Introduction
More than half of prisoners in the United States are estimated to suffer from a substance use disorder (National Center on Addiction and Substance Abuse, 2010). In multiple studies, substance use disorder treatment in jail and prison has been shown to reduce post-release substance use and criminal justice involvement (Kelly, Phinney, & Moos, 2005, Ettner et al., 2006). Recently, mindfulness meditation and yoga in incarcerated settings have shown promising results for reducing drug use upon release (Audy, Cope, and Liebling 2017, Lyons and Cantrell 2016). Mindfulness may be defined as intentional regulation of attention to and awareness of the present moment, and nonjudgmental acceptance of the ongoing flow of sensations, thoughts, and emotional states. Prison-based studies of mindfulness have typically been intensive retreats during which participating prisoners are physically separated from the general population (Bowen et al., 2006, Perelman et al., 2012). One promising shorter treatment modality that could be integrated into existing correctional drug treatment programs is Mindfulness Based Relapse Prevention (MBRP). MBRP is structured similarly to Mindfulness Based Stress Reduction (Kabat-Zinn 1982), and includes yoga, sitting, and walking meditation, with additional discussion of applying mindfulness to prevent drug and alcohol relapse (Bowen, Chawla, & Marlatt, 2011). A study of effectiveness of MBRP with women referred by the criminal justice system reported significantly fewer drug use days and fewer legal and medical problems, compared to a relapse prevention protocol (Witkiewitz et al. 2014). In a smaller study of a similar population MBRP led to fewer drug use days and lower addiction severity (Witkiewitz, Brenna, & Bowen, 2013). Two randomized controlled trials of MBRP as aftercare for patients who had completed treatment in the community showed significantly greater reductions in substance use in the MBRP arm compared with treatment as usual (Bowen et al., 2009) and with cognitive behavioral treatment (Bowen et al., 2014). A recent randomized trial compared MBRP to contingency management and showed greater reductions in stimulant use in the MBRP arm, particularly among those with depression and anxiety disorders (Glasner et al., 2017). An abbreviated mindfulness-based intervention with a non-clinical student population demonstrated improvements in mindfulness and positive affect compared to a control group, suggesting the utility of a broad application and the feasibility of shortening the intervention (Demarzo et al., 2017).
A recent meta-analysis has suggested that the benefits of MBRP over other treatments in reducing substance use may be limited (Grant et al. 2017). However, to the extent that mindfulness interventions in general may have other beneficial effects for prisoners, MBRP may be particularly useful within a jail. A common problem with many drug treatment programs is that the effects are short-lived; multiple treatment episodes are often needed to achieve lasting recovery, and relapse rates are high (Vaillant, 1995). There is evidence to suggest that the effects of mindfulness meditation training, if a mindfulness practice is established, may last longer than cognitive behavioral treatment (Bowen et al., 2014). MBRP might therefore benefit prisoners released into the community who do not access aftercare. Furthermore, MBRP may have direct benefits on well-being for participants in jails and prisons (Grant et al. 2017, Auty, Cope, & Liebling, 2017). One small study in a prison in Taiwan suggested that MBRP was effective in reducing negative affect compared to treatment as usual (Lee, Bowen, & Bai, 2011). Furthermore, mindfulness training has been shown to reduce trauma symptoms for participants with trauma histories (Goodman, 2012, Vujanovic, 2011), and PTSD symptoms are not a barrier to prisoners’ volunteering for and benefiting from meditation (Simpson et al., 2007). One study with an incarcerated population, in the same treatment program as the current study, found a prevalence rate of 21% of probable PTSD (Ruzich, Reichert, & Lurigio, 2014).
