Abstract
Background: To inform global health policies and resources planning, this paper analyzes evolving trends in physical rehabilitation needs, using data on Years Lived with Disability (YLDs) from the Global Burden of Disease Study (GBD) 2017. Methods: Secondary analysis of how YLDs from conditions likely benefiting from physical rehabilitation have evolved from 1990 to 2017, for the world and across countries of varying income levels. Linear regression analyses were used. Results: A 66.2% growth was found in estimated YLD Counts germane to physical rehabilitation: a significant and linear growth of more than 5.1 billion YLDs per year (99% CI: 4.8–5.4; r2 = 0.99). Low-income countries more than doubled (111.5% growth) their YLD Counts likely benefiting from physical rehabilitation since 1990. YLD Rates per 100,000 people and the percentage of YLDs likley benefiting from physical rehabilitation also grew significantly over time, across locations (all p > 0.05). Finally, only in high-income countries did Age-standardized YLD Rates significantly decrease (p < 0.01; r2 = 0.86). Conclusions: Physical rehabilitation needs have been growing significantly in absolute, per-capita and in percentage of total YLDs. This growth was found globally and across countries of varying income level. In absolute terms, growths were higher in lower income countries, wherein rehabilitation is under-resourced, thereby highlighting important unmet needs.
Keywords: rehabilitation, global health, disability, global burden of disease, health services needs and demand
1. Introduction
Worldwide rehabilitation needs are growing in tandem with global population growth, population aging, and higher survival rates for people with severe health conditions and disability [1,2,3]. However, to our knowledge, there is no up-to-date, systematic analysis quantifying worldwide epidemiological trends for the whole set of health conditions likely benefiting from physical rehabilitation. In this paper, we analyze how the global needs for physical rehabilitation have evolved from 1990 to 2017, using data from the Global Burden of Disease Study (GBD) 2017.
The GBD study, which has incorporated data since 1990, is the most comprehensive global epidemiological study to date. It combines data from the best available sources (e.g., scientific literature, official statistics from ministries of health, household surveys, vital registries, hospital data, claims data [4,5]), processed with increasingly sophisticated modelling approaches (e.g., a continuously updated Bayesian meta-regression tool) to provide rigorous global, regional, and national estimates of relevant population health. The data sources used to ground the estimates are colossal and have increased for each cycle of the GBD study. Most recently, the GBD 2017 used a total of 15,449 scientific literature sources (6.5% and 47,4% more than the GBD 2106 and GBD 2015 cycles, respectively), 21,100 sources of epidemiological surveillance data (12.3% and 49.9% more than GDB 2016 and GBD 2015, respectively), and data from an additional 148,842,107 hospital admissions globally, bringing the total number of admissions that inform GBD estimation to more than 2.6 billion [5,6].
For the first time in the study’s history, the GBD 2017 reports data on injuries in terms of their nature or consequence (e.g., hip fracture or spinal cord injury), in addition to and apart from their cause (e.g., falls, road injuries, interpersonal violence) [6]. This new type of data is particularly germane to the planning of services and resources in physical rehabilitation.
Others have used GBD study data to examine rehabilitation needs [7,8]. In the more recent example, the World Health Organization (WHO) used data from the GBD 2015 to examine worldwide needs for mental and physical rehabilitation. They found a 17.6% increase from 2005 to 2015 in Years Lived Disability (YLDs) for health conditions associated with severe disability, and that a remarkable 75% of the total world’s YLDs in 2015 came from health conditions germane to rehabilitation [7]. However, the WHO study did not examine physical rehabilitation needs distinct from the rehabilitation of mental health conditions. Moreover, health conditions with mild disability weights were not considered.
In addition to the WHO’s analysis, a number of studies have used GBD data to examine particular conditions likely benefiting from physical rehabilitation, such as injuries (i.e., their causes) [9], musculoskeletal conditions [10,11], neurological disorders [12,13], stroke [14], cardiovascular diseases [15], chronic respiratory diseases [16], cancer [17], or HIV [18]. However, to our knowledge, no study has used current GBD data to examine YLDs and potential needs for rehabilitation for the broad spectrum of conditions potentially benefiting from physical rehabilitation.
Using publicly available data from the GBD 2017, this paper aimed to provide a systematic global analysis of YLDs for the combined set of health conditions likely benefiting from physical rehabilitation, and specifically answer the following study questions:
How large are the estimated world’s YLDs (i.e., YLD counts, YLDs rates per 100,000 peole, and age-standardized YLD rates) likely benefiting from physical rehabilitation in 2017?
What is the percentage of the world’s YLDs likely benefiting from physical rehabilitation relative to total YLDs?
Did any of these estimates change significantly over time (i.e., since 1990)? If so, by how much? and, finally,
Did any of those trends differ across countries of varying income levels?
The answer to these questions would provide valuable benchmarks to inform global and local health and rehabilitation policies, research, and advocacy. Moreover, such findings could provide direction to funding priorities, as well as timely information for health system planning and strengthening activities, including for determining needs for physical rehabilitation services, as a means to allocate resources accordingly.
2. Methods
2.1. Study Design
Systematic, secondary analysis of public-domain data from the GBD 2017, extracted from the freely-available web platform: the Global Health Data Exchange tool (http://ghdx.healthdata.org/gbd-results-tool).
2.2. Data Selection
From the list of YLD “causes” (i.e., underlying health conditions), “impairments” (i.e., consequences of injury or diseases that have more than one diagnostic cause) and “injuries” (i.e., the nature of the injury), the authors selected those deemed likely to benefit from physical rehabilitation, as described below. Given that YLDs from “causes” are collective exhaustive, to avoid double counting, we do not cumulatively select YLDs from Injuries as a “cause”, but only YLDs from the nature of the injury. In addition, YLDs from “impairments” were limited to those not coming from “causes” we had already selected.
We found no global standard to inform which health conditions potentially benefit from physical rehabilitation; thus, in determining which conditions to focus on as potentially benefitting from physical rehabilitation, we relied on the following: previous works using GBD data for rehabilitation [7,8,19]; papers analyzing publication trends in physical rehabilitation and physical therapy across conditions [20,21,22]; and finally on the below working definition [23,24,25,26,27,28].
Physical rehabilitation uses health-based approaches to optimize physical function and participation in persons with physical impairments (e.g., mobility) or symptoms (e.g., low back pain) that are amenable to recovery, prevention, or management from physical rehabilitation services, facilities or providers (e.g., physical or occupational therapists). From this definition, we excluded rehabilitation of people with oral, mental health, substance abuse disorders, intellectual or sensory impairments per se, although partial overlap often occurs across different forms of rehabilitative interventions for those conditions. Table 1 provides the full list of the included conditions.
Table 1.
List of GBD causes, injuries and impairments selected as generating YLDs that might potentially benefit from physical rehabilitation.
| Causes |
|---|
| Communicable, Maternal, Neonatal or Nutritional: |
| • HIV/AIDs |
| • Leprosy; Zika |
| • Meningitis, Encephalitis; Tetanus |
| • Neonatal Disorders |
| Non-Communicable |
| • Neoplasms |
| • Cardiovascular Diseases (includes Stroke) |
| • Chronic Respiratory Diseases |
| • Neurological disorders, except Epilepsy and Migraine (tension-type headaches included) |
| • Autism Spectrum Disorder |
| • Musculoskeletal conditions (includes Low back Pain and Neck Pain) |
| • Congenital Birth Defects, except Urogenital and Digestive |
| Injuries (nature of the) |
| • Amputations |
| • Burns |
| • Fractures, except skull |
| • Head Injuries |
| • Spinal Injuries |
| • Minor Injuries: muscle and tendon injuries, including sprains and strains lesser dislocations; Open wound(s) |
| • Dislocation of hip; Dislocation of knee; and Dislocation of shoulder |
| • Asphyxiation |
| • Crush injury; Nerve Injury; Severe Chest Injury |
| • Multiple fractures, dislocations, crashes, wounds, pains, and strains |
| Impairments (from the non-selected “causes” combined) |
| • Heart Failure |
| • Guillain-Barré Syndrome |
Of note, within the application of the working definition and exclusion criteria, ‘dubious’ selection decisions existed, e.g., health conditions for which it was not certain whether physical rehabilitation would be applicable or likely to provide benefits. For example, in Autism Spectrum Disorder, psychosocial disfunction and rehabilitative approaches are often dominant, but sensory-processing and motor impairments are prevalent and might benefit from physical rehabilitation as well [29,30,31,32,33,34,35]. In this context, we included this condition, although this choice may lead to an over-estimation of physical rehabilitation needs. By contrast, we excluded some other health conditions, e.g., those for which the benefit of rehabilitation has not been fully established yet. To reduce the bias towards over- vs. under-estimation resulting from ‘dubious’ selection decisions, a priori evidence-based reasoning was established for the conjunct of ‘dubious’ selection decisions (see Appendix A [29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79]).
