Abstract
Background
Plicae around the knee are anatomically normal structures that are remnants of embryonic membranes and are generally asymptomatic. Synovial plica syndrome is known to cause knee symptoms; however, its pathological contribution has been rarely reported. This study aimed to investigate the clinical significance of suprapatellar plicae as well as the morphological characteristics of suprapatellar plicae in patients with knee symptoms who required arthroscopic treatment.
Methods
Of 223 arthroscopic knee surgeries, 125 patients undergoing primary arthroscopy for various diseases were eligible for inclusion in this study. All affected knees were preoperatively examined by two skilled physicians in a routine manner. Each patient was diagnosed with one primary disease entity based on clinical examinations and arthroscopic findings. At least two skilled orthopedic physicians watched the surgical videos together and defined the type of plicae based on the Dandy classification (Dandy DJ. 1990) as follows: (A) absent, (B) the plica was up to one-quarter of the width of the suprapatellar pouch, (C) the plica was between one-quarter and one-third of the width of the suprapatellar pouch, (D) the plica was between one-third and two-thirds of the width of the suprapatellar pouch, (E) the plica was more than two-thirds of the width of the suprapatellar pouch, (F) the plica had a complete membrane, (G) the plica was perforated, (H) arch, (I) pillar, or (J) lateral. Suprapatellar plica syndrome was considered when (1) the patient complained of anterior knee pain and had localized tenderness above the suprapatellar pouch, (2) magnetic resonance imaging revealed suprapatellar plica structures, and (3) other suspicious pathologies accounting for knee symptoms were excluded. We investigated primary disease type, type of plica, and the relationships between them.
Results
The results revealed that meniscus injuries and anterior cruciate ligament injuries caused the majority of primary diseases (approximately 80%). Regarding plica forms, 23 knees were classified as having absent (type A) plicae, 14 knees as having a complete septum (type F), and 88 knees were classified as “other.” There were no significant relationships between disease type and the morphological characteristics of the plicae (chi-squared test, p = 0.35). Suprapatellar pain was observed in five cases, of which two patients were diagnosed with intra-articular free body, one patient with synovitis combined osteoarthritis, and two patients with suprapatellar plica syndrome with a complete septum. The latter two cases experienced knee symptom resolution soon after arthroscopic resection of the plica.
Conclusions
Although the results did not show any relationship between forms of plica remnants and primary disease type, all patients diagnosed with suprapatellar plica syndrome showed complete septum type suprapatellar plicae. A large population study is required in the future.
Keywords: Arthroscopy, Knee, Patellofemoral pain syndrome, Suprapatellar plica
Introduction
Plicae around the knee are anatomically normal structures that are remnants of embryonic membranes and are generally asymptomatic. However, synovial plica syndrome is known to cause knee symptoms, particularly anterior knee pain,1,2 with a prevalence ranging from 3% to 30%.3 Synovial knee plicae have recently been classified into four types according to their location: suprapatellar, infrapatellar, medial, and lateral.3,4 Of these, the medial or “shelf” plica has the pathological potential to be associated with knee symptom.5, 6, 7 However, the pathological contribution of suprapatellar plicae to knee symptoms has seldom been reported, and suprapatellar plica syndrome appears to be overlooked or misdiagnosed occasionally.2,7 Although several authors have described the clinical relationship between suprapatellar plicae and knee symptoms in cases in which the plica forms a complete septum,8,9 the pathophysiology of suprapatellar plica syndrome has not been clearly understood. Moreover, the morphologic association of this type of plica with knee symptoms remains unclear.
