Abstract
Accountable care organizations and health systems have the potential to increase patient engagement in medical care, improve population health outcomes, and reduce costs. Characteristics of highly integrated learning health care systems that seek to achieve these goals have been described in the literature. However, there have been few reports on how health systems, especially those that are loosely integrated, can develop the infrastructure needed to support achievement of these goals. In this report, we describe a learning community strategy that involved forming a coordinating team, a steering committee, and patient and stakeholder advisory committees to address cancer screening and disparities in 2 health systems in southeastern Pennsylvania—Jefferson Health and the Lehigh Valley Health Network. This project engaged diverse patients, health care providers, health system leaders, public and private payers, and other stakeholders in identifying and adapting evidence‐based methods to increase colorectal and lung cancer screening in primary care. Here, we describe components of a health system learning community. In addition, we describe activities in which different components of the learning community were engaged. Finally, we explore prospects for using this type of approach to catalyze the development of learning health care systems.
Keywords: cancer disparities, cancer screening, learning community, learning health care systems
1. BACKGROUND
The learning health care system (LHCS) model was initially proposed by the Institute of Medicine (now the National Academy of Medicine) Roundtable on Evidence‐Based Medicine in 2007.1 Conceptually, this model is intended to characterize a health care setting within which knowledge can be disseminated and new scientific discoveries can be implemented in order to continuously increase patient and family engagement, improve health care quality and value, and reduce the overall cost of care.
Greene et al2 proposed that a health system could purposefully organize itself to facilitate the movement of new information and interventions into practice, and, thus, facilitate the process of becoming an LCHS. Initiating that process would include identifying and characterizing high‐priority population health problems, integrating research evidence with staff experience to identify an evidence‐based intervention strategy to address the problems, adopting a multilevel approach to intervention implementation, conducting process and outcome evaluation, adjusting the intervention to fit population and organizational needs, and supporting implementation and dissemination of effective intervention strategies.
Kraft et al3 further defined the nature of this transformational process. They stated that the process involves developing an organizational culture of continuous learning, forming partnerships of patient and health care providers, locating responsibility for health system change in a center that is dedicated to guiding the transformational process in the health system, and devoting resources to support health system change. This work has been extended by Psek et al,4 who identified 9 components of an LCHS, including data and analytics, people and partnerships, patient and family engagement, ethics and oversight, evaluation and methodology, funding, organization, prioritization, and deliverables.
These and other such frameworks describe important features of an LCHS. However, they provide limited insight into how health systems, especially those that are loosely integrated, can begin to catalyze the process of moving evidence‐based practices into routine care. Below, we outline a learning community model based on organizational change and implementation science theory that can help guide this process. In addition, we illustrate how the model was operationalized in 2 health systems to address disparities in colorectal cancer and lung cancer screening. We also discuss the potential value of the model for catalyzing LCHS development.
2. A HEALTH SYSTEM LEARNING COMMUNITY MODEL
From 2015 to 2017, a Thomas Jefferson University‐led team launched the Reducing Cancer Disparities by Engaging Stakeholders (RCaDES) Initiative. The RCaDES Initiative was supported by the Patient‐Centered Outcomes Research Institute (EAIN 2471) and Thomas Jefferson University as a project to develop a theory‐based strategy to catalyze the process by which health systems can translate evidence‐based practices that address an existing health problem into routine care.
This strategy reflects the integration of constructs included in the Collective Impact Model and the Interactive Systems Framework (ISF) for Dissemination and Implementation. The Collective Impact Model calls for a “backbone organization” that is made up of health system leaders and stakeholders (eg, patients, providers, administrators, and community representatives), that catalyzes interactions among learning community members to advance a solution.
