomized, controlled trial. International Journal of Play Therapy 2012;21(2):57‐73. [Google Scholar]
Shechtman 2010 {published data only}
- Shechtman Z, Mor M. Groups for children and adolescents with trauma‐related symptoms: outcomes and processes. International Journal of Group Psychotherapy 2010;60(2):221‐44. [DOI] [PubMed] [Google Scholar]
Shirk 2014 {published data only}
- Shirk SR, DePrince AP, Crisostomo PS, Labus J. Cognitive behavioral therapy for depressed adolescents exposed to interpersonal trauma: an initial effectiveness trial. Psychotherapy 2014;51:167‐79. [DOI] [PubMed] [Google Scholar]
Stallard 2006 {published data only}
- Stallard P. A randomised controlled trial to determine whether mental health problems and significant psychological distress in children involved in everyday road traffic accidents can be prevented. National Research Register 2003.
- Stallard P, Velleman R, Salter E, Howse I, Yule W, Taylor G. A randomised controlled trial to determine the effectiveness of an early psychological intervention with children involved in road traffic accidents. Journal of Child Psychology and Psychiatry and Allied Disciplines 2006;47(2):127‐34. [DOI] [PubMed] [Google Scholar]
- Stallard P, Velleman R, Salter E, Howse I, Yule W, Taylor G, et al. A randomised controlled trial to determine the effectiveness of an early intervention with child trauma victims. 31st Annual Conference of the British Association for Behavioural and Cognitive Psychotherapies; 2003 July 16 ‐ 19, York. 2003:83.
- Stallard P, Velleman R, Salter W, Howse I, Yule W, Taylor G, et al. Does early intervention prevent psychological distress in children involved in road traffic accidents? The results of a randomised controlled trial. 32nd Congress of the British Association for Behavioural and Cognitive Psychotherapies (jointly with the European Association of Behavioural and Cognitive Therapies); 2004 September 7 ‐ 11; Manchester. 2004:111.
Stein 2003 {published data only}
- Kataoka S, Jaycox LH, Wong M, Nadeem E, Langley A, Tang L, et al. Effects on school outcomes in low‐income minority youth: preliminary findings from a community‐partnered study of a school‐based trauma intervention. Ethnicity and Disease 2011;21(3 Suppl 1):S1‐71‐7. [PMC free article] [PubMed] [Google Scholar]
- Stein BD, Jaycox LH, Kataoka SH, Wong M, Tu W, Elliott MN, et al. A mental health intervention for schoolchildren exposed to violence: a randomized controlled trial. JAMA 2003;290(5):603‐11. [DOI] [PubMed] [Google Scholar]
Taussig 2010 {published data only}
- Taussig HN, Culhane SE. Impact of a mentoring and skills group program on mental health outcomes for maltreated children in foster care [NCT00809315]. Archives of Pediatrics and Adolescent Medicine 2010;164(8):739‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taussig HN, Culhane SE, Garrido E, Knudtson MD. RCT of a mentoring and skills group program: placement and permanency outcomes for foster youth. Pediatrics 2012;130(1):e33‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taussig HN, Culhane SE, Hettleman D. Fostering healthy futures: an innovative preventive intervention for preadolescent youth in out‐of‐home care. Child Welfare 2007;86(5):113‐31. [PMC free article] [PubMed] [Google Scholar]
Tol 2008 {published data only}
- Tol WA, Komproe IH, Jordans MJ, Susanty D, Jong JT. Developing a function impairment measure for children affected by political violence: a mixed methods approach in Indonesia. International Journal for Quality in Health Care 2011;23(4):375‐83. [DOI] [PubMed] [Google Scholar]
- Tol WA, Komproe IH, Jordans MJD, Gross AL, Susanty D, Macy RD, et al. Mediators and moderators of a psychosocial intervention for children affected by political violence. Journal of Consulting and Clinical Psychology 2010;78(6):818‐28. [DOI] [PubMed] [Google Scholar]
- Tol WA, Komproe IH, Susanty D, Jordans MJ, Macy RD, Jong JT. School‐based mental health intervention for children affected by political violence in Indonesia: a cluster randomized trial. JAMA 2008;300(6):655‐62. [DOI] [PubMed] [Google Scholar]
Tol 2012 {published data only}
- Tol WA, Komproe IH, Jordans MJ, Vallipuram A, Sipsma H, Sivayokan S, et al. Outcomes and moderators of a preventive school‐based mental health intervention for children affected by war in Sri Lanka: a cluster randomized trial. World Psychiatry 2012;11(2):114‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tol 2014 {unpublished data only}
- Tol WA, Komproe IH, Jordans MJD, Ndayisaba A, Ntamutumba P, Sipsma H, et al. School‐based mental health intervention for children in war‐affected Burundi: a cluster randomized trial. BMC Medicine 2014;12:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jong J. Efficacy of a School‐Based Psychosocial Intervention to Deal With the Psychosocial Impact of Armed Conflict on School‐Aged Children in Burundi. http://www.controlled‐trials.com/ISRCTN42284825.