Dandy investigated medial suprapatellar plicae in 500 knees from 474 subjects during arthroscopy and classified them into 10 categories based on morphology.10 Later, Zidorn also examined suprapatellar plicae by direct observation in 210 knees from 149 adult cadavers and classified them into four groups.11 Each study described the plica as having a complete septum, an incomplete septum, or no septum, with rates of 4%, 87%, and 9% in the Dandy classification and 16%, 73%, and 11% in the Zidorn classification, respectively. Although plicae are normally asymptomatic regardless of their shape, they are thought to have the pathological potential to cause knee symptoms associated with mechanical irritation, such as impingement.12,13 Notably, however, few studies have addressed suprapatellar plicae among Japanese populations. Hence, this retrospective study aimed to investigate the morphological characteristics of suprapatellar plicae in patients with knee symptoms who required arthroscopic intervention and to determine the clinical significance of suprapatellar plicae among Japanese subjects. We also present two cases of patients from among the study subjects who were diagnosed with suprapatellar plica syndrome.
Materials and methods
Ethics and study subjects
This study was performed under approval from the ethical committee of our institute. We retrospectively investigated patients with knee symptoms who required arthroscopic procedures for treatment between December 2015 and November 2016.
Patients were eligible for inclusion if they (1) were more than 6 years old, (2) agreed to receive knee arthroscopy under general or spinal anesthesia, and (3) were undergoing knee arthroscopy for the first time. Patients were excluded if they (1) had a history of patellar fracture or intra-articular fracture; (2) had an inflammatory autoimmune disease, such as rheumatoid arthritis; or (3) were undergoing “second-look” arthroscopy. Overall, 223 arthroscopic knee surgeries were performed during the study period, and 125 cases were enrolled in this study.
Patients aged 18 years and older and parents of subjects below 18 years old were fully informed of the content of this study. Patients were told that their personal information would be kept confidential.
Physiological examination
All affected knees were examined by two skilled physicians (M.A and M.D.) in a routine manner. Subjects were instructed to lie down on the bed in the supine position and to have both legs relaxed. Then, the examiner sought points of tenderness around the patellofemoral joint to identify the source of pain on the affected knee. Tenderness was regarded as positive when the subject felt pain from the examiner pushing a thumb against the knee using pressure that did not normally evoke pain sensation. Patients with localized tenderness above the suprapatellar pouch were suspected of suprapatellar plica syndrome when no other possible pathologies were identified. The examiner checked the patient's range of motion and performed other disease-specific tests, such as the McMurray test, anterior/posterior drawer test, pivot shift test, and varus/valgus stress test; patellar glide test and apprehension test were performed to assess patella instability.14
Diagnosis of suprapatellar plica syndrome
We diagnosed the primary disease of each case based on preoperative clinical examinations and arthroscopic findings. Therefore, each patient was diagnosed with only one disease entity.
Because of the mechanical nature of plicae, symptoms are believed to occur when the degree of plica irritation increases. Thus, it was essential to collect certain histories from the patients. After obtaining a sufficient history, an interim diagnosis of suprapatellar plica syndrome was determined when the following criteria were fulfilled: (1) the patient complained of anterior knee pain and localized tenderness above the suprapatellar pouch; (2) magnetic resonance imaging (MRI) revealed the structure of a suprapatellar plica as a band of low-intensity signals in the suprapatellar pouch,12,15 and (3) other suspicious pathologies that could account for the knee symptoms were excluded.
Surgical procedures
All arthroscopic procedures were performed under either general or spinal anesthesia and were recorded for later review. Patients lay down in the supine position, the operator squeezed venous blood away from the affected leg's distal foot to the thigh using an elastic bandage, and a tourniquet was then applied at the mid-level of the thigh and inflated to a pressure of 100–120 mmHg over systolic blood pressure. Following standard procedures, routine arthroscopy was performed through a medial and lateral infrapatellar port. After observing all compartments of the knee joint with a surgical telescope, the features of suprapatellar plica were examined at the suprapatellar pouch. When suprapatellar plica was diagnosed as the cause of the knee symptoms, the plica was subtotally removed, leaving a thin edge. The arthroscopic procedure was finished when no other treatable pathologies remained.
Finally, we diagnosed suprapatellar plica syndrome when removal of the plica succeeded in ameliorating knee symptoms in patients who were diagnosed with plica syndrome before arthroscopy and who recovered from knee symptoms after surgery.