Initially, learning community members were guided through a process of achieving agreement on a common agenda that is focused on identifying an evidence‐based approach to achieving the desired change. The backbone organization brings organization leaders and other stakeholders (eg, payers, employers, and community organizations) together to identify important problems, identify an effective evidence‐based strategy that can address a priority need, and engage individuals affected by the problem to adapting and, ultimately, implementing the strategy.5, 6, 7
The ISF focuses on efforts to implement effective, evidence‐based interventions (or programs) in health systems. This model posits that health system change begins with an intervention synthesis stage, where the system recognizes an important health problem, and identifies a strategy that can address the problem, and explores the process of translating/adapting the chosen intervention strategy into practice.2, 8, 9 The framework includes a second stage, where the health system takes steps to ensuring optimal fit with the needs of the target population and the settings in which services are delivered, while maintaining the fidelity of the intervention process. The ISF also includes a final stage in which the intervention is implemented and steps are taken to facilitate intervention maintenance.
When considered together, these 2 frameworks form a multistage, multilevel model that can guide the process of catalyzing change in health systems. This integrated model, described here as the health system learning community model, was used to address cancer screening disparities in 2 health systems.
3. THE HEALTH SYSTEMS AND CANCER SCREENING
Jefferson Health (JH) is a rapidly growing regional health system with Thomas Jefferson University Hospital, the flagship teaching hospital of Thomas Jefferson University in Philadelphia. Other hospitals in the system include Jefferson Hospital for Neuroscience, Methodist Hospital in South Philadelphia, Abington Memorial Hospital in the northern suburb of Montgomery County, Aria Health in Northeast Philadelphia and Lower Bucks County, and Kennedy Health in southern New Jersey. JH serves a catchment area that includes more than 1,560,000 persons.
Based in Allentown, Pennsylvania, Lehigh Valley Health Network (LVHN) is the largest hospital in the Lehigh Valley and the flagship hospital of LVHN. The health system includes 4 full‐service hospitals: Lehigh Valley Hospital‐Cedar Crest in Salisbury Township (with additional clinical campuses at LVH‐17th Street in Allentown and LVHN‐Tilghman in West Allentown), LVH‐Muhlenberg in Bethlehem, LVH‐Hazleton in the Greater Hazleton area, and LVH‐Pocono in East Stroudsburg, with additional clinical campuses throughout Monroe County. Lehigh Valley Health Network serves a region of more than 800 000 individuals.
In 2015, the US Preventive Services Task Force (USPSTF), American Cancer Society, and a number of professional organizations recommended CRC screening for men and women who are asymptomatic for CRC and were 50 to 75 years of age.10, 11 At that time, the colorectal cancer (CRC) screening rate among age‐eligible patients served by JH primary care practices was 45% and was 57% in LVHN primary care practices. Colorectal cancer screening rates were lower among minority patients in JH and LVHN primary care practices. During that period, the USPSTF also recommended annual screening for lung cancer with low‐dose computed tomography (LDCT) in adults aged 55 to 80 years who have a 30 pack‐year smoking history and currently smoke or have quit within the past 15 years,12 and guidelines from the Centers for Medicare and Medicaid Services were similar.13 In 2015, LDCT screening rates for lung cancer (LCa) were below 5% in both health systems, and were comparable to rates reported elsewhere for this recently recommended screening test (CMS, USPSTF). LCa screening rates in the health system were low in the general primary care patient population and across patient population racial/ethnic groups.
4. OPERATIONALIZING THE HEALTH SYSTEM LEARNING COMMUNITY MODEL
As shown in Figure 1, the RCaDES Initiative operationalized the health system learning community model by developing a Coordinating Team and a Steering Committee. We also organized a Patient and Stakeholder Advisory Committee in each health system. Process and impact evaluations were conducted with members of all the components of the learning community throughout the 2‐year initiative.
Figure 1.
