Abstract
Aims:
Chronic, infrequent voiding may be a risk factor for lower urinary tract symptoms (LUTS) in women. To inform this hypothesis, we conducted a rapid literature review and meta-analysis of LUTS by occupation as an indirect measure of infrequent voiding behaviors.
Methods:
Two independent medical librarians searched Pubmed.gov studies (1990–2017) on adult women for occupations, industries, and workplace environment and LUTS outcomes: overactive bladder (OAB), urinary incontinence (UI), urinary tract infections (UTIs), and individual voiding and storage LUTS. Two authors reviewed full text articles meeting content criteria. Among studies with similar UI definitions, we estimated the prevalence of monthly UI using a random effects meta-analysis model.
Results:
Of 1078 unique citations identified, 113 underwent full article review and 33 met inclusion criteria. Twenty-six of these studies examined specific occupation groups, including nurses/midwives (n = 6 studies), healthcare workers/support staff (n = 6), military personnel (n = 3), teachers (n = 3), and other groups (n = 7), whereas eight compared findings across broad occupation groups. UI was reported in 30 studies (23% using validated measures), OAB in 6 (50% validated), and UTIs in 2 (non-validated). In pooled models, the degree of heterogeneity was too high (I2 = 96.9–99.2%) among the studies to perform valid prevalence estimates for LUTS.
Conclusions:
Current literature limits the ability to evaluate LUTS by occupation types. Future studies should characterize voiding frequency and toilet access in a consistent manner by occupation and explore its relation to LUTS development.
Keywords: LUTS, occupation, productivity, risk factors, urinary incontinence, women, workforce
1 |. BACKGROUND
Given the substantial growth of women in the US workforce—47% of US workers are women—more data are needed to understand the possible influence of occupation type and the workplace environment on lower urinary tract symptoms (LUTS).1,2 LUTS include symptoms of urinary frequency, urgency, nocturia and urinary incontinence (UI), and affect the lives of millions of women.3–6 LUTS occur in 40–60% of women, with rates of urgency type UI (UUI) and overactive bladder (OAB) (defined as urgency with increased daytime frequency and nocturia) increasing greatly with age.3,6–8 Thus, recent emphasis is shifting to early recognition of specific modifiable factors to prevent the development and worsening of bladder symptoms over time.9
A possible, but under-studied, risk factor is chronic, infrequent voiding. Chronic, infrequent voiding may be a behavioral risk factor learned over time due to environmental influences and social norms. Infrequent voiding may also occur in the work environment due to limitations with toilet accessand availability, having the autonomy to toilet when needed, and adaptive behaviors to avoid urine production, such as fluid restriction. These differences could also arise due to occupational activities that affect urinary-holding behaviors in adult women, such as heavy lifting, stressful job demands, working in hot/cold environments, and having to wear specific clothing that could limit the ability to toilet when needed. For this study, we focused on how occupations differ in the prevalence of LUTS, using the type of occupation as a surrogate for the many reasons infrequent voiding may occur in the workplace.
Most research to date on this topic has examined LUTS prevalence in single occupation types hypothesized to have low voiding frequency and potentially limited toilet access, although previous studies did not evaluate toilet access directly. In a prior review of this research, nurses, one of the most commonly studied groups, were cited as having a higher prevalence of LUTS, specifically UI.10 Other occupation groups also hypothesized to have low voiding frequency include retail workers, factory workers, other healthcare workers, and women in active military duty. Many women in specific occupations also engage in adaptive behaviors to manage voiding needs that include decreasing fluid and caffeine intake, wearing absorptive products for protection, and avoiding toileting.11,12 Since these reviews, a few recent studies comparing OAB or UI across broad occupation types, such as women in service/sales occupations, non-manual (managers/professionals) versus manual labor occupations, and unemployed women or women who choose to stay at home, have been published.13–15
We hypothesize that occupation types have variations in the prevalence of LUTS. These variations could arise because of urinary-holding behaviors, including infrequent voiding with prolonged holding, due to various environmental factors related to toilet access. Therefore, our research aimed (i) to compare existing evidence that occupation type has an impact on the prevalence of LUTS; (ii) to evaluate the impact of having LUTS in the workplace; and (iii) to describe evidence related to toilet access in the workplace among women.
2 |. METHODOLOGY
Rapid reviews are employed to streamline systematic review methods to synthesize evidence in a short timeframe. Similar to a systematic review, it consists of a structured methodology to search literature, extract and synthesize data, and assess risk of bias, but the degree of comprehensiveness for each step can vary. Our approach was comprehensive and only differs from a systematic review in not having each step conducted by two independent reviewers in order to expedite the timeframe. Our review protocol was registered on PROS-PERO (CRD42017059817), an international registry of systematic and other types of reviews prior to search.16 All English language research reports (clinical trials, cohort studies, case control studies, cross-sectional surveys, and case reports) focused on occupation types and bladder symptoms among women were included in this rapid review.
2.1 |. Literature search strategy
Two independent medical librarians searched for articles published in Pubmed from January 1990 to July 2017 (see supplemental material). A combination of database-specific subject headings and keywords were used in the search strategies, covering the concepts of occupation or workforce AND bladder or LUTS or urination disorders.
2.2 |. Inclusion and exclusion criteria
Inclusion criteria consisted of human studies, with populations limited to females (aged 18 years of age and older) or populations that included both females and males if a sub-analysis existed by sex. Included studies were also required to provide information on both occupation type and LUTS. We excluded studies based on the follow criteria: guidelines (ie, not original research); non-English language studies; those that included males or institutionalized adults exclusively; and those focused on renal diseases (without mention of LUTS), bladder cancer, kidney stones, catheter usage, renal transplant, pelvic organ prolapse, congenital urinary tract abnormalities, neurologic disorders, and surgical interventions.
