Abstract
Objective
The aim of this study was to evaluate the outcomes of open reduction and internal fixation (ORIF) in hamate hook fractures and review the literature on this surgical procedure.
Methods
We report the outcomes of ORIF of hamate hook fractures in 13 consecutive patients (12 men and 1 woman; mean age: 32 years (range, 22–48 years)). In eight patients (61%) the fracture was associated with ulnar nerve neuritis in Guyon's canal. We assessed the following clinical data: age, sex, mechanism of injury, side of the injured hand and associated lesions, fracture classification, average time from injury to correct diagnosis, surgical technique, complications, and length of follow-up.
All patients underwent radiological imaging, including standard radiographs in two planes (anteroposterior and lateral projections), and a CT study. Functional outcomes evaluated were pain, range of motion, grip strength, Disabilities of the arm, shoulder and hand (DASH) and Mayo wrist score.
Results
The mean follow-up was 36 months (range, 12–144 months). All 13 cases were treated with ORIF of the hook of the hamate. Mean VAS pain score was 5 preoperatively (4–9) and 1 (0–2) postoperatively. All patients returned to pre-injury level and only one patient felt pain on activity. Preoperative modified Mayo wrist score was 51 and the postoperative value was 94. All outcomes scores improved significantly from preoperative values. The patients who participated in sports postoperatively were able to do so at or near pre-injury levels. Postoperative average range of wrist motion was 76° in extension, 71° in flexion, 14° in ulnar deviation, and 21° in radial deviation.
Mean grip strength in the hand with the hook fracture was 58 kg compared with 53 Kg in the unaffected hand. All patients returned to their pre-injury level of functioning after 10–12 weeks and there were no complications. Analysis of grip strength revealed values comparable with the unaffected hand.
Conclusion
ORIF of hamate hook fractures is a safe and effective technique to restore normal grip strength and return to pre-injury level. In cases of ulnar nerve neuritis, neurolysis of the deep palmar branch is mandatory.
Level of evidence
Level IV, Therapeutic study.
Keywords: Guyon's canal, Hamate fracture, Hook of the hamate neuritis, Ulnar nerve
Introduction
Fractures of the hamate hook comprise 2–4% of all carpal fractures.1 They may be caused by several mechanisms, such as direct impact on the hypothenar eminence, an indirect shearing force applied by the extrinsic flexor tendons of the ring and small fingers, or microtrauma from repetitive forceful gripping in racquet or bat sports.2, 3, 4
Diagnosis of acute hamate hook fracture is difficult and rarely made at the time of the initial injury. Clinical signs are often mild or nonspecific, and may even be absent. Furthermore, routine radiographs of the wrist and hand are often inconclusive. The carpal tunnel view has been advocated to detect the fracture, but this view is not always feasible because it requires full wrist extension, a position that may be difficult to achieve and painful for the patient. Furthermore, the fracture can be missed on this view as well.5, 6 For this reason, a high index of suspicion is required to establish the diagnosis of hook of hamate fracture in all patients with ulnar pain of the hand after an acute or chronic trauma, especially in racquet or club sports.5 If radiographs are negative, a CT is helpful to define a bone injury.6
With respect to treatment, lower arm cast immobilization is usually proposed to treat acute non-displaced hook fractures.7 However, as this approach frequently fails in delayed fractures,8, 9, 10 most authors recommend surgical intervention. In this regard, hook excision remains the operation of choice for most surgeons.11, 12 However, alternatives to hook excision are available, one of which is ORIF.10
The purpose of this study was to evaluate the outcomes of ORIF in hamate hook fractures and review the literature on this surgical procedure.
Patients and methods
This study was approved by our institutional review board and was conducted accordingly under its protocol and guidelines.
Patients
In a retrospective study over a period of 12 years (2003–2015), we identified 13 patients with a hamate hook fracture who were surgically treated with ORIF. All patients had a minimum follow-up of 1 year after surgery and completed the study follow-up examination.
