Abstract
Online technologies are well integrated into the day-to-day lives of individuals with alcohol and other drug (i.e., substance use) problems. Interventions that leverage online technologies have been shown to enhance outcomes for these individuals. To date, however, little is known about how those with substance use problems naturally engage with such platforms. In addition, the scientific literatures on health behavior change facilitated by technology and harms driven by technology engagement have developed largely independent of one another. In this secondary analysis of the National Recovery Study (NRS), which provides a geo-demographically representative sample of US adults who resolved a substance use problem, we examined a) the weighted prevalence estimate of individuals who engaged with online technologies to “cut down on substance use, abstain from substances, or strengthen one’s recovery” (i.e., recovery-related use of online technology, or ROOT), b) clinical/recovery correlates of ROOT, controlling for demographic covariates, and c) the unique association between ROOT and self-reported history of internet addiction. Results showed one in ten (11%) NRS participants reported ROOT. Significant correlates included greater current psychological distress, younger age of first substance use, as well as history of anti-craving/anti-relapse medication, recovery support services, and drug court participation. Odds of lifetime internet addiction were 4 times greater for those with ROOT (vs. no ROOT). These data build on studies of technology-based interventions, highlighting the reach of ROOT, and therefore, the potential for a large, positive impact on substance-related harms in the US.
Keywords: Recovery, Technology, mHealth, Social network sites, Smartphone applications
1. Introduction
Online technologies, including websites and smartphone applications (“apps”), are well integrated into the day-to-day lives of most individuals living in the United States (US). Among US adults, 88% use the internet, 77% use a smartphone, and 69% use social network sites, like Facebook, Instagram, and Twitter (Smith, 2017). Increasingly during the past decade, researchers have begun leveraging these online technologies to help address alcohol and other drug (i.e., substance use) problems (Fowler, Holt, & Joshi, 2016; Marsch, 2012). (While substance use problems may transcend diagnostic nomenclature, for simplicity, we generally refer to them as substance use disorder, or SUD.) For the 10% of US adults with SUD who seek services (Park-Lee, Lipari, Hedden, Kroutil, & Porter, 2017), accessible and low-cost resources are needed to help boost outcomes. For the 90% who do not seek services (Park-Lee et al., 2017), innovative strategies are needed to engage them with recovery-supportive tools, interventions, and communities.
Online, recovery-supportive technologies may enhance the field’s ability to reach individuals who do not feel they need formal treatment (Park-Lee et al., 2017), have difficulty accessing treatment due to geographical or other life constraints, feel inhibited by fear or shame (Keyes et al., 2010), or may be willing to address their SUD provided only a small effort is required. Of note, a service’s overall public health impact on the societal burden of SUD (Stahre, Roeber, Kanny, Brewer, & Zhang, 2014; Centers for Disease Control and Prevention [CDC], 2018; Rehm et al., 2009; National Drug Intelligence Center, 2011) is a function of both its effectiveness and reach (Glasgow, Klesges, Dzewaltowski, Estabrooks, & Vogt, 2006; Glasgow, Mckay, Piette, & Reynolds, 2001). Thus, given that they are ubiquitous and typically incur little or no cost to the end-user, online technology-based services may help address critical gaps in U.S. systems of SUD care.
1.1. Use of technology in SUD treatment
Prior studies in this area have examined technology use more generally (i.e., not specific to addressing substance use) among treatment-seekers. Specifically, studies conducted in both outpatient and inpatient treatment programs have shown 85–93% of patients own a mobile phone (Dahne & Lejuez, 2015; McClure, Acquavita, Harding, & Stitzer, 2013), 47–72% own a smartphone (Ashford, Lynch, & Curtis, 2018; Dahne & Lejuez, 2015; Milward, Day, Wadsworth, Strang, & Lynskey, 2015), 44% regularly use the internet (McClure et al., 2013), 66% use their phones to access the internet, and 64% download smartphone apps (Dahne & Lejuez, 2015). Three-fourths have a social network site account and two-thirds participate on at least one social network site weekly (Ashford et al., 2018).
Such engagement bodes well for the ultimate, broader application of technology-based intervention (TBI; Marsch, 2012) to SUD treatment. TBIs – which include online technology as well as mobile text message (e.g., Gonzales, Ang, Murphy, Glik, & Anglin, 2014) and offline computer-based technologies (e.g., Carroll et al., 2008) – harness digital innovation to increase the reach, fidelity, and efficiency of existing, evidence-based services in both clinical and non-clinical settings (Onken & Shoham, 2015). In clinical settings, TBIs typically employ psychoeducation and skill building. In non-clinical settings, brief interventions (e.g., personalized normative feedback) are common. Reviews suggest TBIs are generally better than inactive comparison conditions (e.g., self-help reading materials; Fowler et al., 2016; Litvin, Abrantes, & Brown, 2013). They may do as well as clinician-led approaches both for individuals with SUD (Fowler et al., 2016; Litvin et al., 2013), and co-occurring substance use and mental health problems (Sugarman, Campbell, Iles, & Greenfield, 2017). In clinical settings, TBIs that are added to, or substituted for parts of, usual treatment may yield the best outcomes (Carroll et al., 2008; Gustafson et al., 2014; Marsch et al., 2014). While brief interventions among college students are overrepresented in this literature, a review of TBI mechanisms suggests they mobilize change via similar psychological processes as face-to-face interventions, such as modified peer drinking norms, and increased coping skill quality (Dallery, Jarvis, Marsch, & Xie, 2015). Far less is known about how social network sites fare in TBI research, though they, too, have been leveraged to deliver existing evidence-based interventions (Ridout & Campbell, 2014). Importantly, two-thirds of an outpatient SUD sample indicated social network sites would be a good place to receive information to aid initiation or maintenance of substance problem resolution (Ashford et al., 2018).
In order to build on surveys assessing general technology engagement among SUD treatment seekers, and rigorous TBI research, the field may benefit from real-world, naturalistic examinations of online technology engagement specifically to address substance problems (hereafter referred to as recovery-related use of online technology, or ROOT). These data would inform both the baseline reach of ROOT - absent major policies to aid dissemination - and a scientific agenda for future research in the area.
1.2. The current study
This current study leveraged a geo-demographically representative sample of US adults who resolved a substance use problem (from the National Recovery Study, or NRS; Kelly, Bergman, Hoeppner, Vilsaint, & White, 2017; Kelly, Greene, & Bergman, 2017; Kelly, Greene, & Bergman, 2018) to conduct the first nationwide investigation of ROOT. This analysis of ROOT in the NRS had the following specific aims:
-
1)
To examine the overall prevalence of ROOT including engagement with a) online mutual-help organization (MHO) meetings, as well as use of b) recovery-specific social network sites, c) general-interest social network sites, and d) other online technologies (e.g., “non-social” smartphone apps) to aid initiation or maintenance of substance use problem resolution; and
-
2)
To examine clinical/recovery correlates of ROOT, controlling for demographic characteristics.
