Abstract
Background
Lower grip strength on admission to hospital is known to be associated with longer stay, but the link between customary grip and risk of future admission is less clear.
Objective
To compare grip strength with subsequent risk of hospital admission among community-dwelling older people in a UK setting.
Design
Cohort study with linked administrative data.
Setting
Hertfordshire, England.
Subjects
2997 community-dwelling men and women aged 59-73 years at baseline.
Methods
Hertfordshire Cohort Study (HCS) participants completed a baseline assessment between 1998 and 2004, during which grip strength was measured. Hospital Episode Statistics and mortality data to March 2010 were linked with the HCS database. Statistical models were used to investigate the association of grip strength with subsequent elective, emergency and long-stay hospitalisation and readmission.
Results
There was a statistically significant negative association between grip strength and all classes of admission in women, (unadjusted hazard ratio per standard deviation decrease in grip strength for: any admission/death 1.10[95%CI:1.06,1.14]; elective admission/death 1.09[95%CI:1.05,1.13]; emergency admission/death 1.21[95%CI:1.13,1.31]; long-stay admission/death 1.22[95%CI:1.13,1.32]; and unadjusted relative risk per standard deviation decrease in grip strength for 30-day readmission/death 1.30[95%CI:1.19,1.43]). These associations remained significant after adjustment for potential confounding factors (age, height, weight-for-height, smoking, alcohol, social class). In men, unadjusted rates for emergency admission/death, long stay admission/death and readmission/death were significantly associated with grip strength; associations that similarly withstood adjustment.
Conclusion
This study provides the first evidence that grip strength among community-dwelling men and women in the UK is associated with risk of hospital admission over the following decade.
Keywords: hospital admission, readmission, Hospital Episode Statistics, hospitalisation, grip strength
Introduction
Grip strength is a powerful predictor of disability, morbidity and mortality [1]. When measured at or near the point of admission to hospital, it is known to predict admission outcome. Those with weaker grip spend longer in hospital [2-8], are less likely to be discharged home [2] and more likely to be readmitted [7]. However, grip strength is known to be affected by malnutrition and disease [7], thus muscular weakness at admission might be a specific effect of the presenting condition. Alternatively, if weakness is a more general state one might hypothesise, in keeping with a lifecourse approach [9,10], that grip strength measured earlier, in a wider population, might distinguish those who will go on to be admitted from those who will not: that grip strength might predict admission itself. A small number of studies have addressed this issue with mixed results [11-15]. The question is important though, since effective early intervention could have the potential to prevent admission.
Using baseline data from the Hertfordshire Cohort Study (HCS) linked to Hospital Episode Statistics (HES) accrued by participants over the following decade, we have investigated the association between grip strength and subsequent hospital admissions of any sort. Sub-categories of elective, emergency, and long-stay (over seven-day) admissions were examined, as were readmissions within 30 days of discharge. As defined, these outcomes approximate an increasing burden to the NHS by cost, complexity and unpredictability [16].
Methods
The Hertfordshire Cohort Study [17] comprises a group of men and women born in the English county of Hertfordshire between 1931 and 1939 whose birth, infancy and early childhood were documented by Health Visitors. Between the end of 1998 and 2004, 1579 men and 1418 women who still lived there provided information about their lifestyle during a home interview and subsequently attended clinics for detailed physiological investigations including anthropometry and measurement of grip strength. The cohort is flagged on the NHS Central Register for continuous notification of death.
Administrative data relating to secondary care in England are routinely collected in the form of Hospital Episode Statistics. In the inpatient data, a hospital episode is a period of care under one consultant, several of which may be recorded during the period between admission and discharge. With written consent from the cohort members, an extract of HES data covering the period 01/04/1998 to 31/03/2010 was obtained for linkage with HCS. It comprised 15 variables for each episode experienced by a member of the cohort, including start and end dates, and method of admission. Episode data were combined to describe complete admissions, then records relating to the same individual were brought together to create a personal admissions history alongside details of death where appropriate. Admissions that occurred before the baseline clinic were excluded from the analysis; thus histories comprised information on all hospital admissions between the date of attendance at HCS baseline clinic and 31/03/10. Methods have been described elsewhere [18].