2.3 |. Decision process, study selection, and study quality
Seven reviewers performed the initial review of titles and abstracts for relevance using the inclusion and exclusion criteria. Two reviewers then applied these criteria to all selected full text manuscripts and came to consensus about inclusion. Authors extracted data independently using a standardized, pre-piloted form for assessment of study quality, and evidence synthesis.
We used the RTI International (formerly Research Triangle Institute, a non-profit organization) item bank, an existing tool for judging bias and the quality of the evidence.17 After using the tool to rate the manuscripts, we reported our confidence about how close the true effect was to the observed effect (poor, fair, or strong) by considering study limitations, indirectness, imprecision, inconsistency, and publication/reporting bias.
2.4 |. Prevalence estimates and meta-analysis
Data cleaning and extraction were carried out in Microsoft Excel 2016 (Redmond, WA). Statistical analysis and modeling were performed using R 3.2.4 (Vienna, Austria). In order to conduct a meta-analysis of prevalence estimates by occupational groups, we limited the prevalence estimates to studies that used similar definitions. UI prevalence, defined as at least monthly or more, was the only LUTS used in three studies of nurses compared to four studies including broad occupation groups, defined as non-manual labor, manual labor, unemployed, and paid versus non-paid groups. Using these studies that assessed UI by similar definitions, we conducted prevalence estimates using a random effects model18 to incorporate heterogeneity, as measured by the I2 statistics.19
3 |. RESULTS
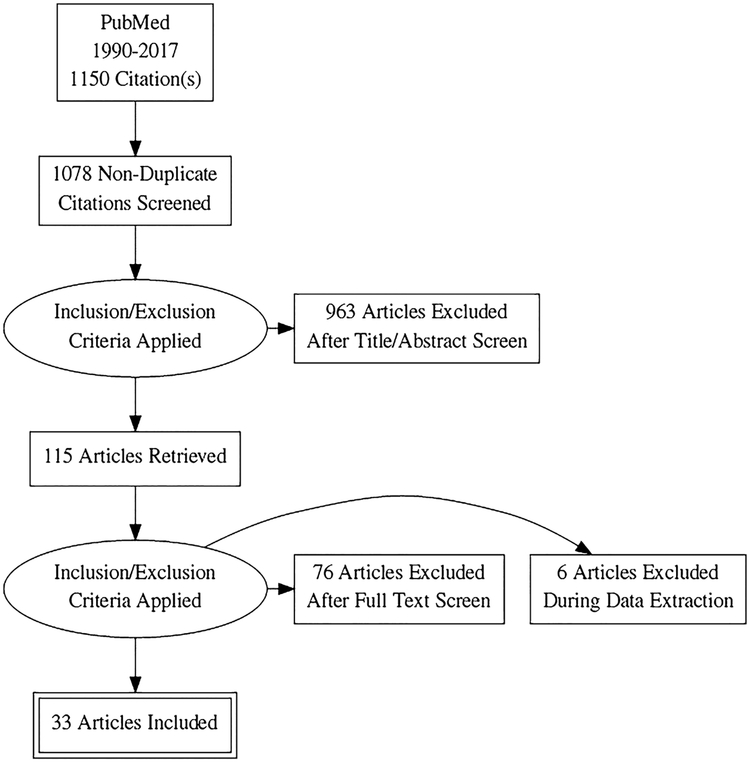
We identified 1150 articles using our search strategy, of which 72 were duplicates. From the remaining 1078 citations, we selected 113 for full text screening, and identified 33 for inclusion in our review (Figure 1).
FIGURE 1.
Flow diagram for studies on occupation and lower urinary tract symptoms
3.1 |. Distribution of occupation and LUTS types across studies
Table 1 describes the 33 studies included in the review and meta-analysis. Of these studies, all were cross-sectional in design with one exception that evaluated the influence of UI on workforce disability and exit.20 Twenty-six reported LUTS within a specific occupation group without comparison to other groups. The remaining eight studies examined broader occupation groups with comparisons across groups. Of the 26 studies within a specific occupation group, 6 studies examined nurses and midwives, 6 examined other health care workers or employees in a healthcare or academic setting,21–31 3 examined US military forces,32–34 3 primary and secondary school teachers,12,35,36 and 7 various other single occupation groups.37–43 Of the eight studies that compared women across broad occupation groups, the authors reported specific occupation types as employed versus non-employed, paid versus non-paid, and manual versus non-manual.13–15,20,44–46 One of the eight examined occupation type as manual, non-manual, sales/service versus unemployed.13
TABLE 1.