Jails in the United States admit almost 20 times as many inmates per year as prisons (Subramanian, Delaney, Roberts, Fishman, & McGarry, 2015). While many jails have substance use disorder treatment programs, these programs could be enriched if there were a body of evidence on programs effective in this setting. However, such research is difficult to conduct for several reasons. First, unpredictability as to length of stay means that it is difficult to give the same dosage of treatment to every research participant. Second, while one pilot study randomized jail inmates into a mindfulness condition vs. treatment as usual (Malouf et al., 2017), no tests of mindfulness interventions in jails or prisons have included an active control group that could account for attention effects, or control for motivation to participate in the treatments. Federal regulations governing research with prisoners discourage treatment as usual as a control, specifying that all prisoner research participants should directly benefit from the study, unless specific permission is granted.1 However, despite these federal guidelines, there have been few randomized controlled trials involving a comparison condition other than treatment as usual in jails and prisons. In the closed social environment of a jail, two participants receiving different treatments have opportunities to discuss the treatments, leading to contamination between study arms, and jail administration may not allow such an arrangement.
Finally, while mindfulness techniques are universal, the way that they are presented and taught may need to be adapted for men of color from urban communities (Amaro 2014), who are disproportionately represented in the criminal justice system and in jails. A study of application of MBRP to a racially and ethnically diverse population of low-income women reported reduced alcohol and drug use and reduction of perceived stress (Amaro et al., 2014). However, no studies with male substance users in jails that we are aware of have involved a culturally competent trainer of color from a similar background to that of the participants.
Study Design
We sought to design an experimental study of a mindfulness based relapse prevention intervention that addressed these barriers to research in a jail environment. Institutional Review Board approval was obtained from the authors’ institution and from the IRB of the jail. In addition, a Certificate of Confidentiality was obtained from the National Institutes of Health. The study was conducted within a drug treatment program at a large urban jail, in which participants were court ordered to specified lengths of treatment. We included an attention control group receiving a communications skills curriculum. Participants were assigned to the treatment vs comparison groups via a novel, cohort based randomization process, described below. In contrast to many research studies, the mindfulness trainings for this mostly African American incarcerated population were conducted by a culturally competent African American male trainer from a socioeconomic background similar to the detainees. To our knowledge, no such individuals have been formally trained in the MBRP program. This trainer has taught stress management via internal self regulation since 1979, including as a therapist for persons with substance use disorders. He also has three decades of experience teaching yoga and meditation to a variety of types of students, including incarcerated juveniles. With the assistance of the Advisory Board, this trainer worked through the MBRP manual and assisted with its extensive adaptation for this population.
Intervention Development
Adaptation of the MBRP curriculum was a multistage process. Using a group of university students and a pre implementation pilot with 11 participants in the jail, we restructured the published MBRP program as a manualized six-week program, in collaboration with the program’s author. This length of time is a balance between the dosage necessary to establish a mindfulness practice (Auty, Cope & Liebling, 2017), and the typically short lengths of stay in jail. The published MBRP manual was rewritten and simplified, based on advisory board feedback, and feedback during the training sessions. A seeing meditation exercise and the “Mountain Meditation” were deleted due to the jail setting and poor relatability. The content of some other meditations were changed; for example, the “Walking down the street” exercise, in which participants reflect on their thoughts and feelings toward an ambiguous stimulus, was changed to a “collect call that is dropped” which is a concern of inmates. Each session consisted of a mindfulness meditation exercise and discussion (approx. 40 minutes) and an exercise applying mindfulness to everyday life and high drug relapse risk situations (approx. 30 minutes). Based on input from the focus group and facilitators, each session began with mindful movement/stretching/chair yoga exercises (5 minutes). An outline of the sessions is shown in Figure 1, and the complete revised manual is available from the corresponding author.