Indeed, toward informing these decisions, we searched PubMed primarily for aggregated evidence, preferably systematic reviews, on the effect of physical rehabilitation approaches (e.g., physical therapy, cardiac rehabilitation, pulmonary rehabilitation) on each type of condition we identified as potentially “dubious” for inclusion. We further gave priority to locating and selecting systematic reviews from Cochrane Database of Systematic Reviews, whenever available (i.e., adding “AND “Cochrane Database Syst Rev” [Journal]” to the search approach). As an example, we found that the quantity, quality and strength of the evidence base for cardiac rehabilitation varies across various cardiac conditions [36,37,38,39,40,41,42], but strong evidence that cardiac rehabilitation approaches are overall cost-effective [44]. Thus, we included YLDs from all cardiovascular conditions as likely benefiting from physical rehabilitation. As another example, we did not include any of the maternal, urological or gynecological conditions, even though there is a body of literature pointing to the fact that physical therapy can be useful for addressing incontinence and pelvic pain [70,71]. However, we found that underlying evidence based on the use of physical therapy for the chronic pelvic pain and incontinence is still considered insufficient [72,75], and the vast majority of urological and gynecological conditions are not typically treated with physical rehabilitation. In addition, data weren’t available in the GBD to identify particular urological/gynecological conditions potentially benefiting from rehabilitation, i.e., there are no GBD “impairments” for consequences of urological/gynecological conditions such as incontinence or pelvic pain. Thus, we excluded the maternal, urological or gynecological diseases altogether, even though some might generate YLDs eventually benefiting from physical rehabilitation.
Finally, among the set of conditions in Table 1, we have selected a few (i.e., a subgroup) for a separate analysis. This subgroup consisted of a narrow, highly conservative set of health conditions historically associated with physical rehabilitation need, i.e., musculoskeletal and key neurological diseases and injuries, including stroke, which frequently cause mobility impairments. Table 2 details the exact subgroup of conditions selected for that separate analysis.
Table 2.
Subgroup of health conditions for a separate, highly conservative analysis of physical rehabilitation need.
| Causes |
|---|
| Communicable, Maternal, Neonatal or Nutritional: |
| • Neonatal Disorders—only the Neonatal Encephalopathy due to Birth Asphyxia and Trauma |
| Non-communicable |
| • Stroke |
| • Neurological disorders, except Epilepsy, Dementia and Migraine |
| • Musculoskeletal conditions (includes Low back Pain and Neck Pain) |
| • Congenital Birth Defects—only Neuro Tube Defects + Congenital Musculoskeletal and Limb Anomalies |
| Injuries (nature of the) |
| • All of those in Table 1 |
2.3. Measures and Data Extraction:
Among the measures available in the webtool, we only extract data for YLDs, i.e., the aggregative measure of the GBD study that focuses exclusively in non-fatal impacts of health conditions. YLDs are the years lived with any short-term or long-term health loss weighted for severity by the disability weights. Concretely, YLDs are computed by combining the estimated prevalence of a health condition with the estimated number of years people typically live with those sequelae, up to the population life expectancy threshold. Importantly, the prevalence of sequelae from each condition is classified by severity levels (e.g., mild, moderate, severe), each one having a respective disability weight [5,6,80,81]. For stroke, for example, disability weights vary from 0.019 for mild consequences to 0.588 for severe consequences plus cognition problems, as determined by population preferences in large discrete choice experiments [81]. Details on how YLDs and disability weights are determined, and the current disability weights for all conditions, are provided elsewhere [5,6,81].
For our metrics, we extracted YLD data for prevalent number (YLD counts), rate (per 100,000 people), and percentage (percentage of YLDs from the selected conditions relative to the total amount of YLDs). For age, we extracted YLDs both for all ages and age-standardized rates. With those specifications, we obtained YLDs likely benefiting from physical rehabilitation under the following forms, used as measures for the analysis:
YLD Counts: Nominal amount of YLDs;
YLD Rates: YLDs per 100,000 people, i.e., adjusted for population size only;
Age-standardized YLD Rates: YLD values adjusted for both population size and ageing;
Percentage of YLDs Benefiting from Physical Rehabilitation: The proportion of YLDs from conditions likely benefiting from physical rehabilitation among total YLDs, provided in percent values.
With regards to location, YLDs were extracted at the global level (i.e., for the world) and for high, upper middle, lower middle, and low-income countries, according to the World Bank Income Levels. We also extracted YLDs for all the years from 1990 to 2017, and for each selected health condition (Table 1).
Using the measures and specifications above, data extraction occurred in early December 2018. All of the selected data were imported from the webtool to Excel spreadsheets for data storage, management, and analysis.
2.4. Data Analysis
To determine the overall physical rehabilitation needs, we combined (i.e., summed) the YLDs data for all the selected health conditions—within each of the “years”, “locations”, and “metrics”. Percent changes from 1990 to 2017 were also computed for the combined values.
For inferential statistics, first we plotted the entire time series of the combined values for each location, within each YLD metric. Using visualization and r2 values of pilot regression models, then we determined which regression model type (i.e., linear, exponential, or logarithmic) best fit the plotted data, and recorded the respective r2 values. Given differences in r2 values <0.02 between the models, we retained the linear regression option. Linear regression analyses, using the analysis of variance (ANOVA)—which account for the data on every year between 1990 and 2017, then were used to test for statistical significance, notably of a non-zero yearly change, considering the full time-period between 1990 and 2017, inclusively. We used the linear regression analytical approach even for the data that fitted an exponential or logarithmic-type of regression. In those cases, we tested the models using either the actual YLD values or a ‘log-transformed’ version of these. As there was no difference in the statistical significance for any case, we retained linear regression analyses using the actual YLD values. This facilitated the interpretation of the results since the coefficient and their confidence intervals refer to the estimated annual change in YLD values, i.e., the slope of the linear regression line. The significance level for the analysis was set at p = 0.05.
3. Results
Table 3 shows the YLDs for all conditions likely benefiting from rehabilitation. For instance, it shows that, from 1990 to 2017, a 66.2% growth was found in estimated YLD Counts likely benefiting from physical rehabilitation, with a significant and linear growth of more than 5.1 billion YLDs per year (99% CI: 4.8–5.4; r2 0.99). While countries from all income levels had significant and linear growths, low-income countries more than doubled (111.5% growth) their YLD Counts, likely benefiting from physical rehabilitation for the 28-year period.
Table 3.
Main analysis: YLDs from all conditions likely benefiting from Physical Rehabilitation (1990–2017).
| Location/Item | # 1990 | # 2017 | % Change (1990–2017) | Regression Model Type | r 2 | b Coefficient | 95% CI | 99% CI |
|---|---|---|---|---|---|---|---|---|
| YLD Counts, Billions | ||||||||
| World | 206 | 343 | 66.2% | Linear | 0.99 | 5.10 * | 4.88–5.32 | 4.80–5.40 |
| High-Income | 58 | 79 | 37.4% | Linear | 0.99 | 0.81 * | 0.77–0.84 | 0.76–0.86 |
| Upper Middle-Income | 76 | 123 | 62.1% | Linear | 0.99 | 1.78 * | 1.69–1.87 | 1.66–1.90 |
| Lower Middle-Income | 62 | 119 | 90.4% | Linear | 0.99 | 2.10 * | 2.02–2.19 | 1.99-2.22 |
| Low-Income | 10 | 21 | 111.5% | Linear | 1 | 0.39 * | 0.38–0.40 | 0.38–0.41 |
| YLD Rates | ||||||||
| World | 3825 | 4488 | 17.3% | Linear | 0.96 | 25.7 * | 23.7–27.7 | 23.0–28.4 |
| High-Income | 5748 | 6643 | 15.6% | Linear | 0.98 | 33.1 * | 31.1–35.1 | 30.4–35.8 |
| Upper Middle-Income | 3594 | 4669 | 29.9% | Linear | 0.96 | 42.6 * | 39.3–46.0 | 38.1–47.2 |
| Lower Middle-Income | 3233 | 3806 | 17.7% | Linear | 0.96 | 21.6 * | 19.9–23.2 | 19.3–23.8 |
| Low-Income | 2977 | 3112 | 4.5% | Logarithmic | 0.50 | 2.5 ** | 0.40–4.55 | −0.33–5.28 |
| Age-Standardized YLD Rates | ||||||||
| World | 4377 | 4334 | −1.0% | Logarithmic | 0.22 | −0.62 | −2.13–0.89 | −2.66–1.42 |
| High-Income | 5007 | 4872 | −2.7% | Logarithmic | 0.86 | −5.36 * | −6.76–(−3.96) | −7.26–(−3.47) |
| Upper Middle-Income | 4106 | 4080 | −0.6% | Linear | 0.04 | 1.34 | −1.38–4.06 | −2.33–5.02 |
| Lower Middle-Income | 4262 | 4314 | 1.2% | Linear | 0.46 | 2.33 * | 1.26–3.40 | 0.89–3.78 |
| Low-Income | 4189 | 4276 | 2.1% | Logarithmic | 0.15 | 0.29 | −3.29–3.87 | −4.55–5.14 |
| % of YLDs Benefiting from Physical Rehabilitation (among Total YLDs) | ||||||||
| World | 36.7% | 40.2% | 9.5% | Linear | 0.97 | 0.135 * | 0.125–0.145 | 0.122–0.148 |
| High-Income | 47.6% | 48.6% | 2.2% | Linear | 0.87 | 0.030 * | 0.026–0.035 | 0.024–0.037 |
| Upper Middle-Income | 37.9% | 42.2% | 11.4% | Linear | 0.97 | 0.170 * | 0.157–0.183 | 0.153–0.187 |
| Lower Middle-Income | 30.7% | 35.9% | 16.8% | Linear | 0.98 | 0.200 * | 0.189–0.211 | 0.185–0.215 |
| Low-Income | 27.8% | 32.1% | 15.4% | Linear | 0.97 | 0.155 * | 0.145–0.165 | 0.141–0.169 |
Data obtained from: http://ghdx.healthdata.org/gbd-results-tool. Abbreviations: YLD—Year Lived with Disability. Legend: * p < 0.01, ** p < 0.05. Notes: The “b coefficient” refers to the annual change within the linear regression model. Different population structures apply to countries with varying income levels, so cross-location comparisons are not valid for the metric YLD Counts.