Rapid review findings related to occupation groups and lower urinary tract symptoms (LUTS), 33 studies
| LUTS type, definition, & characteristics | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study population: Location or survey name | Study 1st author (Journal) | Pub year | Occupation group(s) | Diseased/Non-diseased | Age Mean ± SD, (range) | Type | Validated measure (Y/N) | Characteristics | Time frame | Findings & notes | Quality (poor, fair, good) |
| Studies reporting LUTS among occupation groups or workplace, n = 25 | |||||||||||
| Nurses/Advance practice nurses/Midwives, n = 6 | |||||||||||
| Japan | Araki (J Urol)30 | 2005 | Nursing department in 52 hospitals | 3734/7229 | 35.2 ± 10.8 (20–64) | UI | Y | Frequency; UI subtypes | Weekly or more | Validated questionnaire used, but only weekly UI rates reported; nurses with UI had greater impairments in quality of life | Fair |
| Taiwan: Taipai | Liao (Int J Nursing Studies)23 | 2009 | Employed female nurses | 907/1065 | 31.0 ± 6.3 (21–59) | LUTS and UI | Y | Presence or absence; severity; UI subtypes | Past year | Nurses (47%) likely to decrease fluid intake at work. Of the respondents, 50% reported inadequate bathroom breaks. Nurses with LUTS had greater impairments in quality of life. | Poor |
| China: Beijing | Zhang (Neurourol Urodyn)30 | 2013 | Nurses at three tertiary hospitals | 1070/1685 | 29.5 ± 7.9 (19–58) | OAB and UI | N | Frequency | Monthly | No direct comparison by group; occupation stress inventory given, Nurses with OAB had higher stress | Poor |
| USA; Pennsylvania | Palmer (Int J Clin Pract)25 | 2015 | Advanced practice nursing providers | 113/373 | 45.1 (26–68) | UI | Y | Frequency | Monthly | Validated toileting behavior questionnaire | Poor |
| China: Jinan | Wan (Int J Nursing Studies)29,53 | 2016 | Nurses at three tertiary hospitals | 636 (no response rate) | 30.6 ± 7.9 (22–55) | LUTS and UI | Y | Frequency | Monthly | Validated toileting behavior questionnaire | Poor |
| Australia: NSW | Pierce (Neurourol Urodyn)27 | 2017 | Nurses and midwives | 2907/5041 | 47.4 ± 11.6, (19–74) | UI | Y | Frequency | Monthly | Intent to leave work based on UI reported—women more severe UI had increased intent to leave current job | Fair |
| Healthcare workers—Mixed occupations including clinicians, support staff, and administrative staff, n = 6 | |||||||||||
| South Africa | Bailey (African J Primary Health Care Fam Med) | 2010 | Hospital workers | 109/154 | 28.3 (18–51) | UI | Y | Frequency; UI subtypes | Monthly | Types of hospital workers not identified. Workers with UI had impaired quality of life. | Poor |
| China | Chen (Int Urol Nephrol)31 | 2015 | Physicians | 351/500 | 47.1 ± 5.4 (42–59) | OAB | Y | Frequency | Monthly | Evaluated impact of peri-menopausal symptoms on OAB; OAB a secondary outcome. | Poor |
| USA: Baltimore | Palmer (Women Health J);34 Fitzgerald (AAHON J);10 Hart, K. J. (ClinNurs Res)54 | 2000 | Urban Academic Center Employees (faculty, clinical, and administrative staff) | 232/1113 | 40.3 (18–73) | UI | N | Frequency | Monthly | Discussed strategies to manage UI at work and healthcare seeking | Poor |
| Turkey: Eskisehir | Kaya Y (Low Urin Tract Symptoms)22 | 2016 | Secretaries and Nurses | 281 (218 nurses; 63 secretaries) | 23.8 ± 3.7 | LUTS and UI | Y | Frequency | Monthly | Nurses hypothesized to have more LUTS than secretaries, no differences in UI or LUTS found between the two occupation groups | Poor |
| France: Paris | Peyrat (Br J Urol Int)36 | 2002 | French academic hospital | 1700 | (20–62) | UI | N | Presence or absence; UI subtypes | NA | Evaluated the association of heavy lifting and UI in the workplace | Poor |
| India: Lucknow | Singh38 | 2013 | Hospital healthcare providers and employees in Ob/Gyn department | 3000 (no response rate) | Median 40 (18->70) | UI | N | Frequency; UI subtypes | Weekly | No direct comparison by group | poor |
| Primary and Secondary School, n = 3 | |||||||||||
| France | Kovess-Masfety, V. (BMC Public Health)34 | 2006 | Male and female teachers compared to non-teachers | 5496/10000 Women teachers = 2183; control = 942 | (20–60) | UTI | N | Frequency | Past year | Focus on mental health and other medical diagnoses; Teachers experience higher UTI rates than non-teachers, but do not have higher rates of other health conditions | Poor |
| Taiwan: Taipai | Liao (Int Urogyn J)35 | 2007 | Elementary school teachers at 26 schools | 445/520 | 38.9 | OAB and UI | Y | Severity; frequency; UI subtypes | Monthly | Pad usage and health seeking behavior reported | Poor |
| USA | Nygaard (Int Urogyn J)11 | 1997 | Public school teachers | 791/1492 | 43.1 (22–73) | Voiding frequency, UTI and UI | N | Frequency | UTI: past year; UI: weekly | Fluid intake limited by teachers due to urinary symptoms. | poor |
| Military, n = 3 | |||||||||||
| USA: Iraq and Afghanistan Veterans | Bradley (J Urol)32 | 2014 | Deployed military service members <2 yrs after return | 1773/3538 | 31.1 ± 8.4 | OAB and Urgency UI | Y | Presence or absence | NA | Returning women Veterans with OAB had greater odds of having mental health symptoms and history of sexual assault. | Fair |
| USA: Army | Davis (Military Med)31 | 1999 | Military service—active duty | 563/713 | 28.3 (18–51) | UI | N | Frequency; UI subtypes | Monthly or more | Evaluated interference of symptoms in work related duties | Poor |
| USA: Air force | Fischer (Obstet Gynecol)33 | 1999 | Military service—Air Force Aircrew | 274/426 | NR | UI | N | Presence or absence of “ever” leaked; UI subtypes | NA | Place where UI occurs—home, on duty, flying | poor |
| All other, n = 7 | |||||||||||
| Japan | Azuma (Nurs Health Sc,)36 | 2008 | Retail stores | 975/2175 | 47.6 ± 9.8 (18–72) | UI | Y | Frequency; UI subtypes | Monthly or more | Knowledge and health seeking behaviors included | Poor |
| Norway | Bo (Neurourol Urodyn)37 | 2011 | Fitness instructors | 847/1473; 685 | 32.8 ± 8.3 (18–68) | UI | Y | Frequency | Monthly | Prevalence rate of UI similar across types of | Poor |
| USA | Fitzgerald (Women Health)35 | 2002 | Factory workers—Manufacturing/Distribution of pottery | 269/500 | 40 (16–69) | UI | N | Frequency; UI subtypes | Monthly or more | Health seeking behaviors included | Poor |