We hypothesized that younger age, greater levels of education, and higher levels of income would each be significantly associated with ROOT – in line with prior SUD treatment samples (Ashford et al., 2018; Dahne & Lejuez, 2015; McClure et al., 2013). From the health beliefs model (Finney & Moos, 1995; Rosenstock, 1990), individuals with greater substance use severity may have greater problem recognition, and thus a greater propensity to try a wider range of strategies to resolve their problem. As such, we hypothesized that variables indicative of clinical severity including service utilization (anti-craving/anti-relapse medication, outpatient or inpatient specialty treatment, and recovery support services), younger age of first use, and more substances used in one’s lifetime would also be associated with ROOT. Given the paucity of scientific research to date on ROOT, we also explored several other potential ROOT correlates, such as primary substance and criminal justice history.
In addition, individuals with a history of substance use problems may also have heightened neurobiological vulnerability to reinforcement derived from online technology engagement including both positive, social reinforcement (i.e., receiving “likes” on a post) and negative reinforcement (i.e., avoiding unpleasant feelings; Volkow, Koob, & McLellan, 2016). It is widely accepted that evaluating a new intervention or resource involves an examination of risks to help contextualize benefits. Despite increased research on “internet addiction”, including problematic smartphone and social network site use (Andreassen, Torsheim, Brunborg, & Pallesen, 2012; Elhai, Dvorak, Levine, & Hall, 2017; Kuss, Griffiths, Karila, & Billieux, 2014), research on SUD-related health behavior change facilitated by technology, has developed largely independent of this scientific literature on technology-associated risks. In order to begin highlighting any risks of technology engagement for individuals with SUD, ultimately resulting in a risk-benefit analysis of ROOT, we also explored whether ROOT was associated with a subjective history of “internet addiction”.
2. Method
2.1. Procedure
The NRS assessed US adults (18+ years) who responded “yes” to the screening question “Did you used to have a problem with drugs or alcohol, but no longer do?”. While NRS methods have been detailed elsewhere (Kelly, Bergman, et al., 2017), in brief, NRS data were derived from international survey company GfK’s “KnowledgePanel” (GfK, 2013), which uses address-based sampling to randomly select individuals from 97% of all US households based on the US Postal Service’s Delivery Sequence File. Only a sub-set of the KnowledgePanel received invitations to screen into the survey (i.e., individuals generally receive no more than one study opportunity per week), and, of those, only a subset responded to the NRS screening question.
Since this KnowledgePanel subsample (25,229 of the 39,809 invited to complete the screening question) was no longer representative of US adults, GfK conducted a two-step process, called iterative proportional fitting or raking (Battaglia, Hoaglin, & Frankel, 2009), in order to produce participant weights that, when accounted for in analyses, yielded unbiased estimates of the population of US adults. First, base weights accounted for any over-coverage or under-coverage of geodemographic characteristics in those who were invited to respond to the screening question, as well as systematic differential response to the screening question (e.g., females are overrepresented, and 18–29 year olds are underrepresented in the sample of individuals who responded to the screening question relative to the general population). Next, base weight adjustments are made so sample characteristics map onto eight geo-demographic benchmarks from the March 2015 Current Population Survey (gender; age; race/Hispanic ethnicity; education; census geographical region; household income; home ownership status; and metropolitan area) (United States Census Bureau, 2015). Each individual is assigned one weight that aligns the KnowledgePanel subsample with all eight benchmarks simultaneously.
This survey procedure yields unbiased estimates of the population for those who screened into the NRS (e.g., U.S. adults who resolved a problem with drugs or alcohol). Given the inherent uncertainty when inferring population parameters from sample data, we use 95% confidence intervals throughout the manuscript. Of note, studies have demonstrated that data obtained from the KnowledgePanel are comparable to estimates derived from national surveys that used non-internet methodologies to recruit and collect data, such as household, telephone, or in-person surveys (e.g., Heeren et al., 2008).
2.2. Participants
Results of the primary NRS analyses showed that 9.1% of the US adult population (22.35 million individuals) have resolved a substance use problem (Kelly, Bergman, et al., 2017). Consistent with GfK’s rigorous approach, the sample (N = 2002; M = 46.7 years; SD = 15.3) was diverse demographically in virtually all respects. For example, weighted estimates showed that 40% were female while 61% were White and non-Hispanic, 17% Hispanic, 14% Black and non-Hispanic, 6% Other Race and non-Hispanic, and 2% two or more races and non-Hispanic. Clinically, participants resolved their substance use problem, on average, 11.8 years ago (SD = 11.0) and, among respondents, three-fifths identified alcohol as their primary substance. Half (53.9%) used some type of SUD treatment or other recovery support service, and half (51.6%) were currently abstinent from all substances.
2.3. Measures
2.3.1. Recovery-related use of online technology (ROOT)
Participants were categorized in the ROOT group if they indicated yes to a) any “attendance” at one or more online MHO meetings, b) social network site-related problem resolution, or c) other online resource-related problem resolution, as specified below.
2.3.1.1. Attendance at online MHO meetings.
Individuals reported whether they ever “attended” an online MHO meetings for those MHOs that they acknowledged any lifetime attendance choosing from a list of 12-step (e.g., Alcoholics Anonymous), non-12-step or secular (e.g., SMART Recovery), and religious (Celebrate Recovery) MHOs (Kelly, Urbanoski, Hoeppner, & Slaymaker, 2011)
2.3.1.2. Social network sites.
Participants indicated which social network sites from a given list (or other) they used to help “cut down on substance use, abstain from substances, or strengthen [their] recovery”, including both recovery-specific sites (e.g., InTheRooms.com; Bergman, Kelly, Hoeppner, Vilsaint, & Kelly, 2017) as well as general-interest sites (e.g., Facebook).
2.3.1.3. “Non-social” smartphone apps and other online resources.
Participants indicated whether they “ever used an online resource that was not a social network site to help cut down on substance use, abstain from substances, or strengthen [their] recovery (e.g., mobile smartphone application, or ‘app’, that provided motivating messages to help you quit)”.
2.3.2. Internet addiction
Participants indicated whether they ever had a problem with “internet addiction (other than for sex, gambling or shopping)” in their lifetime as part of a list of seven possible problem behaviors (Laudet, Harris, Kimball, Winters, & Moberg, 2015).