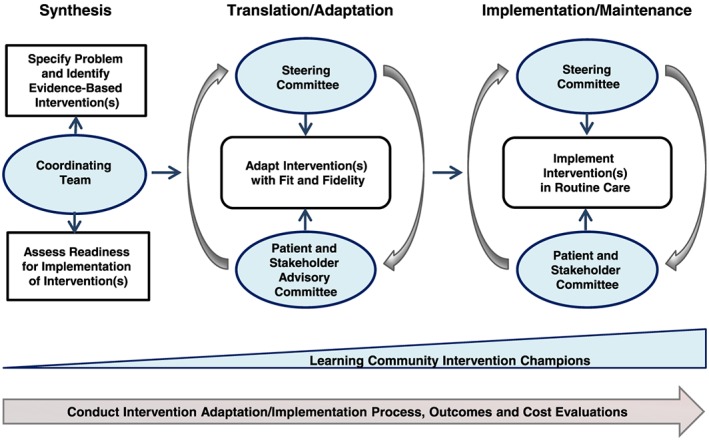
Health system learning community model
Coordinating Team (CT). Members of the CT included an interdisciplinary group of 9 individuals (researchers, primary and specialty care providers, health system administrators, and project managers) with experience in the field of cancer control and prevention implementation science, and program evaluation. The CT, which met on a weekly basis, assumed primary responsibility for forming a learning community that would guide the health systems in identifying, adapting, and implementing evidence‐based practices for reducing CRC and LCa screening disparities.
CT members initially adopted the following shared statement of purpose: “The RCaDES Initiative Coordinating Team will engage and support a learning community that includes health systems, stakeholders, and patients who represent vulnerable populations, in order to translate evidence‐based cancer screening interventions into practice and reduce cancer disparities.” In addition, the Coordinating Team developed the following common agenda: “The CT will (1) recruit SC and PASAC members, (2) catalyze interactions in the learning community, (3) measure screening disparities, (4) identify evidence‐based interventions and best practices, and (5) adapt evidence‐based interventions for implementation.”
To facilitate achievement of the common agenda of each component of the learning community, the CT implemented a continuous communication process that included meetings, emails, and a web‐based platform that allowed learning community members to share documents, complete tasks, and interact in real time. CT members coordinated meetings, developed meeting agendas, and assigned action items that guided all learning community members' activities.
Steering Committee (SC). SC members consisted of a diverse group of about 20 stakeholders and organizations, with members representing the major insurers in the region, along with a local employer coalition, representatives from each participating health system, members of the Jefferson community representing the Office of Diversity, the School of Population Health, and the Sidney Kimmel Cancer Center, state and local health department representatives, and nonprofit organizations with a stake in disparities as well as cancer prevalence. Patient and Stakeholder Advisory Committee (PASAC) representatives also attended the meetings. The SC met 4 times annually, for a total of 8 meetings throughout the RCaDES Initiative.
Initially, SC members adopted the following statement of purpose: “The RCaDES Initiative Steering Committee will review evidence‐based interventions, review screening rates and related disparities, review system readiness for intervention and identify factors likely to influence intervention use, and recommend strategies to support intervention adaptation and implementation.” The SC also developed the following common agenda: “The Steering Committee will work with the Coordinating Team and the Patient and Stakeholder Advisory Committees at JH and LVHN to (1) review health system data on lung cancer screening and disparities, (2) guide an environmental scan on screening interventions and programs, (3) help to identify evidence‐based screening interventions and program for adaptation, (4) recommend approaches for adaptation, and (5) address help to guide implementation.”
The committee also selected co‐leaders to assist in the development of meeting agendas and coordinate the meetings and activities between meetings. SC meeting agendas included a review of cancer screening rates, cancer screening disparities, and evidence‐based practices that could increase screening use. The SC also worked on assessing health system screening rates, identifying evidence‐based intervention practices to raise screening rates, achieving consensus on the need to adapt evidence‐based interventions to fit populations experiencing disparities, and on developing strategies for addressing intervention implementation barriers at the health system level.
The process outlined above is summarized in Figure 2.
Figure 2.