| Taiwan | Lin (Appl Ergon)41 | 2009 | Operators at telecommunication call centers | 868 women/1100 | (25–34) | Urinary frequency | N | Frequency | Daily | Primary aim to evaluate job stress and physical discomfort; frequent urination had a higher odds for having increased job stress | Fair |
| Korea | Kim (Urology)40 | 2015 | male and female nonshift and shift workers ages 40–70 seeking care in urology clinic | 1376 nonshift workers (764 women); 365 shift workers—165 women | 58.5 ± 13.9 | Nocturia | Y | Frequency and volume charts | Daily | Retrospective study; nocturia higher in shift workers; not all participants had LUTS or were seeking care for LUTS | Poor |
| Taiwan | Su (Int Urogyneeol I)43 | 2009 | Electronics industry workers | 2062/2062 | Non pregnant workers: <24, 24–27, 28–30, >30 | UTI | N | Frequency | NA | Urinating 3 or more times was protective for UTI | Poor |
| France: GAZEL cohort | Saadoun (Neurourol Urodyn)42 | 2006 | Utility company employees: blue collar, clerical, supervisors, management | 556/2640 | 55 ± 3 (49–61) | UI | Y | Frequency; severity | Monthly or more | UI rates not reported by specific occupations | Fair |
| Studies comparing LUTS across broad occupation groups, n = 8 | |||||||||||
| USA: OAB POLL | Coyne (Urology)47 | 2012 | Current employment status; working full-time, working part-time, and other work for pay | 3210 women | No symptoms 40.7 ± 13.8 OAB symptoms 45.4 ± 14.2 | OAB | Y | Frequency | Monthly or more | OAB rates not reported by occupation groups; Women with OAB less likely to work full time, increased negative impact in work productivity; men but not women with OAB more likely to be unemployed | Fair |
| USA: National family opinion survey | Fultz (Occupational Med)45 | 2005 | Working full-time, working part-time, volunteer work, retired, homemaker status | 3364/5130 | 44 (18–60) | UI | Y | Frequency severity; UI subtypes | Monthly or more | UI rates not reported by occupation groups; data on UI management and impact on work productivity | Fair |
| USA: National health and retirement survey | Hung (Obstetrics Gynecology)19 | 2014 | Working full-time, working part-time, unemployed, partly retired, retired, disabled, or not in the labor force | 4511 | 59.4 (54–65) | UI | N | Frequency | Monthly or more | UI rates not reported by occupation groups; UI increased risk for work disability but not work force exit in adjusted analysis over time | Fair |
| Denmark: Aarhus | Lam (Dan Med Bull)46 | 1992 | Employers, white collar, skilled workers, housewives, pensioners | 2631 women | (30–59) | UI | N | Frequency; UI subtypes | Past year | Types of UI reported by occupation groups in age-adjusted analysis without direct comparison data on prevalence; data on social context, abstention, and perception | Fair |
| China: Shanghai | Liu (Int J ClinExp Med)13 | 2014 | Manual (intensity) vs non-manual labor | 5433/5467 | median 46.8 (20–100) | LUTS and UI | Y | Frequency; severity; UI subtypes | Monthly or more | Manual labor versus non-manual increased odds of UI in adjusted analysis (OR 6.9, 95%CI 5.7–8.5) | Good |
| Korea: KHANES | Kim (Women & Health)13 | 2016 | Korean Standard Classification of Occupations: non-manual, service/sales, manual workers, unemployed | 5928 women | (19–64) | UI | N | Presence or absence of “current UI” | NA | Non-manual and service/sales occupation groups had increased prevalence of any UI than manual and unemployed groups in unadjusted analysis. In adjusted analysis, women in sales/service vs unemployed women had increased odds of having any UI (OR 1.6, 95%CI 1.2–2.2). | Fair |
| USA: EpiLUTS | Sexton (Am J Managed Care)44 | 2009 | Working full-time, working part-time, and other work for pay | 2820 women | 51 ± 6.5 | LUTS and UI | N | Frequency; UI subtypes | Monthly or more | OAB and UI rates not reported by occupation groups; Women with OAB/UI less likely to work full time and have a negative impact in work productivity; unadjusted analysis | Fair |
| China: Six geographic regions | Wang (Neurourol Urodyn)14 | 2011 | Manual worker, “mental” worker, and unemployed/housewife | 14844/21 513 | 47.5 (18–80) | OAB | Y | Frequency; severity; UI subtypes | Weekly or more | Manual workers versus other groups had increased odds of OAB in adjusted analysis (OR 1.7 95%CI 1.6–1.8) | Good |
LUTS, lower urinary tract symptoms; NA, not applicable; NR, not reported; OAB, overactive bladder; UI, urinary incontinence; UTI, urinary tract infection.
Studies also varied in the type of bladder symptoms reported, the frequency of the symptom recorded, and the use of validated measures to ascertain symptoms (Table 1). UI was the most common bladder symptom reported in 30 publications,11–15,20–39,42–46 7 of which used validated UI measures.21,26,28,37,38,42 Six publications focused on OAB,15,22,31,33,44,47 including three that used validated OAB measures.15,22,44 Five publications reported general LUTS, and all five used validated LUTS measures.14,23,24,30,36 Other publications focused on daytime frequency,12,41 UTIs,12,35 and one on nocturia.40 Only one manuscript reported data using frequency volume charts.40
3.2 |. Comparison of LUTS prevalence by occupation type
Despite the seeming overlap in occupation and LUTS types across studies, we were unable to combine estimates among the specific workforce groups because of the high degree of heterogeneity across estimates. For instance, even though 26 studies reported UI, the I2 value for a pooled estimate of UI across studies (27.1%, 95% confidence interval [CI]: 22.6–31.5%) was high (99.3%), with variations in the definitions of UI reported from each study. Further grouping of studies by similar occupation and period of UI assessment did not reduce heterogeneity. For example, we pooled the data and estimated the prevalence of monthly UI in nurses (n = 3 studies) compared to studies of broad occupation groups (n = 4 studies). Given the high degree of heterogeneity for these pooled estimates (I2 96.9% for nursing studies vs 99.2% for broad occupational group studies, we were not able to report prevalence estimates. Studies also reported a wide age range among nurses (19–74 years) and for broad occupation groups (18–80 years).