2.3.3. Substance use and problem resolution
Participants reported from a list of 15 substances (Dennis, Titus, White, Unsicker, & Hodgkins, 2002) those they used 10 or more times, and, of those, 1) whether they had a problem with that substance, 2) age of first use (from which we created a dichotomous variable capturing first use of any substance < 15 vs. ≥15years)(Substance Abuse and Mental Health Administration, 2017) and 3) primary substance (Brown et al., 1998), categorized as alcohol, cannabis, opioids, and other drugs. Participants reported also how long it had been since resolving their problem (trichotomized into 0–5 years, 5–15 years, and 15+ years).
2.3.4. Service utilization
Participants reported lifetime use of outpatient or inpatient/residential treatment (Institute of Behavioral Research, 2002) and antirelapse/craving medication for alcohol and opioids (e.g., naltrexone [oral and injectable] or buprenorphine/naloxone [Suboxone]; Miller & Del Boca, 1994). We do not report on their participation in MHOs more generally (e.g., AA, NA, SMART Recovery; Kelly et al., 2011) as a function of ROOT, since greater MHO attendance among those with ROOT is an artifact of a participant needing to have reported lifetime MHO attendance in order to respond to an item regarding online MHO attendance, an indicator of ROOT. See Kelly, Bergman, et al. (2017) for data on MHO attendance in the NRS more generally. We do, however, report other community-based recovery support where trained staff typically aid in service provision (e.g., faith-based recovery services or recovery community centers; Institute of Behavioral Research, 2002)
2.3.5. Criminal justice history
We used items from the Form-90 (Miller & Del Boca, 1994) to determine lifetime histories of any arrest (yes/no) and, if arrested, any drug court participation (yes/no).
2.3.6. Recovery capital
Participants completed the Brief Assessment of Recovery Capital (BARC-10; Vilsaint et al., 2017), a validated 10-item short form of the Addiction Recovery Capital Scale (α = 0.93; Groshkova, Best, & White, 2012).
2.3.7. Quality of life
The questionnaire included the EUROHIS-QOL (Schmidt, Muhlan, & Power, 2006), a widely used eight-item measure of quality of life, adapted from the World Health Organization Quality of Life – Brief Version (α = 0.90).
2.3.8. Psychological distress
We used the Kessler-6 (Kessler et al., 2003) to assesses psychological distress, sometimes referred to as psychiatric symptoms, during the past 30 days (α = 0.93).
2.4. Statistical analysis
To examine ROOT prevalence, we calculated the survey-weighted proportion for any of a) lifetime online MHO attendance, as well as lifetime use of b) recovery-specific social network sites, c) general-interest social network sites, and d) non-social smartphone apps and other online resources to initiate or maintain problem resolution.
We used logistic regression models to examine demographic and clinical correlates of ROOT. We first examined demographics as a set, including age, gender, education level, race/ethnicity, household income, and household internet access, and present pseudo-R2 for the model. Next we examined each of the following clinical/recovery characteristics as an individual predictor controlling for the set of demographics mentioned above (i.e., each predictor is tested in its own logistic regression model with ROOT as the outcome, controlling for demographic characteristics): primary substance, number of substances used ten or more times, age at first substance use, complete abstinence, years since initiating current problem resolution episode, as well as lifetime history of taking anti-relapse/craving medication, outpatient or inpatient treatment, recovery support service utilization (apart from MHOs), arrest with and without drug court participation, psychological distress, quality of life, and recovery capital.
We also constructed a logistic regression model to examine whether ROOT (the predictor in this model) is uniquely associated with self-reported history of “internet addiction” (outcome), controlling for the same set of demographics as above, as well as significant clinical/recovery characteristics determined from the prediction of ROOT as above. Here, we were interested in the odds of “internet addiction” associated with ROOT – as a proxy for potential risk.
All analyses were survey-weighted and conducted using the svy package in Stata Version 14 (StataCorp, 2015). All study procedures were approved by the Partners HealthCare Institutional Review Board.
3. Results
3.1. Prevalence of ROOT
Among US adults who resolved a substance use problem, 11.0% (95% CI: 8.8–13.1) reported ROOT. Non-social smartphone apps and other online resources were the most commonly utilized online services, followed in order of prevalence by, general-interest social network sites, online MHOs, and recovery-specific social network sites (Table 1).
Table 1.
Lifetime participation in online mutual-help organizations, social network sites, and non-social smartphone applications and other online resources to “cut down on substance use, abstain from substances, or strengthen recovery” (recovery- related use of online technology; ROOT) among a representative sample of US adults who resolved an alcohol or other drug problem (N = 2002).
| Prevalence % | 95% CI | |
|---|---|---|
| Non-social smartphone apps and online resources (“Other”)a |
5.6 | 3.94–7.26 |
| Online MHO attendance (any) | 4.1 | 2.70–5.44 |
| Alcoholics Anonymous | 2.1 | 1.35–2.83 |
| Narcotics Anonymous | 1.0 | 0.32–1.66 |
| Marijuana Anonymous | 0.7 | 0–1.57 |
| Crystal Methamphetamine Anonymous | 0.3 | 0–0.76 |
| LifeRing Secular Recovery | 0.3 | 0–0.76 |
| SMART Recovery | 0.2 | 0.04–0.43 |
| Women for Sobriety | 0.1 | 0–0.17 |
| Cocaine Anonymous | 0.0 | 0–0.11 |
| Moderation Management | 0.0 | 0–0.12 |
| General-interest social network sites (any) | 4.9 | 3.27–6.44 |
| 3.4 | 2.17–4.63 | |
| 1.1 | 0.25–1.93 | |
| Youtube | 1.3 | 0.36–2.20 |
| 0.9 | 0.15–1.66 | |
| Myspace | 0.6 | 0.01–1.27 |
| 0.6 | 0.01–1.11 | |
| Snapchat | 0.6 | 0–1.35 |
| Tumblr | 0.6 | 0–1.31 |
| Foursquare | 0.5 | 0–1.11 |
| 0.5 | 0–1.22 | |
| Google Plus | 0.3 | 0.03–0.47 |
| Meetup | 0.3 | 0–0.85 |
| Flickr | 0.2 | 0–0.37 |
| Vine | 0.1 | 0–0.20 |
| Recovery-specific social network sites (any) | 3.0 | 1.66–4.35 |
| Daily Strength | 1.0 | 0.13–1.91 |
| In the Rooms | 1.0 | 0.21–1.78 |
| myRecovery | 0.5 | 0–1.07 |
| Addiction Tribe | 0.3 | 0–0.66 |
| iRecover | 0.2 | 0–0.45 |
| Sober Grid | 0.2 | 0–0.39 |
| Recovery-Related Use of Online Technology (any) | 11.0 | 8.84–13.09 |
For this item participants were asked “Have you ever used an online resource that was not a social network site to help you cut down on substance use, abstain from substances, or strengthen your recovery (i.e., mobile smartphone application, or ‘app’, that provided motivating messages to help you quit)?”