Trowell 2002 {published data only}
- McCrone P, Weeramanthri T, Knapp M, Rushton A, Trowell J, Miles G, et al. Cost‐effectiveness of individual versus group psychotherapy for sexually abused girls. Child and Adolescent Mental Health 2005;10(1):26‐31. [DOI] [PubMed] [Google Scholar]
- Trowell J, Kolvin I. Lessons from a psychotherapy outcome study with sexually abused girls. Clinical Child Psychology and Psychiatry 1999;4(1):79‐89. [Google Scholar]
- Trowell J, Kolvin I, Weeramanthri T, Sadowski H, Berelowitz M, Glasser D, et al. Psychotherapy for sexually abused girls: psychopathological outcome findings and patterns of change. British Journal of Psychiatry 2002;180:234‐47. [DOI] [PubMed] [Google Scholar]
- Trowell JA, Berelowitz M, Kolvin I. In: Aveline M, Shapiro DA editor(s). Design and Methodological Issues in Setting Up a Psychotherapy Outcome Study With Girls Who Have Been Sexually Abused. Chichester: John Wiley, 1995. [Google Scholar]
Zehnder 2010 {published data only}
- Zehnder D, Meuli M, Landolt MA. Effectiveness of a single‐session early psychological intervention for children after road traffic accidents: a randomised controlled trial [NCT00296842]. Child and Adolescent Psychiatry and Mental Health 2010;4:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Berger 2007 {published data only}
- Berger R, Pat‐Horenczyk R, Gelkopf M. School‐based intervention for prevention and treatment of elementary‐students' terror‐related distress in Israel: a quasi‐randomized controlled trial. Journal of Traumatic Stress 2007;20(4):541‐51. [DOI] [PubMed] [Google Scholar]
Bolton 2007 {published data only}
- Betancourt T, Bolton P, Bass J, Murray L, Verdeli H, Clougherty K, et al. Phase III: a randomized controlled trial of mental health interventions for Acholi war‐affected youth in Gulu, Northern Uganda. 22nd Annual Meeting, International Society for Traumatic Stress Studies, November 4 ‐ 7 2006, Hollywood, CA. 2006:114.
- Bolton P, Bass J, Betancourt T, Speelman L, Onyango G, Clougherty K, et al. Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: a randomized controlled trial. JAMA 2007;298(5):519‐27. [DOI] [PubMed] [Google Scholar]
Burke 1988 {published data only}
- Burke MM. Short‐term group therapy for sexually abused girls: a learning theory based treatment for negative affect. PhD, University of Georgia, 1988.
Catani 2009 {published data only}
- Catani C, Kohiladevy M, Ruf M, Schauer E, Elbert T, Neuner F. Treating children traumatized by war and tsunami: a comparison between exposure therapy and meditation‐relaxation in North‐East Sri Lanka. BMC Psychiatry 2009;9:22. [DOI: 10.1186/1471-244X-9-22] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2014 {published data only}
- Chen Y, Shen WW, Gao K, Lam CS, Chang WC, Deng H. Effectiveness RCT of a CBT intervention for youths who lost parents in the Sichuan, China, earthquake. Psychiatric Services 2014;65:259‐62. [DOI] [PubMed] [Google Scholar]
Cohen 2004 {published data only}
- Cohen J, Mannarino A, Deblinger E, Steer R. A multisite treatment study for PTSD in sexually abused children. 19th Annual Meeting, International Society for Traumatic Stress Studies, October 29 ‐ November 1, Chicago, IL. 2003.
- Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse‐related PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(4):393‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deblinger E, Mannarino AP, Cohen JA, Steer RA. A follow‐up study of a multisite, randomized, controlled trial for children with sexual abuse‐related PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry 2006;45(12):1474‐84. [DOI] [PubMed] [Google Scholar]
Cooley‐Strickland 2011 {published data only}
- Cooley MR. Community Violence and Youth: Preventing Anxiety Disorders. http://clinicaltrialsgov/show/NCT00073619 2001. [NCT00073619]
- Cooley‐Strickland MR, Griffin RS, Darney D, Otte K, Ko J. Urban African American youth exposed to community violence: a school‐based anxiety preventive intervention efficacy study. Journal of Prevention and Intervention in the Community 2011;39(2):149‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dybdahl 2001 {published data only}
- Dybdahl R. Children and mothers in war: an outcome study of a psychosocial intervention program. Child Development 2001;72(4):1214‐30. [DOI] [PubMed] [Google Scholar]
Ehntholt 2005 {published data only}
- Ehntholt KA, Smith P, Yule W. School‐based CBT group intervention for refugee children who have experienced war‐related trauma. 31st Annual Conference of the British Association for Behavioural and Cognitive Psychotherapies; 2003 July 16 ‐ 19, York. 2003, issue 83.