Of the eight publications that evaluated broader occupational groups, three studies reported prevalence rates (two reported UI and one OAB) across occupational groups.13–15 In multivariable analyses from two of the three studies, women working in manual labor jobs had an increased odds of UI (OR 6.9, 95%CI 5.7–8.5) and OAB (OR 1.7, 95%CI 1.6–1.8) compared to women in non-manual occupations or unemployed women.14,15 In one of the three studies, women in sales/service workforce groups (OR 1.6, 95%CI 1.2–2.2) had a higher odds of UI than unemployed women, whereas no difference was observed for women in manual occupation groups (OR 1.2, 95%CI 0.8–1.7) versus employed women.13
3.3 |. Impact of LUTS on workforce productivity, toileting behaviors, and toilet access
Three of the eight publications surveyed women across occupational groups and evaluated the impact of UI and OAB on workplace productivity and workplace activities, but did not directly compare the impact of LUTS on productivity or toileting behaviors across occupation groups.44,45,47 In these three studies, women experiencing UI and OAB reported that their symptoms had a negative impact on work productivity (concentration and task completion) and workplace activities (performance on physical tasks and general interference) compared to women without LUTS. Women with more severe UI were also more likely to reduce their number of hours worked or change their type of work.45 In a study among a single occupation group, nurses and midwives with more severe UI were more likely to report an intention to leave work at 12 months compared to women with less severe UI in adjusted models.28 In another longitudinal study that evaluated women aged 55–65, the authors found that UI led to increased disability but not workforce exit.20
Nine studies reported that women with LUTS modified toileting behaviors in the workplace due to their symptoms.12,24–26,30,32,35,39,45 In a study that compared UI across occupation groups, women with UI were more likely to wear pads and take frequent bathroom breaks than women without UI.45 In other studies among women in the nursing workforce, nurses reported delaying voiding while at work, avoiding public toilets, voiding with little or no need (“just in case”), reducing fluid consumption due to work demands, and restricting fluid to reduce UI episodes.24–26,30 Other workforce groups, such as teachers, military personnel, and factory workers, also reported similar behavior changes at work, especially related to restricting fluids.12,32,39 Other studies reported higher rates of UTIs among women who restricted their fluid intake due to LUTS.12,35
Only one study evaluated access to toilets and the toilet environment, along with other characteristics relevant to voiding in the workplace.13 Women in this study responded to eight questions about toileting in the workplace: presence of a clean and comfortable workplace toilet, having a dangerous job and high probability of accidents, feeling pressed for time, having decision-making authority, maintaining trust and respect, being in awkward positions for long periods of time, carrying heavy weights, and hiding feelings at work.13 UI rates were higher among women who reported having a dangerous job and a high probability of accidents (P = 0.012), feeling pressed for time (P = 0.045), being in awkward positions for long periods (P < 0.001), and carrying heavy weights (P < 0.001). This study did not report differences in these characteristics across broad occupational groups.
4 |. DISCUSSION
This rapid review and meta-analysis found limited evidence to inform the hypothesis that infrequent voiding in the workplace contributes to LUTS. Few studies compared the prevalence of LUTS across occupation types, and single occupation studies were too variable to allow for informative comparisons across occupations. This high degree of heterogeneity prevented us from investigating claims that nurses and teachers have higher rates of UI than other groups. However, we did find suggestive evidence that LUTS prevalence varies across broad occupational groups. In the small number of studies conducted, women in manual occupations had increased rates of UI and OAB compared to unemployed women or women in non-manual occupations. Women with OAB and UI were also more likely to modify their behaviors in the workplace by decreasing voiding and fluid intake, have decreased work productivity, and were at increased risk for disability. To inform our hypothesis that infrequent voiding contributes to LUTS, higher quality studies are needed to compare LUTS across occupational groups, using validated LUTS questionnaires, especially those that measure changes in toileting access and adaptive behaviors over time, as well as longitudinal data to study the temporal relationship between occupation and LUTS.
In comparison to a 2016 review of 22 studies that evaluated pelvic floor dysfunction in workforce groups, Pierce et al reported that women in nursing occupations may experience higher rates of UI than other occupation groups, although they did not pool prevalence estimates or perform direct comparisons to other occupation groups.10 In our analysis, which included an additional 11 studies, we were not able to make valid comparisons of UI prevalence across specific occupation groups due to the high degree of heterogeneity across prevalence estimates. This high degree of heterogeneity was likely due to the varying definitions and periods used to measure UI, as well as variations in the ages of women in the studies. Future studies should consider the ability to compare LUTS across specific high-risk occupation groups at increased risk for LUTS based on voiding frequency, toileting behaviors, and the workplace toilet environment.
Despite the limited number of studies and lack of direct comparisons across broad occupation groups, the data are supportive of a role for occupation group in the prevalence of LUTS. From the three studies that directly compared UI and OAB rates across workforce groups, those with higher manual labor demands and those in service/retail had an increased odds of UI compared to those in other workforce groups.13–15 Women with manual occupations may have more physical demands at work (eg, heavy lifting or strenuous activity), which may precipitate stress UI, or have limited access to toilets in the workplace due to time or environmental constraints. Women in service and retail occupations may not have adequate time for toileting due to high-paced job demands. Further studies are needed to better understand the physical demands and toilet access of occupations represented by these broad occupational groups. Longitudinal data would also help inform temporal patterns of occupation as a risk factor over time to determine whether participants’ occupations contributed to their LUTS or whether they chose their occupations to accommodate their pre-existing LUTS.