3.2. Correlates of ROOT
In the prediction of ROOT from the set of demographic characteristics, significant positive correlates of ROOT were being 18–29 years old (versus 45–59 and 60 + ), having less education than a high school diploma (vs. high school diploma), Hispanic race/ethnicity (vs. White), and having a household income below $30,000 (vs. $100,000 + ) (p < 0.05; Table 2). Controlling for all demographic characteristics, and testing one predictor at a time, significant positive correlates of ROOT were younger age of first substance use, having taken anti-relapse/craving medication, recovery support service utilization, history of arrest and drug court involvement (vs. no arrest history), and more psychological distress (p < 0.05; Table 2). To demonstrate interpretation of a significant dichotomous predictor, for example, unique odds of ROOT (controlling for demographics) are 5.6 times greater for individuals who have taken anti-relapse/craving medication versus those who have not. To demonstrate interpretation of a significant continuous predictor, for example, each additional 1 year less in age of first substance use is uniquely associated with a 7% increase in ROOT odds (and, conversely, 1 year more a 7% decrease). Fig. 1 shows raw proportions of ROOT to illustrate examples of ROOT correlates, including anti-relapse/craving medication, recovery support services, and criminal justice involvement.
Table 2.
Logistic regression models examining the prediction of recovery-related use of online technology (ROOT; overall prevalence = 11%) from a) the set demographic covariates (top) and b) each individual clinical/recovery variable controlling for the set of demographic correlates (bottom).
| No ROOT column % or mean (SD) |
ROOT column % or mean (SD) |
Adjusted OR | Pseudo R2 | |
|---|---|---|---|---|
| Age, years (%) | ||||
| 18–29 | 15.9 | 29.0 | 1a | |
| 30–44 | 26.2 | 37.8 | .72 | |
| 45–59 | 36.1 | 22.8 | .36** | |
| 60 + | 21.8 | 10.4 | .27*** | |
| Gender (%) | ||||
| Female | 39.0 | 47.6 | 1 | |
| Male | 61.0 | 52.4 | .73 | |
| Education (%) | ||||
| Less than high school | 10.3 | 19.3 | 1 | |
| High school diploma | 37.8 | 24.9 | .42* | |
| Some college, no degree | 23.7 | 25.8 | 0.69 | |
| Associate or bachelor | 22.2 | 21.8 | .63 | |
| degree | ||||
| Graduate degree | 5.9 | 8.2 | 1.16 | |
| Race/Ethnicity (%) | ||||
| White, non-Hispanic | 62.8 | 50.2 | 1 | |
| Black, non-Hispanic | 14.1 | 11.1 | .84 | |
| Other, non-Hispanic | 5.4 | 9.3 | 1.56 | |
| Hispanic | 16.0 | 27.8 | 1.83* | |
| 2+ races, non-Hispanic | 1.7 | 1.7 | 1.10 | |
| Income (%) | ||||
| < 30,000USD | 33.0 | 38.8 | 1 | |
| 30,000–59,999USD | 26.5 | 22.2 | .72 | |
| 60,000–99,999USD | 24.0 | 31.4 | 1.33 | |
| 100,000+ USD | 16.5 | 7.7 | .45* | |
| Household internet access | ||||
| (%) | ||||
| No | 3.2 | 6.5 | 1 | |
| Yes | 96.8 | 93.5 | .36^ | |
| Demographics model | .08 | |||
| Primary substance (%) | .09b | |||
| Alcohol | 51.5 | 48.4 | 1 | |
| Cannabis | 10.4 | 16.0 | 1.27 | |
| Opioids | 5.1 | 6.7 | 1.12 | |
| Other drug | 20.1 | 18.2 | .98 | |
| No responseb | 12.9 | 10.8 | ||
| Complete abstinence (%) | .09 | |||
| No | 47.0 | 59.6 | 1 | |
| Yes | 53.0 | 40.4 | 0.69 | |
| Anti-craving/Anti-relapse | .14 | |||
| medication (%) | ||||
| No | 93.6 | 70.9 | 1 | |
| Yes | 6.3 | 26.7 | 5.58*** | |
| No response | 0.1 | 2.3 | – | |
| Outpatient or inpatient/ | .09 | |||
| residential treatment | ||||
| (%) | ||||
| No | 74.5 | 71.5 | 1 | |
| Yes | 24.7 | 25.8 | 1.31 | |
| No Response | 0.8 | 2.7 | – | |
| Recovery support services | .14 | |||
| (%) | ||||
| No | 80.6 | 49.7 | 1 | |
| Yes | 18.7 | 47.6 | 4.13*** | |
| No response | 0.8 | 2.7 | – | |
| Arrested/drug court | .12 | |||
| involvement (%) | ||||
| Never arrested | 49.6 | 44.0 | 1 | |
| Arrested, no drug court | 44.0 | 32.1 | .88 | |
| Arrested, drug Court | 6.1 | 21.2 | 3.36*** | |
| No response | 0.2 | 2.7 | – | |
| Number of substances | 3.4 (2.6) | 3.6 (2.8) | 1.04 | .09 |
| used M(SD) | ||||
| Age of first substance use | 14.8 (4.5) | 13.2 (4.9) | .93** | .09 |
| M(SD) | ||||
| Psychological distress, M | 4.5 (5.2) | 7.8 (6.0) | 1.08*** | .11 |
| (SD) | ||||
| Quality of life, M(SD) | 29.4 (6.6) | 27.6 (7.1) | .98 | .09 |
| Recovery capital, M(SD) | 47.1 (9.5) | 44.8(11.1) | .99 | .09 |
| Years since problem | 12.3 (11.2) | 8.4 (8.9) | .99 | .08 |
| resolution, M(SD) | ||||
OR = Odds Ratio; CI = Confidence Interval.
p < .05.
p < .01.
p < .001.
p < .07.
Cells with a value of 1 correspond with the reference group for categorical variables.
Pseudo R2 corresponds to the full model predicting ROOT, including the clinical/recovery predictor in a given row, and the set of demographic characteristics (age, gender, education, race/ethnicity, household income, household internet access).