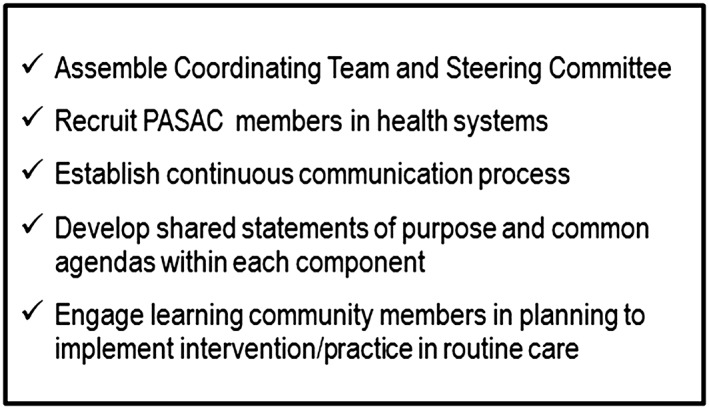
Learning community checklist
Patient and Stakeholder Advisory Committees (PASACs) . The PASACs in both health systems included approximately 12 racially and ethnically diverse patients from primary care practices within each system, primary care providers, specialists, care coordinators and patient navigators, and health system administrators with working knowledge of existing programs and interventions within the health system aimed to increase CRC and LCa screening rates.
Each PASAC adopted the following statement of purpose: “The Patient and Stakeholder Advisory Committee will work with the Coordinating Team and the Steering Committee to review and adapt evidence‐based interventions (EBIs) and programs for cancer screening to achieve good fit and fidelity in health systems and for populations experiencing cancer disparities in care, including African Americans, Hispanics/Latinos, and Asian Americans.” In terms of a common agenda, both PASACS adopted the following: “The Patient and Stakeholder Advisory Committee will work with the Coordinating Team and Steering Committee to review health systems screening disparities; identify evidence‐based screening interventions and programs and adapt screening interventions and programs to fit the needs of populations experiencing disparities in the health systems.”
Patient and Stakeholder Advisory Committee meetings were convened 6 times annually. During the initial meetings, to foster engagement, the CT worked with the PACACs to develop their shared statement of purpose and common agenda. Additionally, PASACs worked through a structured curriculum (year 1—CRC screening and year 2—LCa screening). The basic curriculum included the following modules: (1) building a learning community, (2) adapting educational materials for populations, (3) adapting an evidence‐based intervention/program for populations, (4) adapting interventions for health systems, (5) making recommendations for adapting educational materials for populations and health systems, and (6) making recommendations for adapting decision support contacts for populations and health systems.
Patient and Stakeholder Advisory Committee meetings focused on clarifying roles and responsibilities of learning community members, gaining insights into the core components of cancer screening interventions that might be selected by the health systems, learning about intervention adaptation and implementation, and specifying actionable objectives related to intervention adaptation to maximize intervention fit, fidelity, and effectiveness. The format of each session included group discussions and collaborative activities to develop intervention adaptation and pretesting skills. Group discussions also included presentations on cancer screening challenges experienced by patients, family, and community members as well as health system providers, administrators, and staff.
5. LEARNING COMMUNITY MEMBER ENGAGEMENT
5.1. CT members
Participation in CT meetings was consistently greater than 90%. The project evaluator conducted in‐person interviews with CT members at 6, 12, 18, and 24 months to assess how well the group was able to develop a leadership culture. Specifically, CT members were asked to evaluate their performance in establishing trust, achieving a shared commitment to a common agenda, agreeing to be accountable for task performance related to that agenda, helping to gain access to needed expertise, resolving conflicts effectively, and producing meaningful results. CT performance on each characteristic was rated on a 10‐point response set (not well at all = 1 to extremely well = 10). Responses were summed, and an average scale score was computed. Average scale scores were relatively high initially and improved over time: year 1 interview 1—7.7 and year 1 interview 2—8.4; year 2 interview 1—9.0 and year 2 interview 2—9.2.
5.2. SC member engagement
Steering Committee meeting attendance was good throughout the 2‐year project (median = 71%), ranging from 50% to 85% of members. In year 1, SC members focused attention on CRC screening. Primary goals for this component of the learning community were to achieve an understanding of the SC shared statement of purpose and common agenda related to CRC screening, and to achieve a high level of engagement in achieving the SC common agenda related to LCa screening. Steering Committee members were asked to complete an evaluation instrument that included items designed to measure how completely respondents felt that meeting primary goals had been achieved (not at all = 1, somewhat = 5, completely = 10). Average scores reported on the dimensions of understanding and engagement in year 1 were 8.0 and 7.8, respectively.