We limited our search to studies that included occupation groups as the primary risk factor of interest. Therefore, we did not include the largest study of US nurses, the Nurses’ Health Study (NHS), to date that included cross-sectional and longitudinal data on UI among nurses.8,48,49 However, in the NHS, prevalence, incidence, and remission rates are comparable to other data among US women.6,50,51 And, low fluid intake was not related to high rates of incident UI or UI subtypes over a 4-year period.52 To our knowledge, the NHS participants reported data on job strain and social support, but not on the specific type of nursing occupation, job activities or duty hours, which would help inform our hypothesis.53 Given that the majority of studies in our review were cross-sectional, we were not able to investigate the possible role of fluid intake as a mediator in LUTS development among occupation groups.
Although this manuscript did not meet published criteria for a systematic review, such as having two independent reviewers extract data from all full text manuscripts, our rapid review process remained rigorous.16 Our methodology followed guidelines that included using two independent librarians to implement our search strategy, a large group of independent reviewers during the abstract screening process, two reviewers who approved manuscripts for inclusion/exclusion criteria, and validated methodology for the quality review.16 However, limitations in our approach include only using one database to search for existing studies (Pubmed) and the lack of two independent reviewers during the screening process.
In conclusion, women in the workforce commonly experience UI and LUTS, and modify their behaviors to manage their symptoms. Current literature limits the ability to compare rates of LUTS by occupation among working women, especially in homogeneous high-risk groups, such as elementary school teachers and specific types of nurses. To better characterize the prevalence of LUTS by occupation group additional studies need to use validated LUTS assessments, well-defined occupational groups, and clear comparison groups. Additionally, it is critical that we understand how the work environment affects voiding frequency, access to toilets, autonomy to void when needed, adaptive behaviors to manage LUTS, as well as work productivity, especially over time. Given that the majority of US women work outside the home, this type of research could help inform toileting policies in the workplace environment.
Supplementary Material
ACKNOWLEDGMENTS
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The Prevention of Lower Urinary Tract Symptoms (PLUS) Research Consortium is supported by National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases through cooperative agreements (grants U01DK106786, U01DK106853, U01DK106858, U01DK106898, U01DK106893, U01DK106827, U01DK10–6908, U01DK106892). National Institute on Aging, NIH Office of Research on Women’s Health and Office of Behavioral and Social Sciences Research.
Funding information
DK/NIDDK NIH HHS/United States, Grant numbers: U01 DK106858, U01 DK106908, U01 DK106898, U01 DK106786, U01 DK106892, U01 DK106853, U01 DK106893, U01 DK106827
Footnotes
Roger Dmochowski led the peer-review process as the Associate Editor responsible for the paper.
PLUS research centers
Loyola University Chicago—Linda Brubaker, MD, MS, Multi-PI; Elizabeth Mueller, MD, MSME, Multi-PI; Colleen M. Fitzgerald, MD, MS, Investigator; Cecilia T. Hardacker, RN, MSN, Investigator; Jennifer M. Hebert-Beirne, PhD, MPH, Investigator; Missy Lavender, MBA, Investigator; David A. Shoham, PhD, Investigator.
University of Alabama at Birmingham—Kathryn Burgio, PhD, PI; Cora Beth Lewis, MD, Investigator; Alayne Markland, DO, MSc, Investigator; Gerald McGwin, PhD, Investigator; Beverly Williams, PhD, Investigator, Patricia S. Goode, MD.
University of California San Diego—Emily S. Lukacz, MD, PI; Sheila Gahagan, MD, MPH, Investigator; D. Yvette LaCoursiere, MD, MPH, Investigator; Jesse N. Nodora, DrPH, Investigator.
University of Michigan—Janis M. Miller, PhD, MSN, PI; Lawrence Chin-I An, MD, Investigator; Lisa Kane Low, PhD, MS, CNM, Investigator.
University of Minnesota—Bernard Harlow, PhD, Multi-PI; Kyle Rudser, PhD, Multi-PI; Sonya S. Brady, PhD, Investigator; John Connett, PhD, Investigator; Haitao Chu, MD, PhD, Investigator; Cynthia Fok, MD, MPH, Investigator; Sarah Lindberg, MPH, Investigator; Todd Rockwood, PhD, Investigator.
University of Pennsylvania—Diane Kaschak Newman, DNP, ANP-BC, FAAN PI; Amanda Berry, PhD, CRNP, Investigator; C. Neill Epperson, MD, Investigator; Kathryn H. Schmitz, PhD, MPH, FACSM, FTOS, Investigator; Ariana L. Smith, MD, Investigator; Ann Stapleton, MD, FIDSA, FACP, Investigator; Jean Wyman, PhD, RN, FAAN, Investigator.
Washington University in St. Louis—Siobhan Sutcliffe, PhD, PI; Colleen McNicholas, DO, MSc, Investigator; Aimee
James, PhD, MPH, Investigator; Jerry Lowder, MD, MSc, Investigator; Mary Townsend, ScD, Investigator.
Yale University—Leslie Rickey, MD, PI; Deepa Camenga, MD, MHS, Investigator; Toby Chai, MD, Investigator; Jessica B. Lewis, LMFT, MPhil, Investigator.
NIH Program Office: National Institute of Diabetes and Digestive and Kidney Diseases, Division of Kidney, Urologic, and Hematologic Diseases, Bethesda, MD: NIH Project Scientist: Tamara Bavendam MD, MS; Project Officer: Ziya Kirkali, MD; Scientific Advisors: Chris Mullins, PhD and Jenna Norton, MPH; Steering Committee Chair: Mary H. Palmer, PhD.
Scientific and Data Coordinating Center: University of Minnesota, Minneapolis, MN.
Steering Committee: Chair: Mary H. Palmer, PhD.
CONFLICTS OF INTEREST
Dr. Bavendam has nothing to disclose. Dr. Chu, Dr. Epperson, Dr. Nodora, Dr. Markland, Dr. Shoham, Dr. Smith, Dr. Sutcliffe, Dr. Townsend, and Dr. Zhou report grants from NIH/NIDDK, during the conduct of the study.
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section at the end of the article.