Figure 1:
MBRP Session Outline
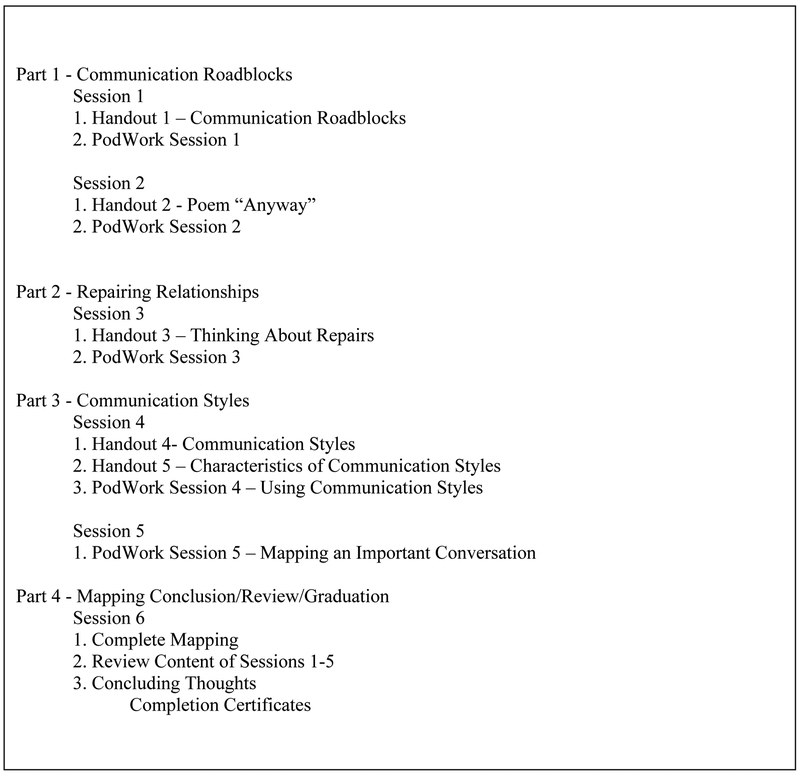
The curriculum utilized in the control arm of the study was adapted from Texas Christian University’s (TCU) Mapping-Enhanced Counseling Manuals for Adaptive Treatment (Joe et al 2012). Listed in the National Registry of Evidence-based Programs and Practices, TCU’s interventions are designed to be administered in substance use disorder treatment programs in a variety of settings including jail-based treatment. TCU curricula are specifically designed to be “mixed and matched” to fit logistical and treatment needs in these settings. This flexibility allowed us to develop a 6 session curriculum matching the mindfulness condition in frequency but 20 minutes shorter. An outline of the comparison arm curriculum is shown in Figure 2.
Figure 2:
Communications Skills Session Outline
Study Population
We conducted both the experimental and comparison interventions in a therapeutic community in a separate wing of the jail. Participants are ordered to this program by a judge either pretrial or because of a violation of probation. Because, as noted above, delivery of different interventions at the same time was not feasible, we enrolled participants into the experimental and comparison groups as randomized cohorts over time, of approximately 25 participants per cohort. The planned order of the 6 experimental [E] and 6 control [C] cohorts across the entire study was randomized with the resulting order:
E, C, C, E, E, C, C, E, E, C, E, C.
Eligibility criteria included having been incarcerated for at least two weeks, English speaking, able to understand the consent process, and with at least six weeks remaining on their court ordered stay in the program. After a brief announcement by staff about the study, research staff obtained informed consent from each potential participant. The baseline assessment questions were read aloud to participants and included demographics, drug use behavior prior to incarceration, and psychosocial measures. Within two weeks of the end of the experimental and control intervention sessions (45 days after baseline), participants again completed psychosocial assessments. Participants were paid $15 for each of the two assessments, deposited into their commissary accounts at the jail.