Plica classification
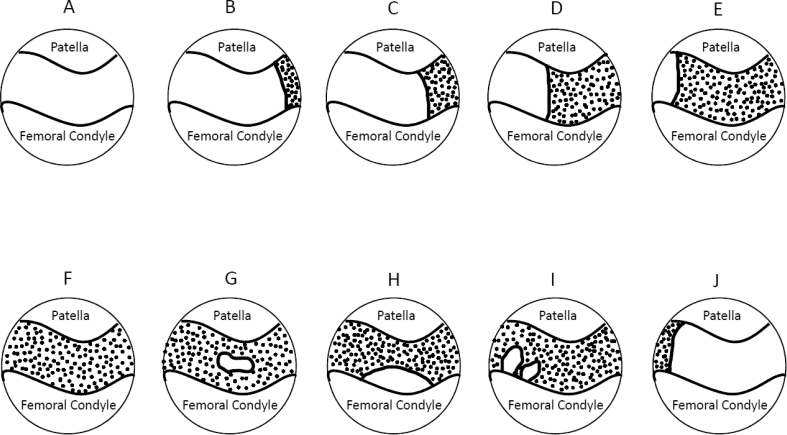
After the arthroscopic procedure, at least two skilled orthopedic physicians who attended arthroscopic treatment watched the surgical videos for every knee and identified the type of plica in accordance with the Dandy classification, as follows10: (A) absent, (B) the plica was up to one-quarter of the width of the suprapatellar pouch, (C) the plica was between one-quarter and one-third of the width of the suprapatellar pouch, (D) the plica was between one-third and two-thirds of the width of the suprapatellar pouch, (E) the plica was more than two-thirds of the width of the suprapatellar pouch, (F) the plica had a complete membrane, (G) the plica was perforated, (H) arch, (I) pillar, or (J) lateral (Fig. 1).
Fig. 1.
Morphological patterns of suprapatellar plicae (from type A to type J) in the arthroscopic view: adapted from Dandy et al..10
The relationships between the morphology of the suprapatellar plicae and diagnosed primary diseases or patients experiencing suprapatellar pain were analyzed with the chi-squared test using BellCurve for Excel (Social Survey Research Information Co., Ltd). Significance was set at p < 0.05.
Results
Demographics
In this study, there were 71 male subjects aged 8–81 (mean, 36.0) years and 54 female subjects aged 9–74 (mean, 34.4) years.
Relationship between disease type and plicae
Table 1 shows the relationships between primary diagnoses of the subjects and plicae. Meniscus injuries and anterior cruciate ligament injuries caused the majority of knee symptoms (approximately 80%). Although suprapatellar pain was identified in five patients of all subjects, two patients were diagnosed with intra-articular free body and one patient with synovitis combined osteoarthritis. We suspected two cases of suprapatellar plica syndrome in this case series before arthroscopic intervention. Table 1 also shows the Dandy classification of each case of suprapatellar plica. In terms of morphology based on this classification, 18.4% of knees were classified as type A, 21.6% as type B, 8.8% as type C, 1.6% as type D, 3.2% as type E, 10.4% as type F, 12.0% as type G, 22.4% as type H, 0.8% as type I, and 0.8% as type J. No significant relationships were found between primary disease type and the morphological characteristics of the plicae (p = 0.35, Cramer's V = 0.27). In five cases with suprapatellar pain, we classified them into one type A, one type E, and three type F, of which one case with type A was diagnosed with synovitis combined with osteoarthritis, one case with type E and one case with type F were diagnosed with intra-articular free body, and two cases with type F whose pain cause was unidentified were diagnosed with suprapatellar plica syndrome. In other words, all patients diagnosed with suprapatellar plica syndrome showed complete septum type suprapatellar plicae. These two patients experienced knee symptom resolution soon after arthroscopic resection of the plica.
Case 1
A 13-year-old girl without a significant trauma history was referred to our hospital for complaints of left knee pain after a physical education class. She did not belong to any sport clubs, and her physical activity level was not high. Before visiting our clinic, she had been conservatively treated with topical analgesics, and general physical therapies included stretching, mobilization, and muscle strengthening training over 3 months; however, her knee pain had not improved with those treatments.
