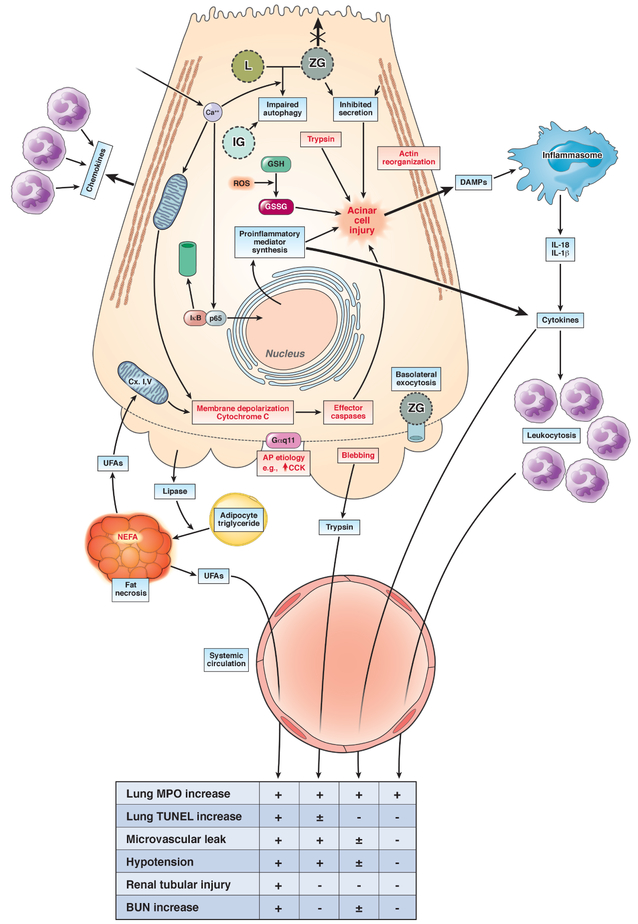
Figure 2: Pathophysiology of systemic injury in AP:
The upper part of the figure describes the initiation of acinar injury by an AP etiology like high dose CCK (↑CCK) during caerulein pancreatitis. The intra-acinar signaling events include the increase in cytosolic calcium (Ca2+), which has a role in mitochondrial depolarization (Memb. Depol.) and cytochrome C leakage, along with activating NF-kB via dissociation and proteasomal degradation of IkB, nuclear translocation of p65. This upregulates inflammatory mediator synthesis, which include cytokines and chemokines, and thus leads to neutrophil infiltration into the pancreas. The trypsin generated due to impaired autophagy involving lysosomes (L) and zymogen granules (ZG) and increased oxidized glutathione (GSSG) [from its reduced form (GSH), due to reactive oxygen species (ROS)], along with concurrent deleterious mechanisms, cause acinar injury. These other mechanisms include the loss of apical microvilli, inhibition of apical secretion, the reorganization of F-actin, basolateral blebbing, release of DAMPs that can activate the inflammasome, and leakage of exocrine enzymes such as lipase, trypsin. The DAMPS can worsen local injury, and may also contribute to systemic injury. Similarly, cytokines can cause the leukocytosis associated with SIRS, which can enter the systemic circulation and are a part of systemic injury. The lower part of the figure describes the types of systemic injury that may occur due to these, along with the underlying mechanisms. The mechanisms include unregulated hydrolysis of adipocyte triglyceride (Adipo. TG) by pancreatic lipase, resulting in fat necrosis, which generates UFAs, that inhibit mitochondrial complex I and V, which decrease ATP and worsen local injury. The effects of UFAs, trypsin, cytokine entry into the systemic circulation, and leukocytosis (from left to right) on end points of systemic injury are mentioned in the table below, with a + indicating 2 or more reports citing the agent in causing the end point. Unclear or weaker evidence is shown as ± or a – respectively.