Abstract
Background
The relevance of transthoracic impedance (TTI) to electrical cardioversion (ECV) success for atrial tachyarrhythmias when using biphasic waveform defibrillators is unknown.
Hypothesis
TTI is predictive of ECV success with contemporary defibrillators.
Methods
De‐identified data stored in biphasic defibrillator memory cards from ECV attempts for atrial fibrillation (AF) or atrial flutter (AFL) over a 2‐year period at our center were evaluated. ECV success, defined as arrhythmia termination and ≥ 1 sinus beat, was adjudicated by 2 blinded cardiac electrophysiologists. The association between TTI and ECV success was assessed via Cochrane‐Armitage trend and Spearman rank correlation tests, as well as simple and multivariable logistic regression. The influence of TTI on the number of shocks and on cumulative energy delivered per patient was also examined.
Results
703 patients (593 with AF, 110 with AFL) receiving 1055 shocks were included. Last shock success was achieved in 88.0% and 98.2% of patients with AF and AFL, respectively. In patients with AF, TTI was positively associated with last shock failure (P trend =0.019), the need for multiple shocks (P trend <0.001), and cumulative energy delivered (ρ = 0.348; P < 0.001). After adjusting for first shock energy, 10‐Ω increments in TTI were associated with odds ratios of 1.36 (95% CI: 1.24–1.49) and 1.22 (95% CI: 1.09–1.37) for first and last shock failure, respectively (P < 0.001 for both).
Conclusions
Although contemporary defibrillators are designed to compensate for TTI, this variable continues to be associated with ECV failure in patients with AF. Strategies to lower TTI during ECV for AF may improve procedural success.
Keywords: Atrial Fibrillation, Cardioversion, Defibrillation, General Clinical Cardiology/Adult
1. INTRODUCTION
Synchronized electrical cardioversion (ECV) is considered a safe and effective method to restore sinus rhythm in patients with atrial fibrillation (AF) or atrial flutter (AFL), thanks in part to advances in defibrillator technology.1, 2, 3, 4 Contemporary defibrillators deliver impedance‐compensated biphasic waveforms that adjust the shock waveform based on the patient's transthoracic impedance (TTI).5, 6 This technology has superseded previous generations of monophasic waveform devices, as it has demonstrated comparable ECV success rates at lower energies and therefore with a lower risk of tissue injury.1, 2, 7
TTI has long been considered an important predictor of ECV success by influencing the current fraction that reaches the myocardium.7, 8, 9 However, though strategies to modify TTI during ECV attempts continue to be endorsed in current guidelines,3 its importance in the era of impedance‐compensated biphasic defibrillators is unclear, with some data suggesting that its influence may be negligible.5, 10 We therefore sought to explore the relevance of TTI on AF and AFL ECV success using contemporary defibrillators. We hypothesized that TTI continues to be associated with ECV failure in patients with atrial tachyarrhythmias.
2. METHODS
2.1. Patient selection, data collection, and study outcomes
All patients undergoing ECV for AF or AFL over a 2‐year period at the University of Ottawa Heart Institute were included. De‐identified data stored in Philips HeartStart XL and HeartStart MRx defibrillators were downloaded using HeartStart Event Review Pro (Philips Healthcare, Andover, MA), including electrocardiograms, number of shocks delivered, energy per shock, and TTI. All rhythm strips were reviewed by 2 cardiac electrophysiologists blinded to the patient's TTI to confirm the baseline rhythm and to determine whether shocks were successful. A shock was considered successful if it terminated the arrhythmia and resulted in ≥1 sinus beat. Otherwise, the shock was considered to have failed.
The primary outcome measure was last‐shock success. Secondary outcomes included first‐shock success, the number of shocks delivered, and the cumulative energy delivered. The study was approved by the Ottawa Health Science Network Research Ethics Board as an institutional quality‐improvement initiative and was in accordance with the Declaration of Helsinki.
