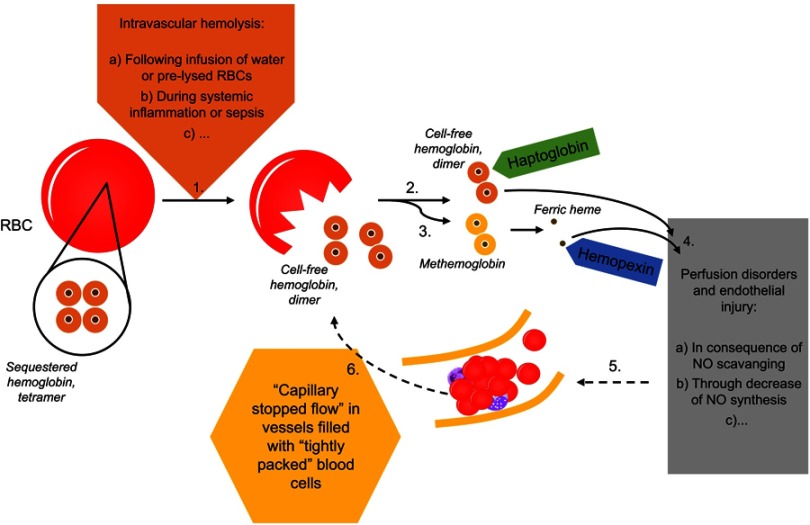
Figure 1.
In the course of intravascular hemolysis (1), eg, induced by infusion of water or pre-lysed red blood cells2–5 or as a consequence of systemic inflammation,15 hemoglobin will be released from the red blood cells (RBCs) into the plasma.1 Normally, cell-free hemoglobin or the during oxidation released ferric heme rapidly will be bound by its scavengers haptoglobin (2) and hemopexin (3). Massive hemolysis may result in saturation and depletion of these hemoglobin removal systems and consequently in an accumulation of hemoglobin and heme in plasma.1 Both, cell-free heme and hemoglobin mediate endothelial injury (4).1 Among others, cell-free hemoglobin is able to effectively scavenge nitric oxide (NO), which in turn leads to perfusion disorders (4).1 Microcirculatory disorders will be associated with a reduced perfused capillary density and red blood cell velocity (5).14 An increased amount of capillaries with either a low or a blocked flow is called as “capillary stopped-flow” or microvascular stasis (5).13,14 One consequence of changes in vessel diameter and concomitant rheological changes to blood cells will be the release of cell components (eg, hemoglobin) from red blood cells (6).13 Causality seems to apply in both directions (1–4 vs 4–1).