Abstract
Anxiety disorders are prevalent and significantly impact young children and their families. One hypothesized risk factor for anxiety is heightened responses to sensory input. Few studies have explored this hypothesis prospectively. This study had two goals: (1) examine whether sensory over-responsivity is predictive of the development of anxiety in a large prospective sample of children, and (2) identify whether anxiety mediates the relationship between sensory over-responsivity and behavioral challenges. Children’s sensory and anxiety symptoms were assessed in a community sample of 917 at 2-5 and again in 191 of these children at 6 years old. Parents also reported on a number of additional behavioral challenges previously found to be associated with both sensory over-responsivity and anxiety separately: irritability, food selectivity, sleep problems, and gastrointestinal problems. Forty three percent of preschool children with sensory over-responsivity also had a concurrent impairing anxiety disorder. Preschool sensory over-responsivity symptoms significantly and positively predicted anxiety symptoms at age six. This relationship was both specific and unidirectional. Finally, school-age anxiety symptoms mediated the relationship between preschool sensory over-responsivity symptoms and both irritability and sleep problems at school-age. These results suggest sensory over-responsivity is a risk factor for anxiety disorders. Furthermore, children who have symptoms of sensory over-responsivity as preschoolers have higher levels of anxiety symptoms at school-age, which in turn is associated with increased levels of school-age behavioral challenges.
Keywords: Pediatric Anxiety, Sensory Over-Responsivity, Risk Factors, Preschool
Pediatric anxiety is common, is associated with significant impairment, and is predictive of later psychopathology and impairment (Costello et al. 2005; Bittner et al. 2007; Copeland et al. 2009; Egger and Angold 2006). Many current interventions focus on alleviating symptoms in older children and adults who already suffer from an anxiety disorder. By the time most children receive these treatments, they have already developed a number of co-occurring behavioral challenges, including difficulties with sleep, recurrent stomachaches, and increased irritability, that further impair both the child and their family’s functioning (Dougherty et al. 2013; Towe-Goodman et al. 2014; Shanahan et al. 2014). To prevent the significant impairment that results from anxiety, treatments need to target premorbid child behaviors or features associated with risk for anxiety. This strategy would aim to reduce or prevent the onset of both anxiety symptoms and associated co-occurring behavioral challenges.
One potential risk factor for anxiety is sensory over-responsivity. Sensory over-responsivity is characterized by heightened and unusual reactions to everyday sensory stimuli, such as the sound of a blender or the feel of a shirt tag (Green and Ben-Sasson 2010; Green et al. 2012; Conelea et al. 2014). The bulk of research on sensory over-responsivity has been done within the context of autism research due to the high prevalence rate and impairment associated with sensory over-responsivity in this clinical group. However, there is evidence supporting sensory over-responsivity as a common comorbidity across a number of psychiatric disorders and it has been shown to affect between 8% and 28% of otherwise typically-developing, disorder-free children (Ben-Sasson et al. 2009, 2010; Carter et al. 2011; C. Van Hulle et al. 2015; Baranek et al. 2006). In the autism literature, symptoms of sensory over-responsivity have been linked to higher levels of both aggression and food selectivity, as well as lower levels of social and adaptive behaviors (Boyd et al. 2010; Cermak et al. 2010; O'Donnell et al. 2012). Additionally, higher levels of sensory over-responsivity are associated with a number of co-occurring difficulties that are also common in children with anxiety, including chronic GI symptoms (Mazurek et al. 2013), sleep disturbance (Hallett et al. 2013; Mazurek and Petroski 2015), and increased parental stress (Ben-Sasson et al. 2013). Thus, sensory over-responsivity is relatively common in young children, significantly impacts both the child and their parents, and may be a risk factor for anxiety.
