Overview
Introduction
The modified Stoppa approach is an intrapelvic, extraperitoneal approach that allows less invasive anatomic reduction and fixation of displaced acetabular fractures of the anterior column, with or without involvement of the quadrilateral plate, and the midterm results have been promising, particularly in elderly patients.
Indications & Contraindications
Step 1: Preoperative Planning and Case Presentation
Assess the acetabular fracture pattern and plan the steps for reduction and methods of fixation.
Step 2: Patient Positioning, Setup, and Skin Incision
Place the patient in the supine position and ensure that a Foley catheter is placed in the bladder and the ipsilateral leg is prepared and draped freely, facilitating reduction maneuvers. After sterile preparation and draping, make a 10-cm horizontal skin incision 2 fingerbreadths superior to the pubic symphysis.
Step 3: Superficial and Deep Dissection
Develop the anterior rectus sheath, split the sheath at the midline, incise the transversalis fascia, and approach the retropubic space.
Step 4: Exposure of the Superior Pubic Ramus and Pelvic Brim with Control of the Neurovascular Structures
Elevate the rectus abdominis muscle insertion at the pubic rami and incise the iliopectineal fascia from the pubic symphysis to the iliopectineal eminence.
Step 5: Extension for Visualization of the Pelvic Crest and the Anterior Wall
To control fractures exiting the iliac crest (e.g., high anterior column fractures,) open the first window of the ilioinguinal approach.
Step 6: Fracture Reduction and Fixation
Reduce the fracture with soft-tissue or skeletal traction, Schanz screws used with the so-called joystick technique, a collinear clamp, and/or a ball-spike pusher; disimpact the acetabular dome, if necessary, and use suprapectineal and infrapectineal reconstruction plates for fixation, if necessary.
Step 7: Wound Closure
Check the urine output for hematuria, suture the anterior lamina of the rectus sheath, and perform a layered closure.
Step 8: Postoperative Care
Postoperatively, instruct the patient to use toe-touch weight-bearing for the first 3 months.
Results
Anatomic reduction was achieved in 72% of our 59 patients2 who were 13 to 89 years old and in 52% to 82% of patients, with a mean age from 38 to 64 years, who were described in other studies12,17,18,21-23,26,27.
Pitfalls & Challenges
Abstract
Background:
The modified Stoppa approach is performed for safe and efficient management of acetabular fractures involving the anterior column. This approach avoids dissection of the inguinal canal, the femoral nerve, and the external iliac vessels as seen in the “second window” of the ilioinguinal approach and has thus been shown to be less invasive than the ilioinguinal approach1. As an intrapelvic approach, it facilitates the management of medial displacement fracture patterns involving the quadrilateral plate and dome impaction that typically occur in the elderly2,3. The reduced morbidity of this approach is of particular relevance for elderly patients who must respond to the stresses of injury and surgery with diminished physiological reserves.
Description:
The specific surgical steps include preoperative planning, patient positioning and setup, a Pfannenstiel incision, superficial and deep dissection, development of the Retzius space and retraction of the bladder, exposure of the superior pubic ramus and iliopectineal eminence, dissection and ligation of a potential corona mortis, exposure of the obturator nerve and vessels, subperiosteal preparation of the pubic ramus with retraction of the external iliac vessels, subperiosteal exposure of the quadrilateral plate with detachment of the internal obturator muscle and exposure of the posterior column, assessment of residual displacement by fluoroscopic views, longitudinal soft-tissue or lateral skeletal traction (optional) for reduction of medial displacement of the femoral head, disimpaction of the acetabular dome fragment and grafting of the supra-acetabular void (optional) under fluoroscopic and arthroscopic (optional) control, and reduction and fixation of extra-articular components (iliac wing posteriorly and pubic ramus anteriorly), the posterior column (infra-acetabular screw), and the quadrilateral plate (buttress plate). Before wound closure, the urine output is checked for occurrence of hematuria, an indication of bladder penetration. The anterior lamina of the rectus sheath is then sutured, and a layered closure performed.
Alternatives:
The ilioinguinal approach might be used instead.
Rationale:
The modified Stoppa approach avoids dissection within the inguinal canal, the second window of the ilioinguinal approach. Therefore, this approach is less invasive and might be an alternative for joint-preserving surgery, especially in the elderly.
Introductory Statement
The modified Stoppa approach is an intrapelvic, extraperitoneal approach that allows less invasive anatomic reduction and fixation of displaced acetabular fractures of the anterior column, with or without involvement of the quadrilateral plate, and the midterm results have been promising, particularly in elderly patients.
Indications & Contraindications
Indications
Elementary and associated displaced acetabular fractures involving predominantly the anterior column (anterior column, anterior wall, anterior column posterior hemitransverse, anteriorly open transverse fractures, or both-column fractures [limited]).
Incongruency of the hip joint.
Involvement of the weight-bearing dome.
Impaction of the weight-bearing dome.
Comminution of the articular surface.
Unstable hip joint.
Associated proximal femoral injuries (femoral neck or trochanteric fractures).
Associated nonorthopaedic injuries (nerve deficits and/or bowel or bladder injuries).
Contraindications
Posterior wall fracture.
Posterior column fracture.
Associated posterior column and posterior wall fractures.
Transverse fracture with displacement predominantly in the posterior column or associated posterior wall fracture.
T-shaped fracture with displacement predominantly in the posterior column or associated posterior wall fracture.
Nonambulatory patient.
Local infection.
Substantial comorbidities.
Step-by-Step Description of Procedure
Step 1: Preoperative Planning and Case Presentation
Assess the acetabular fracture pattern and plan the steps for reduction and methods of fixation.