REFERENCES
- 1.Mosisa A, Hipple S. Trends in labor force participation in the United States. Monthly Lab Rev. 2006;129:35. [Google Scholar]
- 2.Durrheim D, Access to toilets for all. Lancet. 2007;370:1590. [DOI] [PubMed] [Google Scholar]
- 3.Eapen RS, Radomski SB. Review of the epidemiology of overactive bladder. Res Rep Urol. 2016;8:71–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Irwin DE, Milsom I, Hunskaar S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50:1306. [DOI] [PubMed] [Google Scholar]
- 5.Tennstedt SL, Link CL, Steers WD, McKinlay JB. Prevalence of and risk factors for urine leakage in a racially and ethnically diverse population of adults: the Boston Area Community Health (BACH) Survey. Am J Epidemiol. 2008;167:390–399. [DOI] [PubMed] [Google Scholar]
- 6.Maserejian NN, Chen S, Chiu GR, et al. Incidence of lower urinary tract symptoms in a population-based study of men and women. Urology. 2013;82:560–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaughan CP, Johnson TM, Ala-Lipasti MA, et al. The prevalence of clinically meaningful overactive bladder: bother and quality of life results from the population-based FINNO study. Eur Urol. 2011;59:629–636. [DOI] [PubMed] [Google Scholar]
- 8.Lifford KL, Townsend MK, Curhan GC, Resnick NM, Grodstein F. The epidemiology of urinary incontinence in older women: incidence, progression, and remission. J Am Geriatr Soc. 2008; 56:1191–1198. [DOI] [PubMed] [Google Scholar]
- 9.Lukacz ES, Sampselle C, Gray M, et al. A healthy bladder: a consensus statement. Int J Clin Pract. 2011;65:1026–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pierce H, Perry L, Chiarelli P, Gallagher R. A systematic review of prevalence and impact of symptoms of pelvic floor dysfunction in identified workforce groups. J Adv Nurs. 2016;72:1718–34. [DOI] [PubMed] [Google Scholar]
- 11.Fitzgerald ST, Palmer MH, Berry SJ, Hart K. Urinary incontinence. Impact on working women. AAOHN J. 2000;48:112–118. [PubMed] [Google Scholar]
- 12.Nygaard I, Linder M. Thirst at work-an occupational hazard? Int Urogynecol J Pelvic Floor Dysfunct. 1997;8:340–343. [DOI] [PubMed] [Google Scholar]
- 13.Kim Y, Kwak Y. Urinary incontinence in women in relation to occupational status. Women Health. 2017;57:1–18. [DOI] [PubMed] [Google Scholar]
- 14.Liu B, Wang L, Huang SS, Wu Q, Wu DL. Prevalence and risk factors of urinary incontinence among Chinese women in Shanghai. Int J Clin Exp Med. 2014;7:686–696. [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Y, Xu K, Hu H, et al. Prevalence, risk factors, and impact on health related quality of life of overactive bladder in China. Neurourol Urodyn. 2011;30:1448–1455. [DOI] [PubMed] [Google Scholar]
- 16.Ganann R, Ciliska D, Thomas H. Expediting systematic reviews: methods and implications of rapid reviews. Implement Sci. 2010;5:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Viswanathan M, Berkman ND, Dryden DM, Hartling L. AHRQ methods for effective health care Assessing Risk of Bias and Confounding in Observational Studies of Interventions or Exposures: Further Development of the RTI Item Bank. Rockville (MD): Agency for Healthcare Research and Quality (US); 2013. [PubMed] [Google Scholar]
- 18.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clin Trials. 1986;7:177–188. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. [DOI] [PubMed] [Google Scholar]
- 20.Hung KJ, Awtrey CS, Tsai AC. Urinary incontinence, depression, and economic outcomes in a cohort of women between the ages of 54 and 65 years. Obstet Gynecol. 2014;123:822–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Araki I, Beppu M, Kajiwara M, et al. Prevalence and impact on generic quality of life of urinary incontinence in Japanese working women: assessment by ICI questionnaire and SF-36 Health Survey. Urology. 2005;66:88–93. [DOI] [PubMed] [Google Scholar]
- 22.Chen Y, Yu W, Yang Y, et al. Association between overactive bladder and peri-menopause syndrome: a cross-sectional study of female physicians in China. Int Urol Nephrol. 2015;47: 743–749. [DOI] [PubMed] [Google Scholar]
- 23.Kaya Y, Kaya C, Baseskioglu B, Ozerdogan N, Yenilmez A, Demirustu C. Effect of work-Related factors on lower urinary tract symptoms in nurses and secretaries. Low Urin Tract Symp. 2016;8: 49–54. [DOI] [PubMed] [Google Scholar]
- 24.Liao YM, Yang CY, Kao CC, et al. Prevalence and impact on quality of life of lower urinary tract symptoms among a sample of employed women in Taipei: a questionnaire survey. Int J Nurs Stud. 2009;46:633–644. [DOI] [PubMed] [Google Scholar]
- 25.Palmer MH, Fitzgerald S, Berry SJ, Hart K. Urinary incontinence in working women: an exploratory study. Women Health. 1999;29: 67–82. [DOI] [PubMed] [Google Scholar]
- 26.Palmer MH, Newman DK. Women’s toileting behaviours: an online survey of female advanced practice providers. Int J Clin Pract. 2015;69:429–435. [DOI] [PubMed] [Google Scholar]
- 27.Peyrat L, Haillot O, Bruyere F, Boutin JM, Bertrand P, Lanson Y. Prevalence and risk factors of urinary incontinence in young and middle-aged women. BJU Int. 2002;89:61–66. [DOI] [PubMed] [Google Scholar]
- 28.Pierce H, Perry L, Gallagher R, Chiarelli P. Urinary incontinence, work, and intention to leave current job: a cross sectional survey of the Australian nursing and midwifery workforce. Neurourol Urodyn. 2017;36:1876–1883. [DOI] [PubMed] [Google Scholar]