Fig. 1.
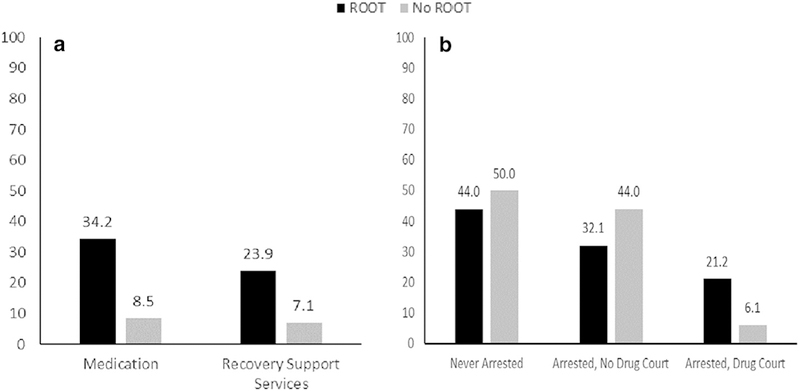
Percentage of participants reporting recovery-related use of online technology (ROOT) or No ROOT as a function of a) lifetime anti-relapse/craving medication and recovery support service use, and b) lifetime criminal justice involvement. Note that non-response to items are not pictured, but are accounted for in proportions displayed (i.e., proportions shown do not add to 100). Also note that in panel a, the “no” responses are implied; for example, 34.2% of the ROOT group had a medication use history (shown) while 65.8% had no medication use history or did not respond to the item (not shown).
3.3. The prediction of self-reported internet addiction from ROOT
The prevalence of “internet addiction” in the entire sample was 4.9% (95% CI: 3.6–6.6), overall, including 12.3% (95% CI: 6.8–21.1) for those with ROOT and 4.0% (95% CI: 2.7–5.7) for those with no ROOT. Controlling for demographic characteristics and significant clinical/ recovery correlates of ROOT from the logistic regression models above, the odds of “internet addiction” were 4.0 times greater for those with ROOT compared to no ROOT (95% CI: 1.7–9.5, p = .001).
4. Discussion
In US adults who resolved a substance use problem, 11% engaged in ROOT. This prevalence estimate suggests 2.5 million U.S. adults have used one or more online technologies to help them “cut down on substance use, abstain from substances, or strengthen their recovery”. Our hypotheses were partially supported, as younger age, and – controlling for demographic characteristics – medication and recovery support service use, and younger age of first substance use were associated with ROOT. Counter to hypotheses, some groups of individuals with more education and higher household income had lower odds of ROOT, while other variables hypothesized to be associated with ROOT had null effects (e.g., outpatient/inpatient specialty treatment).
4.1. Implications of ROOT prevalence
The findings of this cross-sectional epidemiological survey highlight the reach of several types of online technologies, pointing to the need for greater scrutiny of their effectiveness, thereby helping to determine their overall impact on the burden of SUD.
Nearly 7% of the NRS sample engaged with social network sites to support their recovery. Little is known, however, about the nature of individuals’ participation on these sites, and whether they can be effective sources of recovery support. Thus, next steps to build on cross-sectional data including a survey of perceived benefit among participants on a recovery-specific site (Bergman et al., 2017), content analyses of online recovery community posts (D’Agostino et al., 2017), and an assessment of SUD outpatients’ openness to social network site-aided recovery (Ashford et al., 2018), might include longitudinal investigations of social network site-facilitated ROOT. If research shows individuals do, in fact, derive benefit from recovery-specific social network site participation, professional facilitation interventions(Kelly & Bergman, 2016) may be needed to link individuals with these novel resources.
One in 25 NRS participants engaged with online MHOs. Given that face-to-face MHOs are cost-effective resources at the center of many recovery-oriented systems of care (Humphreys et al., 2004; Kelly & Yeterian, 2012), one might hypothesize online MHO meetings also confer benefit, though research is needed to test this assumption. Worth noting is that individuals may access online MHOs via social network sites (Bergman et al., 2017), so these two types of resources are not mutually exclusive.
Finally, this study did not explicitly assess for engagement with non-social network site smartphone applications that help individuals monitor substance use or provide TBI for SUD. That said, one can reasonably assume that the “other” ROOT category – endorsed by 6% of the sample – included these resources given the popularity of smartphones among US adults more generally(Smith, 2017) and SUD treatment seekers more specifically (Dahne & Lejuez, 2015). Importantly, our prior work(Hoeppner et al., 2017) has shown that publicly available smartphone apps intended to address alcohol use rarely include tools to help intervene in real-time (e.g., push notifications based on GPS location). Such innovative tools are thought to explain, in part, the effectiveness of commercially produced apps (Hoeppner et al., 2017). Research on these more accessible, low-cost resources may help empower individuals to choose apps that have been scientifically vetted and are more likely to help them reduce or quit substance use.
4.2. Correlates of ROOT
Younger age was a significant correlate of ROOT, consistent with studies on use of technology in SUD treatment more broadly (Ashford et al., 2018; Dahne & Lejuez, 2015; McClure et al., 2013). Importantly, as might be expected, younger age is related to having resolved a substance use problem more recently, so this effect may simply be an artifact of online technology availability. For those who resolved their problem several years ago, online technologies were less accessible. As the current millennial cohort grows older, however, their propensity to use online technologies to address life challenges like SUD may be similar to their younger counterparts.
Findings that lower levels of education and household income were correlated with ROOT warrant special attention as these effects countered hypotheses based on prior research (Ashford et al., 2018; Dahne & Lejuez, 2015; McClure et al., 2013). One explanation may be that individuals with lower socioeconomic status tend to be limited in the types of services they can access. Perhaps in recognition of these budgetary constraints even if they can access services (i.e., required coinsurance), individuals in lower socioeconomic strata may be on the look-out for free services like those examined in this study. In addition, greater ROOT prevalence among Hispanic compared to White individuals may be explained, in part, by their lower levels of treatment access, attendance, completion, and satisfaction (Guerrero, Marsh, Khachikian, Amaro, & Vega, 2013). Taken together with data showing descriptively higher rates of smartphone as well as Facebook and Instagram use among Hispanic (versus White) individuals (Pew Research Center, 2015; Smith & Anderson, 2018), this suggests they may intuitively compensate for lower engagement with traditional treatment systems by engaging with ROOT. Despite these interesting findings, it is important to highlight that the income and education effects were nonlinear, and only Hispanic ethnicity, but not other racial/ethnic minorities, was a ROOT correlate. Overall, more targeted work is needed to understand the interplay between demography and ROOT.
