Abstract
Aim
To determine whether long-term engagement in occupational diving causes significant changes in spirometric measurements.
Method
All divers with adequate spirometric records spanning at least 10 years were identified from the New Zealand occupational diver database. Changes in lung function over time were compared with normative values derived using published prediction equations. Any significant changes were tested for correlation with age, duration of occupational diving, gender, smoking history and body mass index (BMI).
Results
Spirometry data spanning periods of 10 to 25 years were analysed for 232 divers. Forced vital capacity (FVC) and forced expiratory volume in one second (FEV1) declined with increasing duration of diving, but slightly less than predicted with increasing age, while peak expiratory flow (PEF) declined more than expected for age in longer-term divers. The changes in PEF were statistically significant, and correlated with duration of diving exposure, initial age and final BMI. Nevertheless, the changes were small and probably clinically insignificant.
Conclusion
We compared changes in spirometric parameters over long periods of occupational diving with normative data and found no clinically significant differences that could be attributed to diving. We found no justification for routine spirometry in asymptomatic divers.
Keywords: Lung function, Fitness to dive, Surveillance, Occupational diving, Medicals – diving
Introduction
The lung function of professional divers is important to the performance of their role. The question of whether diving causes lung function deterioration in the long-term has been investigated previously, and changes such as blunted respiratory response to carbon dioxide,[ 1] airway inflammation, airway hyper-reactivity[ 2 , 3] and reduced diffusion capacity for carbon monoxide[ and reduced diffusion capacity for carbon monoxide[ 4 - 7] have been reported. Various pathophysiological theories have been advanced to account for these changes including repeated exposures to the pulmonary effects of inert gas microemboli, and to hyperoxia leading to pulmonary oxygen toxicity.[ 2 , 3]
However, a 1994 consensus recognised that the various published investigations of changes in lung function among occupational divers were of limited quality and often produced conflicting results. The consensus included a plea for further research, particularly longitudinal studies, to further characterise any correlation with diving and any long-term impact on health.[ 8] Since then, studies have continued to produce inconsistent results based on small sample sizes and variable methods.[ 9 - 18] The ongoing limitations of research in this area are evident from two recently published literature reviews.[ 9 , 19]
The first, comparing relevant papers over 30 years to 2014 found fourteen such studies,[ 9] seven of which followed divers for an average of five years or less,[ 10 - 16] and only one for longer than 10 years.[ 17] Seven studies involved fewer than 50 divers. Prospective studies used appropriately matched control groups, while the retrospective studies used different normative datasets for comparison with the divers. Only three longitudinal studies reported changes as percentages of the reference values.[ 11 , 16 , 18]
The second is the most recent and comprehensive review of both short and long-term effects of diving on lung function.[ 19] This included commentary on all published longitudinal studies (including recreational divers) and a large 30-year study of Dutch naval divers[ 20] over a 70-year period to 2017. It emphasised that although past studies have provided disparate results, most agree that lung function changes are of minimal clinical significance. The exception is for the small number of individuals who may be adversely affected in the long-term, but are likely to be identifiable based on their particular diving history or exposure and physiological predisposition to lung function impairment.
Using a large database containing serial spirometry measurements on occupational divers over periods ranging from 10 to 25 years, we sought evidence for any deterioration in lung function that was disproportionate to changes predicted by age-adjusted normative values. The null hypothesis was that there would be no difference between age-adjusted predicted values for spirometric indices and the values obtained from long-term occupational divers.
Method
Ethical approval for this study was granted by the Waitemata District Health Board Human Ethics Committee (reference number RM 13630).