2.2. Statistical analysis
Categorical data are reported as frequency and percentage, and continuous variables as mean ±SD. Analyses of AFL ECV failures were limited due to the small number of events. In patients with AF, associations of first‐shock TTI with last‐shock success and with the need for multiple shocks were assessed via t tests and Cochran‐Armitage trend tests. The association between TTI and the cumulative shock energy delivered was assessed using the Spearman rank correlation coefficient. Individual shock success stratified by shock‐specific TTI was also examined. TTI was divided into quartiles for these analyses. Given the possibility that differences in starting energy and shock energy escalation could influence outcomes, a sensitivity analysis restricted to patients who received a first shock of ≥150 J was performed, as this starting energy has been recommended by others and has been associated with ECV success rates of ≥80%.7, 10 Simple and multivariable logistic regression models were fit to estimate the influence of TTI on last‐shock success, first‐shock success, the need for ≥3 shocks, and cumulative energy delivery in the top quartile of the AF cohort. Odds ratios (ORs) are provided with 95% confidence intervals (CIs). All analyses were performed using SAS software, version 9.4 (SAS Institute, Inc., Cary, NC). Statistical significance was defined as an α level < 0.05 (2‐tailed).
3. RESULTS
3.1. Electrical cardioversion outcomes
In total, 703 patients undergoing ECV for AF or AFL were included (593 with AF and 110 with AFL; Figure 1). In the AFL cohort, first‐shock failure occurred in 5 patients (4.5%) and last‐shock failure in 2 (1.8%), precluding detailed analyses of predictors of ECV failure. In the AF cohort, first‐shock and last‐shock failure were observed in 183 and 71 patients (30.9% and 12.0%), respectively (Table 1). The TTI associated with the first shock ranged from 26 Ω to 146 Ω in patients with AF.
Figure 1.
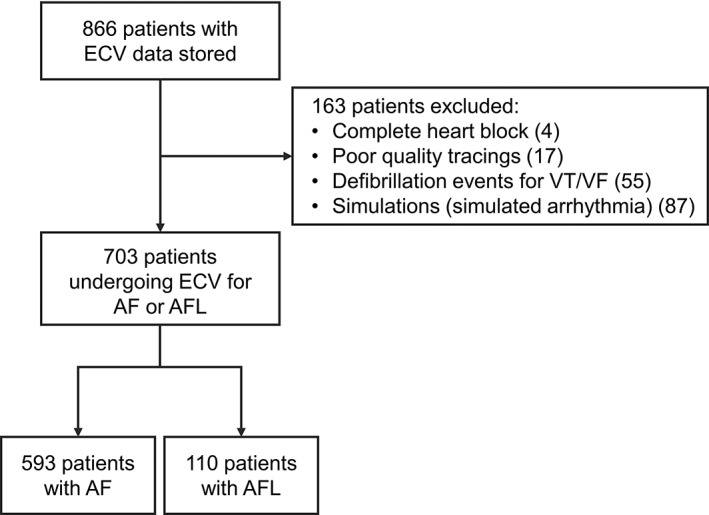
ECV case selection. Abbreviations: AF, atrial fibrillation; AFL, atrial flutter; ECV, electrical cardioversion; VF, ventricular fibrillation; VT, ventricular tachycardia
Table 1.
Details of ECV attempts
| AF, n = 593 | AFL, n = 110 | |
|---|---|---|
| No. of shocks | 1.6 ± 0.9 | 1.1 ± 0.4 |
| Starting energy delivered, J | 147.7 ± 50.0 | 131.5 ± 56.0 |
| Cumulative energy delivered, J | 249.1 ± 166.3 | 149.0 ± 76.1 |
| First shock TTI, Ω | 73.6 ± 20.7 | 76.6 ± 22.6 |
| First shock success | 410 (69.1) | 105 (95.5) |
| Last shock success | 522 (88.0) | 108 (98.2) |
Abbreviations: AF, atrial fibrillation; AFL, atrial flutter; ECV, electrical cardioversion; SD, standard deviation; TTI, transthoracic impedance.
Data are presented as n (%) or mean ±SD.