Several studies have demonstrated that sensory over-responsivity is associated with emotion dysregulation and anxiety in typically developing children, as well as in individuals with autism spectrum disorder, ADHD, and anorexia nervosa (Reynolds and Lane 2009; Mangeot et al. 2001; Green and Ben-Sasson 2010; Green et al. 2012; Pfeiffer et al. 2005; Bitsika et al. 2016; Ben-Sasson et al. 2009; Carter et al. 2011; Farrow and Coulthard 2012; Conelea et al. 2014; Goldsmith et al. 2006; Engel-Yeger and Dunn 2011; Merwin et al. 2013). Despite evidence for a positive correlation between sensory over-responsivity and anxiety across a number of populations, the longitudinal relationship between early sensory over-responsivity and later anxiety has only been demonstrated in a single study of preschoolers with autism (Green et al. 2012). No study has explored sensory over-responsivity as an early emerging risk factor for the development of anxiety in children without autism. As such, the goal of the current study was to establish whether sensory over-responsivity is also a risk factor for anxiety in typically-developing children for whom sensory challenges are not part of a larger diagnostic syndrome.
In summary, previous research has demonstrated:
-
1)
Sensory over-responsivity (A) and anxiety (B) are associated with one another in both clinical and non-clinical samples (A to B);
-
2)
In children with autism, sensory over-responsivity (A) is associated with increased levels of behavioral challenges (C; A to C);
-
3)
There is a relationship between anxiety (B) and these same behavioral challenges (C) in non-ASD children (B to C).
However, no one has directly explored whether anxiety mediates the relationship between sensory over-responsivity and challenging behaviors (Figure 2a). Furthermore, sensory over-responsivity as a predictor of anxiety has not been demonstrated in a longitudinal sample of children without autism.
Fig. 2.
Panel a depicts the hypothesized mediation model whereby school-age anxiety symptoms mediate the relationship between sensory over-responsivity symptoms and behavioral challenges. Panels b-c depict the results of our mediation analyses, which demonstrate that school-age anxiety symptoms mediate the relationship between preschool sensory over-responsivity symptoms and both irritability (panel b) and sleep problems (panel c) at school-age. C1 represents the direct effect of preschool sensory over-responsivity symptoms and each negative outcome adjusting for preschool anxiety symptoms. All parameter estimates are unstandardized. Indirect effects are defined as the product of the a and b paths. The statistical significance of the indirect effect was tested with 95% confidence intervals calculated from a bootstrapping procedure using 10,000 samples.
The current study aims to build upon this previous literature by exploring the relationship between sensory over-responsivity and anxiety in a sample of children recruited from pediatric primary care and assessed longitudinally as part of the Duke Center for Developmental Epidemiology’s Preschool Childhood Anxiety studies. It has been hypothesized that sensory over-responsivity can lead to anxiety through conditioning (Green and Ben-Sasson 2010). For example, a child who suffers from sensory over-responsivity in the auditory domain may find that many experiences, such as going to a restaurant or using a public bathroom, are associated with unpredictable and uncontrollable auditory input that they experience as unpleasant. This may lead the child to maintain a state of hypervigilance and hyperarousal, which in turn leads to the development of an impairing anxiety disorder (Green and Ben-Sasson 2010). Based on this model, we hypothesized that preschool children with sensory over-responsivity would be more likely to have concurrent anxiety disorders and that preschool sensory over-responsivity symptoms would predict anxiety symptoms at school-age. Furthermore, we used mediation analyses to explore the hypothesis that anxiety mediates the relationship between sensory over-responsivity and behavioral challenges, such as sleep difficulties and food selectivity, in young children.