- Ehntholt KA, Smith PA, Yule W. School‐based cognitive‐behavioural therapy group intervention for refugee children who have experienced war‐related trauma. Clinical Child Psychology and Psychiatry 2005;10(2):235‐50. [Google Scholar]
Ensink 2004 {published data only}
- Ensink K, Normandin L, Kernberg PF. Efficacy of a Reflective Functioning Treatment (RFT) for young sexually abused children. Society for Psychotherapy Research 35th Annual General Meeting Book of Abstracts. Rome, Italy, June 16 ‐ 19, 2004.
Ertl 2011 {published data only}
- Ertl V, Pfeiffer A, Schauer E, Elbert T, Neuner F. Community‐implemented trauma therapy for former child soldiers in Northern Uganda: a randomized controlled trial. JAMA 2011;306(5):503‐12. [DOI] [PubMed] [Google Scholar]
Gelkopf 2009 {published data only}
- Gelkopf M, Berger R. A school‐based, teacher‐mediated prevention program (ERASE‐Stress) for reducing terror‐related traumatic reactions in Israeli youth: a quasi‐randomized controlled trial. Journal of Child Psychology and Psychiatry, and Allied Disciplines 2009;50(8):962‐71. [DOI] [PubMed] [Google Scholar]
Gellman 2001 {published data only}
- Gellman AR. Guided imagery: exploring an alternative adjunctive intervention with traumatized adolescents in residential foster care. PhD dissertation, New York University, 2001.
Goenjian 1997 {published data only}
- Goenjian AK, Karayan I, Pynoos RS, Minassian D, Najarian LM, Steinberg AM, et al. Outcome of psychotherapy among early adolescents after trauma. American Journal of Psychiatry 1997;154(4):536‐42. [DOI] [PubMed] [Google Scholar]
Graham‐Bermann 2013 {published data only}
- Graham‐Bermann SA, Lynch S, Banyard V, DeVoe ER, Halabu H. Community‐based intervention for children exposed to intimate partner violence: an efficacy trial. Journal of Consulting and Clinical Psychology 2007;75:199‐209. [DOI] [PubMed] [Google Scholar]
- Graham‐Bermann SA, Miller LE. Intervention to reduce traumatic stress following intimate partner violence: an efficacy trial of the Moms' Empowerment Program (MEP). Psychodynamic Psychiatry 2013;41(2):329‐49. [DOI] [PubMed] [Google Scholar]
- Howell KH, Miller LE, Lilly MM, Graham‐Bermann SA. Fostering social competence in preschool children exposed to intimate partner violence: evaluating the preschool kids' club intervention. Journal of Aggression, Maltreatment and Trauma 2013;22(4):425‐45. [Google Scholar]
Hardin 2002 {published data only}
- Hardin SB, Weinrich S, Weinrich M, Garrison C, Addy C, Hardin TL. Effects of a long‐term psychosocial nursing intervention on adolescents exposed to catastrophic stress. Issues in Mental Health Nursing 2002;23(6):537‐51. [DOI] [PubMed] [Google Scholar]
Jacob 2014 {published data only}
- Jacob N, Neuner F, Maedl A, Schaal S, Elbert T. Dissemination of psychotherapy for trauma spectrum disorders in postconflict settings: a randomized controlled trial in Rwanda. Psychotherapy and Psychosomatics 2014;83:354‐63. [DOI] [PubMed] [Google Scholar]
- Schaal S. Phase 2: A Randomized Controlled Clinical Trial With Orphans and Widows Who Experienced the Genocide Carried Out by Trained Local Psychologists ‐ NET/IPT Versus Waiting List. ClinicalTrialsgov [wwwclinicaltrialsgov] 2007.
Jeffres 2004 {published data only}
- Jeffres MJ. The efficacy of EMDR with traumatized children. Dissertation Abstracts International 2004:4042.
Jensen 2014 {published data only}
- Jensen TK. Trauma‐Focused Cognitive‐Behavioural Therapy for Children: A Study of Process and Outcome. http://www.clinicaltrials.gov/ct2/show/NCT00635752 issue accessed 1‐10‐13.