In year 2, SC meeting primary goals for the first and last meetings were to achieve understanding of the SC shared statement of purpose and common agenda related to LCa screening, and to achieve a high level of engagement in achieving the SC common agenda related to LCa screening. Again, we asked SC members if the common agenda had been achieved. The reporting format was modified, as “yes” and “no” response options provided. Affirmative responses to the understanding and achievement questions were 91% and 100%, respectively.
5.3. PASAC member engagement
During the project, JH and LVHN PASAC member meeting attendance ranged from 50% to 92% (median = 78%). In year 1, PASAC members were asked to report whether understood the group's shared statement of purpose and common agenda related to CRC screening. All of the participants responded in the affirmative. They were asked to indicate the extent to which they had been adequately engaged in the CRC screening intervention adaptation process. Response options for this measure were not at all = 1, somewhat = 2, much = 3, very much = 4. Respondents reported an average score of 3.6. In the second year of the project, we asked PASAC members if they understood the group's shared statement of purpose and common agenda related to LCa screening. Ninety‐four percent of respondents reported that they did understand these statements. We also asked PASAC members if they felt that they had been adequately engaged in the LCa screening program adaptation process. Response options for this variable were strongly disagree = 1 to strongly agree = 5. The average score was 5.0 (Table 1).
Table 1.
PASAC member understanding of and engagement in achieving common agenda
| Year | Measure | N | Response |
|---|---|---|---|
| 1 | Understanding the PASAC common agenda related to CRC screeninga | 19 | Agree = 100% |
| Engagement in achieving the PASAC common agenda related to CRC screeningb | 22 | Mean = 3.6 | |
| 2 | Understanding the PASAC common agenda related to LCa screeninga | 17 | Agree = 94% |
| Engagement in achieving the PASAC common agenda related to LCa screeningc | 11 | Mean = 5.0 |
0 = disagree, 1 = agree.
1 = not at all, 2 = somewhat, 3 = much, 4 = very much.
1 = strongly disagree, 3 = uncertain, 5 = strongly agree.
5.4. JH and LVHN PASAC member activities
During the project, JH and LVHN PASAC member meeting attendance ranged from 50% to 92% (median = 78%). During year 1, training for PASACs in both health systems focused on exploring CRC screening intervention informational content, audience level of understanding or acceptance, language and terminology, fit with population culture, channels of delivery, fidelity of intervention components, and intended actions.14 CT staff also trained PASAC members in screening intervention pretesting methods. More specifically, PASAC members participated in role play and other activities to prepare them to conduct pretesting activities with the adapted intervention with community members.
Patient and Stakeholder Advisory Committee members were then engaged in pretesting a CRC screening patient education brochure. This experience involved conducting focused interviews with 73 individuals in the community across the JH and LVHN catchment areas. Specifically, each PASAC member was asked to approach 3 to 5 community members. In each pretesting session, PASAC followed a structured guide to elicit interviewee impressions of a CRC screening patient educational booklet look and feel, the format and language that were used to present information, and graphics used to represent the population. Patient and Stakeholder Advisory Committee members discussed pretest findings, including the strengths, weaknesses, opportunities, and threats related to implementation of the print materials. Their review of the intervention pretest findings resulted in recommendations that included lowering the reading level of the print materials, indicating where to find additional information, and adding text on the likelihood of finding early stage disease through screening and related outcomes. It was also noted that a centralized health system approach to providing primary care patients with education about the support for screening should be considered.