Measures
How to measure change in mindfulness as a result of a mindfulness intervention is a matter of controversy (Grossman, 2008). In line with several other studies, in this study mindfulness was measured by the Five Facets Mindfulness Questionnaire (FFMQ) (short form) (Bohlmeijer, Klooster, Fledderus, Veehof, & Baer, 2011) a 24 item questionnaire that measures five distinct dimensions of mindfulness: observing, describing of emotions, nonjudging, nonreactivity to emotional states, and acting with awareness. In addition, we administered the 14-item Freiburg Mindfulness Inventory (FMI) (Walach, Buchheld, Buttenmüller, Kleinknecht, & Schmidt, 2006), which measures a single construct of mindfulness and whose items may be more appropriate for a low literacy population. Additional psychosocial measures consisted of the Beck Anxiety Inventory (Beck, Epstein, Brown, & Steer, 1988), the Penn Alcohol/Drug Craving Scale (Flannery, Volpecelli, & Pettinati, 1999) and the PTSD Symptom Checklist (Blanchard, Jones-Alexander, Buckley, &Forneris, 1996). The PTSD Symptom Checklist yields both a scale score, and a cutoff for probable PTSD diagnosis. Cronbach’s alpha coefficients for the psychological measures at baseline were acceptable, ranging from α = 0.69 (the Five-Facets Mindfulness Questionnaire) to α = 0.92 (Beck Anxiety Inventory), for the pilot cohort and first experimental cohort combined (n= 34).
In addition, assessment of treatment fidelity with randomly selected treatment and comparison cohorts included whether each task and learning objective outlined in the manual was completed by the facilitator for the given session, and the extent to which recommended interpersonal and group facilitation skills were utilized (i.e. related skills to participants’ life, flexibility in responding, reading out loud and explaining all handouts). This measure of treatment integrity was adapted from Lane et al.(2004).
Results
Of 12 planned cohorts, we were able to complete 8 (3 experimental cohorts and 5 comparison cohorts). Due to the trainers’ schedules, the final order deviated from the planned randomization in that the eighth cohort was a comparison cohort rather than an experimental cohort. In total, 88 men were enrolled in MBRP training (experimental), and 101 men in the comparison condition. Table 1 shows the characteristics of the study sample at baseline. Fifty- eight percent of the sample were African American men; the average age was 35 years, and most had had 5 or more previous arrests. At baseline, 35% of the sample met criteria for probable PTSD on the PTSD Symptom Scale, in line with the findings of Ruzich et al. (2014). Using independent samples t-tests for continuous variable s and chi-square comparisons for categorical variables at the significance level of p=0.05, there were no statistically significant differences, in demographic or psychosocial characteristics between the treatment and comparison groups at baseline, suggesting that our randomized cohort method was successful in creating equivalent groups.
Table 1.
Characteristics of Participants at Baseline
| Total N= 189 |
Mindfulness Treatment N=88 |
Comparison Treatment N=101 |
|
|---|---|---|---|
| African American, % | 58.9 | 51.9 | 64.6 |
| Hispanic/Latino, % | 18.6 | 19.2 | 18.1 |
| Previously arrested more than 5 times, % | 56.1 | 58.3 | 54.2 |
| Age, mean (standard deviation) | 35.8 (11.3) | 35.9 (11.4) | 35.7 (11.2) |
| High school diploma or higher, % | 58.5 | 57.1 | 59.6 |
| Never participated in yoga or meditation, % | 75.0 | 81.0 | 70.2 |
| Met criteria for PTSD, % | 35.8 | 46.4 | 27.4 |
Table 2 displays correlations between the psychosocial measures of anxiety, drug craving, and PTSD at baseline. These measures were significantly positively correlated with one another and negatively correlated with mindfulness, as measured by the FFMQ and FMI.
Table 2.
Correlations between Psychological Characteristics and Mindfulness at Baseline (n=189)
| Anxiety | PTSD | Drug Craving | Mindfulness (FFMQ) |
|
|---|---|---|---|---|
| Anxiety | 1 | |||
| PTSD | .486** | 1 | ||
| Drug Craving | .391** | .353** | 1 | |
| Mindfulness (FFMQ) | −.373** | −.483** | −.261** | 1 |
| Mindfulness (Freiburg) | −.156* | −.249** | −.210** | .495** |
Note:
= p<.05
= p<.01
FFMQ – Five Facets Mindfulness Inventory; PTSD – Post-traumatic stress disorder
Fifty-four (54) MBRP participants and 72 communication skill participants completed both baseline and follow-up measures for an overall follow-up rate of 69%. Independent t-tests were used to assess differential attrition among those who did not complete the intervention (n=65) vs. those who did (n=124). The analyses revealed that their baseline psychosocial characteristics were not statistically different. Tables 3a and 3b show changes in psychological measures among MBRP and comparison group participants, respectively, who completed both the pre- and post-test assessments. In both study arms, PTSD and craving scores declined while mindfulness scores on the Freiburg scale, though not the FFMQ, increased.