- Jensen TK, Holt T, Ormhaug SM, Egeland K, Granly L, Hoaas LC, et al. A randomized effectiveness study comparing trauma‐focused cognitive behavioral therapy with therapy as usual for youth. Journal of Clinical Child and Adolescent Psychology 2014;43:356‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormhaug SM, Jensen TK, Wentzel‐Larsen T, Shirk SR. The therapeutic alliance in treatment of traumatized youths: relation to outcome in a randomized clinical trial. Journal of Consulting and Clinical Psychology 2014;82:52‐64. [DOI] [PubMed] [Google Scholar]
Jordans 2010 {published data only}
- Jordans MJ, Komproe IH, Tol WA, Kohrt BA, Luitel NP, Macy RD, et al. Evaluation of a classroom‐based psychosocial intervention in conflict‐affected Nepal: a cluster randomized controlled trial [ISRCTN48004304]. Journal of Child Psychology and Psychiatry, and Allied Disciplines 2010;51(7):818‐26. [DOI] [PubMed] [Google Scholar]
Kassam‐Adams 2011 {published data only}
- Kassam‐Adams N, Garcia‐Espana JF, Marsac ML, Kohser KL, Baxt C, Nance M, et al. A pilot randomized controlled trial assessing secondary prevention of traumatic stress integrated into pediatric trauma care. Journal of Traumatic Stress 2011;24(3):252‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kataoka 2003 {published data only}
- Kataoka SH, Stein BD, Jaycox LH, Wong M, Escudero P, Tu W, et al. A school‐based mental health program for traumatized Latino immigrant children. Journal of the American Academy of Child and Adolescent Psychiatry 2003;42(3):311‐8. [DOI] [PubMed] [Google Scholar]
Kenardy 2008 {published data only}
- Kenardy J, Thompson K, Brocque R, Olsson K. Information provision intervention for children and their parents following pediatric accidental injury. European Child and Adolescent Psychiatry 2008;17(5):316‐25. [DOI] [PubMed] [Google Scholar]
King 2000 {published data only}
- King NJ, Tonge BJ, Mullen P, Myerson N, Heyne D, Rollings S, et al. Treating sexually abused children with posttraumatic stress symptoms: a randomized clinical trial. Journal of the American Academy of Child & Adolescent Psychiatry 2000;39(11):1347‐55. [DOI] [PubMed] [Google Scholar]
Krueger 2013 {published data only}
- Krueger SJ. Cognitive behavioral and integrative treatment of abused children: examining cognitive and emotional processes and developmental considerations. Dissertation Abstracts International: Section B: The Sciences and Engineering 2013; Vol. 74.
Lyshak‐Stelzer 2007 {published data only}
- Lyshak‐Stelzer F, Singer P, John P, Chemtob CM. Art therapy for adolescents with posttraumatic stress disorder symptoms: a pilot study. Art Therapy 2007;24(4):163‐9. [Google Scholar]
McWhirter 2011 {published data only}
- McWhirter PT. Differential therapeutic outcomes of community‐based group interventions for women and children exposed to intimate partner violence. Journal of Interpersonal Violence 2011;26(12):2457‐82. [DOI] [PubMed] [Google Scholar]
Murray 2015 {published data only}
- Murray LK, Skavenski S, Kane JC, Mayeya J, Dorsey S, Cohen JA, et al. Effectiveness of trauma‐focused cognitive behavioral therapy among trauma‐affected children in Lusaka, Zambia: a randomized clinical trial. JAMA Pediatriatics 2015;169(8):761‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pfeffer 2002 {published data only}
- Pfeffer CR, Jiang H, Kakuma T, Hwang J, Metsch M. Group intervention for children bereaved by the suicide of a relative. Journal of the American Academy of Child and Adolescent Psychiatry 2002;41(5):505‐13. [DOI] [PubMed] [Google Scholar]
Phipps 2012 {published data only}
- Phipps S, Peasant C, Barrera M, Alderfer MA, Huang Q, Vannatta K. Resilience in children undergoing stem cell transplantation: results of a complementary intervention trial. Pediatrics 2012;129(3):e762‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosner 2014 {published data only}
- Rimane E, Rosner R. Developmentally Adapted Cognitive Processing Therapy for Adolescents and Young Adults With PTSD Symptoms After Physical and Sexual Abuse ‐ D‐CPT. http://wwwdrksde/DRKS00004787 2013. [DOI] [PMC free article] [PubMed]
- Rosner R, Konig HH, Neuner F, Schmidt U, Steil R. Developmentally adapted cognitive processing therapy for adolescents and young adults with PTSD symptoms after physical and sexual abuse: study protocol for a randomized controlled trial. Trials 2014;15:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rubin 2001 {published data only}
- Rubin A, Bischofshausen S, Conroy‐Moore K, Dennis B, Hastie M, Melnick L, et al. The effectiveness of EMDR in a child guidance center. Research on Social Work Practice 2001;11(4):435‐57. [Google Scholar]
Ruf 2010 {published data only}
- Ruf M, Schauer M, Neuner F, Catani C, Elbert T. World Psychiatric Association, International Congress; 2006 July 12 ‐ 16; Istanbul, Turkey. 2006:146.
- Ruf M, Schauer M, Neuner F, Catani C, Schauer E, Elbert T. Narrative exposure therapy for 7‐ to 16‐year‐olds: a randomized controlled trial with traumatized refugee children. Journal of Traumatic Stress 2010;23(4):437‐45. [DOI] [PubMed] [Google Scholar]
Ruf 2012 {unpublished data only}
- Ruf M. Lifeline‐NET (Narrative Exposure Therapy): a short‐term treatment for traumatized refugees and asylum seekers. https://clinicaltrials.gov/show/NCT01720732 2012.