The year 2 PASAC curriculum was modified to focus attention on understanding the recommended LCa screening guidelines and current approaches to screening in each of the health systems. Since LCa screening is a more recent development in clinical care than CRC screening, this step was intended to give PASAC members a deeper understanding of the recommendations and limitations in lung cancer screening. We expanded the PASAC membership to include health system personnel who were responsible for implementing their respective lung cancer screening programs since these are often different units or departments in the health systems. In PASAC meetings, members were able to review lung cancer screening methods, patient eligibility criteria, patient educational materials, and the descriptions of LCa screening program workflows. Discussions focused on the need to identify obstacles to participation and to determine how to improve the fit of existing programs to health system target population needs. Initially, CT staff and PASAC members decided to work on creating a patient‐oriented infographic and an LCa screening program patient educational page for use in screening program outreach to the community. PASAC members were also engaged in an effort to reach out to community members, family members or colleagues to pretesting these materials.
The pretesting effort involved the conduct of 52 interviews with community members to obtain feedback on informational content and presentation. Much of the feedback related to lowering the literacy level of the infographic, making the visual presentation of print information material more appealing for a culturally diverse audience, and explaining to patients and primary care providers how to determine screening eligibility. The development of a centralized strategy of screening program implementation to reach primary care patients was also recommended. Health system leaders and administrators were invited to attend the final JH and LVHN PASAC meetings, where PASAC members presented intervention pretesting results and had an opportunity to discuss how an adapted intervention could be implemented in the health systems.
The process described above is illustrated in Figure 3.
Figure 3.
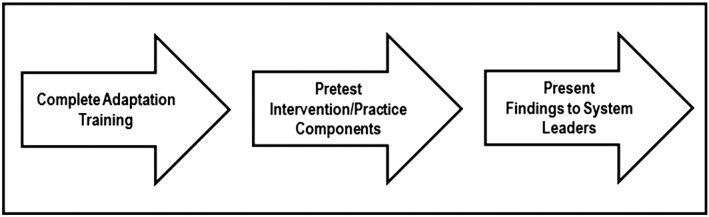
PASAC process
6. CONCLUSION
An integrated Health System Learning Community model guided the development of an organizational infrastructure that was intended to help 2 health systems determine how to raise CRC and LCa screening rates and reduce screening disparities in primary care patient populations. The nature of this infrastructure was shaped by the overarching goal of engaging health system patients, providers, leaders, and other stakeholders to develop and, ultimately, deploy intervention strategies that could have a collective impact on cancer screening rates, especially in populations experiencing disparities.15 This effort resulted in the formation of 3 learning community components, including the CT, SC, and PASACs in each health system.
Initially, the Center for Health Decisions formed a leadership group (CT) that was committed to ensuring that patients from populations targeted for screening, primary care providers, health system leaders, and other stakeholders were represented in the learning community. In addition, CT members embraced the challenge of guiding health system representatives through the process of learning about CRC and LCa screenings, identifying evidence‐based intervention strategies that could be used to address screening disparities, and learning how to obtain feedback from the community related to those strategies that could be used to improve current screening rates. As described by Kraft et al,3 a “unified center” to serve as a knowledge management resource is a key initial step in catalyzing change in a health system.
The SC, another core component of the learning community that represented health system leadership and stakeholders from other healthcare organizations, worked with the CT to review cancer screening data on health system CRC and LCa screening rates, to determine the existence of screening disparities among primary care patients, and to identify evidence‐based practices in CRC screening and LCa screening that could be adapted for implementation. SC members also engaged in discussions about the need to work closely with the PASACs and develop additional components of the learning community, as defined by Psek et al,16 especially as they relate to priority areas that are targeted for change.
As described earlier, the PASACs were the engines of change in each health system. PASAC members embraced the challenges of learning how to pretest those strategies by conducting interviews in the community, carrying out the pretests, and developing recommendations for adapting CRC screening and LCa screening intervention tools to fit the needs of patient populations. A range of talented individuals brought energy, commitment, and insights to this process each year, and recommended changes to improve the fit of selected intervention strategy patient education components to meet the needs of targeted patient populations identified in health system primary care practices. These recommendations have been shared with health system leaders responsible for addressing cancer screening, and deliberations are underway concerning how to implement recommended changes.