Table 3a.
Changes in Psychosocial Outcomes for Mindfulness Treatment Group (n=54)
| Measure | Mean (S.D.) T1 | Mean (S.D) T2 | df | T-Score | P-Value | Effect Size (d) |
|---|---|---|---|---|---|---|
| Anxiety | 32.2 (9.2) | 29.3 (8.0) | 53 | 2.30 | .03 | 0.32 |
| PTSD | 44.1 (15.1) | 34.5 (10.4) | 53 | 4.90 | .00 | 0.67 |
| Drug Craving | 11.0 (6.4) | 8.0 (3.2) | 53 | 3.78 | .00 | 0.52 |
| Mindfulness (FFMQ) | 78.1 (9.7) | 81.1 (11.0) | 53 | −2.07 | .04 | −0.28 |
| Mindfulness (Freiburg) | 36.0 (8.1) | 40.2 (6.3) | 53 | −3.88 | .00 | −0.53 |
Table 3b.
Changes in Psychosocial Outcomes for Comparison Group (n=71)
| Measure | Mean (S.D.) T1 | Mean (S.D) T2 | df | T-Score | P-Value | Effect Size (d) |
|---|---|---|---|---|---|---|
| Anxiety | 29.6 (9.4) | 28.0 (8.1) | 70 | 1.51 | .14 | 0.18 |
| PTSD | 38.9 (12.2) | 33.2 (11.1) | 70 | 4.01 | .00 | 0.48 |
| Drug Craving | 11.9 (6.7) | 8.9 (4.2) | 70 | 4.00 | .00 | 0.47 |
| Mindfulness (FFMQ) | 79.2 (9.1) | 81.3 (10.5) | 70 | −1.93 | .06 | −0.23 |
| Mindfulness (Freiburg) | 34.5 (7.4) | 37.3 (6.6) | 70 | −3.44 | .00 | −0.41 |
Due to attrition between the pre and post tests, the expectation-maximization (EM) method was used to create maximum likelihood estimates and model psychological outcomes (Table 4). The analysis revealed that after controlling for the Freiburg mindfulness pre-test, there was a small but significant improvement (at p < 0.05) in the Freiburg mindfulness score among participants in the mindful meditation condition compared to the communication skills condition.
Table 4:
Hierarchical Regression Analysis Predicting Psychological Outcome Change Scores from Baseline Measures and Condition Type
| Step | Predictor Variable | F (df) for Equation | Δ R2 | b | SE | β | ta |
|---|---|---|---|---|---|---|---|
| Analysis predicting anxiety change scores from the pre-scores and treatment conditions | |||||||
| 1 | Anxiety Pre-Score | 160.00 (1, 199) | .45 | −.57 | .05 | −.67 | −12.65** |
| 2 | Treatment vs. Control | 79.68 (2, 198) | .45 | −.23 | .79 | −.02 | −.29 |
| Analysis predicting PTSD change scores from the pre-scores and treatment conditions | |||||||
| 1 | PTSD Pre-Score | 273.11 (1, 199) | .58 | −.65 | .04 | −.76 | −16.53** |
| 2 | Treatment vs. Control | 135.97 (2, 198) | .58 | .33 | 1.11 | .01 | .30 |
| Analysis predicting Drug Craving change scores from the pre-scores and treatment conditions | |||||||
| 1 | Drug Craving Pre-Score | 540.12 (1, 199) | .73 | −.77 | .03 | −.86 | −23.24** |
| 2 | Treatment vs. Control | 270.71 (2, 198) | .73 | .41 | .40 | .04 | 1.04 |
| Analysis predicting mindfulness (FFMQ) change scores from the pre-scores and treatment conditions | |||||||
| 1 | Mindfulness (FFMQ) Pre-Score | 37.85 (1, 199) | .40 | −.33 | .05 | −.40 | −6.15** |
| 2 | Treatment vs. Control | 18.94 (2, 198) | .40 | −.47 | 1.06 | −.03 | −.44 |
| Analysis predicting mindfulness (Freiburg) change scores from the pre-scores and treatment conditions | |||||||
| 1 | Mindfulness (Freiberg) Pre-Score | 146.51 (1, 199) | .42 | −.52 | .04 | −.65 | −12.10** |
| 2 | Treatment vs. Control | 76.47 (2, 198) | .44 | −1.34 | 0.66 | −.11 | −2.03* |
Note: The first block is an analysis of the pre-score psychological outcome change score. The second block is an analysis of the condition type on the psychological outcome change score controlling for the pre-score.