Statistical methods
The statistical software used was Stata, release 13 [19].
Outcome variables
Different types of admission were coded from each person’s admissions history. We used the stset command to define time to: elective admission; emergency admission; admission exceeding seven days (‘long-stay’) or admission of any type. A further binary variable was created indicating whether or not a participant was ever readmitted within 30 days of discharge. Death was considered as an alternative failure event in all instances.
Exposure variable
Maximum muscle strength was characterised by the best of six grip measurements taken in clinic using a Jamar hand-grip dynamometer.
Confounding variables
These were chosen from the available data based on our a priori understanding of causal pathways to hospital admission and included age, smoking history, alcohol consumption, anthropometry and social class. Height and weight were highly correlated (r=0.44, p<0.001 for men; r=0.32, p<0.001 for women); to avoid multi-collinearity, a sex-specific standardised residual of weight-adjusted-for-height was calculated for inclusion with height in regression models. Registrar General’s social class was coded from the 1990 OPCS Standard Occupational Classification [20] unit group for occupation using computer assisted standard occupational coding [21], according to own current or most recent full-time occupation for men and never-married women, or to husband’s occupation for ever-married women [22].
Data were considered as missing at random and no imputation was carried out for HCS baseline characteristics. Hospital outcome data were ascertained with negligible loss to follow-up which is a major strength of linking a detailed cohort study with routinely collected hospital admissions data.
Data were described using means and standard deviations (SD), medians and inter-quartile ranges (IQR) and frequency and percentage distributions. Associations between grip strength and time to elective admission/death, time to emergency admission/death, time to long-stay admission/death and time to any admission/death were analysed using the Prentice, Williams and Peterson Total Time model. This model allows the association between grip strength and the risk of these outcomes to be examined whilst taking into account admissions that occur after an individual’s first [23]. Participants were not considered at risk of admission during any spell in hospital. The association between grip strength and the variable indicating whether or not a participant had experienced at least one 30-day readmission or died was analysed using log-binomial regression; a suitable technique for estimation of relative risks when the outcome variable is not rare [24]. The assumption of proportional hazards for the PWP-TT model was checked by graphically plotting the scaled Schoenfeld residuals against the logarithm of the survival time; the lack of trend in the residuals implied that the proportionality assumption was satisfied.
All analyses were carried out for men and women separately without adjustment and then after adjustment for the following potential confounding variables: age, height, weight-for-height, alcohol consumption, whether the participant had ever smoked and current social class.
Results
Table 1 shows the characteristics of the study population. Average age of men was 65.7 and women 66.6 years at baseline. Mean grip strength was greater among men (44.0kg) than women (26.5kg). Table 1 also shows the proportions of men and women who experienced admissions of different types during a median 8.1 years’ follow-up.
Table 1. Participant characteristics.