The operational approach of creating a multilevel infrastructure, carrying out data analysis and priority setting, promoting collaborative decision making related to the selection of evidence‐based intervention strategies, and supporting a systematic process of intervention strategy adaptation helped to achieve a high commitment at all levels from learning community members. Moreover, this effort required ongoing, intensive support and leadership from the CT to engage and support both the SC and PASACs also required the development of a user‐friendly communication system that linked participants and the implementation of a training that prepared PASAC members for and guided them through intervention strategy adaptation activities.
Shared themes across the various LCHS models highlight some key elements of a health system learning community: multistakeholder engagement, shared value and mission, identification of the problem, evidence‐based solutions commitment, and a sound operational approach. It is important to note that the RCaDES initiative was built on strong existing relationships with the 2 health systems and was expanded to include other organizations and community members. These relationships facilitated broad engagement and agreement on the shared mission.
As designed, the RCaDES Initiative facilitated the first steps in developing the health systems learning community and ongoing effort and commitment is necessary to continue to build and sustain this community. The project team has worked with health system leaders to prepare and submit research grant applications to the National Institutes of Health, the Patient Centered Outcomes Research Institute, and primary foundations. This effort aims to obtain support for applying the Health System Learning Community Model to address the problem of implementing CRC and LCa screening strategies in primary care patient populations. Recently, JH has received a 4‐year grant from the Bristol‐Myers Squibb Foundation (BMSF) to supports use of the health system learning community model to support the centralized implementation of LCa screening program that is intended to reach vulnerable populations (African American and Asian American residents of Philadelphia) served by JH.
In accordance with the Consolidated Framework for Implementation Research,17 the BMSF‐funded project will engage the CT and the SC in a structured process of identifying factors that are likely to affect the successful implementation in vulnerable populations, including (1) characteristics of the intervention program, (2) features of the health system inner setting, (3) features of the health setting external setting, (4) characteristics of individuals involved in implementation, and (5) intervention implementation steps. Patient and Stakeholder Advisory Committee members will also be engaged in identifying challenges to implementing the LCa screening program from the patient, provider, and community perspectives. During this process, we will develop recommendations on adapting the program to address identified obstacles.
Following the Plan, Study, Do, and Act (PSDA) model described by Langley et al,18 the SC will then define a series of steps that can be taken using existing technology (eg, health system EHR, decision support tools, and collaboration software applications) to implement change across the health systems. Ultimately, we will assess screening program performance in terms of its reach and effectiveness in raising LCa screening and smoking cessation rates. It is important to note that as a member of the RCaDES Initiative learning community, LVHN will participate in the BMSF‐funded project.
Finally, we believe that certain basic infrastructure components – a CT, an SC, and a health system PASAC – are essential to the process of catalyzing health system movement towards becoming an LCHS. Other organizational components that ensure a well‐integrated process of learning (eg, health system senior leadership, data and analytics, funding and resource development, ethics and oversight, evaluation and methodology) are also needed to achieve optimal results.19
In the context of the RCaDES Initiative, we purposefully focused attention on CRC and LCa screening to enhance cancer prevention and control activities in 2 health systems. Much work remains to address issues related to the development of programs that address the continuum of care related to CRC and LCa after screening. Further work is needed to explore how the model described here can be applied to move help health systems become active participants in the process of moving evidence‐based practices related to cancer and other diseases into routine care.
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
ACKNOWLEDGEMENTS
This project was funded in part by the Patient Centered Outcomes Research Institute (PCORI) 080‐27000‐U07301 and Thomas Jefferson University. We would also like to acknowledge Brian Stello, MD, Beth Careyva, MD, Melanie Johnson, MPA, and Kyle Shaak, MPH, who were instrumental in organizing and helping to guide the LVHN PASAC.
