This case series evaluates the topical combination of fluorouracil and calcipotriene as a palliative therapy for refractory extramammary Paget disease.
Key Points
Question
Can a combination of fluorouracil and calcipotriene creams be used safely and effectively as a treatment for refractory extramammary Paget disease (EMPD)?
Findings
In this case series, we report 3 cases of refractory EMPD treated with a topical combination of fluorouracil and calcipotriene. The treatment was well tolerated and was followed by clinical improvement in all cases with demonstrated histopathological response in 2 of the cases.
Meaning
Topical combination of fluorouracil and calcipotriene may be a viable palliative treatment option for patients with refractory EMPD.
Abstract
Importance
Extramammary Paget disease (EMPD), a rare intraepithelial adenocarcinoma, poses a therapeutic challenge with high postoperative recurrence rates and a limited number of effective local treatment options.
Objective
To describe the use and efficacy of a topical combination of fluorouracil and calcipotriene as a palliative therapy for refractory EMPD.
Design, Setting, and Participants
This retrospective case series of 3 women with recurrent, refractory EMPD was conducted at Beth Israel Deaconess Medical Center, Boston, Massachusetts and Washington University School of Medicine, St Louis, Missouri. All patients were treated with a 1:1 mixture of fluorouracil, 5%, cream and calcipotriene, 0.005%, cream or ointment.
Main Outcomes and Measures
Clinical and histopathological findings.
Results
All 3 women (1 in her 50s, 2 in their 70s) presented with recurrent EMPD (vulvar, perianal, and perioral) after surgery and/or irradiation, and their EMPD was refractory to treatment with imiquimod, 5%, cream. Owing to disease progression and/or intolerable adverse effects from imiquimod, the patients began treatment with a 1:1 mixture of fluorouracil, 5%, cream and calcipotriene, 0.005%, cream. This treatment, which was well tolerated, was followed by clinical improvement in symptoms and appearance of the lesions in all 3 cases and histopathological signs of decreased tumor burden in 2 cases. Patients applied the combination topical therapy to affected areas with differing frequencies, ranging from 1 to 2 days per month to 4 consecutive days every 2 weeks.
Conclusions and Relevance
Extramammary Paget disease frequently recurs even after aggressive surgical management and can be refractory to many topical and locoregional therapies. Palliative treatment with a combination of fluorouracil and calcipotriene may be a viable option for patients with recurrent, refractory EMPD.
Introduction
Extramammary Paget disease (EMPD), an uncommon neoplasm of apocrine gland-bearing skin, is often difficult to manage.1 Wide local excision, the mainstay of treatment, carries significant morbidity and recurrence rates of up to 30%.2,3 Even treatment of primary disease with Mohs micrographic surgery has demonstrated local recurrence rates of 16%,4 although this may be reduced with the use of intraoperative immunostaining for cytokeratin-7.5 While irradiation and chemotherapy are also therapeutic options, the data on efficacy are limited.6,7 Alternative treatments such as imiquimod cream and topical fluorouracil monotherapy are described primarily in case reports or series.8,9,10 In this report, we present 3 cases that illustrate the use of combination topical fluorouracil and calcipotriene—a regimen that has been shown to successfully treat actinic keratoses and prevent skin cancer development in mouse models11—as a therapy for refractory EMPD.
Methods
One patient (case 1) was treated at the Washington University School of Medicine, and 2 patients (cases 2 and 3) were treated at the Beth Israel Deaconess Medical Center. Patients were instructed to mix fluorouracil, 5%, cream in a 1:1 weight ratio with calcipotriene, 0.005%, ointment or cream and apply a thin layer to affected areas twice daily for 4 to 6 consecutive days every 2 weeks.
Institutional review board approval and patient written informed consent were waived by the Beth Israel Deaconess Medical Center and Washington University School of Medicine for this report of 3 cases.