Methods
Study Design and Participants
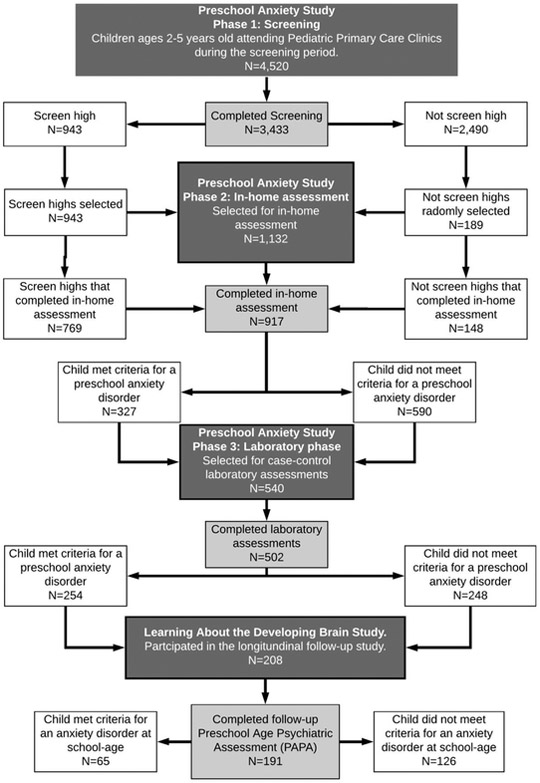
The study design and methods were approved by Duke University School of Medicine Institutional Review Board (IRB). Before the initiation of each study phase, the parent or legal guardian signed informed consent forms approved by the Duke IRB. The participants in this study were part of a set of studies that longitudinally assessed mental health in a large sample of preschool-age children. Figure 1 depicts the design of the two linked studies from which this sample was drawn.
Fig. 1.
Sampling design for the longitudinal studies: the Duke Preschool Anxiety Study and the Learning About the Developing Brain Study
Baseline Sample (N = 917): Duke Preschool Anxiety Study.
A representative sample of children were recruited through primary care clinics as part of the Duke Preschool Anxiety Study, a population-based, screen-stratified study of anxiety in children ages two to five years old. The Duke Preschool Anxiety Study was a three part study that included a screening phase (N = 3,433), an in home assessment phase (N = 917), and a case-control multi-modal (questionnaires, observational and experimental measures) laboratory phase (N = 502) (Franz et al. 2013). Children were screened into the study using a tool developed to assess risk for anxiety disorders based on data from an earlier study (Egger et al. 2006). Children were identified as screen positive if the parents endorsed 4 or more of the 10 items on this screener. All children with a positive screen, plus a random sample of the remaining children, were recruited for the in home assessment phase. This oversampling approach allows us to estimate the prevalence of common psychiatric disorders. By applying weights inversely proportional to selection probability, results are unbiased and representative of the screened population (Pickles et al. 1995). Children in the in home phase who screened positively were similar to children who did not screen positively in sex (χ2=0.37, p = .54) and age (t(908) = 1.50, p =0.13). They differed, however, in their race (χ2=11.58, p < 0.001), with significantly more white children screening low. Table 1 describes the demographic characteristics of the 917 children who participated in the in home phase study sample, which comprises the baseline sample for the current study.
Table 1.
Sample Demographics of Baseline Sample (N=917)
| No Preschool Sensory Over- Responsivity (N=624; 79.5%) |
Preschool Sensory Over-Responsivitya (N=293; 20.5%) |
Statisticse | |
|---|---|---|---|
| Age at Baseline | |||
| Years [Mean (SD)] | 3.97 (1.37) | 3.84 (0.97) | t (914) = 1.3, p = .20 |
| Sex | |||
| Female | 305 (49.8%) | 146 (59.4%) | χ2(1) = 5.4, p = .02 |
| Male | 319 (50.2%) | 147 (40.7%) | |
| Ethnicity/Race | |||
| African American | 275 (31.4%) | 109 (35.8%) | χ2(3) = 2.2, p = .53 |
| Caucasian | 223 (47.4%) | 124 (44.9%) | |
| Hispanic | 69(13.4%) | 35 (10.6%) | |
| Other | 57 (7.9%) | 25 (8.8%) | |
| Povertyb | |||
| Below Federal Poverty Line |
114 (10.2%) | 54(18.7%) | χ2(1) = 9.6, p < .002 |
| Preschool Anxiety Disordersc |
|||
| Any Anxiety | 175 (13.3%) | 152 (43.3%) | χ2(1) = 85.6,p < .001 |
| Generalized Anxiety | 86 (5.9%) | 89 (18.9%) | χ2(1) = 32.3, p < .001 |
| Separation Anxiety | 94 (5.6%) | 100 (29.8%) | χ2(1) = 92.9, p < .001 |
| Social Phobia | 67 (5.7%) | 68 (14.4%) | χ2(1) = 16.3, p < .001 |
| Other Preschool Disorders | |||
| Any Other Disorderd | 106 (8%) | 84 (21%) | χ2(1) = 24.3, p < .001 |
Note. With the exception of age, all values are N (%), where the N’s are absolute numbers and the percentages are weighted back to original screening sample of 3,433 children.