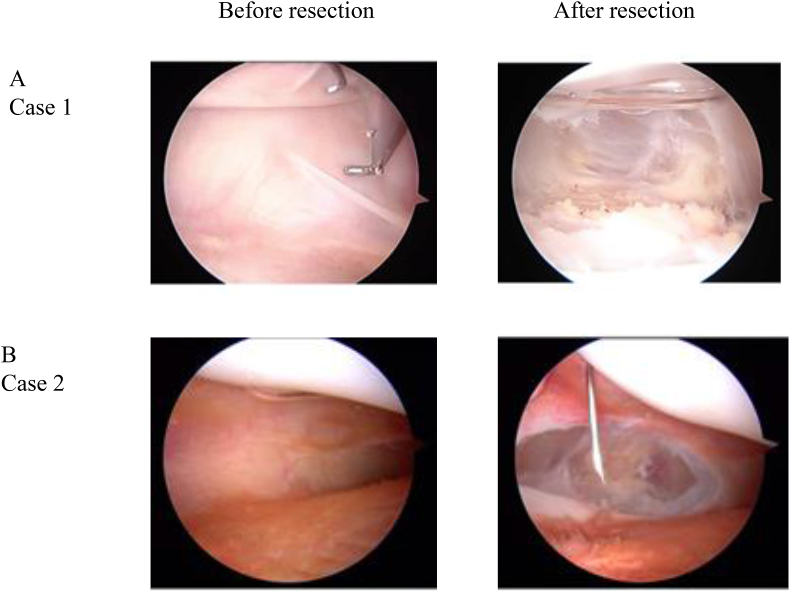
On physical examination, the affected knee was mildly swollen, and the patient had a tender point at the upper edge of the patella. The range of motion of the affected knee was 0° at extension but was limited to 90° at flexion due to pain. Specific tests did not indicate other pathological causes of the knee symptoms. Sagittal MRI showed a structure of low-intensity signal between the patella and the femoral condyle in the suprapatellar pouch (Fig. 2). We suspected suprapatellar plica syndrome in this case, and an arthroscopic intervention was performed. Arthroscopy revealed a complete septum of a suprapatellar plica in the suprapatellar pouch (Fig. 3A). After resecting the complete septum of the plica, the patient's knee symptoms soon resolved. She gradually started doing sport activities from 1 month after surgery and could return to normal sport activity by at least 2 months after surgery. At her 6-month final follow-up, she did not report any knee symptom.
Case 2
A 13-year-old boy was referred to our hospital for complaints of left knee pain after falling that had not resolved after more than 3 months of conservative treatment mainly by physical therapy, including stretching, mobilization, and muscle strengthening training. He did not belong to any sport clubs; thus, his physical activity level was not very high.
On physical examination, the affected knee was mildly swollen, and the patient had tender points at the upper edge of the patella and the lateral joint space between the femur and tibia. The range of motion of the affected knee was 0° at extension but was limited to 90° at flexion. The McMurray test was negative. MRI revealed a structure that suggested the presence of a suprapatellar plica, and other possible pathologies were not identified. Thus, we suspected suprapatellar plica syndrome in this case, and arthroscopic intervention was performed. Arthroscopy revealed a complete septum of a suprapatellar plica in the suprapatellar pouch (Fig. 3B). After resecting the complete septum of the plica, the patient's knee symptoms soon disappeared. He started sport activities from 2 weeks after surgery and could return to normal sport activity by at least 1 month after surgery. He completely recovered from his preoperative symptoms at the 6-month final follow-up.
Table 1.