3.2. Association between TTI and procedural success
Among patients with AF, patients with last‐shock failure had a higher mean first‐shock TTI compared with those with successful last shocks (81.2 ±25.3 vs 72.5 ±19.7 Ω; P = 0.007). Dividing the AF cohort into quartiles based on first‐shock TTI indicated a graded relationship whereby higher TTI was associated lower last‐shock success, higher likelihood of requiring multiple shocks, and higher cumulative energy delivered (Figure 2A–C). Restricting this analysis to patients who received first shocks of ≥150 J found similar associations (n = 344; Figure 2D–F). The findings were also similar in analyses of individual‐shock and shock‐specific TTIs (931 shocks; Figure 3).
Figure 2.
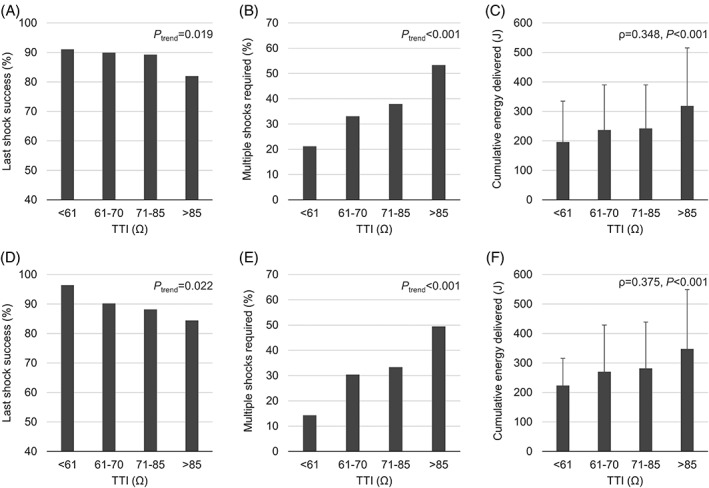
Associations between TTI and (A,D) last shock success, (B,E) the need for multiple shocks, and (C,F) cumulative shock energy delivered in patients with AF. Panels A–C depict data for all patients (n = 593); panels D–F depict data for patients with first shock energies of ≥150 J only (n = 344). ρ denotes Spearman's rank correlation. Error bars represent SD. Abbreviations: AF, atrial fibrillation; SD, standard deviation; TTI, transthoracic impedance
Figure 3.
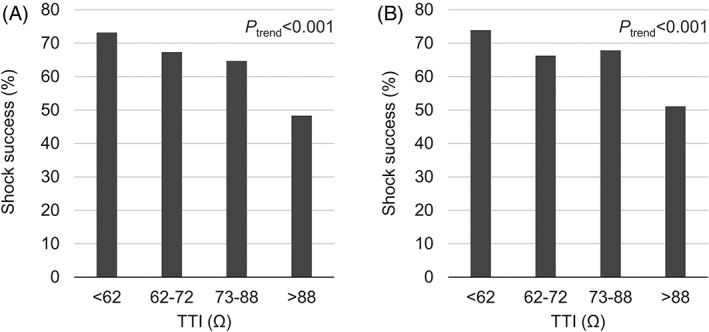
Association between shock‐specific TTI and individual shock success for AF, showing (A) all shocks (n = 931) and (B) all shocks ≥150 J (n = 622). Abbreviations: AF, atrial fibrillation; TTI, transthoracic impedance
Unadjusted regression analyses confirmed that each 10‐Ω increment in TTI was associated with an OR of 1.21 for last‐shock failure in patients with AF (P = 0.001), which was comparable when adjusted for first‐shock energy. Similarly, each 10‐Ω increment in TTI was associated with greater odds of first‐shock failure, of requiring ≥3 shocks, and of receiving ≥324 J of cumulative energy (corresponding to the highest quartile of cumulative energy delivered in the sample) in both simple and multivariable models (P < 0.001 for all; Table 2).
Table 2.