For preoperative planning, review all radiographs (Fig. 1, Video 1) and perform additional computed tomography (CT) (Fig. 2), which offers important preoperative information4-6.
Determine the acetabular fracture pattern according to Judet et al.7. Assess for the main direction of displacement and for medial displacement. Assess for involvement of the quadrilateral plate, for dome impaction, and for displaced iliac wing or low anterior column fractures2,3,7.
The modified Stoppa approach facilitates the management of fractures of the anterior column such as the so-called anterior column posterior hemitransverse, very low anterior column, and low anterior column fractures. As an extension to the modified Stoppa approach, the first window of the ilioinguinal approach by a separate incision to the modified Stoppa approach might become necessary for the management of so-called high anterior column fractures as well as in fractures involving the posterior column (T-type, transverse, or associated both-column fracture, with the main dislocation in the anterior column)7,8. As an extension of the first window of the ilioinguinal approach, an osteotomy of the anterior superior iliac spine might become necessary for management of anterior wall fractures. Video 2 demonstrates the extension in an anatomic specimen, as additional exposure was not needed in the present clinical case.
Exclude patients who have substantial comorbidities or major complicating factors—such as comminution, abrasion, femoral head fracture, or delayed surgery—from open reduction and internal fixation9,10.
Plan the steps of the reduction (e.g., lateral traction using either soft-tissue or skeletal traction with the use of a Schanz screw or a traction table, disimpaction of the acetabular roof, or extension of the modified Stoppa approach) and the methods for stabilization (e.g., infrapectineal buttress plating, infra-acetabular screws, or locking plates)2,11-16.
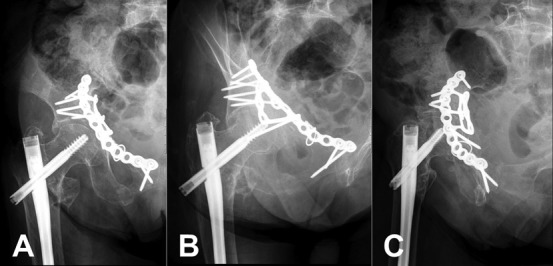
Fig. 1.
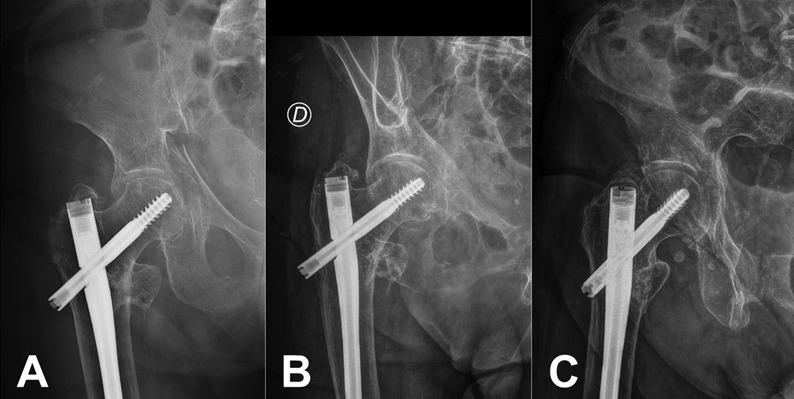
Radiographs showing the acetabular fracture (anterior column posterior hemitransverse fracture) in the right hemipelvis of an 84-year-old female patient in the anteroposterior (Fig. 1-A), obturator oblique (Fig. 1-B), and iliac oblique (Fig. 1-C) views according to Judet. The patient sustained this fracture after a simple fall and had a history of a fall resulting in a trochanteric fracture requiring fixation with an intramedullary nail.
Fig. 2.
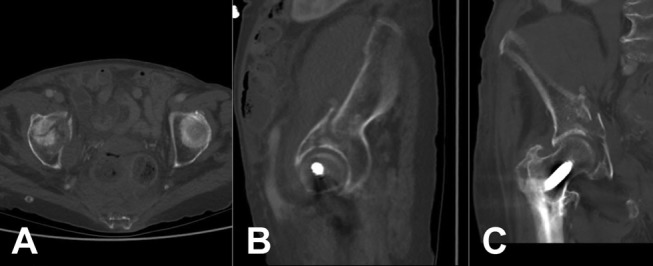
CT scans showing axial (Fig. 2-A), sagittal (Fig. 2-B), and coronal (Fig. 2-C) sections. The femoral head is medially displaced, the quadrilateral plate presents with a breakout, and no relevant dome impaction is noted.
Video 1.
Case presentation.
Video 2.
Options for extending the modified Stoppa approach to visualize the pelvic crest and high anterior column using the lateral (first) window of the ilioinguinal approach.
Step 2: Patient Positioning, Setup, and Skin Incision
Place the patient in the supine position and ensure that a Foley catheter is placed in the bladder and the ipsilateral leg is prepared and draped freely, facilitating reduction maneuvers. After sterile preparation and draping, make a 10-cm horizontal skin incision 2 fingerbreadths superior to the pubic symphysis.
Place the patient in the supine position on a radiolucent operating table (Video 3). Ensure that a pillow is placed underneath both knees for slight flexion of the hip to reduce tension of the iliopsoas muscle. Administer intravenous antibiotics using 1.5 g of cefuroxime preoperatively and place a Foley catheter for decompression and monitoring of potential iatrogenic bladder injuries during surgery.
In the operating room, place both arms of the patient on an arm board in abduction. Start with disinfection of the abdomen, from the costal arch superiorly to the midpoint of both thighs inferiorly. Also prepare and drape the ipsilateral leg to facilitate reduction.