Table 3 also shows significant growths in estimated YLD Rates for the same time-period, worldwide and across countries of all income levels. However, for low-income countries, the growth was not linear (i.e., best fit in a logarithmic model (r2 = 0.5)) and was only significant at a 95% confidence level (p = 0.02). Of note, upper middle-income countries had a yearly growth of 42.6 YLDs per 100,000 people (99% CI: 38.1–47.2; r2 = 0.96), significantly higher than any of the comparators, i.e., no overlap among the 99% CIs.
On Age-standardized YLD Rates, which adjusted YLDs for population size and ageing, Table 3 shows that only high-income and lower middle-income countries had a significant change since 1990, but, while the latter had a linear growth (99% CI: 0.89–3.78; r2 = 0.46), the former had a logarithmic decrease (r2 = 0.86; p < 0.01). Overall, in this metric, we observed the smallest magnitude of changes: a maximum of 2.7% change from 1990 to 2017.
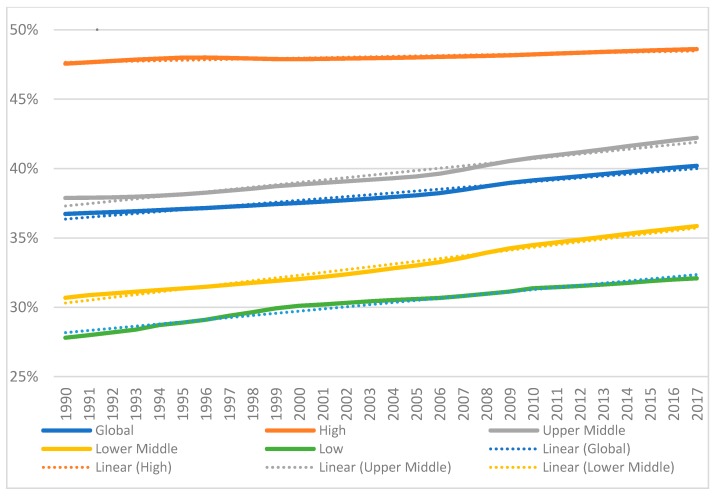
In a final metric, Table 3 shows that the Percentage of YLDs Benefiting from Physical Rehabilitation significantly and linearly increased across locations (all: p < 0.01; minimum r2 = 0.87). However, while high-income countries had the highest percent value in 2017 (48.6%), low and middle-income countries (LMICs) grew significantly on an order of up to seven times: 0.200 (99% CIs 0.185–0.215) versus 0.030 (99 CIs 0.024–0.037). Figure 1 provides a graphical representation of the data on this metric, while Supplementary Material for the three other YLD metrics.
Figure 1.
Percentage of YLDs Benefiting from Physical Rehabilitation among Total YLDs for the globe and across countries of varying income level. Linear regression lines (dotted) displayed.
Finally, Table 4 quantifies YLDs for a conservative subgroup of health conditions historically associated with physical rehabilitation need, i.e., key musculoskeletal and neurological conditions often resulting, primarily, in mobility impairments. The table reveals that a narrow set of conditions accounted for 225 billion YLDs in 2017, nearly two-thirds (65.6%) of the total physical rehabilitation needs (see Table 3). On the evolution over time, the subgroup shows a pattern of the results similar to that of the whole set of conditions, with a few differences relative to the larger group as follows.
Table 4.
YLDs from a narrow set (i.e., subgroup) of health conditions benefiting from Physical Rehabilitation (1990–2017).
| Location/Item | # 1990 | # 2017 | % Change (1990–2017) | Regression Type: Best Fit | r 2 | b Coefficient | 95% CI | 99% CI |
|---|---|---|---|---|---|---|---|---|
| YLD Counts, Billions | ||||||||
| World | 135 | 225 | 66.6% | Linear | 0.99 | 3.32 * | 3.18–3.43 | 3.13–3.51 |
| High-Income | 40.3 | 54.7 | 35.6% | Linear | 0.99 | 0.52 * | 0.50–0.55 | 0.49–0.56 |
| Upper Middle-Income | 49.7 | 82.8 | 66.5% | Linear | 0.99 | 1.24 * | 1.19–1.29 | 1.17–1.31 |
| Lower Middle-Income | 38.8 | 73.9 | 90.6% | Linear | 0.99 | 1.30 * | 1.24–1.36 | 1.22–1.38 |
| Low-Income | 5.9 | 12.5 | 113.6% | Linear | 0.98 | 0.24 * | 0.23–0.25 | 0.22–0.26 |
| YLD Rates | ||||||||
| World | 2506 | 2942 | 17.4% | Linear | 0.96 | 16.6 * | 15.3–17.8 | 14.8–18.3 |
| High-Income | 4030 | 4597 | 14.1% | Linear | 0.97 | 19.7 * | 18.3–21.1 | 17.8–21.6 |
| Upper Middle-Income | 2356 | 3143 | 33.4% | Linear | 0.98 | 30.8 * | 28.9–32.6 | 28.3–33.2 |
| Lower Middle-Income | 2009 | 2367 | 17.8% | Linear | 0.98 | 13.2 * | 12.0–14.4 | 11.6–14.9 |
| Low-Income | 1776 | 1875 | 5.6% | Linear | 0.68 | 3.08 * | 2.22–3.94 | 1.92–4.24 |
| Age-Standardized YLD Rates | ||||||||
| World | 2863 | 2812 | −1.8% | Logarithmic | 0.61 | −1.64 * | −2.66–(−0.61) | −3.02–(−0.25) |
| High-Income | 3504 | 3397 | −3.1% | Logarithmic | 0.83 | −5.25 * | −6.48–(−4.02) | −6.92–(−3.59) |
| Upper Middle-Income | 2664 | 2677 | 0.5% | Linear | 0.18 | 1.72 ** | 0.23–3.22 | −0.30–3.75 |
| Lower Middle-Income | 2657 | 2665 | 0.3% | Linear | 0.03 | 0.38 | −0.44–1.20 | −0.72–1.48 |
| Low-Income | 2564 | 2656 | 3.6% | Linear | 0.82 | 3.33 * | 2.70–3.95 | 2.48–4.17 |
| % of YLDs Benefiting from Physical Rehabilitation (among Total YLDs) | ||||||||
| World | 24.1% | 26.4% | 9.5% | Linear | 0.97 | 0.085 * | 0.079–0.092 | 0.077–0.094 |
| High-Income | 33.3% | 33.6% | 0.9% | Linear | 0.12 | 0.005 | −0.011–0.0005 | −0.013–0.003 |
| Upper Middle-Income | 24.8% | 28.4% | 14.4% | Linear | 0.99 | 0.137 * | 0.131–0.143 | 0.129–0.145 |
| Lower Middle-Income | 19.1% | 22.3% | 16.8% | Linear | 0.97 | 0.122 * | 0.113–0.131 | 0.110–0.134 |
| Low-Income | 16.6% | 19.4% | 16.5% | Linear | 0.95 | 0.107 * | 0.097–0.117 | 0.093–0.120 |
Data obtained from: http://ghdx.healthdata.org/gbd-results-tool. Abbreviations: YLD—Year Lived with Disability. Legend: * p < 0.01, ** p < 0.05. Notes: The “b coefficient” refers to the annual change within the linear regression model. Different population structures apply to countries with varying income levels, so cross-location comparisons are not valid for the metric YLD Counts.
First, YLD Rates for low-income countries grew over time in a linear shape, not logarithmic. Second, the percentage of YLDs Benefiting from Physical Rehabilitation did not significantly change for high-income countries for the subgroup of conditions, while it did in the main analysis. Lastly, in the subgroup of conditions, Age-standardized YLD Rates decreased significantly worlwide but increased significantly in low-income countries.
4. Discussion
This paper is, to our knowledge, the first systematic, secondary analysis of global physical rehabilitation needs, based on publicly-available data from the most comprehensive source of global epidemiological data to date, i.e., the GBD 2017. In addition to an over 66% global increase in YLD Counts from 1990 to 2017 (5.1 billion additional YLDs per year), we found a 17% increase in YLD Rates, i.e., per size of the population. Therefore, the growth of YLDs from all conditions likely benefiting from physical rehabilitation have outpaced that of the population. The key factor influencing per-capita growth has been the global population ageing, which is why the world’s Age-Standardized YLD Rates for all conditions potentially benefitting from physical rehabilitation did not significantly change over the studied time-period. Aging of the population is likely to continue to be a worldwide phenomena for the next several decades (e.g., global population with 65 years or more is predicted to double by 2050, while the overall population is expected to grow by less than 30% [82]). Global needs for physical rehabilitation are likely to continue to grow in tandem, with consequent increased demands for physical rehabilitation.
Growth in need for physical rehabilitation was particularly prominent in LMICs. For instance, in low-income countries, the YLD Counts more than doubled since 1990, likely due to population growth from high fertility rates as YLD Rates grew at a much less pronounced rate. In fact, increases in YLD Counts were inversely proportional to the countries’ income levels, such that the greatest increase in needs for physical rehabilitation was found in countries with lower income levels and the least rehabilitation infrastructure. Indeed, rehabilitation resources in many LMICs remain quite limited [7,19,26,83,84]. The WHO estimates that skilled rehabilitation professionals for many LMICs are currently about one-tenth of those required [7]. Hence, many argue that it is urgent to take action to supply LMICs with increased resources, [24,26,83,84,85,86,87], and this is especially so given the higher nominal increases of physical rehabilitation needs.