Crude and adjusted associations between TTI and ECV outcomes, per 10‐Ω increment
| Crude OR (95% CI) | P Value | Adjusted OR (95% CI)a | P Valuea | |
|---|---|---|---|---|
| Last shock failure | 1.21 (1.08–1.36) | 0.001 | 1.22 (1.09–1.37) | <0.001 |
| First shock failure | 1.33 (1.21–1.45) | <0.001 | 1.36 (1.24–1.49) | <0.001 |
| ≥3 shocks required | 1.21 (1.09–1.34) | <0.001 | 1.23 (1.11–1.36) | <0.001 |
| Cumulative energy ≥324 J | 1.29 (1.18–1.42) | <0.001 | 1.28 (1.17–1.41) | <0.001 |
Abbreviations: CI, confidence interval; ECV, electrical cardioversion; OR, odds ratio; TTI, transthoracic impedance.
Adjusted for starting energy level.
4. DISCUSSION
TTI is considered a determinant of ECV success based primarily on studies using outdated monophasic waveform defibrillators. Contemporary impedance‐compensating biphasic defibrillators have demonstrated greater shock efficacy. Whether TTI is clinically relevant in current practice is therefore unclear. Our analysis of ECV attempts for atrial tachyarrhythmias over a 2‐year period at our center suggest that ECV success and shock efficacy are high in patients with AFL. In contrast, in patients with AF, high TTI continues to identify those in whom ECV is more likely to require more shocks, to require greater energy delivery, and ultimately to fail. Our results are consistent with findings from a smaller study by Fumagalli et al., which suggested an association between high TTI and the need for multiple shocks in 80 patients with AF undergoing ECV using a pulsed biphasic waveform.11
A minimum transcardiac current density is required during ECV attempts for successful cardioversion/defibrillation.12 However, this current is estimated to be as small as 4% of the total applied during ECV attempts, with most of the current shunted around the heart.13 TTI is a measure of the resistance to current across the body, including cardiac and noncardiac structures. The relative contributions of effective transcardiac and ineffective noncardiac current pathways to TTI are poorly understood, as are the relative changes in transcardiac current density when TTI is modified.5, 14 Nevertheless, the negative association between TTI and ECV success observed with monophasic defibrillators suggests that a higher transthoracic current is associated with a higher transcardiac current.10, 14, 15 Contemporary defibrillators deliver biphasic shocks and modify their waveforms in response to the measured TTI. Indeed, in contrast to studies using monophasic shocks, 2 publications reporting on biphasic waveforms in patients with ventricular tachyarrhythmias found that TTI was not predictive of shock success.5, 10
Several potential explanations exist for the discrepancy between our conclusions and those of others. First, we investigated the association between TTI and ECV outcomes in patients with AF and AFL and analyzed outcomes separately for each arrhythmia. White et al. found that the influence of TTI on shock success was negligible, but they studied this association in cardiac arrest patients with shockable rhythms (either VT or VF).5 It is possible that shock efficacy is greater in macro‐reentrant arrhythmias with more easily intercepted singular wavefronts, as suggested by the high success seen in patients with AFL in our analysis, and therefore that differences may have been noted in their analysis if outcomes were stratified by type of arrhythmia. Furthermore, atrial and ventricular tachyarrhythmias generally differ substantially in their duration. It is increasingly recognized that AF can induce structural and electrical changes in the atrial substrate that promote the recurrence and perpetuation of the arrhythmia.16, 17, 18 The chronicity of AF could plausibly render it more refractory to shocks than acute ventricular arrhythmias.19 Our sample size may have also afforded greater power to detect small differences in the study outcomes. Differences in patient characteristics, patient preparation (including electrode placement and therefore shock vectors), starting energy, and in defibrillators used may have also contributed to differences observed.10, 15, 20, 21, 22