The New Zealand national occupational divers' database was searched for all divers registered for 10 years or longer, whether currently registered or not. The identified divers' medical records were searched for spirometric data. Inclusion in this study required the diver to have two adequate spirometry records, including at least forced vital capacity (FVC) and forced expiratory volume in one second (FEV1), but preferably also peak expiratory flow (PEF), separated by at least 10 years. For each diver the most recent and the earliest suitable recordings were selected. De-identified demographic data were collated for stratification and comparison. Changes in FVC, FEV1, FEV1/FVC ratio and PEF between the first and most recent suitable recordings were calculated and expressed as medians for the entire cohort combined, and with subjects stratified into groups with 10–15 years and > 15 years diving activity between observations. In parallel, two algorithms (see Appendix), the Global Lung Function Initiative (GLI-2012) and the third National Health and Nutrition Examination Survey (NHANES III), were used to calculate the age–related changes in these parameters expected for each subject's gender, height and age at the first measurement, and subsequent period of observation. These changes were also expressed as medians for the entire cohort combined, and with subjects stratified into groups with 10–15 years and > 15 years diving activity between the first and final (here termed the 'second') observations.
The primary outcome of this study was a comparison of the changes in spirometric indices over the period of observation to those predicted on the basis of ageing alone, in order to deduce any independent effect of occupational diving. Predicted values and z-values for FVC, FEV1 and the FEV1/FVC ratio were generated using software downloaded from the GLI website.[ 21] Similarly, the predicted values for the same parameters, as well as those for PEF, derived using the NHANES III equations, were extracted from published data for the appropriate ethnic group, gender, height and age.[ 22] Correlations were also sought between changes in lung function and age of the diver, smoking status, gender and body mass index (BMI).
Statistical analysis was performed using SAS® v9.4 software (SAS Institute Inc., Cary, North Carolina, USA). Frequency and proportion (%) were used for describing categorical variables, such as gender, smoking status and type of diving. Median with minimum and maximum were used for describing the continuous variables including age and BMI as they did not follow normal distribution. Duration of diving experience was categorical in some comparison analyses and continuous in the regression models. Median, and its distribution-free 95% confidence intervals, was used to present the study outcomes including observed values, predicted values, percent predicted values and z values of FVC, FEV1, FEV1/FVC and PEF. Spearman correlation was used for simple correlation analysis. Robust regression models (an alternative to least squares regression when data are contaminated with outliers, or for detecting influential observations) and analysis of co-variance with general linear models, were used in multiple regression analyses. A P-value of < 0.05 was considered to be statistically significant. To account for outliers and avoid the possibility of missing important information, type 1 error was not adjusted for multiple comparisons.
Results
The entry criteria were satisfied by 232 divers. The mean interval between recordings was 13.6 years. The group was stratified into those with 10–15 years (n = 159, mean = 11.6 y), and those with greater than 15 years (n = 73, mean 18.1 y) between spirometric recordings. Demographic characteristics, including breakdown into the various occupational diving categories, are represented in Table 1. Of note, the commonest type of diving was 'scientific', comprising over one third of the group. The group was predominantly male and exclusively so for the more experienced group. It should be noted that the group comprised divers using a variety of breathing apparatus, including scuba (open and closed-circuit), surface-supplied gas and saturation systems. Non-smokers (never smoked) comprised three quarters of the group, while the vast majority of the remainder were ex-smokers. The entry criteria dictated that this was a relatively old group of divers, with an average age of 48 y at the time of the second assessment. There was a small mean increase in BMI (1.6 kg∙m-2) over the assessment period.
Table 1. Characteristics of 232 occupational divers stratified by duration of career; ∗ 2nd medical refers to data collected from the divers' most recent medical examinations; BMI – body mass index .