Nonetheless, we note that, in low-income countries, we also observed a logarithmic growth in YLD Rates, flattening around the year 2000 (see Supplementary Material for the graphical representation of the data, page 2). It is possible that global health activities for the Millennium Development Goals, which focused, for example, in preventable neonatal and infectious conditions, have helped control the rise in the prevalence of those conditions, and therefore the resulting YLDs in lower income countries [88]. This interpretation is reinforced by the data in Table 4. In that analysis, which focused on a narrow set musculoskeletal and neurological diseases and injuries (i.e., did not account for infectious or most neonatal conditions), we rather observed a linear instead of logarithmic growth in YLD Rates. Global development and advances in disease treatment and prevention in LMICs (e.g., targeting communicable, neonatal, and maternal conditions) result in higher life expectancy in these countries—hence higher likelihood of people experiencing, surviving, and living longer with chronic conditions or long-term disabilities, including those arising from age-related musculoskeletal or neurological conditions. [1,2,3] This epidemiological transition in LMICs has been observed for longer in high-income countries, and result in a trend for increasing YLD Rates, especially from musculoskeletal and neurogical conditions, which are not likely addressed by vertical, disease-focused approaches. Even infectious or neonatal conditions might not have been addressed in their sequalae (i.e., toward reducing or mitigating their disability through rehabilitation) as much as in its prevalence. For instance, while children with complex health conditions and people with HIV/AIDs increasingly survive in LMICs, the associated disabilities and rehabilitation needs remain often unmet [84,86,89,90,91,92]. In this scenario, granting access to needed rehabilitation (e.g., through horizontal, sustainable health systems’ strengthening [24]), especially in LMICs, is of utmost importance [24,85,87], and justified by the current YLDs data.
In addition to resource increases, innovative solutions might be further developed toward increasing access to timely and high quality rehabilitation services for locations with suboptimal or unevenly distributed rehabilitation resources. Potential solutions are needed for rehabilitation delivered at home and in the community, offering the potential that tele-rehabilitation may help fill the gap [43,86,93,94,95,96,97,98]. Task-shifting to healthcare assistants or team-based community care, especially in LMICs, is another potential option to meet global health needs in LMICs warranting future research and development [99].
Only in high-income countries did Age-standardized YLDs diminish over time, whereas in LMICs they did not significantly change or have significantly increased since 1990. This pattern was consistent for both of our analyses: that on the overall physical rehabilitation needs, and that focused on a narrow set of neurological and musculoskeletal conditions. We hypothesize that the wide implementation of public and private physical rehabilitation services in high-income countries, but to a far lesser extent in LMICs, has contributed to these findings. Historically, LMICs’ health systems and global health activities have been focused in reducing preventable mortality, while the global burden of non-fatal health losses has been lagging in terms of global health priority, resources, and gains [1,5,6,100]. Fortunately, there is now a global awareness about the need to avert preventable YLDs through appropriate healthcare services, including rehabilitation [5,6,24,101]. Similarly, global health policies are, now, more inclusive of people with disabilities and their rehabilitation needs [87,102,103]. Finally, the evidence of cost-effectiveness of rehabilitation is escalating [44,104]. In this context, our finding that Age-standardized YLDs was significantly reduced in high-income countries, but not in LMICs—and at times significantly increased in LMICs, can be yet another indicator of the need to scale up rehabilitation services in LMIC’s health systems [24]. Cardiac rehabilitation programs might be a good example, as they have been proven cost-effective [44], are generally standard practice in high-income countries, yet barely existent in many LMICs [105,106,107], even though service delivery models suitable to the LMICs have been developed [108].
Finally, we found the percentage of YLDs likely benefiting from physical rehabilitation increased significantly and linearly across analyzed locations. Furthermore, we observed a trend toward convergence, as the high-income countries had the highest value in 2017, but the growth in LMICs has been significantly higher since 1990. However, even in high-income countries, a significant growth has been persisting over time in the overall physical rehabilitation needs, indicating that the ceiling has not been reached yet in the percentage of YLDs Benefiting from Physical Rehabilitation. That ceiling, however, was found in the analysis narrowly focused on key musculoskeletal and neurological conditions. Therefore, in high-income countries, the areas of physical rehabilitation practice emerging in the more recent decades (e.g., focused on neoplasms or cardiothoracic conditions) have been, altogether, key for the continued growth in the percentage of YLDs Benefiting from Physical Rehabilitation. The higher the percent value, the higher the expected impact of physical rehabilitation, i.e., in terms of being able to reduce a higher share of the global burden of non-fatal health conditions.
Limitations
The paper’s limitations are the following: First, the YLD measure is, at best, a proxy indicator of need for physical rehabilitation. For instance, functional data at the population level, e.g., from the Model Disability Survey, and/or other disability statistics, whenever available, might be used in alternative or complement to provide a more comprehensive picture of populations’ physical rehabilitation needs [85,109,110,111]. This limitation notwithstanding, the GBD is the most comprehensive source of global epidemiological data to date, and GBD data are widely used to analyze of the needs for, or benefits from, specific types of healthcare [112,113,114,115].
Second, there is no global standard of conditions that potentially benefit from physical rehabilitation which we could use for the selection of specific health conditions to include in our main analyses. To inform that selection, we relied on previous research on physical rehabilitation, a working definition of physical rehabilitation, and tailored searches on PubMed. Nonetheless, tailored searches conducted on PubMed, to identify and help select of health conditions likely benefiting from physical rehabilitation, do not equate to a systematic review itself. For conditions which were particularly uncertain with regards to potential benefits from physical rehabilitation, we employed explicit, a priori evidence-informed reasoning about the potential trade-offs for over- vs. under-estimation of physical rehabilitation needs.
Third, while a separate analysis for a subgroup of health conditions historically associated with physical rehabilitation need is present, it does not equate to minimum requirements in terms of a physical rehabilitation need.
Fourth, once we partly relied on published evidence to ground selection decisions and our trade-off reasoning, any under-research on the rehabilitation of conditions less common in high-income countries (e.g., tuberculosis, malaria) might have biased that reasoning. It is unknown whether the such putative under-research contributes under-estimate the magnitude of physical rehabilitation needs, especially in lower income countries.
Fifth, we used inferential statistics with YLD estimates, rather than direct data collection with metrics to quantify the nature and degree of physical disability. Moreover, the uncertainty intervals of the underlying YLD estimates could not be computed for our ‘combined’ values (i.e., the sum of YLDs from all health conditions likely benefeting from physical rehabilitation), although they exist in the public domain for each included condition in isolation [6].
Sixth, the quantity and accuracy of the data used to compute the GBD estimates is typically lower in lower income countries, which can include a less accurate detection or registry of data for many health conditions, especially non-communicable diseases or injuries. That can partly justify why the LMICs have much lower values for example in the Age-Standardized YLD Rates, across the time-series, when compared to high-income countries. Therefore, it is possible that the true magnitude of physical rehabilitation needs in LMICs remain partly obscure in these results. In addition, the quantity and accuracy of the underlying data in 2017 is likely superior to what it was back in 1990. This means a lower precision for the GBD estimates for the earlier years. However, lower preciseness does not imply systematic error (i.e., bias) toward over- or under-estimation of YLDs for the earlier times. To reduce potential bias, at each new cycle, the GBD study uses the more complete and updated data, measurement and classification systems, and estimation methods to re-calculate the entire time-series, not just the estimates for the more recent years [6].
Seventh, the presence of auto-correlation in the time series was not ruled out, i.e., we did not assess whether error terms were significantly correlated over time. Nonetheless, many of the simple linear regression models had nearly perfect fits with the underlying time series data, meaning that the magnitude of each of those errors was negligible. In addition, we used only simple linear regression analyses which did not account for what had changed over time apart from population growth and ageing. The latter ones here were inherently accounted for when we performed analyses using “Age-standardized YLD Rates” instead of simple YLD counts.
Finally, we focused on evolving trends for overall needs for physical rehabilitation and then in a narrow, conservative subgroup of conditions benefeting from physical rehabilitation, and did not perform sub-group analyses across specific groups of conditions (e.g., musculoskeletal, neurological, cardiac, etc.) as these have been performed by other groups that have used GBD data.
5. Conclusions
This systematic secondary analysis of the GBD 2017 provides global data on current physical rehabilitation needs, and on how those needs evolved since 1990, including across countries of varying income level.
Physical rehabilitation needs have been growing significantly over time across locations, not only in absolute terms, but also per-capita and in percentage of the total amount of total YLDs. This means that not only has physical rehabilitation been growing, but also that physical rehabilitation is now capable of averting a higher portion of the global burden of disability. The highest absolute growth of physical rehabilitation needs was observed in countries of lower income level, which typically have deprived rehabilitation infrastructure. Finally, only in high-income countries did a significant reduction in age-standardized needs per capita occur, which can be related to the wider implementation of physical rehabilitation services in these countries.
The use of the comprehensive, up-to-date GBD estimates for the needs-side of the rehabilitation resources-planning equation, albeit imperfect, is a readily available means to help health planners to meet the physical rehabilitation needs of the global population. These needs were found to be high and increasing, including per-capita, across countries of varying income level.
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/16/6/980/s1, Figure S1: YLD Counts likely benefiting from phyisical rehabilitation along with the “best fit” regression models, Figure S2: YLD Rates (per 100,000 People) likley benefiting from physical rehabilitation along with the “best fit” regression models, Figure S3: Age-standardized YLD Rates likely benefiting from physical rehabilitation along with the “best fit” regression models.
Appendix A
-
A On the side of Over-Estimation, we ended up Including the sequelae (i.e., YLDs) from:
-
All Cardiovascular (“causes”):
-
All Chronic Respiratory Diseases (“causes”):
-
All Neonatal Conditions (“causes”).○ We include all neonatal conditions, including “Hemolytic diseases and other neonatal jaundice”. For instance, although frequently benign, neonatal jaundice can become severe and lead to encephalopathy and neurodevelopment impairments [49]. Hence, sequalae (i.e., YLDs) from this condition would be amenable to physical rehabilitation. Overall, sequalae from neonatal conditions would likely lead to some form of physical, neurological or motor impairments or delays that are amenable to physical rehabilitation, although we acknowledge that they might not be present in all cases and therefore the possibility of some error on side of overestimation.