From the health beliefs model (Finney & Moos, 1995; Rosenstock, 1990), hypotheses that service utilization variables would be associated with ROOT were supported for some (medication and recovery support services) but not all services (inpatient or outpatient treatment). In addition, one could speculate drug court participants had enhanced motivation to meet substance-related targets imposed by the court (e.g., negative toxicology screens) and, therefore, greater willingness to try many different strategies to reach these targets, including the online services examined here. More research is needed to examine whether and why particular SUD services might facilitate ROOT.
In addition to these significant correlates, household internet access (versus no access) was associated with ROOT at a trend (p < .07) level. This trend-level correlate, considered alongside the association between lower household income and ROOT, suggest one’s ability to sustain technology access is a prominent concern. Indeed, prior studies of SUD patients’ technology utilization showed 50–72% had “pay-as-you-go” mobile phone contracts (Dahne & Lejuez, 2015; McClure et al., 2013; Milward et al., 2015). Thus, while individuals with greater challenges may be likely to engage with ROOT, the practical realities of their day-to-day lives could require extra attention. Technology developers may wish to create services accessible by several types of platforms (e.g., website, smartphone application, and text message). If someone derives recovery support from a smartphone application but is temporarily unable to pay for their smartphone, for example, they can access the service via the internet at a library or recovery community center. In addition, systematic effort may be needed to engage individuals with lower severity SUD and/or clinically subthreshold, but nevertheless risky, substance use who are less likely to actively seek out treatment and recovery services. These efforts, for example, might include use of social network sites and other high-volume online spaces to advertise recovery-related online services (Ashford et al., 2018), as well as collaborations with health care gatekeepers, such as primary care providers, who can actively refer patients to engage with these resources.
4.3. ROOT and “internet addiction”
In determining the potential utility of health care services and resources, benefits must be weighed against risks (or side effects), and contextualized within the burden of the problem. Since we focused on lifetime ROOT and perceived internet addiction in this study, it cannot be determined whether internet addiction occurred while an individual was engaging in ROOT. Nevertheless, those with ROOT had four times greater odds of internet addiction, over and above demographic characteristics and clinical variables associated with ROOT like current psychological distress. As such, researchers studying ROOT and TBI in longitudinal work may wish to assess unhealthy use of the internet and social media over time (e.g., Bergen Social Media Addiction Scale; Andreassen, Pallesen, & Griffiths, 2017). With greater work in this area, potential risks may be considered alongside benefits offered by well-designed, theoretically-grounded interventions and services that leverage online technology platforms (Fowler et al., 2016; Litvin et al., 2013; Marsch, 2012; Sugarman et al., 2017).
4.4. Limitations
Chief among study limitations was that temporal precedence (Hill, 1965), and therefore causality, cannot be established, as is the case in all cross-sectional survey research. Second, survey items measuring use of online technology queried lifetime ROOT, thus it is unclear if ROOT corresponded with the most recent episode of problem resolution. Third, items asked broadly about use of technology, thus the specific reasons for which individuals used online technology (e.g., to access social support, to access recovery-related information, etc.) cannot be determined. Fourth, the item querying “other” online resources included smartphones as one potential resource, though individuals did not explicitly indicate smartphone use. A complicating factor is that social network sites are accessible (sometimes exclusively) via smartphone apps. Given the possibility that participants may have been confused by this distinction, analyses emphasized ROOT more generally, rather than separate online resources. Finally, we determined history of internet addiction from participant response to an item querying problem behaviors used in prior recovery research (Laudet et al., 2015). The item did not define internet addiction for participants, however. We emphasize the unprecise nature of such self-diagnosis with quotations around the term, and treat the analyses involving this construct and its implications as hypothesis-generating rather than hypothesis-testing.
5. Conclusion
More than one in ten US adults who resolved a substance use problem engaged in ROOT. Individuals working to reduce or quit substance use with greater clinical severity and psychosocial challenges may be naturally open to using online technologies to bolster their efforts. Future research may help identify the types of online services that enhance substance use outcomes and the individuals for whom they work best. These resources may then be added to help potentiate benefit individuals have derived from other SUD treatment and recovery supports, while also attracting those experiencing substance-related harms but do not want, or believe they need, formal services. Ultimately, therefore, studies that evaluate ROOT may lead to greater identification of empirically-supported resources with immense reach that can be confidently integrated into recovery-oriented systems of care.
HIGHLIGHTS.
11% with a former substance problem report recovery-related use of online technology (ROOT)
Controlling for demographics, clinical severity indicators were ROOT correlates
Controlling for demographics and ROOT correlates, ROOT was associated with “internet addiction”.
References
- Andreassen CS, Pallesen S, & Griffiths MD (2017). The relationship between addictive use of social media, narcissism, and self-esteem: Findings from a large national survey. Addictive Behaviors, 64, 287–293. http://dx.doi.org/10.10167j.addbeh.2016.03.006. [DOI] [PubMed] [Google Scholar]
- Andreassen CS, Torsheim T, Brunborg GS, & Pallesen S (2012). Development of a Facebook addiction scale. Psychological Reports, 110(2), 501–517. 10.2466/02.09.18.pr0.110.2.501-517. [DOI] [PubMed] [Google Scholar]
- Ashford DR, Lynch K, & Curtis B (2018). Technology and social media use among patients enrolled in outpatient addiction treatment programs: Cross-sectional survey study. Journal of Medical Internet Research, 20(3), e84 10.2196/jmir.9172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battaglia MP, Hoaglin DC, & Frankel MR (2009). Practical considerations in raking survey data. Survey Practice.\ 2(5), 1–10. [Google Scholar]
- Bergman BG, Kelly NW, Hoeppner BB, Vilsaint CL, & Kelly JF (2017). Digital recovery management: Characterizing recovery-specific social network site participation and perceived benefit. Psychology of Addictive Behaviors, 31(4), 506–512. 10.1037/adb0000255. [DOI] [PubMed] [Google Scholar]
- Brown SA, Myers MG, Lippke L, Tapert SF, Stewart DG, & Vik PW (1998). Psychometric evaluation of the customary drinking and drug use record (CDDR): A measure of adolescent alcohol and drug involvement. Journal of Studies on Alcohol, 59(4), 427–438. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Nuro KF, ... Rounsaville BJ (2008). Computer-assisted delivery of cognitive-behavioral therapy for addiction: a randomized trial of CBT4CBT. The American Journal of Psychiatry, 165(7), 881–888. 10.1176/appi.ajp.2008.07111835 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) (2018). Provisional counts of drug overdose deaths, as of 8/6/2017. [cited 2018 March 7]. Available from: https://www.cdc.gov/nchs/data/health_policy/monthly-drug-overdose-death-estimates.pdf.