| n(%) | Men (n=1579) | Women (n=1418) |
|---|---|---|
| Age (yrs)+ | 65.7 (2.9) | 66.6 (2.7) |
| Height (cm)+ | 174.2 (6.5) | 160.8 (5.9) |
| Weight (kg)+ | 82.4 (12.7) | 71.4 (13.4) |
| BMI (kg/m2)+ | 27.2 (3.8) | 27.6 (4.9) |
| Ever smoked regularly | 1059 (67.1) | 553 (39) |
| Alcohol consumption: Non-drinker | 89 (5.6) | 283 (20.0) |
| Very low (<1M, <1F) | 178 (11.3) | 360 (25.4) |
| Low (1-10M, 1-7F) | 636 (40.3) | 553 (39.0) |
| Moderate (11-21M, 8-14F) | 335 (21.2) | 154 (10.9) |
| Fairly high (22-35M, 15-21F) | 177 (11.2) | 43 (3.0) |
| High (>35M, >21F) | 163 (10.3) | 25 (1.8) |
| Social class (Manual) | 908 (59.3) | 827 (58.4) |
| Grip strength (kg)+ | 44.0 (7.5) | 26.5 (5.8) |
| Number of systems medicated* | 1.0 (0.0, 2.0) | 1.0 (1.0, 2.0) |
| Ever any admission | 1185 (75.0) | 976 (68.8) |
| Ever any admission / died | 1197 (75.8) | 985 (69.5) |
| Ever elective admission | 1051 (66.6) | 882 (62.2) |
| Ever elective admission/died | 1105 (70.0) | 910 (64.2) |
| Ever emergency admission | 608 (38.5) | 433 (30.5) |
| Ever emergency admission/died | 638 (40.4) | 450 (31.7) |
| Ever long stay (>7 day) admission | 429 (27.2) | 316 (22.3) |
| Ever long stay (>7 day) admission/died | 486 (30.8) | 340 (24.0) |
| Ever readmission (<30 days) | 371 (23.5) | 244 (17.2) |
| Ever readmission (<30 days) / died | 458 (29.0) | 288 (20.3) |
| Deaths | 189 (12.0) | 86 (6.1) |
Mean(SD)
Median (Lower quartile, Upper quartile)
SD: standard deviation
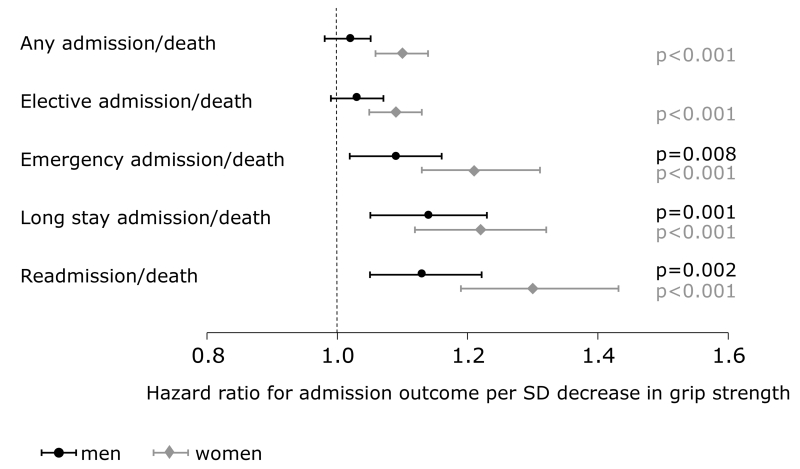
Among those who were admitted at least once, the median number of admissions was 3 (IQR 1-6) in men and 2 (IQR 1-5) in women. Median time to 1st admission was 2.6 years (IQR 1.1-4.9), with a median total of 7 days spent in hospital (IQR 2-19). Table 2 and Figure 1 show the association between grip strength and hospital admission, by type. Among women, lower grip strength was strongly associated with increased risk of all types of admission/death considered in this analysis; any admission/death (unadjusted hazard ratio (HR) per SD decrease in grip strength: 1.10 [95%CI: 1.06, 1.14]), elective admission/death (HR: 1.09 [95%CI: 1.05, 1.13]) emergency admission/death (HR: 1.21 [95%CI: 1.13, 1.31]) long-stay admission/death (HR: 1.22 [95%CI: 1.13, 1.32]) and 30-day readmission/death (relative risk (RR): 1.30 [95%CI: 1.19, 1.43]) the associations being robust to adjustment as outlined above.
