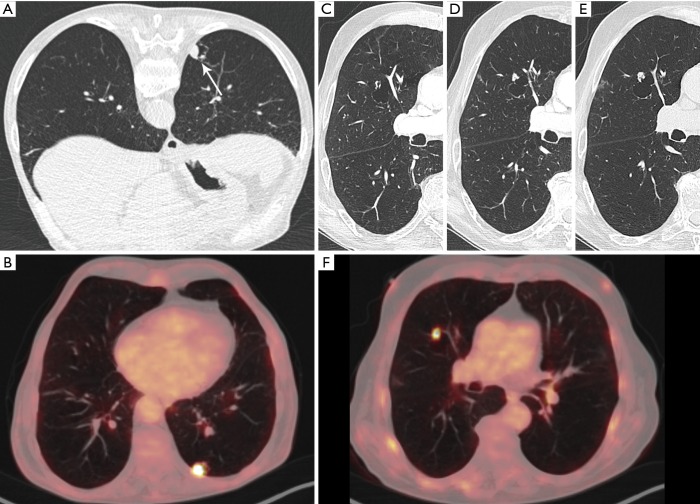
Figure 3.
A 76-year-old man was referred to the radiology department for CT-guided transthoracic biopsy. (A) Axial CT-image (prone position) in lung window setting showed a cystic airspace lesion with an endophytic solid nodule (white arrow). (B) An 18F-FDG-PET was previously performed for further evaluation and showed a high uptake in the nodule/solid part of the cystic airspace lesion. Histopathologic examination showed an infiltrating squamous cell carcinoma. At the time of diagnosis, there was a thin-walled cystic lesion in the right upper lobe, with no signs of a solid component or adjacent nodule (C). First follow-up chest CT 6 months after the initial examination showed a new exophytic solid nodule abutting the cyst wall (D). CT-examination another 3 months later showed (E) despite the short time interval a clear increase in size of the solid component. 18F-FDG-PET at that moment showed—in regard to the small size of the nodule—an intense uptake (F). No definitive diagnosis could be obtained due to the patient’s clinical status. The lesion was presumed to be a new lung cancer and the patient was treated with radiotherapy. CT, computed tomography; 18F-FDG-PET, 18F-fluorodeoxyglucose positron emission tomography.