For this analysis, preschool sensory over-responsivity was modeled as a dichotomous variable. Children were included in the preschool sensory over-responsivity group if they met criteria for at least one sensory over-responsivity on the PAPA.
Poverty status was not reported for 73 children.
For this analysis, preschool anxiety disorders were modeled dichotomously. Children had to meet diagnostic an impairment criteria for each disorder to be included in the group.
Other disorders included ADHD, conduct disorder, depression, and oppositional defiant disorder.
Differences between the no preschool sensory over-responsivity and the preschool sensory over-responsivity groups were tested with chi-square statistics and t-tests. Numbers in parentheses represent degrees of freedom and p-values are for the weighted analyses.
All children (N = 327) who met criteria for generalized anxiety (GAD), separation anxiety (SAD), and/or social phobia were invited to participate in the laboratory phase of the Preschool Anxiety Study. Of these children, 254 participated in the laboratory assessment phase of the study (Figure 1). A random sample of children from the non-anxious group, stratified by age and gender, were also invited to participate in the laboratory assessment phase of the study. Of the 502 children who participated in this phase of the study, the children who met criteria for anxiety were similar in age, sex, and race to children who were in the non-anxious group. Inclusion criteria for the Preschool Anxiety Study were (i) the child was between 24 and 71 months old and (ii) the child attended the pediatric clinic during a screening period. Exclusion criteria were (i) the child was not accompanied by a parent/legal guardian who could provide consent, (ii) the parent/legal guardian lacked adequate fluency in English to complete the screen, (iii) the index child was known to have an IQ < 70, autism, or other pervasive developmental disorder, (iv) the child’s sibling was participating in the study, or (v) the provider decided that the child was too medically ill at the visit for the parent to be approached about the study. Detailed descriptions of the diagnostic assessments used to determine eligibility and the rationale for inclusion criteria have been described previously (Egger et al. 2006; Franz et al. 2013; Zucker et al. 2015).
Longitudinal Follow-Up Sample (N = 191): Learning About the Developing Brain Study.
Children who participated in the case-control laboratory phase of the Preschool Anxiety Study were recruited to take part in a five year prospective, longitudinal study of early childhood brain development and anxiety disorders. Children were eligible for the Learning About the Developing Brain (LADB) study if they participated in the third phase of the Preschool Anxiety Study and were between the ages of 4 and 8 during the first wave of data collection. Of the 452 eligible children, a random sample of 309 were contacted about participation in the LADB study. Of the 309 families, we were unable to reach and/or schedule 67 families, 15 refused to participate in the study, and 19 were scheduled but failed to show up at their laboratory appointments. The final sample size for the Learning About the Developing Brain Study consisted of 208 children, of which 191 parents completed a follow-up interview with the Preschool-age Psychiatry Assessment (PAPA, described below). These 191 children comprised the longitudinal follow-up sample for the current study. Of these children, 127 (61%) met criteria for an anxiety disorder when they were 2-5 years old. Table 2 describes the demographic characteristics of the 191 children who comprised the follow-up sample.
Table 2.