Stand together with the scrub nurse on the uninjured side and place an assistant and the image intensifier at the injured side. Optionally, use an autoclavable ring retractor (SynFrame; DePuy Synthes), which is mounted to the operating table.
Identify the essential landmarks: the umbilicus, pubic symphysis, anterior superior iliac spines, and iliac crest. Perform a typical 10-cm horizontal Pfannenstiel incision 2 fingerbreadths superior to the pubic symphysis (Fig. 3-A).
Figs. 3-A through 3-D Schematic drawings showing the incision and dissection.
Fig. 3-A.
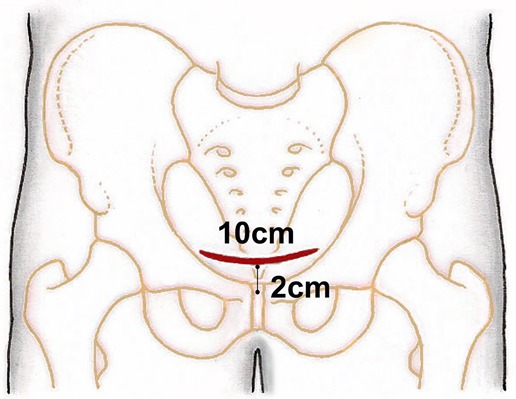
Fig. 3-A The landmarks for incision. A typical 10-cm horizontal Pfannenstiel incision is made 2 fingerbreadths superior to the pubic symphysis.
Video 3.
Patient positioning, setup, and skin incision.
Step 3: Superficial and Deep Dissection
Develop the anterior rectus sheath, split the sheath at the midline, incise the transversalis fascia, and approach the retropubic space.
Mobilize the subcutaneous fatty tissue and develop the anterior rectus fascia (Fig. 3-B, Video 4).
Identify and protect the spermatic cord or round ligament, split the rectus sheath midline between the 2 pyramidalis muscles, and incise the transversalis fascia superior to the pubic symphysis to gain access to the retropubic space of Retzius (Fig. 3-C).
Mobilize and protect the bladder with blunt dissection with a swab. Place a retractor underneath the pubic symphysis to protect urogenital structures (Fig. 3-D, Video 5).
Fig. 3-B.
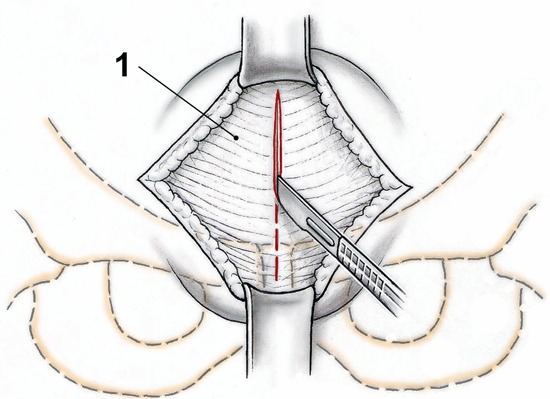
The superficial dissection. The subcutaneous fatty tissue is mobilized to develop the anterior rectus fascia (1), which is then incised in the midline.
Fig. 3-C.
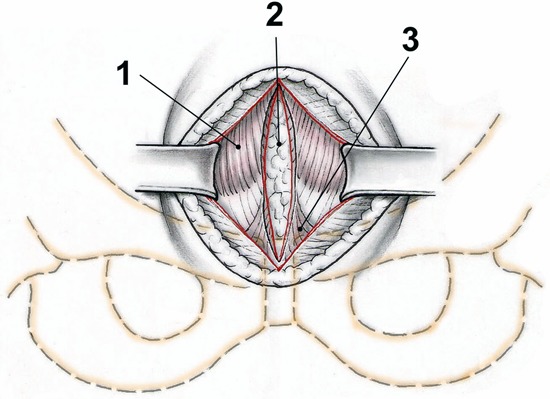
The interval between the rectus abdominis muscles (1) with the extraperitoneal fatty tissue (2) and distally the 2 pyramidalis muscles (3).
Fig. 3-D.
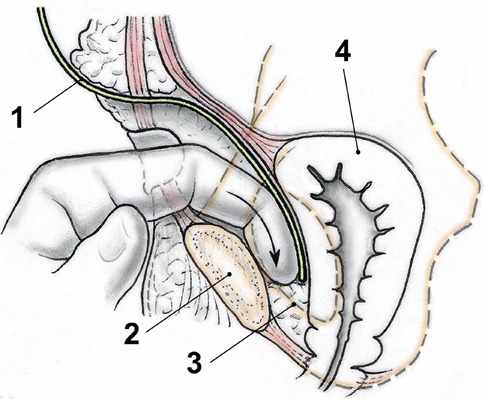
A malleable retractor (1) is placed underneath the symphysis (2) in the Retzius space (3) to protect the bladder (4).
Video 4.
Superficial dissection.
Video 5.
Deep dissection.
Step 4: Exposure of the Superior Pubic Ramus and Pelvic Brim with Control of the Neurovascular Structures
Elevate the rectus abdominis muscle insertion at the pubic rami and incise the iliopectineal fascia from the pubic symphysis to the iliopectineal eminence.
Place a Hohmann retractor around the superior pubic ramus to elevate the rectus abdominis muscle. A complete detachment of the rectus abdominis insertion at the pubic ramus is not necessary.
Perform a blunt epiperiosteal dissection of the pelvic brim up to the supra-acetabular region.