Morphological characteristics of suprapatellar plica based on Dandy classification.
| Primary disease | Number (%) | Number of case with suprapatellar pain | Number of case in each classification category |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | |||
| Meniscus injury | 58 (46.4%) | 9 | 14 | 6 | 2 | 2 | 4 | 5 | 15 | 1 | ||
| Anterior crucial ligament injury | 39 (31.2%) | 9 | 8 | 3 | 4 | 7 | 7 | 1 | ||||
| Osteoarthritis | 13 (10.4%) | 1 | 3 | 2 | 2 | 2 | 4 | |||||
| Patellar instability | 4 (3.2%) | 2 | 1 | 2 | 1 | |||||||
| Osteochondritis dissecans | 2 (1.6%) | 1 | 1 | |||||||||
| Patella partita | 2 (1.6%) | 1 | 1 | |||||||||
| Intra-articular tumor | 2 (1.6%) | 1 | 1 | |||||||||
| Intra-articular free body | 2 (1.6%) | 1 | 1 | |||||||||
| Posterior crucial ligament injury | 1 (0.8%) | 1 | ||||||||||
| Suprapatellar plica syndrome | 2 (1.6%) | 2 | 2 | |||||||||
| Total | 125 | 5 | 23 | 26 | 11 | 2 | 4 | 14 | 15 | 28 | 1 | 1 |
Fig. 2.
Preoperative T2-weighted magnetic resonance image in the sagittal view. The arrow indicates the structure of the suprapatellar plica.
Fig. 3.
Arthroscopic view before and after resection of the suprapatellar plica.
Discussion
To our knowledge, this is the first report to classify suprapatellar plicae in Japanese subjects who underwent arthroscopic treatment. Of five cases with suprapatellar pain, two patients were found to have suprapatellar plica syndrome, and their symptoms were relieved soon after arthroscopic resection of the plicae. Although the results did not show any relationship between forms of plica remnants and primary disease type, all patients diagnosed with suprapatellar plica syndrome showed complete septum type suprapatellar plicae.
Suprapatellar plicae, or bursa, are also referred to as “superior plicas,“16 “septum-like folds,“17 or “suprapatellar septa.“11 These terms describe the structure that is located at the border between the suprapatellar bursa and the knee joint cavity and can be differentiated from the medial patellar plica or “shelf.“10,18 The knee joint is believed to have formed in the eighth week of fetal life with three compartments: the medial and lateral tibiofemoral compartments and the suprapatellar bursa.5,19 Then, the synovial septa are partially resorbed over the next several weeks, and a single joint cavity is created. However, if the resorption process fails, remnants of the unabsorbed membrane are recognized as synovial plicae after birth.5 Several authors have reported in previous studies that suprapatellar plicae remain in some form at rates of approximately 91%,10 89%,11 or 89%,20 consistent with the results in this study (85.7%). These findings suggest that plica remnants remain at a similar incidence among different races.
Although suprapatellar plicae are found frequently in the knee joint with variable shapes, symptomatic suprapatellar plicae are rarely found. Dupont reported only three cases of symptomatic suprapatellar plicae from among 12,000 arthroscopies.4 The pathophysiology of symptomatic plicae remains unclear. Bae et al. reported 34 cases in 23 patients of symptomatic complete-type suprapatellar plicae. In 30 of those cases, the authors succeeded in improving knee symptoms in 90% of cases after arthroscopic plica resection.8 Kim et al. reported a case of a symptomatic arch-type plica in which knee symptoms resolved after arthroscopic excision.21 Regardless of its shape, previous reports have suggested that biomechanical irritation, such as from blunt trauma and increased activity, caused knee symptoms by driving a pathological plica reaction.1, 2, 3, 4 When cases are limited to those among Japanese populations, several articles have reported the clinical significance of suprapatellar plicae. Adachi et al. reported the case of a professional baseball pitcher who presented with chronic anterior knee pain experienced while pitching who had a complete septum of a suprapatellar plica. However, the authors concluded that the knee pain occurred due to cartilage damage rather than to the existence of the plica.9 Some authors have also reported relationships between knee symptoms and a complete septum of a suprapatellar plica in Japanese patients with knee pain.22 Moreover, in this study, we found that two patients who were considered to have suprapatellar plica syndrome before arthroscopy had a complete septum of a plica, and their symptoms resolved soon after arthroscopic resection. These findings suggest that pathological changes in the suprapatellar plicae are more likely to occur in Japanese individuals when there is a complete septum rather than with other types of plicae.