4.1. Study limitations
There are several important limitations to our study. Given the de‐identified nature of the data, we were unable to account for patient and procedural characteristics that could confound or modify the associations between TTI and ECV outcomes. For instance, certain anthropometric measures may explain the relationships observed.11, 20, 23 Nevertheless, TTI would still be a marker of patients in whom ECV outcomes are suboptimal. Though our data are from a single center, the considerable variability in starting energy and shock energy escalation suggests nonuniform practices, which is consistent with the variability in ECV techniques seen at other centers.24 Furthermore, our findings were similar in sensitivity analyses restricted to patients who received ≥150 J for their first shock, which has been the suggested starting energy by others.7, 10 We used data from biphasic truncated exponential (BTE) waveform defibrillators only. Whether similar findings would have been observed with other waveforms is unknown. A recent network meta‐analysis found equal ECV efficacy between BTE and rectilinear biphasic waveforms25; however, a small study has suggested that ECV using a pulsed biphasic waveform may be less effective than BTE.22
5. CONCLUSION
In patients undergoing ECV for AF with contemporary biphasic defibrillators, higher TTI was associated with worse ECV outcomes, including a greater number of shocks, greater cumulative energy requirements, and procedural failure. American guidelines suggest applying pressure to electrodes to reduce TTI3; however, few physicians know to do this even when using handheld paddles,20 and there is no protocol that has been agreed upon for routine AF ECV. Whether strategies to reduce TTI during AF ECV with biphasic defibrillators can improve procedural success is unknown and warrants further study. We recently initiated a study using a stepwise protocol that incorporates applying pressure to electrodes to reduce TTI, which may serve to improve ECV practice (http://www.ClinicalTrials.gov NCT02192957).
Conflicts of interest
DHB was supported by the University of Ottawa Heart Institute Leadership Chair in Electrophysiology and the Tier 1 University of Ottawa Chair in Electrophysiology Research. The authors declare no other potential conflicts of interest.
Sadek MM, Chaugai V, Cleland MJ, Zakutney TJ, Birnie DH, Ramirez FD. Association between transthoracic impedance and electrical cardioversion success with biphasic defibrillators: An analysis of 1055 shocks for atrial fibrillation and flutter. Clin Cardiol. 2018;41:666–670. 10.1002/clc.22947
Mouhannad M. Sadek, MD, and Varsha Chaugai, MEng, contributed equally to this work.
REFERENCES
- 1. Mittal S, Ayati S, Stein KM, et al. Transthoracic cardioversion of atrial fibrillation: comparison of rectilinear biphasic versus damped sine wave monophasic shocks. Circulation. 2000;101:1282–1287. [DOI] [PubMed] [Google Scholar]
- 2. Page RL, Kerber RE, Russell JK, et al; BiCard Investigators. Biphasic versus monophasic shock waveform for conversion of atrial fibrillation: the results of an international randomized, double‐blind multicenter trial. J Am Coll Cardiol. 2002;39:1956–1963. [DOI] [PubMed] [Google Scholar]
- 3. January CT, Wann LS, Alpert JS, et al; ACC/AHA Task Force Members . 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Heart Rhythm Society [published correction appears in Circulation. 2014;130:e270–e271]. Circulation. 2014;130:2071–2104. [DOI] [PubMed] [Google Scholar]
- 4. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893–2962. [DOI] [PubMed] [Google Scholar]
- 5. White RD, Blackwell TH, Russell JK, et al. Transthoracic impedance does not affect defibrillation, resuscitation or survival in patients with out‐of‐hospital cardiac arrest treated with a non‐escalating biphasic waveform defibrillator. Resuscitation. 2005;64:63–69. [DOI] [PubMed] [Google Scholar]
- 6. Koninklijke Philips Electronics , N.V. HeartStart MRx service manual. 2005.