| All(n = 232) | > 15 y(n = 73) | 10–15 y(n = 159) | |
| Male/Female (%) | 90/10 | 100 | 86/14 |
| non-smoker (%) | 74 | 70 | 75 |
| smoker and ex-smoker (%) | 26 | 30 | 25 |
| No. dives/year (at 2nd medical ∗) | 60 (0−350) | 55 (0−272) | 62 (0−350) |
| Age (at 2nd medical∗) | 48 (31−75) | 52 (38−75) | 46 (31−73) |
| Δ BMI (kg∙m-2) | 1.6 (-6.3−12.2) | 2 (-4.1−9.0) | 1.4 (-6.3−12.2) |
| Δ Age (years) | 13.6 (10−25) | 18.1 (15−25) | 11.6 (10−14) |
| Oxygen saturation (%) | 98 (1) | 97 (1) | 98 (1) |
| Employment | |||
| Scientific (%) | 35 | 30 | 36 |
| Commercial (%) | 19 | 24 | 17 |
| Instructor (%) | 17 | 9 | 21 |
| Construction (%) | 14 | 14 | 14 |
| Aquaculture (%) | 7 | 9 | 6 |
| Military/Police/Customs (%) | 4 | 4 | 4 |
| Filming (%) | 3 | 10 | 1 |
| HBU attendant (%) | 1 | 0 | 1 |
Initial FVC measurements among our divers were not significantly different from the age-adjusted norms. Comparisons of subsequent observed and predicted changes in spirometric indices over the period of observation are presented in Table 2. These data showed a reduction in FVC and FEV1 with increasing duration of diving career, but this was less than predicted on the basis of increasing age by either prediction method. Similarly, the FEV1/FVC ratio decreased in longer-term divers but essentially as predicted on the basis of increasing age. PEF decreased as predicted by NHANES III for the group overall, but statistically significantly more than predicted for age for the longer career group, and less than predicted for the shorter career group. The overall reduction in observed PEF values together with an increase in percentage of predicted values is explained by the slower rate of decline in observed relative to predicted values.
Table 2. Long-term changes in observed and predicted values of diver lung function; data are presented as medians (95% confidence limits); FVC – forced vital capacity; FEV1 – forced expiratory volume in 1 sec; PEF – peak expiratory flow; ∗ For PEF, n (all) = 195, n (> 15y) = 56, n (10-15y) = 139 .
| Diving duration group | Lung function parameter | |||
| All (n = 232) | Δ FVC (L) | Δ FEV1 (L) | Δ FEV1/FVC | Δ PEF∗(L⋅s-1) |
| Observed | -0.16 (-0.22, -0.07) | -0.30 (-0.36, -0.21) | -0.04 (-0.04, -0.03) | -0.31 (-0.68, -0.08) |
| Predicted (NHANES III) | -0.28 (-0.32, -0.25) | -0.35 (-0.39, -0.32) | -0.03 (-0.03, -0.03) | -0.29 (-0.37, -0.23) |
| Predicted (GLI) | -0.32 (-0.35, -0.29) | -0.37 (-0.35, -0.40) | -0.02 (-0.03, -0.02) | X |
| > 15y (n = 73) | ||||
| Observed | -0.36 (-0.60, -0.20) | -0.52 (-0.69, -0.36) | -0.03 (-0.05, -0.02) | -0.79 (-1.41, -0.17) |
| Predicted (NHANES III) | -0.41 (-0.45, -0.37) | -0.50 (-0.55, -0.46) | -0.04 (-0.04, -0.03) | -0.50 (-0.60, -0.42) |
| Predicted (GLI) | -0.47 (-0.52, -0.40) | -0.55 (-0.58, -0.51) | -0.03 (-0.03, -0.03) | X |
| 10–15y (n = 159) | ||||
| Observed | -0.07 (-0.16, 0.04) | -0.22 (-0.31, -0.15) | -0.04 (-0.05, -0.03) | -0.10 (-0.55, 0.16) |
| Predicted (NHANES III) | -0.23 (-0.25, -0.19) | -0.29 (-0.31, -0.27) | -0.02 (-0.02, -0.02) | -0.22 (-0.28, -0.15) |
| Predicted (GLI) | -0.27 (-0.29, -0.23) | -0.32 (-0.35, -0.30) | -0.02 (-0.02, -0.02) | X |
The annual changes in observed values of FVC, FEV1 and PEF are presented in Table 3. However, these data do not discriminate between any effect of diving exposure and changes expected with ageing. Therefore, we present the observed changes as deviations in percentage of predicted values (Table 4) and as changes in z-values (Table 5, GLI comparison only).