Table 2. Associations between grip strength and risk of admission outcomes among Hertfordshire Cohort Study participants.
| Association between grip strength and the risk of each outcome* | Men | Women | |||
|---|---|---|---|---|---|
| Hazard ratio (95% CI) | P-value | Hazard ratio (95% CI) | P-value | ||
| Any admission/death* | Unadj | 1.02 (0.98,1.06) | 0.332 | 1.10 (1.06,1.14) | <0.001 |
| Adj | 1.02 (0.98,1.06) | 0.328 | 1.10 (1.06,1.14) | <0.001 | |
| Any elective admission/death* | Unadj | 1.03 (0.99,1.07) | 0.155 | 1.09 (1.05,1.13) | <0.001 |
| Adj | 1.03 (0.99,1.08) | 0.122 | 1.09 (1.05,1.14) | <0.001 | |
| Any emergency admission/death* | Unadj | 1.09 (1.02,1.16) | 0.008 | 1.21 (1.13,1.31) | <0.001 |
| Adj | 1.08 (1.01,1.15) | 0.031 | 1.21 (1.12,1.30) | <0.001 | |
| Any admission lasting longer than 7 days/death* | Unadj | 1.14 (1.05,1.23) | 0.001 | 1.22 (1.13,1.32) | <0.001 |
| Adj | 1.14 (1.04,1.24) | 0.005 | 1.20 (1.10,1.30) | <0.001 | |
| Readmission within 30 days/death** | Unadj | 1.13 (1.05,1.22) | 0.002 | 1.30 (1.19,1.43) | <0.001 |
| Adj | 1.15 (1.05,1.25) | 0.002 | 1.30 (1.19,1.43) | <0.001 | |
Estimates of association are hazard ratios (95% CI) from PWP-TT models, corresponding to the risk of each type of hospital admission per SD decrease in grip strength.
Estimates of association are relative risks (95% CI) from log-binomial regression models, corresponding to the risk of each type of hospital admission per SD decrease in grip strength.
Unadj and Adj indicate whether or not models were adjusted for potential confounding variables. Adjusted models accounted for age, height, weight for height residual, smoking status, alcohol consumption and social class
Figure 1. Effect of grip strength on risk of admission outcomes per SD decrease in grip strength in men and women (unadjusted).
Among men, lower grip strength was associated with increased risk of emergency admission/death (unadjusted HR per SD decrease in grip strength: 1.09 [95%CI: 1.02, 1.16]), long-stay admission/death (HR: 1.14 [95%CI: 1.05, 1.23]) and 30-day readmission/death (RR: 1.13 [95%CI: 1.05, 1.22]). Again, the associations were robust to adjustment. There was no association between grip strength and risk of overall, or elective, admission/death.
Discussion
This study provides the first evidence that grip strength among community-dwelling men and women in the UK is associated with risk of hospital admission over the following decade. Among women, lower grip strength is strongly associated with increased risk of all types of admission/death considered in this analysis. Among men, an association is seen with emergency admissions, those that last more than seven days and those that follow within 30 days of a previous discharge.
There is limited previous work with which to compare our results. Grip strength measured at or shortly after admission has been found to be associated with length of hospital stay among older people in a number of settings [2-4,6,8], with destination on discharge [2] and with readmission within 6 months [7]. However, none of these studies measured grip strength before admission. Measurement on admission has two shortcomings: first, it is too late to forestall admission; and secondly, measured strength may differ from habitual strength if grip has been impaired as a result of the presenting condition.
A few studies have been carried out among older people in mainland Europe [11-13] and the US [14,15] to investigate the prospective association between customary grip strength and admission, with varying results. In Belgium [11], among 560 men and women aged 80+, significantly higher rates of hospital admission were observed among those in the weakest tertile of grip strength over nearly 3 years’ follow-up. Conversely, a sample of 279 patients in Germany [12], followed-up for 18 months, found no association between grip strength and risk of hospital admission. Neither did a study of 764 men and women aged 75+ in The Netherlands [13] amongst whom individuals with complex problems were over-represented. Although this study found no association between grip strength and hospitalisation in the year following measurement, it did show an association with self-reported hospitalisation in the year preceding measurement, suggesting an effect of ill-health on grip.