Report of Cases
Case 1
A woman in her 50s presented with an erythematous plaque involving the upper vermillion and cutaneous lip. The patient had known recurrent adenocarcinoma of the oral cavity, which had been treated with subtotal resection, irradiation, and systemic therapy including trastuzumab and capecitabine. Punch biopsy demonstrated adenocarcinoma with pagetoid spread, and she was initially treated with photodynamic therapy and imiquimod, 5%, cream. These therapies were discontinued when repeated biopsies showed no histological improvement in disease.
After 1 year without treatment, she was treated with 3 rounds of fluorouracil plus calcipotriene creams twice daily for 6 days every 3 weeks. This treatment was well tolerated and was followed by substantial clinical improvement (Figure 1A and B). Repeated biopsy after 9 weeks (3 cycles) of treatment demonstrated decreased density of intraepithelial adenocarcinoma cells (Figure 1C and D). Additional immunofluorescence staining revealed interval increase in the T cells and antigen-presenting cells, highlighting immune activation by combination therapy (Figure 2). The patient refused systemic therapy and surgery for her intraoral disease, which relapsed as a 2-cm adenocarcinoma of the hard palate.
Figure 1. Clinical and Histopathological Images of Refractory Extramammary Paget Disease in Case 1.
A, Thick erythematous plaque involving the upper vermillion and cutaneous lip. B, After 10 months of combination fluorouracil and calcipotriene therapy, there is significantly reduced thickness and erythema of the skin with resultant hypopigmentation. C and D, Cytokeratin-7 immunostaining of lesional specimens. C, Staining highlights extensive pagetoid scatter of atypical, neoplastic cells in the epidermis (original magnification ×100). D, After 9 weeks (3 cycles) of combination therapy, a repeated skin biopsy displays marked reduction in density of neoplastic cells (original magnification ×40).
Figure 2. Immunofluorescence-Stained Lesional Specimens From Case 1.
Immunofluorescence staining reveals T cells (CD3+, green) and human leukocyte antigen class II (HLA II)+ antigen-presenting cells (HLA II+, magenta) infiltrating refractory extramammary Paget disease lesional specimens before (A) and after (B) 9 weeks (3 cycles) of combination fluorouracil and calcipotriene therapy.
Case 2
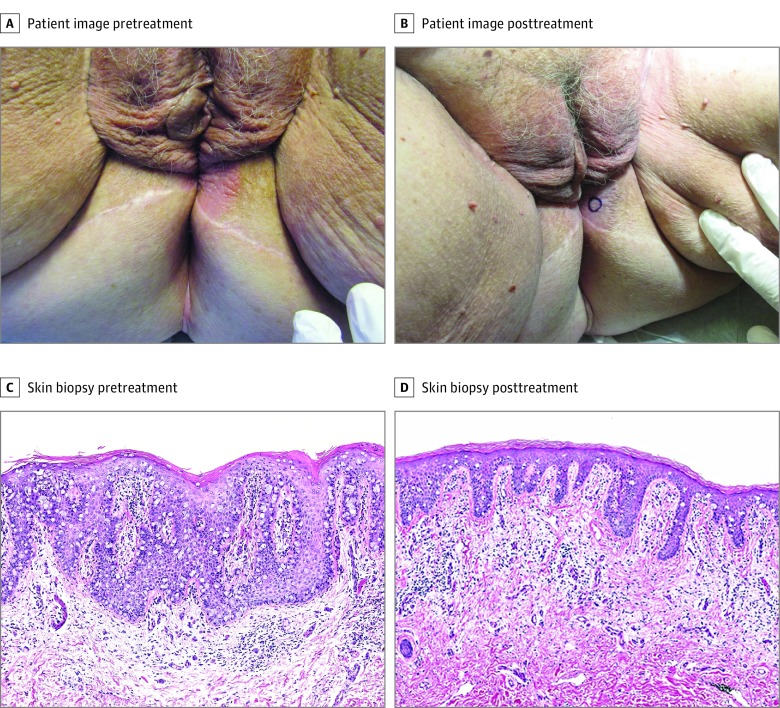
A woman in her 70s presented with persistent perianal EMPD within 1 year of wide local excision. A 5-month course of imiquimod, 5%, cream provided no substantial benefit. The disease progressed to involve the perineum, and she complained of fatigue and weakness. Her treatment regimen was transitioned to fluorouracil plus calcipotriene ointment twice daily for 3 to 4 days per month, and there was clinical improvement in lesion size and associated pruritus (Figure 3A and B). A punch biopsy acquired after initiation of treatment revealed a decrease in density of intraepidermal neoplastic cells with decreased appendageal involvement (Figure 3C and D).