-
Alzheimer’s Disease and other Dementias.○ A wide scope of mental, cognitive as well as physical impairments and rehabilitation needs are associated with these conditions, which progress to affect the activities of daily living (ADLs) and mobility, inclusively from deconditioning. Evidence points out that exercise programs may at least improve the ability to perform ADLs in people with dementia, as in the following examples:Therapeutic interventions that include aerobic and strengthening exercises may help improve independence in ADLs and improve physical performance in people with Alzheimer’s Disease [50]. Strong evidence also supports the benefits of occupation-based interventions and physical exercise for adults with Alzheimer’s Disease and related major neurocognitive disorders [51]. Some evidence hints that physical activity can even improve or slow down decreases in cognitive functioning [52,53]. Even though a Cochrane review in 2015 found no evidence of benefit from exercise on cognition, neuropsychiatric symptoms, or depression, benefits in ADLs were found [54]. Finally, another systematic review hints that preliminary support exists for the effectiveness of physical therapy and exercise interventions in patients with Huntington’s Disease [55].Overall, the inclusion of these conditions can lead to an over-estimation of YLDs amenable to physical rehabilitation as the severity and respective disability weights of these conditions also account for cognitive and mental health needs.
-
Autism Spectrum Disorder:○ Even though psychosocial dysfunction might be dominant, sensory-processing and motor impairments are prevalent and might be addressed by physical rehabilitation approaches [29,30,31,32,33,34,35], yet these impairments are not always present and psychosocial disfunction is often dominant. This means that YLDs from this condition are also germane to other forms of rehabilitative or habilitative interventions—therefore, the possible over-estimation of physical rehabilitation needs from YLDs that came from this condition.
-
-
B On the side of Under-Estimation, we ended up Excluding the sequelae (i.e., YLDs) from:
-
Tuberculosis:○ Although physical impairments might come as sequalae of this condition, we only found a study protocol for a scoping review on the subject [56], whose findings may inform a further systematic review to explore the effectiveness of rehabilitation strategies used to address physical impairments and activity limitations in people with this infection. At today’s level of synthesized evidence, we did not include this condition.
-
Malaria:○ We did not find a strong, recent body of evidence systematically reviewed regarding the effect of physical or even cognitive rehabilitation interventions, even though cognitive impairments are prevalent sequelae in a sub-set of people with malaria and rehabilitative solutions have been proposed, including physical therapy and speech therapy [57]. Malaria is pointed out as one of the possible causes of the disproportionate, high prevalence of cerebral palsy in low-income countries [58]. While that consequence would be amenable to physical rehabilitation, we did not find a systematic study or review on that linkage, inclusively detailing the proportion of cases with sequalae from malaria that lead to cerebral palsy. Therefore, we did not include YLDs from this condition.
-
Other Neglected Tropical Diseases (apart from Leprosy and Zika Virus):○ For Zika Virus and Leprosy we have found reviews or overviews on the likely benefit of physical rehabilitation approaches [59,60,61]. All other conditions in this category were not included, given the lack of identified research or reviews of research focused on the rehabilitation of those conditions.
-
Epilepsy:
-
Migraine:○ There is a body of evidence supporting the benefits of physical therapy for migraine and other headaches, but the methodological shortcomings reduce the confidence in the results [64]. Besides, physical therapy in migraine is more controversial than in tension-type headaches (TTH), since migraine pathogenesis involves activation of sub-cortical structures and the trigemino-vascular system, whereas pathogenesis of TTH is more associated with musculoskeletal disorders, e.g., muscle pain [65]. Finally, we have found systematically reviewed information supporting specific types of physical therapy interventions for TTH [66]. Hence, we have included TTH, but not migraine, even though it cannot be ruled out the effectiveness of physical therapy across headache conditions.
-
Attention Deficit Hyperactivity Disorder:○ Even though occupational therapy interventions can have positive impacts in children’s participation and executive functions [67], the cognitive-functional scope of the intervention only partly relates with physical rehabilitation, and we did not find any systematic reviews supporting the benefit of interventions within the realm of physical rehabilitation for this condition.
-
Diabetes○ Even at the 5th level of the GBD hierarchy, the one with higher detail, we do not have the data for amputation as a consequence of diabetes, for example in contrast with kidney diseases. In these circumstances, we altogether exclude YLDs from diabetes to avoid many false positives in terms of physical rehabilitation need, notably from kidney and eye impairments.
-
All mental health conditions and substance abuse.
-
Maternal, Urological, or Gynecological or conditions.○ Even though there is a body of literature pointing out that physical therapy can be useful on strengthening the pelvic floor muscles and reducing related incontinence (versus no treatments) or even reduce vestibulodynia [70,71], the underlying evidence base, for example on the chronic pelvic pain and incontinence (when added to another active treatment) still is considered insufficient [72,73,74,75]. Finally, it was complex to depict which are the GBD “causes” resulting in those symptoms, and there are no GBD “impairments” for example about incontinence. So, we altogether have excluded the maternal, urological or gynecological diseases, even though some might generate YLDs eventually amenable to physical rehabilitation.
-
Nutritional deficiencies:○ Sequalae from nutritional deficiencies can be many and varied. Therefore, some of the YLDs can be amenable to physical rehabilitation while many others not. For instance, even though Iodine Deficiency can lead to fatigue and that can be possibly addressed by physical rehabilitation, it often leads to more significant sequalae in terms of mental development [76,77]. We avoided the inclusion of conditions from which we can expect a high rate of YLDs not amenable to physical rehabilitation.
-
Unspecific conditions such as “Other Non-communicable diseases”, “Effect of different environmental factors” and “Complications following therapeutic procedures”○ In some cases, these unspecific conditions might lead to physical rehabilitation needs (e.g., hemorrhage after neurosurgery that leads to spinal cord damage) or not (e.g., wound infection after surgery). In a conservative approach, we opt not to include too many false positives.
-
Physical rehabilitation needs from deconditioning in turn arising from non-specific causes (e.g., hospital-associated deconditioning), or even physical rehabilitation needs arising from senescence, i.e., with no need for an underlying disease or injury.
-
Author Contributions
Conceptualization, T.S.J., M.D.L., and H.H.; Methodology, T.S.J., M.D.L., and H.H.; Data Curation, T.S.J.; Writing—Original Draft Preparation, T.S.J.; Writing—Review and Editing, T.S.J., M.D.L., and H.H.; Visualization, T.S.J., M.D.L., and H.H.; Project Administration, T.S.J. and H.H.; Supervision, M.D.L., and H.H.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Chatterji S., Byles J., Cutler D., Seeman T., Verdes E. Health, functioning, and disability in older adults—Present status and future implication. Lancet. 2015;385:563–575. doi: 10.1016/S0140-6736(14)61462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization and World Bank . World Report on Disability. WHO; Geneva, Switzerland: 2011. [Google Scholar]
- 3.World Health Organization . World Report on Ageing and Health. WHO; Geneva, Switzerland: 2015. [Google Scholar]
- 4.GBD 2016 DALYs and HALE Collaborators Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1260–1344. doi: 10.1016/S0140-6736(17)32130-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211–1259. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization . Rehabilitation 2030: A Call for Action. The Need to Scale up Rehabilitation. WHO; Geneva, Switzerland: 2017. [(accessed on 12 July 2018)]. Available online: http://www.who.int/disabilities/care/NeedToScaleUpRehab.pdf?ua=1. [Google Scholar]