Since it is widely recognized that suprapatellar plicae are normal structures in the knee joint and that the pathophysiology of symptomatic plicae remains unclear, the pathological potential of suprapatellar plicae appears to have been poorly described among physicians. This study revealed that approximately 11% of individuals who were treated with arthroscopy had a complete septum of a suprapatellar plica, suggesting a potential relationship between knee symptoms and suprapatellar plicae. Thus, it is important for orthopedic physicians to consider suprapatellar plica syndrome when treating patients with knee symptoms.
The important point for diagnosing suprapatellar plica syndrome is to suspect this disease initially by knowing its clinical signs. Although this disease should be suspected in patients at any age, it is less common among children below 10 years old.3 Dull knee pain is a common symptom, and the pain is often aggravated during stair climbing.2,8 On physical examination, patients have tenderness over the upper edge of the patella. MRI examination is useful for detecting structures of a suprapatellar septum as a band of low-intensity signals in the suprapatellar pouch in the sagittal view and for identifying other pathologies.12 Differential diagnoses include tendinitis, medial patellar plica or “shelf,” meniscus injury, cartilage injury, and osteochondritic lesions.3,5
In terms of treatment for suprapatellar plica syndrome, conservative treatment, such as rest, physiotherapy, and anti-inflammatory topical agents, is initially recommended. Patellar bracing and stretches are thought to be useful for improving pathological conditions of plicae; however, if they fail, arthroscopy should be considered to determine the potential pathology and for fundamental treatment, as in the two cases we described here.
There are several limitations in the current study. First, a sample bias and the retrospective study design should be considered when interpreting the results because this study was performed in a single tertiary hospital. Multicenter and prospective studies are preferred for understanding the true distribution of plicae by this classification in a large population. Second, this study included only patients who required arthroscopic intervention. Third, although we were successful in alleviating knee symptoms of patients after plica resection, histopathological examinations were not performed; thus, we could not completely exclude other patellofemoral pain syndromes such as suprapatellar tendinitis and prepatellar bursitis. A future study involving a large population is required to shed light on these limitations.
Conclusion
We retrospectively investigated the shapes of suprapatellar plicae in patients with knee symptoms who required arthroscopic intervention and the clinical significance of suprapatellar plicae among Japanese subjects. Although the results did not show any relationship between forms of plica remnants and primary disease type, all patients diagnosed with suprapatellar plica syndrome showed complete septum type suprapatellar plicae.
Conflicting interests
The Authors have no conflict of interest relevant to this article.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.asmart.2019.03.001.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Patel D. Plica as a cause of anterior knee pain. Orthop Clin N Am. 1986;17(2):273–277. [PubMed] [Google Scholar]
- 2.Abrahams S., Kern J.H. Anterior knee pain: plica syndrome, the forgotten pathology? Physiotherapy. 2001;87(10):523–528. [Google Scholar]
- 3.Lee P.Y.F., Nixion A., Chandratreya A., Murray J.M. Synovial plica syndrome of the knee: a commonly overlooked cause of anterior knee pain. Surg J. 2017;3(1):e9–e16. doi: 10.1055/s-0037-1598047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dupont J.Y. Synovial plicae of the knee. Controversies and review. Clin Sports Med. 1997 Jan;16(1):87–122. doi: 10.1016/s0278-5919(05)70009-0. [DOI] [PubMed] [Google Scholar]