We assessed the following clinical data: age, sex, mechanism of injury, side of the injured hand and associated lesions, fracture classification, average time from injury to correct diagnosis, surgical technique, complications, and length of follow-up. The range of motion (ROM) values was measured on both sides. Electromyography was performed in all cases with ulnar nerve symptoms. The presence of positive sharp waves, fibrillations, fasciculations, multiple durations, and poly-phases were observed and evaluated. The patients were assessed for relief of clinical symptoms and recovery of sensibility (static 2-point discrimination) after surgery. All patients underwent radiological imaging, including standard radiographs in two planes (anteroposterior and lateral projections), carpal tunnel view and a CT study. From the CT, fractures were classified by their location as distal (close to the tip), central (middle third of the hamate hook), or proximal (at the base of the hamate hook).13, 14
Surgical technique
In all patients, ORIF of the hamate hook fracture was performed under regional anesthesia, with tourniquet control. A headless bone compression screw (Micro Acutrak screw, Acumed, Hillsboro, OR) was used in all patients. The surgical technique was similar to that described by Scheufler et al10, 15 and Bochoura et al.16 A Bruner-type incision was made starting just proximal to the wrist crease and extended over Guyon's canal. Skin flaps were elevated and the ulnar nerve and artery were identified proximally and followed distally, releasing Guyon's canal. The ulnar nerve was followed to its deep branch and the deep arterial branch and mobilized. The sensory branches of the ulnar nerve were also identified and mobilized. After protecting neurovascular structures and identifying the tip of the hamate hook, subperiosteal dissection was carried with blade scalpel to the base of the fracture. After reduction, a K-wire guide was introduced under fluoroscopic control, perpendicular to the tip of the hook and advanced through the fracture up to the hamate body bone. The drill bit was then introduced over the guide wire and after pre-drilling, appropriate screw length was introduced until the fracture gap was closed and compressed, and completely buried inside the bone (Fig. 1). A radiographic control was performed to confirm correct placement of the screw inside the bone (Fig. 2). Finally, the skin was approximated with interrupted 5-0 monofilament sutures.
Fig. 1.
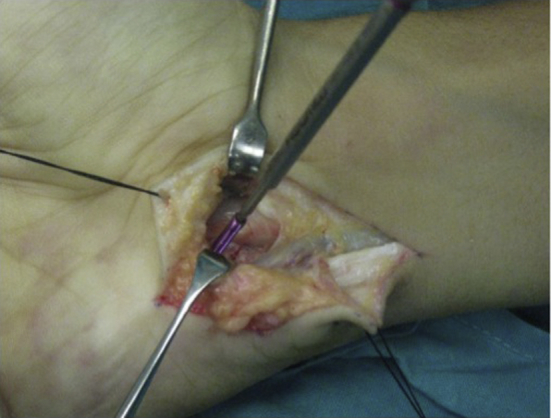
Intraoperative photograph showing screw insertion.
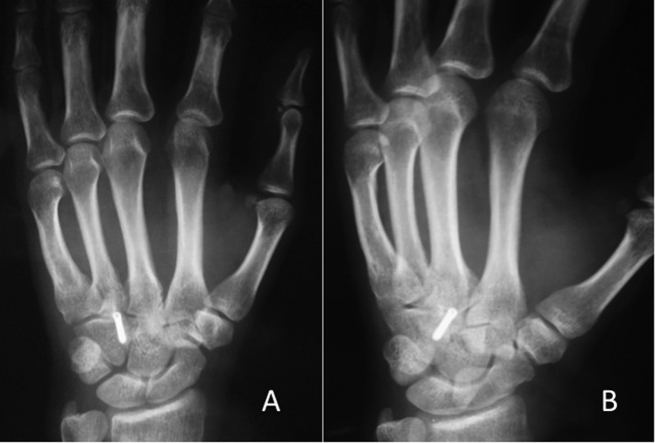
Fig. 2.
Radiographic confirmation of the correct position of the screw inside the hamate bone (A-Posteroanterior and B-Lateral).
Postoperative treatment
A plaster cast was applied with the wrist in slight extension. Finger exercises were encouraged after surgery. The plaster and sutures were removed 2 weeks after surgery. No physiotherapy was required. Return to normal daily activity including amateur sports was encouraged 12 weeks after surgery.
Outcome measurements
Functional outcomes evaluated were pain, range of motion (ROM), grip strength, Disabilities of the arm, shoulder and hand (DASH) and Mayo wrist score.
Pain was assessed using a visual analog scale (VAS) with scores ranging from no pain (0) to severe pain (10). The postoperative ROM (flexion-extension and radioulnar deviation) was measured with a goniometer and compared with the unaffected hand. Grip strength was measured bilaterally in all patients using the Jamar dynamometer (Sammons Preston, Inc., Bolingbrook, Illinois) and compared with the unaffected side.10 DASH scores were completed at the final follow-up. DASH was scored on a scale of 0–100, where 0 = no disability and 100 = most severe disability. For postoperative evaluation, we used the modified Mayo Wrist Score. This score includes measurements for pain, work status, ROM, and grip strength (0–100). A score of 90–100 points was considered excellent, 80–89 good, 65–79 fair and <65 poor.