The largest study to date to have considered grip strength among its predictors and hospital admission among its outcomes is the Health Aging and Body Composition Study in the US [14]. Comprehensive baseline (1997-8) measurements of muscle strength, mass and density were made in 3011 men and women aged 70-80 years. The cohort was followed for a mean of 4.7 years during which hospital admissions were self-reported. As in the Belgian study [11], participants with the weakest grip had a significantly increased risk of hospitalisation. Another US study, of 758 participants of the Cardiovascular Health Study who had been diagnosed with heart failure, compared grip strength shortly after diagnosis with hospitalisation over a mean follow-up of 3.4 years, by the end of which 75% of participants had died. Andersen and Gill models showed that weak grip (defined as a binary variable) was associated with hospitalisation; this relationship was unchanged in composite analyses considering hospital admission/death as the endpoint.
The results of these previous studies cannot be generalised internationally because thresholds for admission may differ between healthcare systems. Our study, set in the UK, is equal in size to the biggest previous study [14], has a longer period of follow-up than any other and is free from bias attributable to mortality. This latter point is important in interpreting the results of earlier studies, which differed in their ascertainment of hospitalisation. Those relying on self-report [13,14] were inevitably biased towards individuals who did not die, which may have affected the reported associations between grip strength and hospitalisation.
Moreover, ours is the first study to show a graded relationship by category among admission outcomes that approximate an increasing burden to the NHS by cost, complexity and unpredictability [16]. It is also the first to identify a gender differential in the effect of grip on hospitalisation, previous studies having controlled for sex rather than conducting separate analyses. More marked associations between lower grip strength and increased risk of subsequent hospital admission in women than men could reflect a genuine gender difference as a result of a threshold effect (mean grip strength at baseline was 44kg in men and 26.5kg in women). Alternatively, the difference may be an artefact of a greater survival bias among men if the weakest men from the wider population, who might have been expected to experience a greater burden of morbidity, were under-represented in the cohort.
Our study had some limitations. First, the assumptions underlying survival models required us to treat hospitalisation and death as alternative failure events because they share similar risk factors. However, the contribution of death to each outcome was small. For example, 1185 men ever had an admission of any sort; adding deaths increased this figure to 1197. The variable representing 30-day readmission was the least frequently occurring outcome we studied: 371 men fell into this group alone; the addition of deaths increased the figure to 458. Thus around 1% of men in the any admission/death analysis, and 19% in the readmission/death analysis experienced the outcome solely as a result of their death. The corresponding figures for women were 1% and 15%. Treating deaths in this way did not, therefore, detract greatly from modelling the risk of hospital admission. An alternative approach would have been to use a competing risks survival model, but this is difficult to implement in a multiple-failure setting.
Secondly, doubts have been expressed over the validity of Hospital Episode Statistics [25]. However, case ascertainment through HES has been compared with that of a number of disease-specific registries [26-28] and in general, HES has been found to be the more complete. Finally, we were unable to investigate admissions ending in discharge to residential care because there were too few such cases among the Hertfordshire participants: 99% of HCS admissions ended in discharge to usual residence or death.
Conversely, our study had diverse strengths. It was conducted prospectively and had a median interval of 2.6 years from measurement of customary grip strength to first admission. Linkage with HES data provided almost attrition-proof follow-up for the whole cohort; bias resulting from loss to follow-up is therefore unlikely.
We studied inpatient admissions of all types (including day cases, diagnostic investigations and minor surgical procedures as well as longer and more complex admissions) and found a remarkably clear signal that within these data grip is associated, over a comparatively long lag-time, with admissions of all types in women and with emergency and long-stay admissions and 30-day readmissions in men.
The advantages of the Hertfordshire Cohort Study have been described elsewhere [17]. In brief, it is a high quality database containing measurements carried out to a strict protocol by trained fieldworkers. It is maintained by an experienced multidisciplinary team with meticulous levels of data entry, record keeping and statistical analysis. The recently added HES data have been scrutinised and cleaned to the same standards [18].