Myers RE, DiCarlo M, Romney M, et al. Using a health system learning community strategy to address cancer disparities. Learn Health Sys. 2018;2:e10067 10.1002/lrh2.10067
REFERENCES
- 1. Institute of Medicine (IOM) . The Learning Healthcare System: Workshop Summary (IOM Roundtable on Evidence‐Based Medicine) [Internet]. Roundtable on Evidence‐Based Medicine. 2007;374 http://www.ncbi.nlm.nih.gov/books/NBK53488/
- 2. Greene SM, Reid RJ, Larson EB. Implementing the learning health system: from concept to action. Ann Intern Med. 2012. Aug 7;157(3):207‐210. [DOI] [PubMed] [Google Scholar]
- 3. Kraft S, Caplan W, Trowbridge E, et al. Building the learning health system: describing an organizational infrastructure to support continuous learning. Learn Heal Syst. 2017. Oct 1;1(4):e10034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Psek WA, Stametz RA, Bailey‐Davis LD, et al. Operationalizing the learning health care system in an integrated delivery system. EGEMS (Washington, DC). 2015;3(1):1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McMillan DW, Chavis DM. Sense of community: a definition and theory. J Community Psychol. 1986;14(1):6‐23. [Google Scholar]
- 6. Smith M, Saunders R, Stuckhardt L, Mcginnis JM. (Eds). Best care at lower cost: the path to continuously learning health care in America. Committee on the Learning Health Care System in America; Institute of Medicine; 2012:450. [PubMed] [Google Scholar]
- 7. Collective Impact [Internet] . [accessed 2018 May 10]. https://ssir.org/articles/entry/collective_impact
- 8. Wandersman A, Duffy J, Flaspohler P, et al. Bridging the gap between prevention research and practice: the interactive systems framework for dissemination and implementation. Am J Community Psychol. 2008;41(3–4):171‐181. [DOI] [PubMed] [Google Scholar]
- 9. Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. 2015;10(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. U.S. Preventive Services Task Force . Screening for colorectal cancer: U.S. Preventive services task force recommendation statement. Ann Intern Med. 2008;149(9):627‐637. [DOI] [PubMed] [Google Scholar]
- 11. American Cancer Society. American Cancer Society Recommendations for Colorectal Cancer Early Detection [Internet] . [accessed 2017 Jul 17]. https://www.cancer.org/cancer/colon‐rectal‐cancer/detection‐diagnosis‐staging/acs‐recommendations.html
- 12. Final Update Summary: Lung Cancer: Screening ‐ US Preventive Services Task Force [Internet]. [accessed 2018 May 10]. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/lung‐cancer‐screening
- 13. CMS . Medicare Coverage of Screening for Lung Cancer with Low Dose Computed Tomography (LDCT). 2015. [accessed 2018 May 10]; https://www.cms.gov/Outreach‐and‐Education/Medicare‐Learning‐Network‐MLN/MLNMattersArticles/Downloads/mm9246.pdf
- 14. Putting Public Health Evidence in Action Training Workshop|CPCRN [Internet]. [accessed 2018 May 10]. http://cpcrn.org/pub/evidence‐in‐action/
- 15. Aragón TJ, Garcia BA. Designing a learning health organization for collective impact. J Public Heal Manag Pract. 2015;21:S24‐S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Psek W, Davis FD, Gerrity G, et al. Leadership Perspectives on Operationalizing the Learning Health Care System in an Integrated Delivery System. EGEMS (Washington, DC) [Internet]. 2016. [Accessed 2018 May 10;4(3):1233 http://www.ncbi.nlm.nih.gov/pubmed/27683668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Keith RE, Crosson JC, O'Malley AS, Cromp DA, Taylor EF. Using the Consolidated Framework for Implementation Research (CFIR) to produce actionable findings: A rapid‐cycle evaluation approach to improving implementation. Implement Sci. 2017;12(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Langley G, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. Quality. 2009;512. [Google Scholar]
- 19. Platt J, Spector‐Bagdady K, Platt T, et al. Ethical, legal, and social implications of learning health systems. Learn Heal Syst [Internet]. 2018. Jan 1; accessed 2018 May 102(1):e10051 10.1002/lrh2.10051 [DOI] [PMC free article] [PubMed] [Google Scholar]