Table 3. Annual observed change in occupational diver lung function; FVC – forced vital capacity; FEV1 – forced expiratory volume in 1 sec; PEF – peak expiratory flow; ∗ For PEF, n (All) = 195, n (> 15y) = 56, n (10–15y) = 139; data are presented as medians (95% confidence limits) .
| Lung function | Diving duration group | ||
| parameter | All (n = 232) | > 15 y (n = 73) | 10−15 y (n = 159) |
| Δ FVC (ml) | -10.3 (-16.7, -5.8) | -21.3 (-33.3, -10.5) | -5.8 (-13.3, -3.3) |
| Δ FEV1(ml) | -23.2 (-28.3, -17.3) | -29.6 (-37.5, -19.3) | -20.0 (-26.0, -12.9) |
| Δ PEF∗(ml·sec-1) | -21.9 (-46.4, -6.7) | -43.7 (-73.7, -8.3) | -9.0 (-45.8, 14.0) |
Table 4. Long-term changes in % predicted values of diver lung function using GLI-2012 and NHANES III values; FVC – forced vital capacity; FEV1 – forced expiratory volume in 1 sec; PEF – peak expiratory flow; ∗ For PEF, n (All) = 195, n (> 15y) = 56, n (10–15y) = 139; data are presented as medians (95% confidence limits) .
| Lung function | Diving duration group | |||||
| parameter | All (n = 232) | > 15 y (n = 73) | 10−15 y (n = 159) | |||
| GLI | NHANES III | GLI | NHANES III | GLI | NHANES III | |
| Δ FVC | 3.1 (1.8, 5.2) | 2.6 (1.0, 4.5) | 0.5 (-2.0, 5.2) | 0.5 (-2.4, 3.7) | 3.6 (2.4, 6.7) | 4.1 (1.8, 5.9) |
| Δ FEV1 | 2.5 (0.6, 3.8) | 2.0 (0.2, 3.1) | 2.4 (-3.0, 4.0) | 0.5 (-3.6, 4.4) | 2.5 (0.6, 4.4) | 2.3 (0.6, 4.0) |
| Δ FEV1/FVC | -1.35 (-2.5, -0.1) | -1.3 (-2.3, -0.1) | 0 (-2.6, 1.5) | -0.1 (-1.6, 2.4) | -2.5 (-2.7, -0.2) | -1.4 (-2.6, -1.2) |
| Δ PEF∗ | X | 0.4 (-3.6, 3.3) | X | -1.95 (-8.4, 3.6) | X | 0.5 (-3.1, 5.5) |
Table 5. Long-term changes in z-values of diver lung function using GLI-2012 values; FVC – forced vital capacity; FEV1 – forced expiratory volume in 1 sec; data are presented as medians (95% confidence limits) .
| Lung function | Diving duration group | ||
| All (n = 232) | > 15 y (n = 73) | 10−15 y (n = 159) | |
| Δ FVC | 0.25 (0.11,0.43) | 0.04 (-0.24,0.39) | 0.34 (0.18,0.52) |
| Δ FEV1 | 0.18 (0.05,0.34) | 0.08 (-0.21,0.36) | 0.19 (0.05,0.38) |
| Δ FEV1/FVC | -0.18 (-0.32,-0.07) | -0.03 (-0.31,0.19) | -0.23 (-0.35,-0.14) |
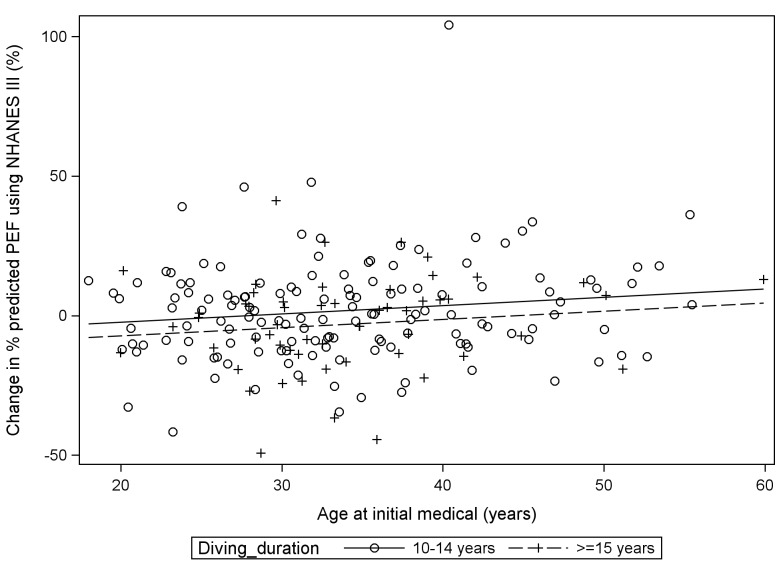
There was a minor rise in percentage of predicted value and z-value of FVC (3.1%, 0.25 respectively), a smaller rise for FEV1 (2.5%, 0.18 respectively), and a consequent reduction in the values for the FEV1/FVC ratio (-1.35%, -0.18 respectively). These changes were greater for the less experienced sub-group, so there was a trend towards zero change with increasing duration of occupational diving. The magnitude of PEF changes was greater for the more experienced sub-group, with a significant median reduction in percentage of predicted value (-1.95%). The analysis of covariance plot represented by Figure 1 demonstrates the small but significant difference between the increase in percent predicted values of PEF (using NHANES III data) for the two groups of divers based on their age at initial examination.
Figure 1.
Relationship between age at the earliest spirometry test, diving exposure and long-term changes in % predicted values of divers’ peak expiratory flow (PEF) based on NHANES III prediction equations