- 29.Singh U, Agarwal P, Verma ML, Dalela D, Singh N, Shankhwar P. Prevalence and risk factors of urinary incontinence in Indian women: a hospital-based survey. Indian J Urol. 2013;29:31–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wan X, Wu C, Xu D, Huang L, Wang K. Toileting behaviours and lower urinary tract symptoms among female nurses: a cross-sectional questionnaire survey. Int J Nurs Stud. 2016;65:1–7. [DOI] [PubMed] [Google Scholar]
- 31.Zhang C, Hai T, Yu L, et al. Association between occupational stress and risk of overactive bladder and other lower urinary tract symptoms: a cross-sectional study of female nurses in China. Neurourol Urodyn. 2013;32:254–260. [DOI] [PubMed] [Google Scholar]
- 32.Davis G, Sherman R, Wong MF, McClure G, Perez R, Hibbert M. Urinary incontinence among female soldiers. Military Med. 1999; 164:182–187. [PubMed] [Google Scholar]
- 33.Bradley CS, Nygaard IE, Mengeling MA, et al. Urinary incontinence, depression and posttraumatic stress disorder in women veterans. Am J Obstet Gynecol. 2012;206:502 e501–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fischer JR, Berg PH. Urinary incontinence in United States air force female aircrew. Obstet Gynecol. 1999;94:532–536. [DOI] [PubMed] [Google Scholar]
- 35.Kovess-Masfety V, Sevilla-Dedieu C, Rios-Seidel C, Nerriere E, Chan Chee C. Do teachers have more health problems? Results from a French cross-sectional survey. BMC Pub Health. 2006;6: 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liao YM, Dougherty MC, Biemer PP, et al. Prevalence of lower urinary tract symptoms among female elementary school teachers in Taipei. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:1151–1161. [DOI] [PubMed] [Google Scholar]
- 37.Azuma R, Murakami K, Iwamoto M, Tanaka M, Saita N, Abe Y. Prevalence and risk factors of urinary incontinence and its influence on the quality of life of Japanese women. Nurs Health Sci. 2008;10:151–158. [DOI] [PubMed] [Google Scholar]
- 38.Bo K, Bratland-Sanda S, Sundgot-Borgen J. Urinary incontinence among group fitness instructors including yoga and pilates teachers. Neurourol Urodyn. 2011;30:370–373. [DOI] [PubMed] [Google Scholar]
- 39.Fitzgerald ST, Palmer MH, Kirkland VL, Robinson L. The impact of urinary incontinence in working women: a study in a production facility. Women Health. 2002;35:1–16. [DOI] [PubMed] [Google Scholar]
- 40.Kim JW. Effect of shift work on nocturia. Urology. 2016;87: 153–160. [DOI] [PubMed] [Google Scholar]
- 41.Lin YH, Chen CY, Lu SY. Physical discomfort and psychosocial job stress among male and female operators at telecommunication call centers in Taiwan. Appl Ergon. 2009;40:561–568. [DOI] [PubMed] [Google Scholar]
- 42.Saadoun K, Ringa V, Fritel X, Varnoux N, Zins M, Breart G. Negative impact of urinary incontinence on quality of life, a cross-sectional study among women aged 49–61 years enrolled in the GAZEL cohort. Neurourol Urodyn. 2006;25:696–702. [DOI] [PubMed] [Google Scholar]
- 43.Su SB, Wang JN, Lu CW, Wang HY, Guo HR. Prevalence of urinary tract infections and associated factors among pregnant workers in the electronics industry. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:939–945. [DOI] [PubMed] [Google Scholar]
- 44.Sexton CC, Coyne KS, Vats V, Kopp ZS, Irwin DE, Wagner TH. Impact of overactive bladder on work productivity in the United States: results from EpiLUTS. Am J Manag Care. 2009;15:S98–s107. [PubMed] [Google Scholar]
- 45.Fultz N, Girts T, Kinchen K, Nygaard I, Pohl G, Sternfeld B. Prevalence, management and impact of urinary incontinence in the workplace. Occup Med (Lond). 2005;55:552–557. [DOI] [PubMed] [Google Scholar]
- 46.Lam GW, Foldspang A, Elving LB, Mommsen S. Social context, social abstention, and problem recognition correlated with adult female urinary incontinence. Dan Med Bull. 1992; 39:565–570. [PubMed] [Google Scholar]
- 47.Coyne KS, Sexton CC, Thompson CL, et al. Impact of overactive bladder on work productivity. Urology. 2012;80:97–103. [DOI] [PubMed] [Google Scholar]
- 48.Grodstein F, Fretts R, Lifford K, Resnick N, Curhan G. Association of age, race, and obstetric history with urinary symptoms among women in the Nurses’ Health Study. Am J Obstet Gynecol. 2003;189:428–434. [DOI] [PubMed] [Google Scholar]
- 49.Townsend MK, Danforth KN, Lifford KL, et al. Incidence and remission of urinary incontinence in middle-aged women. Am J Obstet Gynecol. 2007;197:167 e161–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nygaard I, Barber MD, Burgio KL, et al. Prevalence of symptomatic pelvic floor disorders in US women. Jama. 2008; 300:1311–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thom DH, Brown JS, Schembri M, Ragins AI, Subak LL, Van Den Eeden SK. Incidence of and risk factors for change in urinary incontinence status in a prospective cohort of middle-aged and older women: the reproductive risk of incontinence study in Kaiser. J Urol. 2010;184:1394–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Townsend MK, Jura YH, Curhan GC, Resnick NM, Grodstein F. Fluid intake and risk of stress, urgency, and mixed urinary incontinence. Am J Obstet Gynecol. 2011;205:73 e71–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schernhammer ES, Hankinson SE, Rosner B, et al. Job stress and Breast cancer Risk: the nurses’ health study. Am J Epidemiol. 2004;160:1079–1086. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.