Finally, we conducted a thorough review of the most appropriate statistical analysis techniques for the rich HCS/HES multiple failure dataset. After comparison of a number of modelling techniques (Time-to-first event Cox modelling; Andersen and Gill and Prentice, Williams and Peterson Total Time (PWP-TT) multiple failure models) which differed in their ability to include repeated hospitalisations and account for an individual’s previous number of admissions when assessing their risk of admission, the PWP-TT model was chosen for this analysis. In general, the models under consideration agreed as to the rank of the estimates of risk produced, the significance of the supporting p-values and the effect of statistical adjustment, but differed somewhat in the magnitude of their estimates: those from the PWP-TT model were typically more conservative than those from other models.
Conclusion
This study provides the first evidence that grip strength among community-dwelling men and women in the UK is associated with risk of hospital admission over the following decade.
References
- 1.Bohannon RW. Hand-grip dynamometry predicts future outcomes in aging adults. J Geriatric Phys Ther. 2008;31:3–10. doi: 10.1519/00139143-200831010-00002. 2001. [DOI] [PubMed] [Google Scholar]
- 2.Kerr A, Syddall HE, Cooper C, Turner GF, Briggs RS, Aihie Sayer A. Does admission grip strength predict length of stay in hospitalised older patients? Age Ageing. 2006;35:82–4. doi: 10.1093/ageing/afj010. [DOI] [PubMed] [Google Scholar]
- 3.Roberts HC, Syddall HE, Cooper C, Sayer AA. Is grip strength associated with length of stay in hospitalised older patients admitted for rehabilitation? Findings from the Southampton grip strength study. Age Ageing. 2012;41:641–6. doi: 10.1093/ageing/afs089. [DOI] [PubMed] [Google Scholar]
- 4.Keevil V, Mazzuin Razali R, Chin AV, Jameson K, Aihie Sayer A, Roberts HC. Grip strength in a cohort of older medical inpatients in Malaysia: a pilot study to describe the range, determinants and association with length of hospital stay. Arch Gerontol Geriatr. 2013;56:155–9. doi: 10.1016/j.archger.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Mendes J, Azevedo A, Amaral TF. Handgrip strength at admission and time to discharge in medical and surgical inpatients. JPEN J Parenter Enteral Nutr. 2014;38:481–8. doi: 10.1177/0148607113486007. [DOI] [PubMed] [Google Scholar]
- 6.Sultan P, Hamilton MA, Ackland GL. Preoperative muscle weakness as defined by handgrip strength and postoperative outcomes: a systematic review. BMC Anesthesiol. 2012 doi: 10.1186/1471-2253-12-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gariballa S, Alessa A. Sarcopenia: Prevalence and prognostic significance in hospitalized patients. Clin Nutr. 2013;32:772–6. doi: 10.1016/j.clnu.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Shyam Kumar AJ, Beresford-Cleary N, Kumar P, Barai A, Vasukutty N, Yasin S, et al. Preoperative grip strength measurement and duration of hospital stay in patients undergoing total hip and knee arthroplasty. Eur J Orthop Surg Traumatol. 2013;23:553–6. doi: 10.1007/s00590-012-1029-5. [DOI] [PubMed] [Google Scholar]
- 9.Kuh D, Ben-Shlomo Y, Lynch J, Power C. Lifecourse epidemiology. J Epidemiol Community Health. 2003;57:778–83. doi: 10.1136/jech.57.10.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stein C, Moritz I. A life course perspective of maintaining independence in older age. WHO; Geneva: 1999. Report No: WHO/HSC/AHE/99.2. [Google Scholar]
- 11.Legrand D, Vaes B, Mathei C, Adriaensen W, Van Pottelbergh G, Degryse J-M. Muscle strength and physical performance as predictors of mortality, hospitalization, and disability in the oldest old. J Am Geriatr Soc. 2014;62:1030–8. doi: 10.1111/jgs.12840. [DOI] [PubMed] [Google Scholar]