- 7. Adgey AA, Walsh SJ. Theory and practice of defibrillation: (1) atrial fibrillation and DC conversion. Heart. 2004;90:1493–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sado DM, Deakin CD. How good is your defibrillation technique? J R Soc Med. 2005;98:3–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kerber RE, Grayzel J, Hoyt R, et al. Transthoracic resistance in human defibrillation: influence of body weight, chest size, serial shocks, paddle size and paddle contact pressure. Circulation. 1981;63:676–682. [DOI] [PubMed] [Google Scholar]
- 10. Walsh SJ, McCarty D, McClelland AJ, et al. Impedance compensated biphasic waveforms for transthoracic cardioversion of atrial fibrillation: a multi‐centre comparison of antero‐apical and antero‐posterior pad positions. Eur Heart J. 2005;26:1298–1302. [DOI] [PubMed] [Google Scholar]
- 11. Fumagalli S, Boni N, Padeletti M, et al. Determinants of thoracic electrical impedance in external electrical cardioversion of atrial fibrillation. Am J Cardiol. 2006;98:82–87. [DOI] [PubMed] [Google Scholar]
- 12. Zipes DP, Fischer J, King RM, et al. Termination of ventricular fibrillation in dogs by depolarizing a critical amount of myocardium. Am J Cardiol. 1975;36:37–44. [DOI] [PubMed] [Google Scholar]
- 13. Lerman BB, Deale OC. Relation between transcardiac and transthoracic current during defibrillation in humans [published correction appears in Circ Res. 1991;69:1426]. Circ Res. 1990;67:1420–1426. [DOI] [PubMed] [Google Scholar]
- 14. Deakin CD, Sado DM, Petley GW, et al. Differential contribution of skin impedance and thoracic volume to transthoracic impedance during external defibrillation. Resuscitation. 2004;60:171–174. [DOI] [PubMed] [Google Scholar]
- 15. Ewy GA. Optimal technique for electrical cardioversion of atrial fibrillation. Circulation. 1992;86:1645–1647. [DOI] [PubMed] [Google Scholar]
- 16. Hirsh BJ, Copeland‐Halperin RS, Halperin JL. Fibrotic atrial cardiomyopathy, atrial fibrillation, and thromboembolism: mechanistic links and clinical inferences. J Am Coll Cardiol. 2015;65:2239–2251. [DOI] [PubMed] [Google Scholar]
- 17. Shah AJ, Liu X, Jadidi AS, et al. Early management of atrial fibrillation: from imaging to drugs to ablation. Nat Rev Cardiol. 2010;7:345–354. [DOI] [PubMed] [Google Scholar]
- 18. Lim HS, Hocini M, Dubois R, et al. Complexity and distribution of drivers in relation to duration of persistent atrial fibrillation. J Am Coll Cardiol. 2017;69:1257–1269. [DOI] [PubMed] [Google Scholar]
- 19. Gallagher MM, Guo XH, Poloniecki JD, et al. Initial energy setting, outcome and efficiency in direct current cardioversion of atrial fibrillation and flutter. J Am Coll Cardiol. 2001;38:1498–1504. [DOI] [PubMed] [Google Scholar]
- 20. Ramirez FD, Fiset SL, Cleland MJ, et al. Effect of applying force to self‐adhesive electrodes on transthoracic impedance: Implications for electrical cardioversion. Pacing Clin Electrophysiol. 2016;39:1141–1147. [DOI] [PubMed] [Google Scholar]
- 21. Walker RG, Melnick SB, Chapman FW, et al. Comparison of six clinically used external defibrillators in swine. Resuscitation. 2003;57:73–83. [DOI] [PubMed] [Google Scholar]
- 22. Schmidt AS, Lauridsen KG, Adelborg K, et al. Cardioversion efficacy using pulsed biphasic or biphasic truncated exponential waveforms: a randomized clinical trial. J Am Heart Assoc. 2017;6:pii:e004853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Glover BM, Walsh SJ, McCann CJ, et al. Biphasic energy selection for transthoracic cardioversion of atrial fibrillation: the BEST AF trial. Heart. 2008;94:884–887. [DOI] [PubMed] [Google Scholar]
- 24. Hernández‐Madrid A, Svendsen JH, Lip GY, et al. Cardioversion for atrial fibrillation in current european practice: results of the European Heart Rhythm Association survey. Europace. 2013;15:915–918. [DOI] [PubMed] [Google Scholar]
- 25. Inácio JF, dos Santos Gomes da Rosa M, Shah J, et al. Monophasic and biphasic shock for transthoracic conversion of atrial fibrillation: systematic review and network meta‐analysis. Resuscitation. 2016;100:66–75. [DOI] [PubMed] [Google Scholar]