- 8.Gupta N., Castillo-Laborde C., Landry M.D. Health-related rehabilitation services: Assessing the global supply of and need for human resources. BMC Health Serv. Res. 2011;11:276. doi: 10.1186/1472-6963-11-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haagsma J.A., Graetz N., Bolliger I., Naghavi M., Higashi H., Mullany E.C., Abera S.F., Abraham J.P., Adofo K., Alsharif U., et al. The global burden of injury: Incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj. Prev. 2016;22:3–18. doi: 10.1136/injuryprev-2015-041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.March L., Smith E.U., Hoy D.G., Cross M.J., Sanchez-Riera L., Blyth F., Buchbinder R., Vos T., Woolf A.D. Burden of disability due to musculoskeletal (MSK) disorders. Best Pract. Res. Clin. Rheumatol. 2014;28:353–366. doi: 10.1016/j.berh.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 11.Hoy D., March L., Brooks P., Blyth F., Woolf A., Bain C., Williams G., Smith E., Vos T., Barendregt J., et al. The global burden of low back pain: Estimates from the Global Burden of Disease 2010 study. Ann. Rheum. Dis. 2014;73:968–974. doi: 10.1136/annrheumdis-2013-204428. [DOI] [PubMed] [Google Scholar]
- 12.Whiteford H.A., Ferrari A.J., Degenhardt L., Feigin V., Vos T. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. PLoS ONE. 2015;10:e0116820. doi: 10.1371/journal.pone.0116820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.GBD 2015 Neurological Disorders Collaborator Group Global, regional, and national burden of neurological disorders during 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017;16:877–897. doi: 10.1016/S1474-4422(17)30299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Global Burden of Diseases, Injuries and Risk Factors Study 2013 and Stroke Experts Writing Group Global burden of stroke and risk factors in 188 countries, during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016;15:913–924. doi: 10.1016/S1474-4422(16)30073-4. [DOI] [PubMed] [Google Scholar]
- 15.Roth G.A., Johnson C., Abajobir A., Abd-Allah F., Abera S.F., Abyu G., Ahmed M., Aksut B., Alam T., Alam K., et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017;70:1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.GBD 2015 Chronic Respiratory Disease Collaborators Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir. Med. 2017;5:691–706. doi: 10.1016/S2213-2600(17)30293-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Global Burden of Disease Cancer Collaboration Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3:524–548. doi: 10.1001/jamaoncol.2016.5688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.GBD 2015 HIV Collaborators Estimates of global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2015: The Global Burden of Disease Study 2015. Lancet HIV. 2016;3:e361–e387. doi: 10.1016/S2352-3018(16)30087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jesus T.S., Koh G., Landry M., Ong P., Green P., Lopes A., Hoenig H. Finding the “Right-Size” Physical Therapy Workforce: International Perspective Across 4 Countries. Phys. Ther. 2016;96:1597–1609. doi: 10.2522/ptj.20160014. [DOI] [PubMed] [Google Scholar]
- 20.Jesus T.S. Systematic Reviews and Clinical Trials in rehabilitation: Comprehensive analyses of publication trends. Arch. Phys. Med. Rehabil. 2016;97:1853–1862.e2. doi: 10.1016/j.apmr.2016.06.017. [DOI] [PubMed] [Google Scholar]
- 21.Kamper S.J., Moseley A.M., Herbert R.D., Maher C.G., Elkins M.R., Sherrington C. 15 years of tracking physiotherapy evidence on PEDro, where are we now? Br. J. Sports Med. 2015;49:907–909. doi: 10.1136/bjsports-2014-094468. [DOI] [PubMed] [Google Scholar]
- 22.Yamato T.P., Arora M., Stevens M.L., Elkins M.R., Moseley A.M. Quality, language, subdiscipline and promotion were associated with article accesses on Physiotherapy Evidence Database (PEDro) Physiotherapy. 2018;104:122–128. doi: 10.1016/j.physio.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 23.Meyer T., Gutenbrunner C., Bickenbach J., Cieza A., Melvin J., Stucki G. Towards a conceptual description of rehabilitation as a health strategy. J. Rehabil. Med. 2011;43:765–769. doi: 10.2340/16501977-0865. [DOI] [PubMed] [Google Scholar]
- 24.Krug E., Cieza A. Strengthening health systems to provide rehabilitation services. Bull. World Health Organ. 2017;95:167. doi: 10.2471/BLT.17.191809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jesus T.S., Bright F., Kayes N., Cott C.A. Person-centred rehabilitation: What exactly does it mean? Protocol for a scoping review with thematic analysis towards framing the concept and practice of person-centred rehabilitation. BMJ Open. 2016;6:e011959. doi: 10.1136/bmjopen-2016-011959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jesus T.S., Landry M.D., Dussault G., Fronteira I. Human Resources for Health (and Rehabilitation): Six Rehab-Workforce Challenges for the Century. Hum. Resour. Health. 2017;15:8. doi: 10.1186/s12960-017-0182-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.NIH Medical Rehabilitation Coordinating Committee National Institutes of Health Research Plan on Rehabilitation: NIH Medical Rehabilitation Coordinating Committee. Phys. Ther. 2017;97:104–407. doi: 10.1093/ptj/pzx026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gutenbrunner C., Meyer T., Melvin J., Stucki G. Towards a conceptual description of Physical and Rehabilitation Medicine. J. Rehabil. Med. 2011;43:760–764. doi: 10.2340/16501977-0866. [DOI] [PubMed] [Google Scholar]
- 29.Downey R., Rapport M.J. Motor activity in children with autism: A review of current literature. Pediatr. Phys. Ther. 2012;24:2–20. doi: 10.1097/PEP.0b013e31823db95f. [DOI] [PubMed] [Google Scholar]
- 30.Bhat A.N., Landa R.J., Galloway J.C. Current perspectives on motor functioning in infants, children, and adults with autism spectrum disorders. Phys. Ther. 2011;91:1116–1129. doi: 10.2522/ptj.20100294. [DOI] [PubMed] [Google Scholar]
- 31.Srinivasan S.M., Pescatello L.S., Bhat A.N. Current perspectives on physical activity and exercise recommendations for children and adolescents with autism spectrum disorders. Phys. Ther. 2014;94:875–889. doi: 10.2522/ptj.20130157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lim Y.H., Partridge K., Girdler S., Morris S.L. Standing Postural Control in Individuals with Autism Spectrum Disorder: Systematic Review and Meta-analysis. J. Autism Dev. Disord. 2017;47:2238–2253. doi: 10.1007/s10803-017-3144-y. [DOI] [PubMed] [Google Scholar]
- 33.Weitlauf A.S., Sathe N., McPheeters M.L., Warren Z.E. Interventions Targeting Sensory Challenges in Autism Spectrum Disorder: A Systematic Review. Pediatrics. 2017;139:e20170347. doi: 10.1542/peds.2017-0347. [DOI] [PubMed] [Google Scholar]
- 34.Watling R., Hauer S. Effectiveness of Ayres Sensory Integration® and Sensory-Based Interventions for People with Autism Spectrum Disorder: A Systematic Review. Am. J. Occup. Ther. 2015;69:6905180030p1–6905180030p12. doi: 10.5014/ajot.2015.018051. [DOI] [PubMed] [Google Scholar]
- 35.Kindregan D., Gallagher L., Gormley J. Gait deviations in children with autism spectrum disorders: A review. Autism Res. Treat. 2015;2015:741480. doi: 10.1155/2015/741480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sibilitz K.L., Berg S.K., Tang L.H., Risom S.S., Gluud C., Lindschou J., Kober L., Hassager C., Taylor R.S., Zwisler A.D. Exercise-based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database Syst. Rev. 2016;3:CD010876. doi: 10.1002/14651858.CD010876.pub2. [DOI] [PubMed] [Google Scholar]
- 37.Risom S.S., Zwisler A.D., Johansen P.P., Sibilitz K.L., Lindschou J., Gluud C., Taylor R., Svendsen J.H., Berg S.K. Exercise-based cardiac rehabilitation for adults with atrial fibrillation. Cochrane Database Syst. Rev. 2017;2:CD01119. doi: 10.1002/14651858.CD011197.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Taylor R.S., Sagar V.A., Davies E.J., Briscoe S., Coats A.J., Dalal H., Lough F., Rees K., Singh S. Exercise-based rehabilitation for heart failure. Cochrane Database Syst. Rev. 2014;4:CD003331. doi: 10.1002/14651858.CD003331.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Anderson L., Nguyen T.T., Dall C.H., Burgess L., Bridges C., Taylor R.S. Exercise-based cardiac rehabilitation in heart transplant recipients. Cochrane Database Syst. Rev. 2017;4:CD012264. doi: 10.1002/14651858.CD012264.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Anderson L., Taylor R.S. Cardiac rehabilitation for people with heart disease: An overview of Cochrane systematic reviews. Cochrane Database Syst. Rev. 2014;12:CD011273. doi: 10.1002/14651858.CD011273.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Anderson L., Thompson D.R., Oldridge N., Zwisler A.D., Rees K., Martin N., Taylor R.S. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 2016;1:CD00180. doi: 10.1002/14651858.CD001800.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Price K.J., Gordon B.A., Bird S.R., Benson A.C. A review of guidelines for cardiac rehabilitation exercise programmes: Is there an international consensus? Eur. J. Prev. Cardiol. 2016;23:1715–1733. doi: 10.1177/2047487316657669. [DOI] [PubMed] [Google Scholar]
- 43.Xia T.L., Huang F.Y., Peng Y., Huang B.T., Pu X.B., Yang Y., Chai H., Chen M. Efficacy of Different Types of Exercise-Based Cardiac Rehabilitation on Coronary Heart Disease: A Network Meta-analysis. J. Gen. Intern. Med. 2018;33:2201–2209. doi: 10.1007/s11606-018-4636-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shields G.E., Wells A., Doherty P., Heagerty A., Buck D., Davies L.M. Cost-effectiveness of cardiac rehabilitation: A systematic review. Heart. 2018;104:1403–1410. doi: 10.1136/heartjnl-2017-312809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Puhan M.A., Gimeno-Santos E., Cates C.J., Troosters T. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2016;12:CD005305. doi: 10.1002/14651858.CD005305.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McCarthy B., Casey D., Devane D., Murphy K., Murphy E., Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2015;2:CD003793. doi: 10.1002/14651858.CD003793.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dale M.T., McKeough Z.J., Troosters T., Bye P., Alison J.A. Exercise training to improve exercise capacity and quality of life in people with non-malignant dust-related respiratory diseases. Cochrane Database Syst. Rev. 2015;11:CD009385. doi: 10.1002/14651858.CD009385.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dowman L., Hill C.J., Holland A.E. Pulmonary rehabilitation for interstitial lung disease. Cochrane Database Syst. Rev. 2014;10:CD006322. doi: 10.1002/14651858.CD006322.pub3. [DOI] [PubMed] [Google Scholar]