p < .05
p < .01
While the statistical significance of this finding should be qualified in view of multiple comparisons made within these data, it suggests that the Freiberg measure may have been more responsive than the more commonly used FFMQ with this population. There were no significant differences between study arms in improvements in the other psychological outcomes, although the decline in anxiety and PTSD was greater in the experimental condition than the control condition.
Discussion
A six week mindfulness intervention is feasible in a jail setting, and results suggest that it may reduce symptoms of drug craving and PTSD, and result in a small but significant increase in mindfulness as measured by the Freiberg inventory. The current study is the first to our knowledge to involve a culturally competent mindfulness trainer from the same background as many of the participants. This study is also the first to compare MBRP in a jail setting to a manualized attention control condition of equivalent frequency and roughly comparable session length, rather than treatment as usual.
A novel cohort randomization process was used to assign participants to conditions. While this design may be subject to history effects, it permits a more robust comparison than treatment as usual, and is more feasible for a jail setting than randomization by participant. We were unable to adhere completely to the initial randomization plan; however, there were no significant differences on measured variables between the two treatment arms at baseline.
Since mindfulness interventions outside of jail settings have been shown to be efficacious in reducing PTSD symptoms, we may speculate as to why our intervention did not significantly outperform the communications skills condition on this measure. It may be that one session per week for six weeks is inadequate to convey mindfulness concepts and establish a mindfulness practice among participants. It is also likely that participants in both conditions were improving in their PTSD, anxiety, and craving symptoms due to their participation in the jail treatment or positive interactions with the research staff and peers, effects that may have outweighed between-group differences.
Several limitations of the study should be noted. First, we were unable to follow participants in the community to assess substance use after release from jail. To explore the effect of the intervention on recidivism after release from incarceration and with the consent of participants, we plan to compare de-identified arrest information prospectively on the participants enrolled in the experimental vs. comparison arms. This analysis will be ongoing in the future. Second, despite the fact that most participants had a court order to complete a treatment program, our follow up rate of 69% was low, primarily because participants were released or transferred. Third, since both the treatment and comparison interventions took place in a therapeutic jail community, we are unable to distinguish the effects of MBRP from the beneficial effects of other treatment received by participants.
In conclusion, MBRP is a promising intervention as an adjunct to jail substance use disorder treatment. MBRP may be especially beneficial in jail, because it is a very stressful environment and because participants are likely to have abstained from alcohol and drug use for a period of time. More research is needed on mindfulness interventions adapted for disadvantaged populations such as those in jails and prisons.
Acknowledgments:
The authors are grateful to Michelle Champagne and Yirser Ra Hotep for outstanding group facilitation and research assistance. We thank our Advisory Board, especially Sarah Bowen, James Carmody, and Arthur Lurigo for their insights during study design and implementation; all errors and omissions are those of the authors. We also thank the WestCare Foundation for facilitating access to their program. Research reported in this publication was supported in its entirety by a $1.9 million grant to Chicago State University from the National Institute on Drug Abuse of the National Institute of Health, under grant award R24DA03640. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Circuit Court of Cook County.