Figure 3. Clinical and Histopathological Images of Refractory Extramammary Paget Disease (EMPD) in Case 2.
A, A 3-cm, well-demarcated, thin erythematous plaque on the left perineum extending to the left labia majora. B, Reduced erythema and peripheral extension of left perineal lesion after 8 months of combination therapy. C and D, Hematoxylin-eosin–stained lesional specimens (original magnification ×100). C, Pretreatment specimen reveals well-developed EMPD with a relatively high density of tumor cells and epidermal hyperplasia. D, After 8 months of combination fluorouracil and calcipotriene treatment, a repeated skin biopsy reveals a lower density of intraepidermal neoplastic cells, a less hyperplastic epidermis, and upper dermal changes that include superficial perivascular edema and lymphocytic inflammation.
Case 3
A woman in her 70s presented with a 20-year history of recalcitrant vulvar EMPD following wide local excision. At presentation, she began treatment with imiquimod with promising initial improvement. After 12 months, she experienced diminishing benefits with persistent, scattered, thin pink-red plaques involving the bilateral labia majora, mons pubis, and inguinal folds. In addition, she had fatigue, fevers, and difficulty swallowing associated with extended courses of treatment. After imiquimod therapy was discontinued, she transitioned to fluorouracil plus calcipotriene cream twice daily for 1 to 2 days. She tolerated this treatment well without significant adverse reactions and noted improvement in the thickness and peripheral inflammation of her lesions.
Discussion
Treatment of EMPD is challenging and complicated by morbid surgical or radiotherapy procedures with high rates of disease persistence and recurrence.4,5,6,7 Patients and clinicians often turn to alternative topical therapies, which are inconsistently effective.8
The 3 patients described herein presented with persistent or recurrent EMPD following surgical management. All patients were treated first with imiquimod, 5%, cream (as well as systemic and photodynamic therapy in case 1), which either failed to achieve sustained improvement or carried intolerable adverse effects. The combination therapy of fluorouracil and calcipotriene provided palliation and clinical improvement of previously refractory disease. Though their cutaneous disease did not fully clear, all patients tolerated the treatment and responded after a few applications with alleviated pruritus and discomfort, reduced thickness and peripheral extension of lesions, and decreased tumor burden in 2 cases.
The presumed mechanism of this proposed combination therapy relies on the synergistic immune-activating effects of fluorouracil and calcipotriene, whereby antigen-presenting cells are stimulated, and cytokines such as thymic stromal lymphopoietin induce T-cell immunity against the tumor.11 Our immunostained samples from case 1 further support this immune-mediated therapeutic effect.
Limitations
Our study offers preliminary observations and is limited by the small number of cases and the absence of a control group. While our limited experience has been promising, larger studies with longer follow-up are necessary to confirm this clinical benefit, identify optimal treatment parameters, and elucidate biological and immunological mechanisms of action. Clinicians and patients should uphold shared decision-making regarding the risks and benefits of this proposed palliative treatment option compared with other potentially more definitive options. Furthermore, a small subset of patients may have underlying invasive adenocarcinoma and an increased risk of noncontiguous carcinoma, which would not be addressed by this treatment modality.