Sample Demographics of Longitudinal Sample (N=191)
| No Preschool Sensory Over-Responsivity (N=126, 80.4%) |
Preschool Sensory Over-Responsivitya (N=65, 19.6%) |
Statisticsd | |
|---|---|---|---|
| Age at Follow-up | |||
| Years [Mean (SD)] | 6.74 (0.70) | 6.68 (0.39) | t(l 88) = 0.6, p = .57 |
| Sex | |||
| Female | 73 (60.4%) | (64.5%) | χ2(1) = 0.2, p = .63 |
| Male | 53 (39.6%) | 33 (35.5%) | |
| Ethnicity/Race | |||
| African American | 70 (44.2%) | 27 (39.2%) | χ2(1) = 4.7, p = .20 |
| Caucasian | 34 (35.9%) | 27 (52.0%) | |
| Hispanic | 12 (13.8%) | 9 (7.3%) | |
| Other | 10 (6.1%) | 2 (1.53%) | |
| Povertyb | |||
| Below Federal Poverty Line |
28 (13.9%) | 21 (28.8%) | χ2(1) = 4.5, p = .03 |
| School-age Anxiety Disordersa | |||
| Any Anxiety | 38 (14.9%) | 27 (51.9%) | χ2(1) = 25.2, p < .001 |
| Generalized Anxiety | 21 (8.4%) | 19 (36.9%) | χ2(1) = 21.4, p < .001 |
| Separation Anxiety | 10 (2.0%) | 10 (8.12%) | χ2(1) = 3.8, p = .05 |
| Social Phobia | 13 (5.7%) | 7 (14.13%) | χ2(1)= 3.3, p = .07 |
| Other School-age Disorders | |||
| Any Other Disorderc | 20 (7.1%) | 14 (11.4%) | χ2(1) = 0.8, p = .37 |
| School-age Sensory Over-Responsivitya | 26 (15.6%) | 32 (56.11%) | χ2(1) = 28.9, p < .001 |
Note. With the exception of age, all values are N (%), where the N’s are absolute numbers and the percentages are weighted back to original screening sample of 3,433 children.
School-age anxiety, school-age other disorders, and both preschool and school-age sensory over-responsivity were all modeled as dichotomous variables. Children were included in the preschool sensory over-responsivity group if they met criteria for at least one sensory over-responsivity on the PAPA.
Poverty status was not reported for 73 children.
Other disorders included ADHD, conduct disorder, depression, and oppositional defiant disorder.
Differences between the no preschool sensory over-responsivity and the preschool sensory over-responsivity groups were tested with chi-square statistics and t-tests. Numbers in parentheses represent degrees of freedom and p-values are for the weighted analyses.
Preschool Age Psychiatric Assessment
Children were assessed using the Preschool Age Psychiatric Assessment (PAPA; Egger et al. 2006). The PAPA was administered in the in-home assessment phase of the Preschool Anxiety Study when the children were two to five years old and repeated as part of the Learning About the Developing Brain study when the children were six years old.
The PAPA is a comprehensive parent/caregiver reported interview that assesses symptoms for a range of psychiatric disorders in preschool age children. In the current study, interviewers were trained to fidelity through a multi-step process that included two weeks of in classroom training on the instrument, followed by live observation of the trainer conducting at least 4 on-study interviews. Once this was complete, each interviewer conducted a minimum of 10 on-study interviews that were reviewed by the trainers, who provided the trainee with structured comments and feedback on both the administration and the scoring of the PAPA. Every interview was checked by an expert interviewer to insure fidelity to the instrument glossary and once a week audio from an interview was randomly selected to be reviewed by the entire study team to insure against interviewer drift and fidelity of coding.
A study of the test-retest reliabilities of the PAPA (Egger et al. 2006) concluded that the diagnostic reliability of the PAPA is on a par with those achieved by older child, adolescent and adult psychiatric interviews, with kappas ranging from 0.36 to 0.79. Further, test-retest intraclass correlations for DSM-IV syndrome scale scores ranged from 0.56 to 0.89. The mean test-retest interval was 11 days and the second interview was completed by a new interviewer who was blind to the results of the first. As such, the results of the test-retest study of the PAPA suggest that there is reasonable concordance between interviews done within 2 weeks of one another by different interviewers.
Anxiety.
Children were identified as either (A) meeting both symptom and impairment criteria for GAD, SAD, and/or social phobia (disorder present) or (B) not meeting criteria for these anxiety disorders (disorder absent). To avoid tapping into normative fears, impairment from anxiety was required for all anxiety diagnoses. Additionally, a continuous anxiety symptom count variable was created by summing the individual symptoms of GAD, SAD, and social phobia for each subject. Although the PAPA measures a number of additional disorders (e.g. panic, specific phobia, OCD, etc), the Preschool Anxiety Study and the Learning about the Developing Brain study were designed to focus only on GAD, SAD, and social phobia. As such, these were the anxiety disorders that were explored in the current study.