Multiple regression analysis showed that the change in percent of predicted value of PEF correlated significantly with the age of the diver at initial assessment (P = 0.002), the duration of diving exposure (P = 0.037) and the BMI at second assessment (P = 0.035). The only other significant correlation was between the BMI at second assessment and changes in z-values and % predicted values of FVC (P = 0.04 and P = 0.025 respectively) and FEV1/FVC (P = 0.017 and P = 0.009 respectively). No significant correlations were apparent between changes in any of the lung function parameters and smoking status. Diver age and gender were controlled for in the comparison data and no additional correlation was found with these parameters.
Discussion
From the very early days of occupational diving it has been widely accepted that detailed physical examination, with a strong focus on respiratory function, was mandatory for screening of prospective occupational divers and for routine surveillance of experienced divers. Traditionally, routine surveillance entailed annual measurement of spirometric indices, and this practice has prevailed in most countries despite a lack of evidence for its utility.
This study was undertaken because of inconsistent findings from small studies of divers' lung function, variable control methods and a lack of studies extending as far as 25 years of diving activity. Our database contained 232 occupational divers with adequate spirometric recordings covering a period of 10–25 years of diving activity. We compared changes in the principal spirometric parameters with normative data and found no significant differences that could be attributed to diving experience rather than increasing age. Therefore, the main finding of this study relevant to working divers is that while small changes in some spirometric parameters may reach statistical significance, there is no evidence of change attributable to diving that is likely to be of clinical significance in the long-term. Prospective occupational divers, and those who remain in the industry for many years, should be encouraged by this further evidence of the relative lack of harm to the respiratory system from diving.
These results were confluent with our previous study of a cohort of 336 divers over a mean period of 5.6 years, except that in that study we found small but statistically significant reductions in the percent of predicted values for FEV1 and PEF using NHANES III normative data.[ 22] The current study found no significant change for FEV1 and a small but statistically significant rise in percent of predicted PEF. Our results also support those of a prospective study of 37 Norwegian professional divers who showed no correlation between diving exposure (total number of dives) and FVC and FEV1 over 12 years.[ 17]
These findings also cast doubt on the utility of routine annual spirometric measurement in all occupational divers. There seems little point in conducting serial investigation for changing spirometry over a diving career in the absence of convincing evidence that such change is a feature of long-term diving. However, we recognise that spirometry would be indicated if some other aspect of a diver’s medical history, likely to be detected on their annual health questionnaire, implied that significant change was plausible (such as a significant respiratory illness in the preceding year).