Identify and ligate a potential so-called corona mortis (Fig. 4-A, Video 5).
Incise the periosteum from the symphysis to the supra-acetabular region and dissect the bone subperiosteally. Mobilize the iliopectineal fascia from the pubic ramus.
Identify the external iliac vessels, the neurovascular obturator bundle, and the iliacus muscle (Fig. 4-B).
Place the Hohmann and malleable retractors subperiosteally to expose the fracture site at the pelvic brim and the quadrilateral plate after mobilization of the obturator internus muscle (Fig. 4-C). Ensure that traction to the obturator nerve is as light as possible; alternatively, the retractor can be placed medial to the obturator nerve.
Figs. 4-A through 4-K Images showing the open reduction and internal fixation of an acetabular fracture using the modified Stoppa approach.
Fig. 4-A.
The epigastric inferior artery (1), which may have an anastomosis—the so-called corona mortis (2)—with the obturator artery (3).
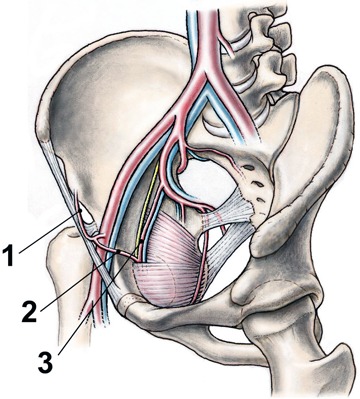
Fig. 4-B.
The exposure with an intrapelvic view from medial with the rectus abdominis (1), the obturator internus (2), the iliopsoas (3) and rectus abdominis muscles (4), and the neurovascular bundle (5) with the obturator nerve and vessels.
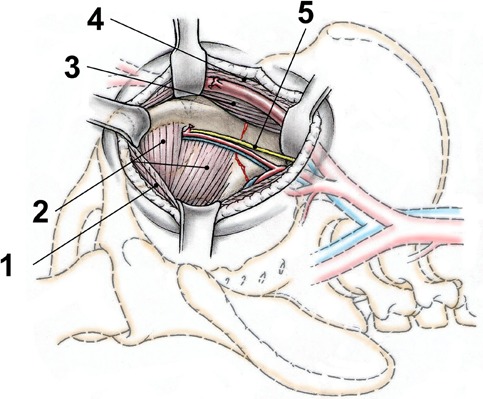
Fig. 4-C.
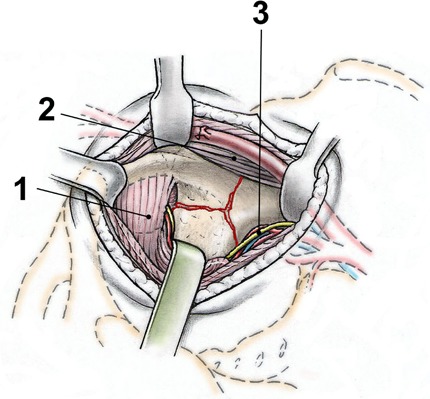
The exposure after partial detachment of the obturator internus muscle (1) and retraction of this muscle, the iliopsoas muscle (2), and the obturator nerve and vessels (3). Traction to the obturator nerve should be avoided if possible; alternatively, the retractor can be placed medial to the neurovascular bundle.
Step 5: Extension for Visualization of the Pelvic Crest and the Anterior Wall
To control fractures exiting the iliac crest (e.g., high anterior column fractures,) open the first window of the ilioinguinal approach.
Perform a separate 6 to 10-cm incision on the iliac crest and expose the abdominal wall musculature and detach it subperiosteally from the iliac crest and the iliac wing (shown on a cadaveric specimen in Video 2).
The first window of the ilioinguinal approach7 has been reported by some authors to be necessary in 55% to 93% of patients1,2,17-20, whereas others21-23 have described this combination as their standard procedure.
To obtain additional access for reduction, e.g., in low anterior column fractures and anterior wall fractures, the modified Stoppa approach presented here might be extended with the use of an additional modified Smith-Petersen approach24,25.
Step 6: Fracture Reduction and Fixation
Reduce the fracture with soft-tissue or skeletal traction, Schanz screws used with the so-called joystick technique, a collinear clamp, and/or a ball-spike pusher; disimpact the acetabular dome, if necessary, and use suprapectineal and infrapectineal reconstruction plates for fixation, if necessary.
Assess the extent of dislocation intraoperatively using anteroposterior and Judet views obtained with the image intensifier.
Use manual longitudinal soft-tissue traction or a traction table for the reduction of the medial displacement of the femoral head (Video 6).
In the case of residual medialization of the femoral head despite soft-tissue traction, place a Schanz screw into the greater trochanter under fluoroscopic control for lateral manual skeletal traction.
Use the femoral head as a template for anatomic reconstruction of the joint. Do not overdistract the joint as it may result in an overcorrection or secondary traction-related nerve palsies (Fig. 4-D). With an anterior dislocation of the quadrilateral plate, elevate an impacted dome fragment directly through the fracture (Fig. 4-E). Alternatively, perform an iliac osteotomy of the anterior column to provide access to the impacted dome11. Disimpact the dome fragment using a raspatory (Fig 4-F) and buttress the disimpacted dome fragment using a cortical screw placed from the infrapectineal side (Fig. 4-G).
Reduce displaced extra-articular components (such as the iliac wing posteriorly and the pubic ramus of the anterior column) using a Schanz screw, which is placed into the iliac wing and used as a joystick, or a Farabeuf clamp placed at the iliac crest (Fig. 4-H).