Footnotes
“In cases in which those studies require the assignment of prisoners…to control groups which may not benefit from the research, the study may proceed only after the Secretary has consulted with appropriate experts, including experts in penology, medicine, and ethics, and published notice, in the FEDERAL REGISTER, of the intent to approve such research.” 46 Code of Federal Regulations 45, section 110(e)(iv).
References
- Amaro H (2014). Implementing Mindfulness-Based Relapse Prevention in diverse populations: Challenges and future directions. Substance Use and Misuse 49:612–616. [DOI] [PubMed] [Google Scholar]
- Amaro H, Spear S, Vallejo Z, Conron K, Black D (2014) Feasibility, acceptability, and preliminary outcomes of a mindfulness-based relapse prevention intervention for culturally-diverse, low-income women in substance use disorder treatment. Substance Use and Misuse. 49(5). 547–559. [DOI] [PubMed] [Google Scholar]
- Auty KM, Cope A, & Liebling A (2017). A systematic review and meta-analysis of yoga and mindfulness meditation in prison: Effects on psychological well-being and behavioural functioning. Journal of Offender Therapy and Comparative Criminology 61: 689–710. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, & Steer RA (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology 56: 893–897. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34, 8, 669–73. [DOI] [PubMed] [Google Scholar]
- Bohlmeijer E, Klooster PM, Fledderus M, Veehof M, & Baer R (2011). Psychometric properties of the Five Facet Mindfulness Questionnaire in depressed adults and development of a short form. Assessment, 18(3):308–320. [DOI] [PubMed] [Google Scholar]
- Bowen S, Chawla N, & Marlatt GA (2011). Mindfulness-based relapse prevention for addictive behaviors: A clinician’s guide. New York, NY: Guilford Press. [Google Scholar]
- Bowen S, Witkiewitz K, Dillworth TM, Chawla N, Simpson TL, Ostafin BD, …Marlatt GA (2006). Mindfulness meditation and substance use in an incarcerated population. Psychology of Addictive Behaviors 20(3):343–7. [DOI] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Collins S, Witkiewitz K, Hsu S, Grow J, Clifasefi S, …& Marlatt A (2009). Mindfulness-Based Relapse Prevention for substance use disorders: A pilot efficacy trial. Substance Abuse, 30, 205–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, . . . Larimer ME (2014). Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. JAMA Psychiatry, 71, 547–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 4, 385–396. [PubMed] [Google Scholar]
- Demarzo M, Montero-Marin J, Puebla-Guedea M, Navarro-Gil M, Herrera-Mercadal P, Moreno-Gonzalez S, Calvo-Carrion S, Bafaluy-Franch L, Garcia-Campayo J (2017) Efficacy of 8- and 4-session mindfulness-based interventions in a non-clinical population: A controlled study. Frontiers in Psychology 8(8),13–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettner SL, Huang D, Evans E, Ash DR, Hardy M,…Hser YI, (2006) Benefit-cost in the California Treatment Outcome Project: Does substance abuse treatment “pay for itself”? Health Service Research, 41,192–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flannery BA, Volpicelli JR, & Pettinati HM (1999). Psychometric properties of the Penn Alcohol Craving Scale. Alcoholism: Clinical and Experimental Research, 23, 1289–1295. [PubMed] [Google Scholar]
- Glasner S, Mooney LJ, Ang A, Garneau HC, Hartwell E, Brecht M, & Rawson RA (2017). Mindfulness-based relapse prevention for stimulant dependent adults: A pilot randomized clinical trial. Mindfulness, 8 (1), 126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman RD & Calderon AM (2012) The use of mindfulness in trauma counseling. Journal of Mental Health Counseling, 34, 254–268. [Google Scholar]
- Grossman P (2008). On measuring mindfulness in psychosomatic and psychological research. Journal of Psychosomatic Research, 64(4), 405–408. [DOI] [PubMed] [Google Scholar]