LIMITATIONS
First, and most significantly, we used years of occupational diving as a surrogate for diving exposure. Clearly, this is a blunt measure of exposure, but we had no access to more precise data. The ideal would have been to record number of dives with times, depths and gases used, but we lacked such records over the long period of observation involved. Even the number of dives per year was not consistently recorded, and most likely inaccurate. Such detail may only be available in the setting of a prospective study. With this limitation acknowledged, it nevertheless seems implausible that divers would maintain medical fitness certification for occupational diving over a prolonged period in the absence of moderate diving activity.
Secondly, we cannot exclude some degree of selection bias, where divers may have quit with less than 10 years' experience due to deteriorating lung function. We know from a previous study that there is an attrition rate of nearly 80% over a five-year period for New Zealand occupational divers, suggesting the possibility of a significant 'healthy worker effect'. However, we think this is unlikely to have influenced our findings in relation to spirometric changes. The collective qualitative experience of the medical authors among our group is that occupational diver attrition due to deterioration in lung health in the absence of a discrete accident (such as pulmonary barotrauma) or a non-diving medical explanation is virtually unheard of. For example, in the current study, no diver was found to have clinically significant lung function deterioration. From our previous study of those remaining in the job for a mean of 5.6 years, only two out of 336 divers were found to have abnormal spirometry, but after further investigation neither was considered unfit for diving.[ 23]
Thirdly, we restricted this study to what we considered to be the principal spirometric parameters, namely FVC, FEV1, FEV1/FVC ratio and PEF, to avoid erosion of the sample size, since the other parameters were far less consistently recorded, especially in the older clinical records. We do not believe this detracts from our findings, but it does make this study a less than complete survey of lung function.
Fourthly, as with most retrospective studies, the quality of spirometric data was beyond our control, and likely to have varied widely.
Finally, we chose to compare our data with the NHANES III and GLI normative data because these sets of prediction equations are widely accepted internationally, despite the fact that neither set is based on data drawn from the New Zealand population. An argument against using such 'normal' population data is that, with a cohort comprising only divers, we are not dealing with a 'normal' population, so they would more appropriately be compared with a control group of similar fitness engaged in equally strenuous activity. Previous studies have used such occupations as submariners,[ 15] policemen[ 24] and non-diving offshore workers[ 25] for comparison. However, any error introduced because of our selection of comparative data is not likely to be significant, and we have previously demonstrated close alignment of the NHANES III data with data from NZ divers.[ 18]
Conclusions
The small changes in lung function found in divers with a 10–25 year occupational diving history are generally confluent with predictions based on ageing, and not likely to be clinically significant. There appears to be no justification for routine spirometry in asymptomatic divers.
Appendix
Brief background to the derivation of spirometric reference values used in this study.
THIRD NATIONAL HEALTH AND NUTRITION EXAMINATION SURVEY (NHANES III)
The NHANES III prediction equations are based on data collected from a random sample of the population across the USA between 1988 and 1994. The initial total of 20,627 subjects from three ethnic groups (Caucasian, Afro-American and Mexican-American) was reduced to 7,429 after exclusions to comply with the criteria that all subjects were asymptomatic, life-long non-smokers and could provide at least two acceptable spirometric manoeuvres. Subjects were between 8 and 80 years old. The analysis and resulting prediction equations were published in 1999.22 The equations are race/ethnic group and gender specific, with age and height as independent variables. The equations are polynomials of the form:
Lung function parameter = b0 + b1xAge + b2xAge2 + b3xHeight2
where b0 is the intercept and b1, b2 and b3 are coefficients that vary for each lung function parameter with race/ethnic group and gender. There are also different sets of coefficient values for males under 20 and females under 18 years old. This set of equations gained considerable global popularity, and has recently been the reference dataset most commonly used throughout New Zealand.[ 26]
GLOBAL LUNG FUNCTION INITIATIVE
A new set of lung function reference value prediction equations was developed and published in 2012 by the Global Lung Function Initiative (GLI-2012).[ 21] This large collaborative study resolved many of the inherent problems with the existing collection of published prediction equations for spirometric reference values. Specifically, problems with existing datasets included small population/ethnic group sample numbers, out-moded methodologies and discontinuity between age groups. Through collaboration with researchers from 70 centres in 26 countries across five continents, and including data from earlier significant studies, such as NHANES III, continuous equations suitable for ages from three to 95 years based on data from 74,187 healthy non-smokers were derived.[ 21] The equation is in the form of a linear regression expression using age and height as independent variables, with coefficients dependent on lung function parameter, gender and ethnic group. The four ethnic groupings specified are Caucasian (providing most of the data), Afro-American and North and South East Asian. Another set of equations, based on an average of the others, can be used for 'other' ethnic groupings. The authors consider the development of this dataset complete for the Caucasian group, but ongoing for possible future modification when further data has been collected from the other ethnic groups. Calculations for individuals or large groups have been facilitated by the GLI-2012 group’s provision of the required software on their website.[ 21] This dataset has been endorsed by the major respiratory and thoracic societies from Europe, America, Asia, Australia and New Zealand.