For direct reduction of the quadrilateral plate, use a ball-spike pusher in a medial to lateral direction. Alternatively, use an infrapectineal buttress plate acting as an indirect reduction tool (Figs. 4-I and 4-J, Video 7).
Reduce and compress a displaced posterior column with a collinear clamp and perform fixation with screws (Fig. 4-K).
For fixation, use non-locking, precontoured low-profile reconstruction plates and 3.5-mm cortical screws. In addition, place an infrapectineal buttress plate if necessary. Alternatively, use a combined plate for suprapectineal and infrapectineal fixation, which can also be used for reduction of the quadrilateral plate (Fig. 4-J).
Rule out intra-articular screw misplacement with an image intensifier (Fig. 5).
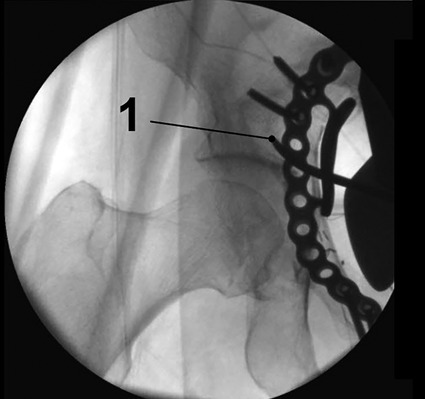
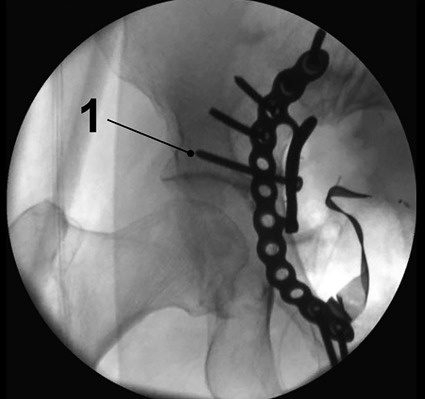
Fig. 5.
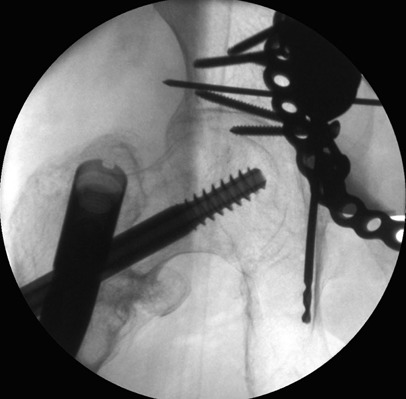
Intraoperative fluoroscopic image with an obturator-outlet view showing drilling for the position of an infra-acetabular screw placed according to the description by Culemann et al. to increase fixation strength14,29.
Video 6.
Fracture reduction.
Fig. 4-D.
Intraoperative anteroposterior view of a right hip using the image intensifier. The femoral head (1) is under traction using the Hana orthopaedic surgical table (Mizuho OSI), allowing for static traction for reduction of an acetabular dome fragment (2).
Fig. 4-E.
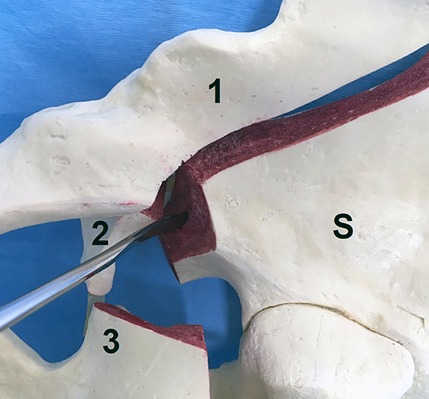
Photograph with a medial view of a Sawbones fracture model (Pacific Research Laboratories) of a right hemipelvis showing a dislocated anterior column posterior hemitransverse acetabular fracture with the displaced anterior column (1), quadrilateral plate (2), posterior hemitransverse fracture (3), and the stable part (S) of the right hemipelvis. The raspatory is used for subchondral disimpaction of an acetabular dome fragment directly through the fracture with the femoral head under traction.
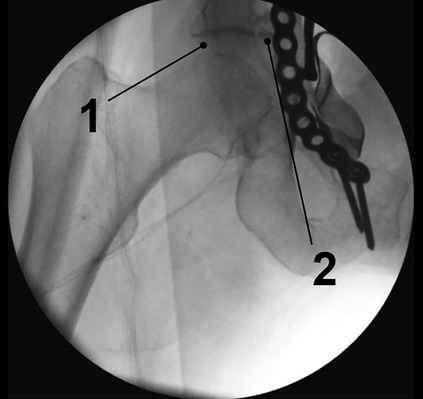
Fig. 4-F.
Intraoperative anteroposterior view of a right hip using the image intensifier. The acetabular dome fragment is reduced using a raspatory (1) inserted through an iliac osteotomy of the anterior column to provide access after fracture fixation.
Fig. 4-G.
Intraoperative anteroposterior view of a right hip joint using the image intensifier. The acetabular dome fragment is reduced and is buttressed using a 3.5-mm cortical screw placed from the infrapectineal side (1).
Fig. 4-H.
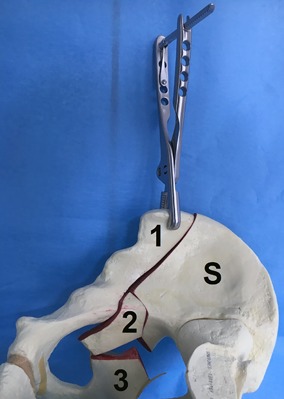
Photograph of the medial view of a Sawbones fracture model of a right hemipelvis depicting a dislocated anterior column posterior hemitransverse acetabular fracture with the displaced anterior column (1), quadrilateral plate (2), posterior hemitransverse fracture (3), and the stable part (S) of the hemipelvis. A Farabeuf clamp is used for reduction of the anterior column by a separate incision at the lateral window of the ilioinguinal approach.