- D’Agostino AR, Optican AR, Sowles SJ, Krauss MJ, Escobar Lee K, & Cavazos-Rehg PA (2017). Social networking online to recover from opioid use disorder: A study of community interactions. Drug and Alcohol Dependence, 181, 5–10. 10.1016/j.drugalcdep.2017.09.010 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahne J, & Lejuez CW (2015). Smartphone and mobile application utilization prior to and following treatment among individuals enrolled in residential substance use treatment. Journal of Substance Abuse Treatment, 58, 95–99. 10.1016/j.jsat.2015.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallery J, Jarvis B, Marsch L, & Xie H (2015). Mechanisms of change associated with technology-based interventions for substance use. Drug and Alcohol Dependence, 150, 14–23. 10.1016/j.drugalcdep.2015.02.036 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Titus JC, White MK, Unsicker J, Hodgkins D. Global appraisal of individual needs: Administration guide for the GAIN and related measures. Bloomington, IL: Chestnut Health Systems. Available at www.chestnut.org/li/gain/gadm1299.pdf.;2002. [Google Scholar]
- Elhai JD, Dvorak RD, Levine JC, & Hall BJ (2017). Problematic smartphone use: A conceptual overview and systematic review of relations with anxiety and depression psychopathology. Journal of Affectve Disorders, 207, 251–259. 10.1016/j.jad.2016.08.030. [DOI] [PubMed] [Google Scholar]
- Finney JW, & Moos RH (1995). Entering treatment for alcohol abuse: A stress and coping model. Addiction, 90(9), 1223–1240. 10.1111/jM360-0443.1995.tb01092.x. [DOI] [PubMed] [Google Scholar]
- Fowler LA, Holt SL, & Joshi D (2016). Mobile technology-based interventions for adult users of alcohol: A systematic review of the literature. Addictive Behaviors, 62, 25–34. 10.1016/j.addbeh.2016.06.008. [DOI] [PubMed] [Google Scholar]
- GfK, 2013. KnowledgePanel Design Summary (Available from:) http://www.knowledgenetworks.com/knpanel/docs/knowledgepanel(R)-design-summarydescription.pdf. [Google Scholar]
- Glasgow RE, Klesges LM, Dzewaltowski DA, Estabrooks PA, & Vogt TM (2006). Evaluating the impact of health promotion programs: Using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Education Research, 21(5), 688–694. 10.1093/her/cyl081. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Mckay HG, Piette JD, & Reynolds KD (2001). The RE-AIM framework for evaluating interventions: What can it tell us about approaches to chronic illness management? Patient Education and Counseling, 44, 119–127. 10.1016/S0738-3991(00)00186-5. [DOI] [PubMed] [Google Scholar]
- Gonzales R, Ang A, Murphy DA, Glik DC, & Anglin MD (2014). Substance use recovery outcomes among a cohort of youth participating in a mobile-based texting aftercare pilot program. Journal of Substance Abuse Treatment, 47(1), 20–26. 10.1016/j.jsat.2014.01.010 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groshkova T, Best D, & White W (2012). The assessment of recovery capital: Properties and psychometrics of a measure of addiction recovery strengths. Drug and Alcohol Review. 10.1111/j.1465-3362.2012.00489.x. [DOI] [PubMed] [Google Scholar]
- Guerrero EG, Marsh JC, Khachikian T, Amaro H, & Vega WA (2013). Disparities in Latino substance use, service use, and treatment: Implications for culturally and evidence-based interventions under health care reform. Drug and Alcohol Dependence, 133(3), 805–813. 10.1016/j.drugalcdep.2013.07.027. [DOI] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Chih MY, Atwood AK, Johnson RA, Boyle MG, ... Shah D (2014). A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA Psychiatry, 71 (5), 566–572. 10.1001/jamapsychiatry.2013.4642 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeren T, Edwards EM, Dennis JM, Rodkin S, Hingson RW, & Rosenbloom DL (2008). A comparison of results from an alcohol survey of a prerecruited internet panel and the National Epidemiologic Survey on alcohol and related conditions. Alcoholism, Clinical and Experimental Research, 32(2), 222–229. 10.1111/j.1530-0277.2007.00571.x. [DOI] [PubMed] [Google Scholar]
- Hill AB (1965). The environment and disease: Association or causation? Proceedings of the Royal Society of Medicine, 58(5), 295–300. [PMC free article] [PubMed] [Google Scholar]
- Hoeppner BB, Schick MR, Kelly LM, Hoeppner SS, Bergman B, & Kelly JF (2017). There is an app for that - or is there? A content analysis of publicly available smartphone apps for managing alcohol use. Journal of Substance Abuse Treatment, 82, 67–73. 10.1016/j.jsat.2017.09.006. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Wing S, Mccarty D, Chappel J, Gallant L, Haberle B, ... Weiss R (2004). Self-help organizations for alcohol and drug problems: Toward evidence-based practice and policy. Journal of Substance Abuse Treatment, 26, 151–158. 10.1016/S0740-5472(03)00212-5. [DOI] [PubMed] [Google Scholar]
- Institute of Behavioral Research. TCU Comprehensive Intake (TCU CI). Fort Worth, TX: Texas Christian University, Institute of Behavioral Research; Available at ibr.tcu.edu; 2002. [Google Scholar]
- Kelly JF, & Bergman BG (2016). Twelve-step mutual-help organizations and facilitation interventions. In Mistral W (Ed.). Action on addiction: Integrated approaches to drug and alcohol problems (pp. 169–181). London, UK: Routledge. [Google Scholar]
- Kelly JF, Bergman BG, Hoeppner BB, Vilsaint CL, & White WL (2017). Prevalence and pathways of recovery from drug and alcohol problems in the United States population: Implications for practice, research, and policy. Drug and Alcohol Dependence, 181 (Supplement C), 162–169. 10.1016/j.drugalcdep.2017.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Greene MC, & Bergman BG (2017). Is recovery from cannabis use problems different from alcohol and other drugs? Results from a national probability-based sample of the United States adult population. The International Journal on Drug Policy, 53, 55–64. http://dx.doi.org/10.1016Zj.drugpo.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Greene MC, & Bergman BG (2018). Beyond abstinence: Changes in indices of quality of life with time in recovery in a nationally representative sample of u.s. adults. Alcoholism, Clinical and ExperimentalResearch. 10.1111/acer.13604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Urbanoski KA, Hoeppner BB, & Slaymaker V (2011). Facilitating comprehensive assessment of 12-step experiences: A multidimensional measure of mutual-help activity. Alcoholism Treatment Quarterly, 29(3), 181–203. 10.1080/07347324.2011.586280 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, & Yeterian JD (2012). Empirical awakening: The new science on mutual help and implications for cost containment under health care reform. Substance Abuse, 33, 85–91. 10.1080/08897077.2011.634965. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, ... Zaslavsky AM (2003). Screening for serious mental illness in the general population. Archives of General Psychiatry, 60(2), 184–189. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Hatzenbuehler ML, Mclaughlin KA, Link B, Olfson M, Grant BF, & Hasin D (2010). Stigma and treatment for alcohol disorders in the United States. American Journal of Epidemiology, 172(12), 1364–1372. 10.1093/aje/kwq304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuss DJ, Griffiths MD, Karila L, & Billieux J (2014). Internet addiction: A systematic review of epidemiological research for the last decade. Current Pharmaceutical Design, 20(25), 4026–4052. [DOI] [PubMed] [Google Scholar]