Statistical analysis
Data were analysed using SPSS computer software system, version 21 (Chicago, IL, USA). The paired “t” test was used to evaluate differences in grip strength between hands treated by ORIF and unaffected hands.
Results
There were 12 men and 1 woman, with mean age of 32 years (range, 22–48 years). The mean follow-up was 36 months (range, 12–144 months). The etiology was 3 motorcycle accidents, 3 falls on the outstretched hand during a basketball game, 2 bicycle accidents, 2 direct hits by a golf club, 2 tennis racket traumas, and 1 unspecific accident while diving (Table 1). The right hand was affected in eleven cases.
Table 1.
Demographic data of patients with hamate hook fractures.
| Patients | Age (yr) | Sex | Fracture Type | Etiology |
|---|---|---|---|---|
| 1 | 24 | Male | III | Bicycle accident |
| 2 | 42 | Male | II | Tennis |
| 3 | 31 | Male | II | Motorcycle accident |
| 4 | 30 | Male | II | Motorcycle accident |
| 5 | 22 | Male | III | Basketball |
| 6 | 26 | Male | III | Motorcycle accident |
| 7 | 35 | Male | III | Bicycle accident |
| 8 | 37 | Male | III | Diving |
| 9 | 42 | Male | III | Golf |
| 10 | 34 | Male | III | Golf |
| 11 | 23 | Male | III | Basketball |
| 12 | 27 | Male | III | Basketball |
| 13 | 48 | Female | II | Tennis |
All patients had symptoms of pain over the hypothenar area of the hand. Eight patients complained of numbness, tingling and/or paresthesia in the ulnar nerve in the finger pulp of the ring and little fingers, with a positive Tinel's sign at Guyon's canal, symptoms and signs that usually present in neuritis of the ulnar nerve. We had two cases of preoperative involvement of the motor branch of the ulnar nerve and these patients required a neurolysis of the deep motor branch of the ulnar nerve. All patients who underwent neurolysis for preoperative ulnar nerve irritation accomplished complete relief from the numbness of the ring and little fingers. With regard to fracture classification, 3 cases fell into type II, and 10 into type III.
In no case was the fracture detected radiographically. Because of this and due to persistence of clinical symptoms a CT was performed, confirming the fracture in all cases. The average time from injury to correct diagnosis was 3.2 weeks (ranging 2 days to 9 weeks).
All 13 cases were treated by means of ORIF of the hook of the hamate. Mean VAS pain score was 5 preoperatively (4–9) and 1 (0–2) postoperatively. All patients returned to pre-injury level and only one patient felt pain on activity. Preoperative modified Mayo wrist score was 51 and the postoperative value was 94. All outcomes scores improved significantly from preoperative values. The patients who participated in amateur sports postoperatively were able to do so at or near pre-injury levels. Postoperative average ROM was 76° in extension, 71° in flexion, 14° in ulnar deviation, and 21° in radial deviation. ROM in the unaffected side was 74° in extension, 78° in flexion, 12° in ulnar deviation and 20° in radial deviation.
Mean grip strength in the hand with the hook fracture was 58 kg compared with 53 Kg in the unaffected hand. However, this difference was not statistically significant (Table 2). Fracture consolidation was confirmed in all cases by CT scan (Fig. 3).
Table 2.
Grip Strength testinga.
| Patients | Unaffected Hand (Kg.) | Affected Hand (Kg.) |
|---|---|---|
| 1 | 57 | 50 |
| 2 | 52 | 51 |
| 3 | 63 | 65 |
| 4 | 70 | 63 |
| 5 | 61 | 58 |
| 6 | 58 | 63 |
| 7 | 65 | 56 |
| 8 | 73 | 64 |
| 9 | 67 | 63 |
| 10 | 64 | 56 |
| 11 | 55 | 58 |
| 12 | 58 | 51 |
| 13 | 35 | 28 |
Measurement were performed at the end of the follow up with a Jamar dynamometer.