Conclusions
Extramammary Paget disease is difficult to manage with the current treatment mainstays, surgery and irradiation, which provide inconsistent and often transient clinical benefit while carrying patient morbidity. Owing to the high recurrence rates despite aggressive management, there is an unmet need for effective, minimally invasive therapies to treat this intraepithelial adenocarcinoma with few off-target effects. Palliative treatment with a combination of fluorouracil and calcipotriene may be a novel option for patients with progressive or refractory EMPD.
References
- 1.Ibrahim SF, Grekin RC, Neuhaus IM. Mammary and extramammary Paget’s disease In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, eds. Fitzpatrick’s Dermatology in General Medicine. 8th ed New York, NY: McGraw-Hill; 2012:1372-1376. [Google Scholar]
- 2.Mengjun B, Zheng-Qiang W, Tasleem MM. Extramammary Paget’s disease of the perianal region: a review of the literature emphasizing management. Dermatol Surg. 2013;39(1, pt 1):69-75. doi: 10.1111/dsu.12019 [DOI] [PubMed] [Google Scholar]
- 3.Fanning J, Lambert HC, Hale TM, Morris PC, Schuerch C. Paget’s disease of the vulva: prevalence of associated vulvar adenocarcinoma, invasive Paget’s disease, and recurrence after surgical excision. Am J Obstet Gynecol. 1999;180(1, pt 1):24-27. doi: 10.1016/S0002-9378(99)70143-2 [DOI] [PubMed] [Google Scholar]
- 4.Hendi A, Brodland DG, Zitelli JA. Extramammary Paget’s disease: surgical treatment with Mohs micrographic surgery. J Am Acad Dermatol. 2004;51(5):767-773. doi: 10.1016/j.jaad.2004.07.004 [DOI] [PubMed] [Google Scholar]
- 5.Damavandy AA, Terushkin V, Zitelli JA, et al. . Intraoperative immunostaining for cytokeratin-7 during Mohs micrographic surgery demonstrates low recurrence rates in extramammary Paget’s disease. Dermatol Surg. 2018;44(3):354-364. [DOI] [PubMed] [Google Scholar]
- 6.Ye JN, Rhew DC, Yip F, Edelstein L. Extramammary Paget’s disease resistant to surgery and imiquimod monotherapy but responsive to imiquimod combination topical chemotherapy with 5-fluorouracil and retinoic acid: a case report. Cutis. 2006;77(4):245-250. [PubMed] [Google Scholar]
- 7.Itonaga T, Nakayama H, Okubo M, et al. . Radiotherapy in patients with extramammary Paget’s disease—our own experience and review of the literature. Oncol Res Treat. 2014;37(1-2):18-22. doi: 10.1159/000358161 [DOI] [PubMed] [Google Scholar]
- 8.Machida H, Moeini A, Roman LD, Matsuo K. Effects of imiquimod on vulvar Paget’s disease: a systematic review of literature. Gynecol Oncol. 2015;139(1):165-171. doi: 10.1016/j.ygyno.2015.07.097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen K, Liang H, Peng J, Zheng Y. Successful treatment of metastatic extramammary Paget’s disease with pemetrexed monotherapy systematically and 5-fluorouracil topically. Indian J Dermatol Venereol Leprol. 2018. doi: 10.4103/ijdvl.IJDVL_171_17 [DOI] [PubMed] [Google Scholar]
- 10.Del Castillo LF, Garcia C, Schoendorff C, Garcia JF, Torres LM, Garcia Almagro D. Spontaneous apparent clinical resolution with histologic persistence of a case of extramammary Paget’s disease: response to topical 5-fluorouracil. Cutis. 2000;65(5):331-333. [PubMed] [Google Scholar]
- 11.Cunningham TJ, Tabacchi M, Eliane JP, et al. . Randomized trial of calcipotriol combined with 5-fluorouracil for skin cancer precursor immunotherapy. J Clin Invest. 2017;127(1):106-116. doi: 10.1172/JCI89820 [DOI] [PMC free article] [PubMed] [Google Scholar]