Footnotes
Acknowledgements
We thank Mr Murray Polson (CEO, Erudite Software Ltd) for developing and maintaining the electronic database for New Zealand occupational divers, and retrieving much of the data required for this study.
Funding: nil
Conflict of interest: nil
Contributor Information
C Sames, Slark Hyperbaric Unit, Waitemata District Health Board, Auckland, New Zealand.
DF Gorman, Dept of Medicine, University of Auckland, Auckland.
SJ Mitchell, Dept of Anaesthesiology, University of Auckland.
L Zhou, Waitemata and Auckland District Health Boards, Auckland.
References
- Earing CMN, McKeon DJ, Kubis H. Divers revisited: The ventilator response to carbon dioxide in experienced scuba divers . Respir Med. 2014. pp. 758–65. [DOI] [PubMed]
- Thorsen E, Segedal K, Kambestad B, Gulsvic A. Divers' lung function: small airways disease? . Br J Ind Med. 1990;47(8):519–23. doi: 10.1136/oem.47.8.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thom SR, Milovanova TN, Bogush M, Bhopale VM, Yang M, Bushmann K, et al. Microparticle production, neutrophil activation, and intravascular bubbles bubbles following open-water SCUBA diving . J Appl Physiol. 2012;112:1268–78. doi: 10.1152/japplphysiol.01305.2011. [DOI] [PubMed] [Google Scholar]
- Cotes JE, Davey IS, Reed JW, Rooks M. Respiratory effects of a single saturation dive to 300m . Br J Ind Med. 1987;44:76–82. doi: 10.1136/oem.44.2.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dujic Z, Eterovic D, Denoble P, Krstacic G, Tocilj J, Gosovic S. Effect of a single air dive on pulmonary diffusing capacity in professional divers . J Appl Physiol. 1993;74:55–61. doi: 10.1152/jappl.1993.74.1.55. [DOI] [PubMed] [Google Scholar]
- Thorsen E, Segedal K, Kambestad BK. Mechanisms of reduced pulmonary function after a saturation dive . Eur Respir J. 1994;7:4–10. doi: 10.1183/09031936.94.07010004. [DOI] [PubMed] [Google Scholar]
- Thorsen E, Risberg J, Segedal K, Hope S. Effects of venous gas microemboli on pulmonary gas transfer function . Undersea Hyperb Med. 1995;22:347–53. [PubMed] [Google Scholar]
- Hope A Lund T Elliott DH Halsey MJ Wiig H Long-term health effects of diving. An international consensus conference. In: Brubakk K Neuman TS, editors. Bennett and Elliott's physiology and medicine of diving 5th ed; Edinburgh: Saunders; 2003. p. 656 [Google Scholar]
- Pougnet R, Pougnet L, Lucas D, Uguen M, Henckes A, Dewitte J, et al. Longitudinal change in professional divers’ lung function: literature review . Int Marit Health. 2014;65:223–9. doi: 10.5603/IMH.2014.0042. [DOI] [PubMed] [Google Scholar]
- Watt SJ. Effect of commercial diving on ventilatory function . Br J Ind Med. 1985;42:59–62. doi: 10.1136/oem.42.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorsen E, Segadal K, Kambestad BK, Gulsvik A. Pulmonary function one and four years after a deep saturation dive . Scand J Work Environ Health. 1993;19:115–20. doi: 10.5271/sjweh.1498. [DOI] [PubMed] [Google Scholar]