Saxe 2012 {published data only}
- Saxe GN, Heidi EB, Fogler J, Navalta CP. Innovations in practice: preliminary evidence for effective family engagement in treatment for child traumatic stress‐trauma systems therapy approach to preventing dropout. Child and Adolescent Mental Health 2012;17(1):58‐61. [DOI] [PubMed] [Google Scholar]
Schaal 2009 {published data only}
- Schaal S, Elbert T, Neuner F. Narrative exposure therapy versus interpersonal psychotherapy: a pilot randomized controlled trial with Rwandan genocide orphans. Psychotherapy and Psychosomatics 2009;78(5):298‐306. [DOI] [PubMed] [Google Scholar]
Schauer 2008 {unpublished data only}
- Schauer E. Trauma treatment for children in war: build‐up of an evidence‐based large‐scale mental health intervention in north‐eastern Sri Lanka. PhD thesis submitted to Konstanz University, 2008.
Scheeringa 2011 {published data only}
- Scheeringa MS, Weems CF, Cohen JA, Amaya‐Jackson L, Guthrie D. Trauma‐focused cognitive‐behavioral therapy for posttraumatic stress disorder in three‐through six year‐old children: a randomized clinical trial. Journal of Child Psychology & Psychiatry and Allied Disciplines 2011;52(8):853‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shelby 1995 {published data only}
- Shelby JS. Crisis intervention with children following Hurricane Andrew: a comparison of two treatment approaches. Dissertation Abstracts International 1995:1121.
Shooshtary 2008 {published data only}
- Shooshtary MH, Panaghi L, Moghadam JA. Outcome of cognitive behavioral therapy in adolescents after natural disaster. Journal of Adolescent Health 2008;42(5):466‐72. [DOI] [PubMed] [Google Scholar]
Soltanifar 2012 {unpublished data only}
- Soltanifar A. The Efficacy of Developmental Attachment‐Based Play Therapy on Developmental Trauma Disorder Symptoms in Children From 3 to 9 Years Old. Iranian Registry of Clinical Trials, http://www.irct.ir/searchresult.php?id=5280&number=8.
- Soltanifar A, Rezaei Ardani A, Soltanifar A, Jafarzadeh Fadaki M, Modarres Gharavi M, Mokhber N. Attachment‐based play therapy for Iranian children and parenting stress of their mothers. Middle‐East Journal of Scientific Research 2013;18(4):432‐37. [Google Scholar]
Stronach 2012 {published data only}
- Stronach EP. Preventive interventions and sustained attachment security in maltreated children: a 12‐month follow‐up of a randomized controlled trial dissertation. Dissertation Abstracts International 2013; Vol. 74, issue 3‐B(E). [DOI] [PMC free article] [PubMed]
- Stronach EP, Toth SL, Rogosch F, Cicchetti D. Preventive interventions and sustained attachment security in maltreated children. Development and Psychopathology 2013;25(4):919‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thabet 2005 {published data only}
- Thabet AA, Vostanis P, Karim K. Group crisis intervention for children during ongoing war conflict. European Child and Adolescent Psychiatry 2005;14(5):262‐9. [DOI] [PubMed] [Google Scholar]
Wang 2011 {published data only}
- Wang Z‐Y, Yang F, Wang Y‐Y, Gao J, Qian M‐Y. Effects of group intervention on depression and post‐traumatic stress symptoms among junior middle school students in earthquake area. Chinese Mental Health Journal 2011;25(4):284‐8. [Google Scholar]
Wolmer 2011a {published data only}
- Wolmer L, Hamiel D, Laor N. Preventing children's posttraumatic stress after disaster with teacher‐based intervention: a controlled study. Journal of the American Academy of Child and Adolescent Psychiatry 2011;50(4):340‐8. [DOI] [PubMed] [Google Scholar]
Wolmer 2011b {published data only}
- Wolmer L, Hamiel D, Barchas JD, Slone M, Laor N. Teacher‐delivered resilience‐focused intervention in schools with traumatized children following the second Lebanon War. Journal of Traumatic Stress 2011;24(3):309‐16. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Crombach 2012 {unpublished data only}
- Crombach A. Treatment of Aggressive Behavior and Post‐Traumatic Stress Disorder. http://www.clinicaltrials.gov/ct2/show/NCT01519193.
Elbert 2009 {unpublished data only}
- Elbert T. Trauma and Truth Interventions (NET) Versus Conflict Resolution and Social Skills Trainings for Vulnerable Youths in Northern Uganda. http://clinicaltrials.gov/ct2/show/NCT00893750.
Elbert 2013 {unpublished data only}
- Elbert T. MemoTV: Epigenetic, Neural and Cognitive Memories of Traumatic Stress and Violence in Former Offenders of the Townships of South Africa. http://clinicaltrialsgov/show/NCT02012738 2013.
Hultmann 2012 {unpublished data only}
- Hultmann O. Identification and Treatment of Children Exposed or Subjected to Intimate Partner Violence or Child Abuse in Sweden. http://www.controlled‐trials.com/ISRCTN58027256.
Jessiman 2013 {unpublished data only}
- Jessiman P. Letting the Future In: Therapeutic Intervention for Child Sexual Abuse – Randomised Trial. http://www.controlled‐trials.com/ISRCTN65340805.