- Grant S, Colaiaco B, Motala A, Shanman R, Booth M, Sorbero M, Hempel S (2017) Mindfulness-based Relapse Prevention for substance use disorders: A systematic review and meta-analysis. Journal of Addiction Medicine, 11, 386–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joe GW, Knight K, Simpson DD, Flynn PM, Morey JT, Bartholomew NG,…O’Connell AM (2012). An evaluation of six brief interventions that target drug-related problems in correctional populations. Journal of Offender Rehabilitation, 51(1–2):9–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J (1982) An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry 4, 33–47. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Finney JW, &Moos R (2005). Substance use disorder patients who are mandated to treatment: Characteristics, treatment process, and 1- and 5-year outcomes. Journal of Substance Abuse Treatment, 28, 213–223. [DOI] [PubMed] [Google Scholar]
- Lane KL, Bocian KM, MacMillan DL, & Gresham FM (2004). Treatment integrity: An essential--but often forgotten--component of school-based interventions. Preventing School Failure, 48, 36–43. [Google Scholar]
- Lee KH, Bowen S, & Bai AF (2011). Psychosocial outcomes of mindfulness-based relapse prevention in incarcerated substance abusers in Taiwan: A preliminary study. Journal of Substance Use, 16, 476–483. [Google Scholar]
- Malouf ET, Youman K, Stuewig J, Witt EA, & Tangney JP (2017). A pilot RCT of a values-based mindfulness group intervention with jail inmates: Evidence for reduction in post-release risk behavior. Mindfulness, 8(3), 603–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center on Addiction and Substance Abuse (2010). Behind bars II: Substance abuse and America’s prison population. New York, NY: National Center on Addiction and Substance Abuse at Columbia University. [Google Scholar]
- Perelman AM, Miller SL, Clements CB, Rodriguez A, Allen K, & Cavanaugh R (2012). Meditation in a deep South prison: A longitudinal study of the effects of Vipassana. Journal of Offender Rehabilitation, 51,176–198. [Google Scholar]
- Ruzich D, Reichert J, & Lurigio AJ (2014). Probable posttraumatic stress disorder in a sample of urban jail detainees. International Journal of Law and Psychiatry, 37, 455–463. [DOI] [PubMed] [Google Scholar]
- Simpson TL, Kaysen D, Bowen S, MacPherson LM, Chawla N, Blume A, … Larimer M (2007). PTSD symptoms, substance use, and Vipassana meditation among incarcerated individuals. Journal of Traumatic Stress, 20, 239–249. [DOI] [PubMed] [Google Scholar]
- Subramanian R, Delaney R, Roberts S, Fishman N, & McGarry P (2015). Incarceration’s front door: The misuse of jails in America. Vera Institute of Justice. Available at https://www.vera.org/publications/incarcerations-front-door-the-misuse-of-jails-in-america [Google Scholar]
- Vaillant GE (1995). The natural history of alcoholism revisited. Cambridge, MA: Harvard University Press. [Google Scholar]
- Vujanovic AA, Niles B, Pietrefesa A, Schmertz SK, & Potter CM (2011) Mindfulness in the treatment of posttraumatic stress disorder among military veterans. Professional Psychology: Research and Practice, 42, 24–31. [Google Scholar]
- Walach H, Buchheld N, Buttenmüller V, Kleinknecht N, & Schmidt S (2006). Measuring mindfulness: the Freiburg Mindfulness Inventory (FMI). Personality and Individual Differences, 40, 1543–1555. [Google Scholar]
- Witkiewitz K, Brenna L, & Bowen S (2013). Mindfulness-based relapse prevention with racial and ethnic minority women. Addictive Behavior, 38, 2821–2824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Warner K, Sully B, Barricks A, Stauffer C, Thompson B & Luoma J (2014). Randomized trial comparing mindfulness-based relapse prevention with relapse prevention for women offenders at a residential addiction treatment center. Substance Use and Misuse, 49, 536–546. [DOI] [PubMed] [Google Scholar]