- Skogstad M, Thorsen E, Haldorsen T. Lung function over the first 3 years of a professional diving career . Occup Environ Med. 2000;57:390–5. doi: 10.1136/oem.57.6.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick DT, Conkin J. Improved pulmonary function in working divers breathing nitrox at shallow depths . Aviat Space Environ Med. 2003;74:763–7. [PubMed] [Google Scholar]
- Lucas D, Loddé D, Choucroun P, Jegaden D, Mialon P, Sarni D, et al. Five year study of changes in the lung function of a cohort of 31 professional divers . Med Marit. 2005;5:17–28. [Google Scholar]
- Tetzlaff K, Theysohn J, Stahl C, Schlegel S, Koch A, Muth CM. Decline of FEV1 in scuba divers . Chest. 2006;130:238–43. doi: 10.1378/chest.130.1.238. [DOI] [PubMed] [Google Scholar]
- Chong SJ, Tan TW, Lim JY. Changes in lung function in Republic of Singapore Navy divers . Diving Hyperb Med. 2008;38:68–70. [PubMed] [Google Scholar]
- Skogstad M, Skare O. Pulmonary function among professional divers over 12 years and the effect of total number of dives . Aviat Space Environ Med. 2008;79:883–7. doi: 10.3357/ASEM.2333.2008. [DOI] [PubMed] [Google Scholar]
- Sames C, Gorman DF, Mitchell SJ, Gamble G. The long-term effects of compressed gas diving on lung function in New Zealand occupational divers: a retrospective analysis . Diving Hyperb Med. 2009;39:133–7. [PubMed] [Google Scholar]
- Tetzlaff K, Thomas PS. Short- and long-term effects of diving on pulmonary function . Eur Respir Rev. 2017;26 doi: 10.1183/16000617.0097-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voortman M, van Ooij PJAM, van Hulst RA, Zanen P. Pulmonary function in professional navy divers and changes during their professional careers . Undersea Hyperb Med. 2016;43:649–57. [PubMed] [Google Scholar]
- Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH. et al. ERS Global Lung Function Initiative . Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations . [cited 2017 December 26];Eur Respir J. 2012 40:1324–43. doi: 10.1183/09031936.00080312. Available from: http://www.ers-education.org/guidelines/global-lung-function-initiative/tools.aspx . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general US population . Am J Respir Crit Care Med. 1999;159:179–87. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- Sames C, Gorman D, Mitchell SJ, Gamble G. Utility of regular medical examinations of occupational divers . Intern Med J. 2009;59:763–70. doi: 10.1111/j.1445-5994.2009.02055.x. [DOI] [PubMed] [Google Scholar]
- Skogstad M, Thorsen E, Haldorsen T, Kjuus H. Lung function over six years among professional divers . Occup Environ Med. 2002;59:629–33. doi: 10.1136/oem.59.9.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macdiarmid JI Ross JAS Taylor CL Watt SJ Adie W Osman LM et al. Co-ordinated investigation into the possible long-term health effects of diving at work. Examination of the long-term health impact of diving: the ELTHI Study. University of Aberdeen, Scotland: HSE Books; 2004. [Google Scholar]
- Marsh S, Aldington S, Williams M, Weatherall M, Robiony-Rogers D, et al. Pulmonary function testing in New Zealand: the use and importance of reference ranges . Respirology. 2007;12:367–74. doi: 10.1111/j.1440-1843.2007.01071.x. [DOI] [PubMed] [Google Scholar]