Kassam‐Adams 2016 {published and unpublished data}
- Kassam‐Adams N, Marsac ML, Kohser KL, Kenardy J, March S, Winston FK. Pilot Randomized Controlled Trial of a Novel Web‐Based Intervention to Prevent Posttraumatic Stress in Children Following Medical Events. Journal of Pediatric Psychology 2015;41(1):138‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsac ML, Kohser KL, Winston FK, Kenardy J, March S, Kassam‐Adams N. Using a web‐based game to prevent posttraumatic stress in children following medical events: design of a randomized controlled trial. European Journal of Psychotraumatology 2013;4:21311. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kramer 2014 {unpublished data only}
- Landolt M. Psychological Interventions in Children After Road Traffic Accidents or Burns: A Randomized Controlled Study. http://clinicaltrials.gov/show/NCT01085370.
Mahmoudi‐Gharaei 2006 {published data only}
- Mahmoudi‐Gharaei J, Mohammadi M, Bina M, Yasami M, Fakour Y. Supportive and cognitive behavioral group interventions on Bam earthquake related PTSD symptoms in adolescents. Tehran University Medical Journal 2006;64(8):57‐67. [Google Scholar]
Narimani 2013 {published data only}
- Narimani M, Basharpoor S, Gamarigive H, Abolgasemi A. Impact of cognitive processing and holographic reprocessing on posttraumatic symptoms improvement amongst Iranian students. Advances in Cognitive Science 2013;15:50‐62. [Google Scholar]
Ooi 2010 {unpublished data only}
- Ooi C. A Pretest Posttest 3‐Month Follow‐up Randomised Controlled Trial of a Group Intervention "Teaching Recovery Techniques" to Prevent Worsening of Early Posttraumatic Stress Symptoms in Young Migrants. http://www.anzctr.org.au/ACTRN12611000948998.aspx.
Rowe 2013 {published data only}
- Rowe C. Family‐Based Drug Services for Young Disaster Victims (Katrina). ClinicalTrials.gov 2013; Vol. https://clinicaltrials.gov/ct2/show/NCT01859000.
- Rowe CL, Greca AM, Alexandersson A. Family and individual factors associated with substance involvement and PTS symptoms among adolescents in greater New Orleans after Hurricane Katrina. Journal of Consulting and Clinical Psychology 2010;78(6):806‐17. [DOI] [PubMed] [Google Scholar]
Ruggiero 2015 {published data only}
- Ruggiero KJ. Web‐based Intervention for Disaster‐Affected Youth and Families. http://clinicaltrials.gov/show/NCT01606514.
- Ruggiero KJ, Davidson TM, McCauley J, Gros KS, Welsh K, Price M, et al. Bounce Back Now! Protocol of a population‐based randomized controlled trial to examine the efficacy of a web‐based intervention with disaster‐affected families. Contemporary Clinical Trials 2015;40:138‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggiero KJ, Price M, Adams Z, Stauffacher K, McCauley J, Danielson CK, Knapp R, Hanson RF, Davidson TM, Amstadter AB, Carpenter MJ, Saunders BE, Kilpatrick DG, Resnick HS. Web intervention for adolescents affected by disaster: population‐based randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry 2015;54(9):709‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shen 2012 {published data only}
- Shen P‐Y, Zhu X‐Y, Xin Y. Effects of expressive group counseling on psychological well‐being in children after earthquake. Chinese Mental Health Journal 2012;26:466‐70. [Google Scholar]
Zang 2013 {published and unpublished data}
- Zang Y. Resilience and Implications From Writings of Children Traumatised by the Earthquake: A Study of Guided Narrative Technique. Chinese Clinical Trial Registry (ChiCTR), http://www.chictr.org/en/proj/show.aspx?proj=4143.
- Zang Y. The Effect of a Guided Narrative Technique Among Children Traumatised by the Earthquake: Pilot Study. Chinese Clinical Trial Registry (ChiCTR), http://www.chictr.org/en/proj/show.aspx?proj=4142.
- Zang Y, Hunt N, Cox T. The effect of guided narrative technique among children traumatised by the earthquake. In: Barrette C, Haylock B, Mortimer D editor(s). Trauma Imprints: Performance, Art, Literature and Theoretical Practice. 1st Edition. Oxford, UK: Inter‐disciplinary Press, 2011:173‐282. [ISBN: 978‐1‐84888‐085‐6] [Google Scholar]
References to ongoing studies
Belcher 2009 {unpublished data only}
- Belcher HME. FamilyLive Feasibility and Effectiveness Study. http://www.clinicaltrials.gov/ct2/show/NCT01524185 issue accessed 1‐10‐13.
Dorsey 2012 {unpublished data only}
- Dorsey S, Whetten K. Randomized Controlled Trial of Trauma‐Focused CBT in Tanzania and Kenya. http://clinicaltrials.gov/ct2/show/NCT01822366.
