Fig 3. Pooled comparison of five anaesthesiologists’ prediction performance with and without assistance by Prescience.
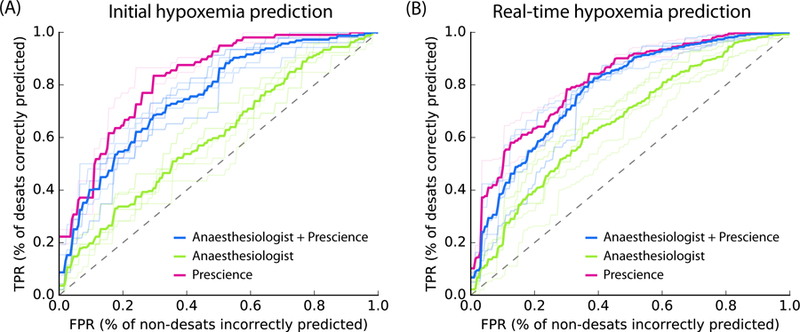
Receiver Operating Characteristic (ROC) plots comparing five anaesthesiologists’ predictions from recorded data with and without Prescience assistance. Light colored lines represent individual anaesthesiologist’s performances; dark lines represent their average performance. (A) For initial risk prediction, anaesthesiologists (green, AUC = 0.60) performed significantly better with Prescience assistance (blue, AUC = 0.76; P-value < 0.0001) than without Prescience assistance, and Prescience performed better in a direct comparison with anaesthesiologists (purple, AUC = 0.83; P-value < 0.0001). (B) For intraoperative real-time (next 5 minute) risk prediction anaesthesiologists (green, AUC = 0.66) again performed better with Prescience assistance (blue, AUC = 0.78; P-value < 0.0001), and Prescience alone outperformed anaesthesiologists predictions (purple, AUC = 0.81; P-value < 0.0001). Note that the False Positive Rate (FPR) (x-axis) measures how many points without upcoming hypoxemia were incorrectly predicted to have upcoming hypoxemia. The True Positive Rate (TPR) (y-axis) measures what fraction of hypoxemic events were correctly predicted. P-values were computed using bootstrap resampling over the tested time points while measuring the difference in area between the curves. If we instead resample over anaesthesiologists we observe bootstrap P-values of 0, and t-test P-values < 0.001 for Prescience improvements. See Supplementary Figure 8 for plots of the statistical separation between the mean ROC curves across all false positive rates.