- 5.Schindler O.S. The sneaky plica' revisited: morphology, pathophysiology and treatment of synovial plicae of the knee. Knee Surg Sports Traumatol Arthrosc. 2014;22(2):247–262. doi: 10.1007/s00167-013-2368-4. [DOI] [PubMed] [Google Scholar]
- 6.Liu D.S., Zhuang Z.W., Lyu S.R. Relationship between medial plica and medial femoral condyle--a three-dimensional dynamic finite element model. Clin Biomech. 2013;28(9-10):1000–1005. doi: 10.1016/j.clinbiomech.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Al-Hadithy N., Gikas P., Mahapatra A.M., Dowd G. Review article: plica syndrome of the knee. J Orthop Surg. 2011;19(3):354–358. doi: 10.1177/230949901101900319. [DOI] [PubMed] [Google Scholar]
- 8.Bae D.K., Nam G.U., Sun S.D., Kim Y.H. The clinical significance of the complete type of suprapatellar membrane. Arthroscopy. 1998;14(8):830–835. doi: 10.1016/s0749-8063(98)70019-2. [DOI] [PubMed] [Google Scholar]
- 9.Adachi N., Ochi M., Uchio Y., Kawasaki K., Yamasaki K. The complete type of suprapatellar plica in a professional baseball pitcher: consideration of a cause of anterior knee pain. Arthroscopy. 2004;20(9):987–991. doi: 10.1016/j.arthro.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 10.Dandy D.J. Anatomy of the medial suprapatellar plica and medial synovial shelf. Arthroscopy. 1990;6(2):79–85. doi: 10.1016/0749-8063(90)90002-u. [DOI] [PubMed] [Google Scholar]
- 11.Zidron T. Classification of the suprapatellar septum considering ontogenetic development. Arthroscopy. 1992;8:459–464. doi: 10.1016/0749-8063(92)90008-y. [DOI] [PubMed] [Google Scholar]
- 12.Vassiou K., Vlychou M., Zibis A., Nikolopoulou A., Fezoulidis I., Arvanitis D. Synovial plicae of the knee joint: the role of advanced MRI. Postgrad Med. 2015;91(1071):35–40. doi: 10.1136/postgradmedj-2013-132176. [DOI] [PubMed] [Google Scholar]
- 13.Guney A., Bilal O., Oner M., Halici M., Turk Y., Tuncel M. Short- and mid-term results of plica excision in patients with mediopatellar plica and associated cartilage degeneration. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1526–1531. doi: 10.1007/s00167-010-1125-1. [DOI] [PubMed] [Google Scholar]
- 14.Rossi R., Dettoni F., Bruzzone M., Cottino U., D'Elicio D.G., Bonasia D.E. Clinical examination of the knee: know your tools for diagnosis of knee injuries. Sports Med Arthrosc Rehabil Ther Technol. 2011;28(3):25. doi: 10.1186/1758-2555-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.García-Valtuille R., Abascal F., Cerezal L. Anatomy and MR imaging appearances of synovial plicae of the knee. Radiographics. 2002;22(4):775–784. doi: 10.1148/radiographics.22.4.g02jl03775. [DOI] [PubMed] [Google Scholar]
- 16.Jouanin T., DuPont J.Y., Halimi P., Lassau J.P. The synovial folds of the knee joint: anatomical study. Anat Clin. 1982;1(4):47–53. [Google Scholar]
- 17.Henche H.R., Holder J. Springer; Berlin: 1987. Die Arthroskopie des Kniegelenkes; pp. 58–59. [Google Scholar]
- 18.Ieda Y., Kotani A., Ishii Y. Bilateral plica synovialis mediopatellaris syndrome: a case report. J Orthop Sci. 2003;8(2):218–221. doi: 10.1007/s007760300036. [DOI] [PubMed] [Google Scholar]
- 19.Ogata S., Uhthoff H.K. The development of synovial plicae in human knee joints: an embryologic study. Arthroscopy. 1990;6(4):315–321. doi: 10.1016/0749-8063(90)90063-j. [DOI] [PubMed] [Google Scholar]
- 20.Harty M.I., Joyce J.J. Synovial folds in the knee joint. Orthop Rev. 1977;7:91–92. [Google Scholar]
- 21.Kim S.J., Shin S.J., Koo T.Y. Arch type pathologic suprapatellar plica. Arthroscopy. 2001;17(5):536–538. doi: 10.1053/jars.2001.21845. [DOI] [PubMed] [Google Scholar]
- 22.Fukutoku Y., Tashiro Y., Sakamoto A., Matsuda S., Okazaki K., Iwamoto Y. Suprapatellar synovial plica with complete type of septum – a report of three cases. Orthop Traumatol. 2012;61:623–626. (In Japanese) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.