- Laudet AB, Harris K, Kimball T, Winters KC, & Moberg DP (2015). Characteristics of students participating in collegiate recovery programs: a national survey. Journal of Substance Abuse Treatment, 51, 38–46. 10.1016/j.jsat.2014.11.004 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litvin EB, Abrantes AM, & Brown RA (2013). Computer and mobile technology-based interventions for substance use disorders: An organizing framework. Addictive Behaviors, 38(3), 1747–1756. http://dx.doi.org/10.1016Zj.addbeh.2012.09.003. [DOI] [PubMed] [Google Scholar]
- Marsch LA (2012). Leveraging technology to enhance addiction treatment and recovery. Journal of Addictive Diseases, 31(3), 313–318. 10.1080/10550887.2012.694606 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsch LA, Guarino H, Acosta M, Aponte-Melendez Y, Cleland C, Grabinski M, ... Edwards J (2014). Web-based behavioral treatment for substance use disorders as a partial replacement of standard methadone maintenance treatment. Journal of Substance Abuse Treatment, 46(1), 43–51. 10.1016/j.jsat.2013.08.012 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure EA, Acquavita S, Harding E, & Stitzer M (2013). Utilization of communication technology by patients enrolled in substance abuse treatment. Drug and Alcohol Dependence, 129(1–2), 145–150. 10.1016/j.drugalcdep.2012.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, & Del Boca FK (1994). Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol, Supplement 12, 112–118. [DOI] [PubMed] [Google Scholar]
- Milward J, Day E, Wadsworth E, Strang J, & Lynskey M (2015). Mobile phone ownership, usage and readiness to use by patients in drug treatment. Drug and Alcohol Dependence, 146(Supplement C), 111–115. 10.1016/j.drugalcdep.2014.11.001. [DOI] [PubMed] [Google Scholar]
- National Drug Intelligence Center (2011). The Economic Impact of Illicit Drug Use on American Society. Washington D.C: United States Department of Justice. [Google Scholar]
- Onken L, & Shoham V (2015). Technology and the stage model of behavioral intervention development In Marsch LA, Lord SE, & Dallery J (Eds.). Behavioral healthcare and technology: Using science-based innovations to transform practice (pp. 3–12). New York, NY: Oxford University Press. [Google Scholar]
- Park-Lee E, Lipari RN, Hedden SL, Kroutil LA, & Porter JD (2017). Receipt of services for substance use and mental health issues among adults: Results from the 2016 national survey on drug use and health. NSDUH data review. Retrieved from http://www.samhsa.gov/data/.2017. [PubMed] [Google Scholar]
- Pew Research Center (2015). The smartphone difference. [cited 2016 February 20]. Available from: http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/.
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, & Patra J (2009). Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet, 373(9682), 2223–2233. 10.1016/s0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Ridout B, & Campbell A (2014). Using Facebook to deliver a social norm intervention to reduce problem drinking at university. Drug and Alcohol Review, 33(6), 667–673. 10.1111/dar.12141. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM (1990). The health belief model: Explaining health behavior through expectancies In Glanz K, Lewis FM, & Rimer BK (Eds.). Health behavior and health education: Theory, research, and practice; (pp. 39–62). San Francisco, CA US: Jossey-Bass. [Google Scholar]
- Schmidt S, Muhlan H, & Power M (2006). The EUROHIS-QOL 8-item index: Psychometric results of a cross-cultural field study. European Journal of Public Health, 16(4), 420–428. 10.1093/eurpub/cki155. [DOI] [PubMed] [Google Scholar]
- Smith A (2017). Record Shares of Americans Now Own Smartphones, Have Home Broadband: Pew Research Center. [cited 2018 March 7]. Available from: www.pewresearch.org/fact-tank/2017/01/12/evolution-of-technology/. [Google Scholar]
- Smith A, & Anderson M (2018). Social media use in 2018: Pew research center. [cited march 14 2018]. Available from: http://assets.pewresearch.org/wp-content/uploads/sites/14/2018/03/01105133/PI_2018.03.01_Social-Media_FINAL.pdf. [Google Scholar]
- Stahre M, Roeber J, Kanny D, Brewer RD, & Zhang X (2014). Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Preventing Chronic Disease, 11(E109), 10.5888/pcd11.130293 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp (2015). Stata statistical software: Release 14. [computer program]. College Station, TX: StataCorp LP. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2016 national survey on drug use and health (HHS publication No. SMA 17–5044, NSDUH series H-52). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; Retrieved from http://www.samhsa.gov/data/.2017. [Google Scholar]
- Sugarman DE, Campbell ANC, Iles BR, & Greenfield SF (2017). Technology- based interventions for substance use and comorbid disorders: An examination of the emerging literature. Harvard Review of Psychiatry, 25(3), 123–134. 10.1097/hrp.0000000000000148 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau (2015). Current population survey (CPS). Available from: https://www.census.gov/programs-surveys/cps/about.html.
- Vilsaint CL, Kelly JF, Bergman BG, Groshkova T, Best D, & White W (2017). Using item response theory to develop and validate a 10-item brief assessment of recovery capital (BARC-10) for alcohol and other drug use disorders. Drug and Alcohol Dependence, 17, 71–76. 10.1016/j.drugalcdep.2017.03.022. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Koob GF, & McLellan AT (2016). Neurobiologic advances from the brain disease model of addiction. The New England Journal of Medicine, 374(4), 363–371. 10.1056/NEJMra1511480. [DOI] [PMC free article] [PubMed] [Google Scholar]