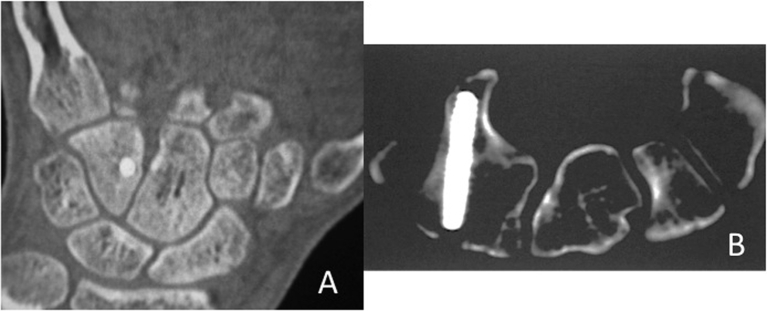
Fig. 3.
A) Coronal and B) Axial CT showing consolidation of the fracture.
Discussion
A high index of suspicion is required to correctly establish a diagnosis of hamate hook fracture after acute or chronic injuries over the hypothenar area of the hand, even when the radiographic study is negative. For this reason CT is the radiological modality of choice in the diagnosis of hamate hook fracture.1, 2, 3 MRI can rate the integrity of surrounding soft tissue but we do not consider it an essential test to diagnose this fracture. Initial management of hamate hook fractures can be conservative or surgical.7 Conservative treatment with lower arm cast immobilization has been advocated as first-line treatment in acute nondisplaced hook fractures.7, 12 However, this approach carries a high failure (nonunion) rate, especially when the diagnosis and casting are delayed. Surgical treatment of hamate hook fracture consists of fragment excision or ORIF.10, 15
ORIF constitutes the logical treatment of hamate hook fracture, because it restores the native anatomy and function of the carpal bone.15, 16 The effects of hamate hook excision lead to 4–5 mm of ulnar displacement of the little finger profundus tendon. Flexor tendon force decreases between 11% and 15%.2, 3, 4
In addition, depending on the degree of wrist flexion or extension, an increase of 7–11 mm in proximal excursion of the profundus tendon has been reported Demirkan et al17 concluded that the pulley effect of the hamate hook provides a biomechanical advantage for ulnar flexor tendon function and that excision may compromise power grip strength. Despite these biomechanical findings, however, a number of studies have shown that the final results of hamate hook excision are comparable to those of ORIF.10, 15 For this reason, excision of the hook remains the operation of choice for most surgeons, not only because there is more experience with this approach but also because patients can return to pre-injury activities soon after surgery and have no risk of fracture nonunion.12, 19
Bansal et al20 demostrated a higher rate of adverse events after surgical excision, approximately 25% compared with the existing literature. Transient ulnar nerve dysfunction was relatively common but all patients fully recovered by 5 months.
ORIF, in contrast with excision of the hook of hamate, has a longer recovery time and possible nonunion and/or hardware complications.20, 21 However, our results and those described in the literature with ORIF treatment are as good as those obtained with excision.10, 13, 14, 15, 18, 20
Conclusions
Based on evidence to date we believe that the ORIF for hamate hook fractures is a valid and effective approach to treatment, especially in patients with heavy physical work requirements who cannot tolerate a possible reduction in grip strength, as Scheufler et al suggests.9, 10 In cases of ulnar nerve neuritis, neurolysis of the deep palmar branch is mandatory.
Conflict of interest
There are no known conflicts of interest in the current manuscript in accordance with the International Committee of Medical Journal Editors Guidelines.