Roos 2013 {unpublished data only}
- Roos. A Randomized Comparison of Eye Movement Desensitization and Reprocessing (EMDR) and Cognitive Behavioral Writing Therapy (CBWT) in Pediatric Posttraumatic Stress Disorder Following Single‐Incident Trauma NTR3870. http://www.trialregister.nl/trialreg/admin/rctview.asp?TC=3870. [NTR3870] [DOI] [PubMed]
Sansom‐Daly 2012 {unpublished data only}
- Sansom‐Daly UM, Wakefield CE, Bryant RA, Butow P, Sawyer S, Patterson P, et al. Online group‐based cognitive‐behavioural therapy for adolescents and young adults after cancer treatment: a multicenter randomised controlled trial of Recapture Life‐AYA. BMC Cancer 2012;12:339. [DOI] [PMC free article] [PubMed] [Google Scholar]
Toth 2011 {unpublished data only}
- Toth S, Todd J. Prevention of Depression in Maltreated and Nonmaltreated Adolescents. http://clinicaltrials.gov/show/NCT01534377.
Additional references
AACAP 1998
- American Academy of Child, Adolescent Psychiatry. Practice parameters for the assessment and treatment of children and adolescents with posttraumatic stress disorder. Journal of the American Academy of Child and Adolescent Psychiatry 1998;37 Suppl 10:4‐26. [DOI] [PubMed] [Google Scholar]
AACAP 2010
- Cohen JA, Bukstein O, Walter H, Benson RS, Chrisman A, Farchione TR, et al. Practice parameter for the assessment and treatment of children and adolescent with posttraumatic stress disorder. Journal of the American Academy of Child and Adolescent Psychiatry 2010;49(4):414‐30. [PubMed] [Google Scholar]
Achenbach 1983
- Achenbach TM, Edelbrock CS. Manual for the Child Behavior Checklist. Burlington, VT: University of Vermont, Department of Psychiatry, 1983. [Google Scholar]
APA 2000
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV‐TR). 4th Edition. Washington, DC: American Psychiatric Association, 2000:463‐468. [Google Scholar]
Bisson 2013
- Bisson JI, Roberts NP, Andrew M, Cooper R, Lewis C. Psychological therapies for chronic post‐traumatic stress disorder (PTSD) in adults. Cochrane Database of Systematic Reviews 2013, Issue 12. [DOI: 10.1002/14651858.CD003388.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
BluePages 2012
- BluePages. http://bluepages.anu.edu.au/treatments/what_works/psychological_treatments/ (accessed 20 August 2012).
Bryant 2001
- Bryant RA, Friedman M. Medication and non‐medication treatments of post‐traumatic stress disorder. Current Opinion in Psychiatry 2001;14(2):119‐23. [Google Scholar]
Carr 2004
- Carr A. Interventions for post‐traumatic stress disorder in children and adolescents. Pediatric Rehabilitation 2004;7(4):231‐44. [DOI] [PubMed] [Google Scholar]
Donnelly 2002
- Donnelly CL, Amaya‐Jackson L. Post‐traumatic stress disorder in children and adolescents: epidemiology, diagnosis and treatment options. Paediatric Drugs 2002;4(3):159‐70. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fletcher 2003
- Fletcher KE. Childhood posttraumatic stress disorder. In: Mash EJ, Barkley RA editor(s). Child Psychopathology. 2nd Edition. New York, NY: The Guildford Press, 2003:330‐71. [Google Scholar]
Foa 1997
- Foa EB, Meadows EA. Psychosocial treatments for posttraumatic stress disorder: a critical review. Annual Review of Psychology 1997;48:449‐80. [DOI] [PubMed] [Google Scholar]
Forman‐Hoffman 2013
- Forman‐Hoffman VL, Zolotor AJ, McKeeman JL, Blanco R, Knauer SR, Lloyd SW, et al. Comparative effectiveness of interventions for children exposed to nonrelational traumatic events. Pediatrics 2013;131(3):526‐39. [DOI] [PubMed] [Google Scholar]
Foy 1996
- Foy DW, Madvig BT, Pynoos RS, Camilleri AJ. Etiologic factors in the development of posttraumatic stress disorder in children and adolescents. Journal of School Psychology 1996;34(2):133‐45. [Google Scholar]
Gillies 2012
- Gillies D, Taylor F, Gray C, O'Brien L, D'Abrew N. Psychological therapies for the treatment of post‐traumatic stress disorder in children and adolescents. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD006726.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Henken 2007
- Henken T, Huibers MJ, Churchill R, Restifo KK, Roelofs JJ. Family therapy for depression. Cochrane Database of Systematic Reviews 2007, Issue Issue 3. Art. No.: CD006728. [DOI: 10.1002/14651858.CD006728] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: Wiley Blackwell, 2008. [Google Scholar]
Kovacs 1992
- Kovacs M. Children's Depression Inventory. https://www.mhs.com/ecom/(3jkh5055rnqsekfhnxgzn145)/TechBrochures/CDI.pdf 1992 (accessed 18 May 2007).