- 49.Olusanya B.O., Kaplan M., Hansen T.W.R. Neonatal hyperbilirubinaemia: A global perspective. Lancet Child Adolesc. Health. 2018;2:610–620. doi: 10.1016/S2352-4642(18)30139-1. [DOI] [PubMed] [Google Scholar]
- 50.Rao A.K., Chou A., Bursley B., Smulofsky J., Jezequel J. Systematic review of the effects of exercise on activities of daily living in people with Alzheimer’s disease. Am. J. Occup. Ther. 2014;68:50–56. doi: 10.5014/ajot.2014.009035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Smallfield S., Heckenlaible C. Effectiveness of Occupational Therapy Interventions to Enhance Occupational Performance for Adults with Alzheimer’s Disease and Related Major Neurocognitive Disorders: A Systematic Review. Am. J. Occup. Ther. 2017;71:7105180010p1–7105180010p9. doi: 10.5014/ajot.2017.024752. [DOI] [PubMed] [Google Scholar]
- 52.Du Z., Li Y., Li J., Zhou C., Li F., Yang X. Physical activity can improve cognition in patients with Alzheimer’s disease: A systematic review and meta-analysis of randomized controlled trials. Clin. Interv. Aging. 2018;13:1593–1603. doi: 10.2147/CIA.S169565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Phillips C., Baktir M.A., Das D., Lin B., Salehi A. The Link Between Physical Activity and Cognitive Dysfunction in Alzheimer Disease. Phys. Ther. 2015;95:1046–1060. doi: 10.2522/ptj.20140212. [DOI] [PubMed] [Google Scholar]
- 54.Forbes D., Forbes S.C., Blake C.M., Thiessen E.J., Forbes S. Exercise programs for people with dementia. Cochrane Database Syst. Rev. 2015;15:CD006489. doi: 10.1002/14651858.CD006489.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fritz N.E., Rao A.K., Kegelmeyer D., Kloos A., Busse M., Hartel L., Carrier J., Quinn L. Physical Therapy and Exercise Interventions in Huntington’s Disease: A Mixed Methods Systematic Review. J. Huntingt. Dis. 2017;6:217–235. doi: 10.3233/JHD-170260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Van Aswegen H., Roos R. Physical impairments and activity limitations experienced by people with tuberculosis: A scoping review protocol. JBI Database Syst. Rev. Implement. Rep. 2015;15:49–54. doi: 10.11124/JBISRIR-2016-002963. [DOI] [PubMed] [Google Scholar]
- 57.Bangirana P., Idro R., John C.C., Boivin M.J. Rehabilitation for cognitive impairments after cerebral malaria in African children: Strategies and limitations. Trop. Med. Int. Health. 2006;11:1341–1349. doi: 10.1111/j.1365-3156.2006.01685.x. [DOI] [PubMed] [Google Scholar]
- 58.Kakooza-Mwesige A., Andrews C., Peterson S., Wabwire Mangen F., Eliasson A.C., Forssberg H. Prevalence of cerebral palsy in Uganda: A population-based study. Lancet Glob. Health. 2017;5:e1275–e1282. doi: 10.1016/S2214-109X(17)30374-1. [DOI] [PubMed] [Google Scholar]
- 59.Landry M.D., Raman S.R., Kennedy K., Bettger J.P., Magnusson D. Zika Virus (ZIKV), Global Public Health, Disability, and Rehabilitation: Connecting the Dots. Phys. Ther. 2017;97:275–279. doi: 10.2522/ptj.20160476. [DOI] [PubMed] [Google Scholar]
- 60.Wim Brandsma J. Rehabilitation of leprosy-affected people: An overview. Clin. Dermatol. 2016;34:66–69. doi: 10.1016/j.clindermatol.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 61.Van Brakel W., Cross H., Declercq E., Deepak S., Lockwood D., Saunderson P., Smith W.C., Batty J., Nahodilova L., Soutar D., et al. Review of leprosy research evidence (2002–2009) and implications for current policy and Practice–ILEP Technical Commission. Lepr. Rev. 2010;81:228–275. [PubMed] [Google Scholar]
- 62.Farina E., Raglio A., Giovagnoli A.R. Cognitive rehabilitation in epilepsy: An evidence-based review. Epilepsy Res. 2015;109:210–218. doi: 10.1016/j.eplepsyres.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 63.Barr W. Cognitive Rehabilitation for Epilepsy: What Do We Really Know? Epilepsy Curr. 2016;16:87–88. doi: 10.5698/1535-7511-16.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Luedtke K., Allers A., Schulte L.H., May A. Efficacy of interventions used by physiotherapists for patients with headache and migraine-systematic review and meta-analysis. Cephalalgia. 2016;36:474–492. doi: 10.1177/0333102415597889. [DOI] [PubMed] [Google Scholar]
- 65.Fernández-de-Las-Peñas C., Cuadrado M.L. Physical therapy for headaches. Cephalalgia. 2016;36:1134–1142. doi: 10.1177/0333102415596445. [DOI] [PubMed] [Google Scholar]
- 66.Espí-López G.V., Arnal-Gómez A., Arbós-Berenguer T., González Á.A., Vicente-Herrero T. Effectiveness of Physical Therapy in Patients with Tension-type Headache: Literature Review. J. Jpn. Phys. Ther. Assoc. 2014;17:31–38. doi: 10.1298/jjpta.Vol17_005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hahn-Markowitz J., Berger I., Manor I., Maeir A. Impact of the Cognitive-Functional (Cog-Fun) Intervention on Executive Functions and Participation Among Children with Attention Deficit Hyperactivity Disorder: A Randomized Controlled Trial. Am. J. Occup. Ther. 2017;71:7105220010p1–7105220010p9. doi: 10.5014/ajot.2017.022053. [DOI] [PubMed] [Google Scholar]
- 68.Cooney G.M., Dwan K., Greig C.A., Lawlor D.A., Rimer J., Waugh F.R., McMurdo M., Mead G.E. Exercise for depression. Cochrane Database Syst. Rev. 2013;9:CD004366. doi: 10.1002/14651858.CD004366.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schuch F.B., Vancampfort D., Richards J., Rosenbaum S., Ward P.B., Stubbs B. Exercise as a treatment for depression: A meta-analysis adjusting for publication bias. J. Psychiatr. Res. 2016;77:42–51. doi: 10.1016/j.jpsychires.2016.02.023. [DOI] [PubMed] [Google Scholar]
- 70.Morin M., Carroll M.S., Bergeron S. Systematic Review of the Effectiveness of Physical Therapy Modalities in Women with Provoked Vestibulodynia. Sex. Med. Rev. 2017;5:295–322. doi: 10.1016/j.sxmr.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 71.Dumoulin C., Cacciari L.P., Hay-Smith E.J.C. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst. Rev. 2018;10:CD005654. doi: 10.1002/14651858.CD005654.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ayeleke R.O., Hay-Smith E.J., Omar M.I. Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women. Cochrane Database Syst. Rev. 2015;11:CD010551. doi: 10.1002/14651858.CD010551.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhang F.W., Wei F., Wang H.L., Pan Y.Q., Zhen J.Y., Zhang J.X., Yang K.H. Does pelvic floor muscle training augment the effect of surgery in women with pelvic organ prolapse? A systematic review of randomized controlled trials. Neurourol. Urodyn. 2016;35:666–674. doi: 10.1002/nau.22784. [DOI] [PubMed] [Google Scholar]
- 74.Fuentes-Márquez P., Cabrera-Martos I., Valenza M.C. Physiotherapy interventions for patients with chronic pelvic pain: A systematic review of the literature. Physiother. Theory Pract. 2018 doi: 10.1080/09593985.2018.1472687. [DOI] [PubMed] [Google Scholar]
- 75.Klotz S.G., Schön M., Ketels G., Löwe B., Brünahl C.A. Physiotherapy management of patients with chronic pelvic pain (CPP): A systematic review. Physiother. Theory Pract. 2018 doi: 10.1080/09593985.2018.1455251. [DOI] [PubMed] [Google Scholar]
- 76.Redman K., Ruffman T., Fitzgerald P., Skeaff S. Iodine Deficiency and the Brain: Effects and Mechanisms. Crit. Rev. Food Sci. Nutr. 2016;56:2695–2713. doi: 10.1080/10408398.2014.922042. [DOI] [PubMed] [Google Scholar]
- 77.Niwattisaiwong S., Burman K.D., Li-Ng M. Iodine deficiency: Clinical implications. Cleve Clin. J. Med. 2017;84:236–244. doi: 10.3949/ccjm.84a.15053. [DOI] [PubMed] [Google Scholar]
- 78.Kortebein P. Rehabilitation for hospital-associated deconditioning. Am. J. Phys. Med. Rehabil. 2009;88:66–77. doi: 10.1097/PHM.0b013e3181838f70. [DOI] [PubMed] [Google Scholar]
- 79.Galloza J., Castillo B., Micheo W. Benefits of Exercise in the Older Population. Phys. Med. Rehabil. Clin. N. Am. 2017;28:659–669. doi: 10.1016/j.pmr.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 80.Burstein R., Fleming T., Haagsma J., Salomon J.A., Vos T., Murray C.J.L. Estimating distributions of health state severity for the Global Burden of Disease study. Popul. Health Metr. 2015;13:31. doi: 10.1186/s12963-015-0064-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Salomon J.A., Haagsma J.A., Davis A., de Noordhout C.M., Polinder S., Havelaar A.H., Cassini A., Devleesschauwer B., Kretzschmar M., Speybroeck N., et al. Disability weights for the Global Burden of Disease 2013. Lancet Glob. Health. 2015;3:e712–e723. doi: 10.1016/S2214-109X(15)00069-8. [DOI] [PubMed] [Google Scholar]
- 82.United Nations . World Population Prospects: Key Findings & Advance Tables. UN; New York, NY, USA: 2017. [(accessed on 11 February 2018)]. Available online: https://esa.un.org/unpd/wpp/Publications/Files/WPP2017_KeyFindings.pdf. [Google Scholar]