- 12.Nikolaus T, Bach M, Oster P, Schlierf G. Prospective value of self-report and performance-based tests of functional status for 18-month outcomes in elderly patients. Aging Clin Exp Res. 1996;8:271–6. doi: 10.1007/BF03339578. [DOI] [PubMed] [Google Scholar]
- 13.Chan OYA, van Houwelingen AH, Gussekloo J, Blom J, den Elzen WPJ. Comparison of quadriceps strength and handgrip strength in their association with health outcomes in older adults in primary care. Age. 2014;36:9714. doi: 10.1007/s11357-014-9714-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cawthon PM, Fox KM, Gandra SR, Delmonico MJ, Chiou C-F, Anthony MS, et al. Do muscle mass, muscle density, strength, and physical function smilarly influence risk of hospitalization in older adults? J Am Geriatr Soc. 2009;57:1411–9. doi: 10.1111/j.1532-5415.2009.02366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chaudhry SI, McAvay G, Chen S, Whitson H, Newman AB, Krumholz HM, et al. Risk factors for hospital admission among older persons with newly diagnosed heart failure Findings from the Cardiovascular Health Study. J Am Coll Cardiol. 2013;61:635–42. doi: 10.1016/j.jacc.2012.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Department of Health Reference Costs 2011-12. https://www.gov.uk/government/publications/nhs-reference-costs-financial-year-2011-to-2012.
- 17.Syddall HE, Aihie Sayer A, Dennison EM, Martin HJ, Barker DJ, Cooper C. Cohort profile: the Hertfordshire Cohort Study. Int J Epidemiol. 2005;34:1234–42. doi: 10.1093/ije/dyi127. [DOI] [PubMed] [Google Scholar]
- 18.Simmonds SJ, Syddall HE, Walsh B, Evandrou M, Dennison EM, Cooper C, et al. Understanding NHS hospital admissions in England: linkage of Hospital Episode Statistics to the Hertfordshire Cohort Study. Age Ageing. 2014;43:653–60. doi: 10.1093/ageing/afu020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.StataCorp. Stata Statistical Software: Release 13. StataCorp LP; College Station, TX: 2013. [Google Scholar]
- 20.Office of Population Censuses and Surveys . Standard Occupational Classification, Vol 1 Structure and definition of major, minor and unit groups. HMSO; London: 1990. [Google Scholar]
- 21.Elias P, Halstead K, Prandy K. Computer Assisted Standard Occupational Coding. H.M. Stationery Office; 1993. [Google Scholar]
- 22.Arber S, Ginn J. Gender and inequalities in health in later life. Social Sci Med. 1993;36:33–46. doi: 10.1016/0277-9536(93)90303-l. [DOI] [PubMed] [Google Scholar]
- 23.Castaneda J, Gerritse B. Appraisal of several methods to model time to multiple events per subject: Modelling time to hospitalizations and death. Revista Colombiana De Estadistica. 2010;33:43–61. [Google Scholar]
- 24.Barros A, Hirakata V. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brennan L, Watson M, Klaber R, Charles T. The importance of knowing context of hospital episode statistics when reconfiguring the NHS. BMJ. 2012;344:2432. doi: 10.1136/bmj.e2432. [DOI] [PubMed] [Google Scholar]
- 26.Barrow P, Waller P, Wise L. Comparison of hospital episodes with “drug-induced” disorders and spontaneously reported adverse drug reactions. Br J Clin Pharmacol. 2006;61:233–7. doi: 10.1111/j.1365-2125.2005.02554.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gill M, Goldacre MJ, Yeates DG. Changes in safety on England’s roads: analysis of hospital statistics. BMJ. 2006;333:73–5. doi: 10.1136/bmj.38883.593831.4F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moller H, Richards S, Hanchett N, Riaz S, Luechtenborg M, Holmberg L, et al. Completeness of case ascertainment and survival time error in English cancer registries: impact on 1-year survival estimates. Br J Cancer. 2011;105:170–6. doi: 10.1038/bjc.2011.168. [DOI] [PMC free article] [PubMed] [Google Scholar]