Kramer 2011
- Kramer DN, Landolt MA. Characteristics and efficacy of early psychological interventions in children and adolescents after single trauma: a meta‐analysis. European Journal of Psychotraumatology 2011;2:7858. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leenarts 2013
- Leenarts LE, Diehle J, Doreleijers TA, Jansma EP, Lindauer RJ. Evidence‐based treatments for children with trauma‐related psychopathology as a result of childhood maltreatment: a systematic review. European Child and Adolescent Psychiatry 2012;22(5):269‐83. [DOI] [PubMed] [Google Scholar]
MacDonald 2012
- Macdonald G, Higgins JPT, Ramchandani P, Valentine JC, Bronger LP, Klein P, et al. Cognitive‐behavioural interventions for children who have been sexually abused. Cochrane Database of Systematic Reviews 2012, Issue 5. [DOI: 10.1002/14651858.CD001930; Art. No.: CD001930.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
McNally 1996
- McNally RJ. Assessment of posttraumatic stress disorder in children and adolescents. Journal of School Psychology 1996;3(2):147‐61. [Google Scholar]
Neuner 2004
- Neuner F, Schauer M, Klaschik C, Karunakara U, Elbert T. A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. Journal of Consulting and Clinical Psychology 2004;72(4):579‐87. [DOI] [PubMed] [Google Scholar]
Parry‐Jones 1995
- Parry‐Jones W, Barton J. Post‐traumatic stress disorder in children and adolescents. Current Opinion in Psychiatry 1995;8(4):227‐30. [Google Scholar]
Perrin 2000
- Perrin S, Smith P, Yule W. Practitioner review: the assessment and treatment of post‐traumatic stress disorder in children and adolescents. Journal of Child Psychology and Psychiatry and Allied Disciplines 2000;41(3):277‐89. [PubMed] [Google Scholar]
Roberts 2010
- Roberts NP, Kitchiner NJ, Kenardy J, Bisson JI. Early psychological interventions to treat acute traumatic stress symptoms. Cochrane Database of Systematic Reviews 2010, Issue 3. [DOI: 10.1002/14651858.CD007944.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Robertson 2004
- Robertson M, Humphreys L, Ray R. Psychological treatments for posttraumatic stress disorder: recommendations for the clinician based on a review of the literature. Journal of Psychiatric Practice 2004;10(2):106‐18. [DOI] [PubMed] [Google Scholar]
Rose 2002
- Rose S, Bisson J, Churchill R, Wessely S. Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews 2002, Issue Issue 2. Art. No.: CD000560. [DOI: 10.1002/14651858.CD000560] [DOI] [PubMed] [Google Scholar]
Saigh 1996
- Saigh PA, Green BL, Korol M. The history and prevalence of posttraumatic stress disorder with special reference to children and adolescents. Journal of School Psychology 1996;34(2):107‐31. [Google Scholar]
Saigh 2000
- Saigh PA, Yasik AE, Oberfield RA, Green BL, Halamandaris PV, Rubenstein H, et al. The Children's PTSD Inventory: development and reliability. Journal of Traumatic Stress 2000;13(3):369‐80. [DOI] [PubMed] [Google Scholar]
Schaffer 1983
- Schaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, et al. A Children's Global Assessment Scale (CGAS). Archives of General Psychiatry 1983;40(11):1228‐31. [DOI] [PubMed] [Google Scholar]
Sones 2011
- Sones HM, Thorp SR, Raskind M. Prevention of posttraumatic stress disorder. Psychiatric Clinics of North America 2011;34(1):79‐94. [DOI] [PubMed] [Google Scholar]
Spielberger 1973
- Spielberger CD. Manual for the State‐Trait Anxiety Inventory for Children. Palo Alto, CA: Consulting Psychologists Press, 1973. [Google Scholar]
Varni 2001
- Varni JW, Seid M, Kurtin PS. PedsQL™ 4.0: reliability and validity of the Pediatric Quality of Life Inventory™ Version 4.0 generic core scales in healthy and patient populations. Medical Care 2001;39(8):800‐12. [DOI] [PubMed] [Google Scholar]
WHO 1990
- World Health Organization. Chapter V. Mental and behavioural disorders (F40‐F48). International Classification of Diseases 10. Geneva: World Health Organization, 1990:www3.who.int/icd/currentversion/gf40.htm (accessed 6 September 2006). [Google Scholar]
Yule 2001
- Yule W. Post‐traumatic stress disorder in children and adolescents. International Review of Psychiatry 2001;13(3):194‐200. [Google Scholar]
References to other published versions of this review
Gillies 2007
- Gillies D, O'Brien L, Rogers P, Meekings C. Psychological therapies for the prevention and treatment of post‐traumatic stress disorder in children and adolescents (Protocol). Cochrane Database of Systematic Reviews 2007, Issue Issue 3. Art. No.: CD006726. [DOI: 10.1002/14651858] [DOI] [PMC free article] [PubMed] [Google Scholar]