- 83.Kamenov K., Mills J.A., Chatterji S., Cieza A. Needs and unmet needs for rehabilitation services: A scoping review. Disabil. Rehabil. 2018 doi: 10.1080/09638288.2017.1422036. in press. [DOI] [PubMed] [Google Scholar]
- 84.Bright T., Wallace S., Kuper H. A Systematic Review of Access to Rehabilitation for People with Disabilities in Low- and Middle-Income Countries. Int. J. Environ. Res. Public Health. 2018;5:2165. doi: 10.3390/ijerph15102165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.World Health Organization . Rehabilitation 2030: A Call for Action. Meeting Report. WHO; Geneva, Switzerland: 2017. [(accessed on 21 March 2018)]. Available online: http://www.who.int/disabilities/care/rehab-2030/en/ [Google Scholar]
- 86.Magnusson D., Sweeney F., Landry M. Provision of rehabilitation services for children with disabilities living in low- and middle-income countries: A scoping review. Disabil. Rehabil. 2017 doi: 10.1080/09638288.2017.1411982. in press. [DOI] [PubMed] [Google Scholar]
- 87.Kuper H., Hanefeld J. Debate: Can we achieve universal health coverage without a focus on disability? BMC Health Serv. Res. 2018;18:738. doi: 10.1186/s12913-018-3547-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fehling M., Nelson B.D., Venkatapuram S. Limitations of the Millennium Development Goals: A literature review. Glob. Public Health. 2013;8:1109–1122. doi: 10.1080/17441692.2013.845676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Participant Working Group of the Dar es Salaam Seventh International Conference on Birth Defects and Disabil Prevention of Congenital Disorders and Care of Affected Children: A Consensus Statement. JAMA Pediatr. 2016;170:790–793. doi: 10.1001/jamapediatrics.2016.0388. [DOI] [PubMed] [Google Scholar]
- 90.Bright T., Felix L., Kuper H., Polack S. Systematic review of strategies to increase access to health services among children over five in low- and middle-income countries. Trop. Med. Int. Health. 2018;23:476–507. doi: 10.1111/tmi.13044. [DOI] [PubMed] [Google Scholar]
- 91.Nixon S., Cameron C., Mweshi M., Nkandu E.M., Okidi C., Tattle S., Yates T. “It Is an Eye-Opener That There Is a Relationship between Rehabilitation and HIV”: Perspectives of Physiotherapists and Occupational Therapists in Kenya and Zambia on the Role of Rehabilitation with Adults and Children Living with HIV. Physiother. Can. 2016;68:290–297. doi: 10.3138/ptc.2015-42GH. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Stevens M., Kirsh B., Nixon S.A. Rehabilitation interventions for children living with HIV: A scoping review. Disabil. Rehabil. 2014;36:865–874. doi: 10.3109/09638288.2013.821184. [DOI] [PubMed] [Google Scholar]
- 93.Martins S.C., Pontes-Neto O.M., Alves C.V., de Freitas G.R., Filho J.O., Tosta E.D., Cabral N.L. Past, present, and future of stroke in middle-income countries: The Brazilian experience. Int. J. Stroke. 2013;8(Suppl. A):106–111. doi: 10.1111/ijs.12062. [DOI] [PubMed] [Google Scholar]
- 94.Yan L.L., Li C., Chen J., Miranda J.J., Luo R., Bettger J., Zhu Y., Feigin V., O’Donnell M., Zhao D., et al. Prevention, management, and rehabilitation of stroke in low- and middle-income countries. eNeurologicalSci. 2016;2:21–30. doi: 10.1016/j.ensci.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Furlan A.D., Irvin E., Munhall C., Giraldo-Prieto M., Fullerton L., McMaster R., Danak S., Costante A., Pitzul K., Bhide R.P., et al. Rehabilitation service models for people with physical and/or mental disability living in low- and middle-income countries: A systematic review. J. Rehabil. Med. 2018;50:487–498. doi: 10.2340/16501977-2325. [DOI] [PubMed] [Google Scholar]
- 96.Sureshkumar K., Murthy G.V.S., Kuper H. Protocol for a randomised controlled trial to evaluate the effectiveness of the ‘Care for Stroke’ intervention in India: A smartphone-enabled, carer-supported, educational intervention for management of disabilities following stroke. BMJ Open. 2018;8:e020098. doi: 10.1136/bmjopen-2017-020098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Rawstorn J.C., Gant N., Direito A., Beckmann C., Maddison R. Telehealth exercise-based cardiac rehabilitation: A systematic review and meta-analysis. Heart. 2016;102:1183–1192. doi: 10.1136/heartjnl-2015-308966. [DOI] [PubMed] [Google Scholar]
- 98.Hossain M.S., Harvey L.A., Rahman M.A., Bowden J.L., Islam M.S., Taylor V., Muldoon S., Herbert R.D. A pilot randomised trial of community-based care following discharge from hospital with a recent spinal cord injury in Bangladesh. Clin. Rehabil. 2017;31:781–789. doi: 10.1177/0269215516654207. [DOI] [PubMed] [Google Scholar]
- 99.ATTEND Collaborative Group Family-led rehabilitation after stroke in India (ATTEND): A randomised controlled trial. Lancet. 2017;390:588–599. doi: 10.1016/S0140-6736(17)31447-2. [DOI] [PubMed] [Google Scholar]
- 100.GBD 2017 DALYs and HALE Collaborators Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1859–1922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Mills T., Marks E., Reynolds T., Cieza A. Rehabilitation: Essential along the Continuum of Care. In: Gelband H., Horton S., Jha P., Laxminarayan R., Mock C.N., Nugent R., editors. Disease Control Priorities: Improving Health and Reducing Poverty. 3rd ed. The World Bank; Washington, DC, USA: 2017. The International Bank for Reconstruction and Development. [PubMed] [Google Scholar]
- 102.United Nations Disability-Inclusive Sustainable Development Goals. [(accessed on 20 July 2018)]; Available online: http://www.un.org/disabilities/documents/sdgs/disability_inclusive_sdgs.pdf.
- 103.Tebbutt E., Brodmann R., Borg J., MacLachlan M., Khasnabis C., Horvath R. Assistive products and the Sustainable Development Goals (SDGs) Glob. Health. 2016;12:79. doi: 10.1186/s12992-016-0220-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Howard-Wilsher S., Irvine L., Fan H., Shakespeare T., Suhrcke M., Horton S., Poland F., Hooper L., Song F. Systematic overview of economic evaluations of health-related rehabilitation. Disabil. Health J. 2016;9:11–25. doi: 10.1016/j.dhjo.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 105.Lima de Melo Ghisi G., Pesah E., Turk-Adawi K., Supervia M., Lopez Jimenez F., Grace S.L. Cardiac Rehabilitation Models around the Globe. J. Clin. Med. 2018;7:260. doi: 10.3390/jcm7090260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Pesah E., Supervia M., Turk-Adawi K., Grace S.L. A Review of Cardiac Rehabilitation Delivery Around the World. Prog. Cardiovasc. Dis. 2017;60:267–280. doi: 10.1016/j.pcad.2017.08.007. [DOI] [PubMed] [Google Scholar]
- 107.Turk-Adawi K., Sarrafzadegan N., Grace S.L. Global availability of cardiac rehabilitation. Nat. Rev. Cardiol. 2014;10:586–596. doi: 10.1038/nrcardio.2014.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Grace S.L., Turk-Adawi K.I., Contractor A., Atrey A., Campbell N., Derman W., Melo Ghisi G.L., Oldridge N., Sarkar B.K., Yeo T.J., et al. Cardiac rehabilitation delivery model for low-resource settings. Heart. 2016;102:1449–1455. doi: 10.1136/heartjnl-2015-309209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.McPherson A., Durham J., Richards N., Gouda H., Rampatige R., Whittaker M. Strengthening health information systems for disability-related rehabilitation in LMICs. Health Policy Plan. 2017;32:384–394. doi: 10.1093/heapol/czw140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Trani J.F., Babulal G.M., Bakhshi P. Development and Validation of the 34-Item Disability Screening Questionnaire (DSQ-34) for Use in Low and Middle Income Countries Epidemiological and Development Surveys. PLoS ONE. 2015;10:e0143610. doi: 10.1371/journal.pone.0143610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Oberhauser C., Chatterji S., Sabariego C., Cieza A. Development of a metric for tracking and comparing population health based on the minimal generic set of domains of functioning and health. Popul. Health Metr. 2016;14:19. doi: 10.1186/s12963-016-0088-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Higashi H., Barendregt J.J., Kassebaum N.J., Weiser T.G., Bickler S.W., Vos T. Burden of injuries avertable by a basic surgical package in low- and middle-income regions: A systematic analysis from the Global Burden of Disease 2010 Study. World J. Surg. 2015;39:1–9. doi: 10.1007/s00268-014-2685-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bickler S., Higashi H., Kassebaum N., Weiser D., Chang D., Barendregt J., Noormahomed E., Vos T. Global Burden of Surgical Conditions. In: Debas H.T., editor. Essential Surgery: Disease Control Priorities. 3rd ed. Volume 1 The World Bank; Washington, DC, USA: 2015. The International Bank for Reconstruction and Development. [Google Scholar]
- 114.Rose J., Weiser T.G., Hider P., Wilson L., Gruen R.L., Bickler S.W. Estimated need for surgery worldwide based on prevalence of diseases: A modelling strategy for the WHO Global Health Estimate. Lancet Glob. Health. 2015;3(Suppl. 2):S13–S20. doi: 10.1016/S2214-109X(15)70087-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Marcenes W., Kassebaum N.J., Bernabé E., Flaxman A., Naghavi M., Lopez A., Murray C.J. Global burden of oral conditions in 1990–2010: A systematic analysis. J. Dent. Res. 2013;92:592–597. doi: 10.1177/0022034513490168. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.