Fig. 4-I.
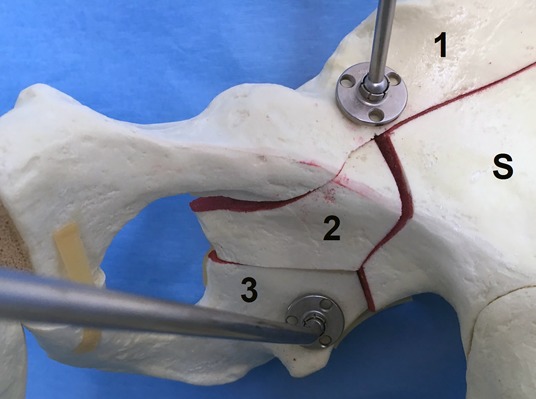
Photograph of the medial view of a Sawbones fracture model of a right hemipelvis depicting the reduction of a dislocated anterior column posterior hemitransverse acetabular fracture with the displaced anterior column (1), quadrilateral plate (2), posterior hemitransverse fracture (3), and the stable part (S) of the right hemipelvis. For reduction of the anterior column, the quadrilateral plate, and the posterior column, ball-spike pushers (straight and/or curved) are used with spiked washers attached to the pushers.
Fig. 4-J.
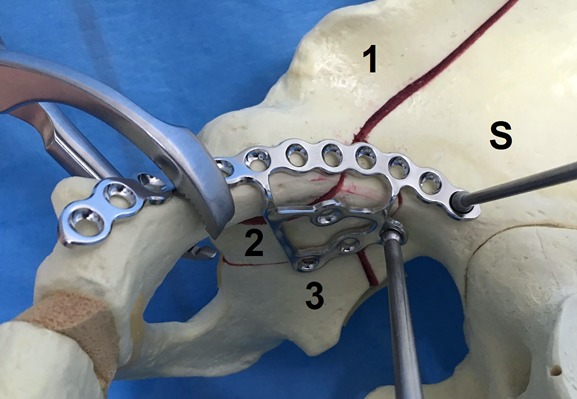
Photograph of the medial view of a Sawbones fracture model of a right hemipelvis depicting the reduction of a dislocated anterior column posterior hemitransverse acetabular fracture with the displaced anterior column (1), quadrilateral plate (2), posterior hemitransverse fracture (3), and the stable part (S) of the right hemipelvis. For reduction of the anterior column, the quadrilateral plate, and the posterior column, ball-spike pushers (straight and/or curved) pushing a combined plate for suprapectineal and infrapectineal fixation can be used.
Fig. 4-K.
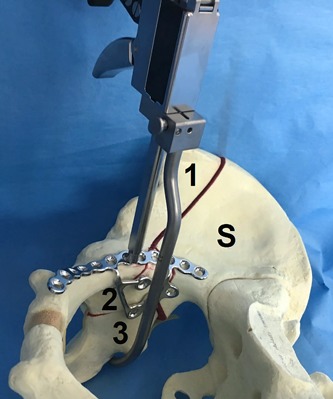
Photograph of the medial view of a Sawbones fracture model of a right hemipelvis depicting a dislocated anterior column posterior hemitransverse acetabular fracture with the displaced anterior column (1), quadrilateral plate (2), posterior hemitransverse fracture (3), and the stable part (S) of the right hemipelvis. A collinear reduction clamp can be used for compression of the posterior column to the anterior column.
Video 7.
Fracture fixation.
Step 7: Wound Closure
Check the urine output for hematuria, suture the anterior lamina of the rectus sheath, and perform a layered closure.
Place a suction drain in the Retzius space routinely and remove if drainage is <40 mL per 24 hours (Video 8).
Close the anterior lamina of the rectus sheath using absorbable sutures after wound irrigation if hemostasis and clear urine output is noted.
Perform a layered closure of the subcutaneous and cutaneous tissues.
Video 8.
Wound closure.
Step 8: Postoperative Care
Postoperatively, instruct the patient to use toe-touch weight-bearing for the first 3 months.
Check the accuracy of the reduction using plain radiographs (Fig. 6) and CT scans (Fig. 7, Video 9).
Restrict mobilization to toe-touch weight-bearing for the first 3 months.
Prescribe low-molecular-weight heparin for this period as prophylaxis against deep venous thrombosis.
Allow for full weight-bearing as tolerated with the assistance of a physiotherapist if fracture consolidation is evident 3 months postoperatively.
Follow the patients routinely with clinical and radiographic evaluations at 6 and 12 weeks and then 12 and 24 months after surgery.
In the case presented, the patient did not show any signs of posttraumatic osteoarthritis 1 year postoperatively (Fig. 8).
Fig. 6.