Funding
This work received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
All procedures were performed in accordance with the ethical standards of the authorized ethics committee for human experimentation (institutional and national) and the Helsinki Declaration of 1975, as revised in 2000.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Boulas H.J., Milek M.A. Hook of the hamate fractures: diagnosis, treatment, and complications. Orthop Rev. 1990;19(6):518–529. [PubMed] [Google Scholar]
- 2.O'Shea K., Weiland A.F. Fractures of the hamate and pisiform bones. Hand Clin. 2012;28(3):287–300. doi: 10.1016/j.hcl.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 3.Papp S.W. Carpal bone fractures. Orthop Clin North Am. 2007;38(2):251–260. doi: 10.1016/j.ocl.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Guha A.R., Marynissen H. Stress fracture of the hook of the hamate. Br J Sports Med. 2002;36(3):224–225. doi: 10.1136/bjsm.36.3.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kato H., Nakamura R., Horii E. Diagnostic imaging for fracture of the hook of the hamate. J Hand Surg Am. 2002;5(1):19–24. doi: 10.1142/s0218810400000090. [DOI] [PubMed] [Google Scholar]
- 6.Andresen R., Radmer S., Sparmann M., Bogusch G., Banzer D. Imaging of hamate bone fractures in conventional x-rays and high-resolution computed tomography: an in vitro study. Invest Radiol. 1999;34(1):46–50. doi: 10.1097/00004424-199901000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Whalen J.L., Bishop A.T., Linscheid R.L. Nonoperative treatment of acute hamate hook fractures. J Hand Surg Am. 1992;17(3):507–511. doi: 10.1016/0363-5023(92)90363-t. [DOI] [PubMed] [Google Scholar]
- 8.Stark H.H., Chao E.K., Zemel N.P., Rickard T.A., Ashworth C.R. Fracture of the hook of the hamate. J Bone Joint Surg Am. 1989;71(8):1202–1207. [PubMed] [Google Scholar]
- 9.Scheufler O., Radmer S., Erdmann D., Germann G., Pierer G., Andresen R. Therapeutic alternatives in nonunion of hamate hook fractures. Personal experience in 8 patients and review of literature. Ann Plast Surg. 2005;55(2):149–154. doi: 10.1097/01.sap.0000168697.05149.75. [DOI] [PubMed] [Google Scholar]
- 10.Scheuffler O., Andresen R., Radmer S., Erdmann D., Exner K., Germann G. Hook of hamate fractures: critical evaluation of different therapeutic procedures. Plast Reconstr Surg. 2005;115(2):488–497. doi: 10.1097/01.prs.0000149480.25248.20. [DOI] [PubMed] [Google Scholar]
- 11.Tolat A.R., Humphrey J.A., McGovern P.D., Compson J. Surgical excision of ununited hook of hamate fractures via the carpal tunnel approach. Injury. 2014;45(10):1554–1556. doi: 10.1016/j.injury.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Devers B.N., Douglas K.C., Naik R.D., Lee D.H., Watosn J.T., Weikert D.R. Outcomes of hook of hamate fracture excision in high-level amateur athletes. J Hand Surg Am. 2013;38(1):72–76. doi: 10.1016/j.jhsa.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 13.Scheufler O., Kamusella P., Tadda L., Radmer S., Russo S.G., Andresen R. High incidence of hamate hook fractures in underwater rugby players: diagnostic and therapeutic implications. J Hand Surg Am. 2013;18(3):357–363. doi: 10.1142/S0218810413500391. [DOI] [PubMed] [Google Scholar]
- 14.Xiong G., Dai L., Zheng W., Sun Y., Tian G. Clinical classification and treatment strategy of hamate hook fracture. J Huazhong Univ Sci Technol. 2010;30(6):762–766. doi: 10.1007/s11596-010-0654-7. [DOI] [PubMed] [Google Scholar]
- 15.Scheufler O., Radmer S., Andresen R. Dorsal percutaneous cannulated mini-screw fixation for fractures of the hamate hook. J Hand Surg Am. 2012;17(2):287–293. doi: 10.1142/S0218810412970039. [DOI] [PubMed] [Google Scholar]
- 16.Bachoura A., Wroblewski A., Jacoby S.M., Osterman L.A., Culp R.W. Hook of hamate fractures in competitive baseball players. Hand. 2013;8(3):302–307. doi: 10.1007/s11552-013-9527-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Demirkan F., Calandruccio J.H., Diangelo D. Biomechanical evaluation of flexor tendon function after hamate hook excision. J Hand Surg Am. 2003;28(1):138–143. doi: 10.1053/jhsu.2003.50005. [DOI] [PubMed] [Google Scholar]
- 18.Norman A., Nelson J., Green S. Fractures of the hook of hamate: radiographics signs. Radiology. 1985;154(1):49–53. doi: 10.1148/radiology.154.1.3964951. [DOI] [PubMed] [Google Scholar]
- 19.Kadar A., Bishop A.T., Suchyta M.A., Moran S.L. Diagnosis and management of hook of hamate fractures. J Hand Surg Eur. 2018;43(5):539–545. doi: 10.1177/1753193417729603. [DOI] [PubMed] [Google Scholar]
- 20.Bansal A., Carlan D., Moley J., Goodson H., Goldfarb C.A. Return to play and complications after hook of hamate fracture surgery. J Hand Surg Am. 2017;42(10):803–809. doi: 10.1016/j.jhsa.2017.06.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mandegaran R., Gidwani S., Zavareh A. Concomitant hook of hamate fractures in patients with scaphoid fracture: more common than you might think. Skeletal Radiol. 2018;47(4):505–510. doi: 10.1007/s00256-017-2814-3. [DOI] [PMC free article] [PubMed] [Google Scholar]