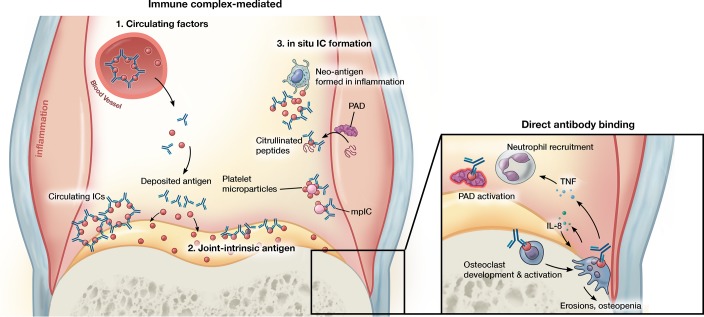
Figure 2. Antibody-mediated mechanisms of inflammatory arthritis.
Joint inflammation mediated by antibodies can proceed via distinct and not mutually exclusive pathways. ICs formed in circulation can precipitate in joint tissue and trigger enhanced vascular permeability that enables entry of pathogenic antibodies into the joint. ICs/antibody clusters can form within the joint through binding to joint-intrinsic antigens such as collagen, blood-borne antigen deposited on cartilage, or antigens formed de novo in the inflamed milieu such as citrullinated peptides and platelet microparticles, the latter generating microparticle-associated immune complexes (mpICs). Independent of IC formation, antibodies can mediate pathology via binding to specific targets. For example, antibodies promote citrullination by altering the activation threshold of PADs and stimulate the development or activation of osteoclasts. In addition to promotion of bone erosions and local osteopenia, osteoclasts may promote further osteoclastogenesis and contribute to neutrophil recruitment via IL-8 and other mediators. Illustrated by Mao Miyamoto.