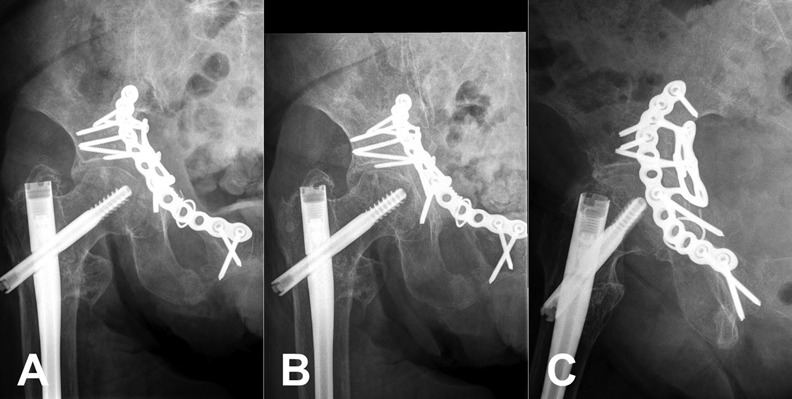
Radiographs showing the anatomic postoperative reduction in the anteroposterior (Fig. 6-A), obturator oblique (Fig. 6-B), and iliac oblique views according to Judet (Fig. 6-C).
Fig. 7.
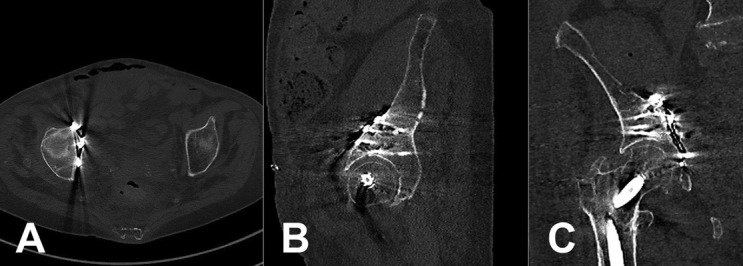
CT scans showing anatomic reduction on axial (Fig. 7-A), sagittal (Fig. 7-B), and coronal sections (Fig. 7-C).
Fig. 8.
Radiographs, made 1 year after surgery, showing no signs of posttraumatic osteoarthritis in the anteroposterior (Fig. 8-A), obturator oblique (Fig. 8-B), and iliac oblique (Fig. 8-C) views, according to Judet.
Video 9.
Postoperative evaluation and follow-up.
Results
Anatomic reduction was achieved in 72% of our 59 patients2 who were 13 to 89 years old and in 52% to 82% of patients, with a mean age from 38 to 64 years, who were described in other studies12,17,18,21-23,26,27. In 1 randomized controlled trial, the operative time, blood loss, and amount of blood transfusions were reduced after utilization of the modified Stoppa approach compared with the ilioinguinal approach1. Conversion to total hip replacement was performed in up to 14% of the cases26.
In 69% of our patients (mean age, 57 years) with preserved hips, the clinical outcome at the midterm follow-up was excellent or good. Conversion to total hip replacement was necessary in 16% of our patients within the first 2 years. No differences in outcome were observed in patients who were <60 years old and those who were ≥60 years old2.
Pitfalls & Challenges
Limited access (e.g., in cases with displaced iliac wing or low anterior column fractures).
An additional first window of the ilioinguinal approach is required in 55% to 93% of patients1,2,17-20.
An additional first window of the ilioinguinal approach as a standard procedure21-23.
An additional modified Smith-Petersen approach is required2.
Limited variability of screw directions posteriorly28.
Stretching of the obturator nerve during exposure of the quadrilateral plate.
Traction injuries to the lateral femoral cutaneous nerve and/or femoral nerve.
Postoperative abdominal wall hernia.
Acknowledgments
Note: The authors thank Bertrand W. Parcells, MD, Associate Professor, Department of Orthopedics, Monmouth Medical Center, Long Branch, New Jersey, for linguistic help in the preparation of the manuscript.
Footnotes
Published outcomes of this procedure can be found at: Injury. 2013 Dec;44(12):1793-8.
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSEST/A234).
References
- 1.Ma K, Luan F, Wang X, Ao Y, Liang Y, Fang Y, Tu C, Yang T, Min J. Randomized, controlled trial of the modified Stoppa versus the ilioinguinal approach for acetabular fractures. Orthopedics. 2013. October 1;36(10):e1307-15. [DOI] [PubMed] [Google Scholar]
- 2.Bastian JD, Tannast M, Siebenrock KA, Keel MJ. Mid-term results in relation to age and analysis of predictive factors after fixation of acetabular fractures using the modified Stoppa approach. Injury. 2013. December;44(12):1793-8. Epub 2013 Aug 15. [DOI] [PubMed] [Google Scholar]
- 3.Ferguson TA, Patel R, Bhandari M, Matta JM. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br. 2010. February;92(2):250-7. [DOI] [PubMed] [Google Scholar]
- 4.Lange TA, Alter AJ., Jr Evaluation of complex acetabular fractures by computed tomography. J Comput Assist Tomogr. 1980. December;4(6):849-52. [DOI] [PubMed] [Google Scholar]
- 5.Hüfner T, Pohlemann T, Gänsslen A, Assassi P, Prokop M, Tscherne H. [The value of CT in classification and decision making in acetabulum fractures. A systematic analysis]. [German.]. Unfallchirurg. 1999. February;102(2):124-31. [DOI] [PubMed] [Google Scholar]
- 6.Harley JD, Mack LA, Winquist RA. CT of acetabular fractures: comparison with conventional radiography. AJR Am J Roentgenol. 1982. March;138(3):413-7. [DOI] [PubMed] [Google Scholar]
- 7.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. preliminary report. J Bone Joint Surg Am. 1964. December;46:1615-46. [PubMed] [Google Scholar]
- 8.Tosounidis TH, Giannoudis VP, Kanakaris NK, Giannoudis PV. The ilioinguinal approach: state of the art. JBJS Essential Surg Tech. 2018. June 27;8(2):e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mears DC. Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J Am Acad Orthop Surg. 1999. Mar-Apr;7(2):128-41. [DOI] [PubMed] [Google Scholar]
- 10.Pohlemann T, Culemann U. Summary of controversial debates during the 5th “Homburg Pelvic Course” 13-15 September 2006. Injury. 2007. April;38(4):424-30. Epub 2007 Mar 30. [DOI] [PubMed] [Google Scholar]
- 11.Casstevens C, Archdeacon MT., dʼHeurle A, Finnan R. Intrapelvic reduction and buttress screw stabilization of dome impaction of the acetabulum: a technical trick. J Orthop Trauma. 2014. June;28(6):e133-7. [DOI] [PubMed] [Google Scholar]
- 12.Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994. August;(305):112-23. [PubMed] [Google Scholar]
- 13.Culemann U, Holstein JH, Köhler D, Tzioupis CC, Pizanis A, Tosounidis G, Burkhardt M, Pohlemann T. Different stabilisation techniques for typical acetabular fractures in the elderly—a biomechanical assessment. Injury. 2010. April;41(4):405-10. Epub 2009 Dec 24. [DOI] [PubMed] [Google Scholar]
- 14.Culemann U, Marintschev I, Gras F, Pohlemann T. Infra-acetabular corridor—technical tip for an additional screw placement to increase the fixation strength of acetabular fractures. J Trauma. 2011. January;70(1):244-6. [DOI] [PubMed] [Google Scholar]
- 15.Qureshi AA, Archdeacon MT, Jenkins MA, Infante A, DiPasquale T, Bolhofner BR. Infrapectineal plating for acetabular fractures: a technical adjunct to internal fixation. J Orthop Trauma. 2004. March;18(3):175-8. [DOI] [PubMed] [Google Scholar]
- 16.Sen RK, Tripathy SK, Aggarwal S, Goyal T, Mahapatra SK. Comminuted quadrilateral plate fracture fixation through the iliofemoral approach. Injury. 2013. February;44(2):266-73. Epub 2012 Nov 28. [DOI] [PubMed] [Google Scholar]
- 17.Khoury A, Weill Y, Mosheiff R. The Stoppa approach for acetabular fracture. Oper Orthop Traumatol. 2012. September;24(4-5):439-48. [DOI] [PubMed] [Google Scholar]
- 18.Sagi HC, Afsari A, Dziadosz D. The anterior intra-pelvic (modified Rives-Stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010. May;24(5):263-70. [DOI] [PubMed] [Google Scholar]
- 19.Isaacson MJ, Taylor BC, French BG, Poka A. Treatment of acetabulum fractures through the modified Stoppa approach: strategies and outcomes. Clin Orthop Relat Res. 2014. November;472(11):3345-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shazar N, Eshed I, Ackshota N, Hershkovich O, Khazanov A, Herman A. Comparison of acetabular fracture reduction quality by the ilioinguinal or the anterior intrapelvic (modified Rives-Stoppa) surgical approaches. J Orthop Trauma. 2014. June;28(6):313-9. [DOI] [PubMed] [Google Scholar]
- 21.Andersen RC, O’Toole RV, Nascone JW, Sciadini MF, Frisch HM, Turen CW. Modified Stoppa approach for acetabular fractures with anterior and posterior column displacement: quantification of radiographic reduction and analysis of interobserver variability. J Orthop Trauma. 2010. May;24(5):271-8. [DOI] [PubMed] [Google Scholar]
- 22.Jakob M, Droeser R, Zobrist R, Messmer P, Regazzoni P. A less invasive anterior intrapelvic approach for the treatment of acetabular fractures and pelvic ring injuries. J Trauma. 2006. June;60(6):1364-70. [DOI] [PubMed] [Google Scholar]
- 23.Laflamme GY, Hebert-Davies J, Rouleau D, Benoit B, Leduc S. Internal fixation of osteopenic acetabular fractures involving the quadrilateral plate. Injury. 2011. October;42(10):1130-4. Epub 2010 Dec 14. [DOI] [PubMed] [Google Scholar]
- 24.Kloen P, Siebenrock KA, Ganz R. Modification of the ilioinguinal approach. J Orthop Trauma. 2002. September;16(8):586-93. [DOI] [PubMed] [Google Scholar]
- 25.Smith-Petersen MN. Approach to and exposure of the hip joint for mold arthroplasty. J Bone Joint Surg Am. 1949. January;31A(1):40-6. [PubMed] [Google Scholar]
- 26.Hirvensalo E, Lindahl J, Kiljunen V. Modified and new approaches for pelvic and acetabular surgery. Injury. 2007. April;38(4):431-41. [DOI] [PubMed] [Google Scholar]
- 27.Ponsen KJ, Joosse P, Schigt A, Goslings JC, Luitse JS. Internal fracture fixation using the Stoppa approach in pelvic ring and acetabular fractures: technical aspects and operative results. J Trauma. 2006. September;61(3):662-7. [DOI] [PubMed] [Google Scholar]
- 28.Bastian JD, Savic M, Cullmann JL, Zech WD, Djonov V, Keel MJ. Surgical exposures and options for instrumentation in acetabular fracture fixation: pararectus approach versus the modified Stoppa. Injury. 2016. March;47(3):695-701. Epub 2016 Jan 29. [DOI] [PubMed] [Google Scholar]
- 29.Marintschev I, Gras F, Schwarz CE, Pohlemann T, Hofmann GO, Culemann U. Biomechanical comparison of different acetabular plate systems and constructs—the role of an infra-acetabular screw placement and use of locking plates. Injury. 2012. April;43(4):470-4. Epub 2012 Jan 18. [DOI] [PubMed] [Google Scholar]