Sensory Over-Responsivity.
Sensory over-responsivity was measured at both baseline and follow-up with the PAPA. Children were coded as “0” if there was no evidence of sensory over- responsivity or “2” if the sensory experience (e.g. being touched) resulted in the child becoming emotionally upset, the child becoming physically aggressive, or the child physically withdrawing. Sensory over-responsivity was measured in response to nine sensory experiences:1) physical contact with other people; 2) contact with fabrics, clothes tags, etc.; 3) contact with food textures; 4) visual experiences (e.g. reaction to bright or harsh lights); 5) auditory experiences, including loud or high-pitched noises; 6) olfactory experiences; 7) tastes; 8) sensations of motion; and 9) any other sensory experiences. Both a dichotomous sensory over- responsivity variable, and a continuous sensory over-responsivity symptom count score was created. For the dichotomous variable, children were identified as either (A) the parent endorsed any sensory over-responsivity (present) or (B) the parent did not endorse any sensory over-responsivity (absent). A symptom count variable comprised of the sum of the domains for which the parent endorsed a sensory over-responsivity was also calculated (possible range 0-9). The weighted test-retest reliability of this sensory over-responsivity symptom count variable was calculated using the intracclass correlation coefficient (ICC) on the sample reported in (Egger et al. 2006) and was 0.58, which is within the range of other weighted ICCs reported for other symptom count variables in the PAPA.
Associated Behavioral Challenges.
Definitions and descriptive statistics for each of the associated behavioral challenges are included in Table 3. Our analyses focused on sleep problems, irritability, gastrointestinal (GI) problems, and food selectivity due to their previously demonstrated associations with both sensory over-responsivity and anxiety. All associated behavioral challenge variables were measured at both time points with the PAPA, although the current analyses focus solely on school-age behavioral challenges. Sleep problems included the sum of individual sleep related symptoms reported in Shanahan et al. (2014), which used the Child and Adolescent Psychiatric Assessment (CAPA) from which the PAPA is based, plus additional problems that are measured in the PAPA due to their prevalence in the preschool period (e.g. reluctance to go to sleep). Sleep problems were modeled as a continuous variable from 0–18 possible endorsed items. The weighted test-retest reliability of the sleep problem score was calculated using the ICC on the sample reported in (Egger et al. 2006) and was 0.79. Irritability was defined based on Copeland et al. (2015) and included the frequency of episodes of both phasic (e.g. temper tantrums) and tonic (e.g. anger) symptoms of irritability. To explore the test retest reliability of irritability, a summary variable identifying children falling within the top 25% of the sample for frequency of irritability was computed and agreement was tested using a weighted kappa. The test retest reliability of irritability was κ=0.37. Food selectivity included the sum of endorsed symptoms of food selectivity and related eating behaviors as described in Zucker et al. (2015). Finally, GI problems included all GI symptoms included in the PAPA. Of the 191 children in the follow-up sample, 88 (46%) had at least 1 GI symptoms and 33 (17%) had at least one feeding symptom over the 3 month primary period. Weighted kappas for both the presence of food selectivity and GI problems were calculated and were found to be κ=0.72 and κ=0.49, respectively. The test retest reliability statistics for all of the behavioral challenges variables were within the range of the weighted ICCs and kappas reported for other variables in the PAPA (Egger et al. 2006).
Table 3.
Behavioral Challenges at School-Age
| Domain | Description | Descriptive Statistics |
|---|---|---|
| Sleep Problems | Sleep symptoms were modeled as a
continuous variable from 0-18 possible endorsed
items: • reluctance to sleep alone • sleeping with family members • bedtime resistance • leaving the bed • night waking • rising to check on family members • hypersomnia • restless sleep • difficulty being roused in the morning • daytime sleepiness and falling asleep in the car • tiredness, inadequately rested by sleep, and fatigability • nightmares and night terrors • somnambulism • irregular sleep |
Mean (std): 2.6 (1.9) Range:0-11 |
| Irritability | Irritability was defined as is the frequency of both phasic symptoms of irritability, namely temper tantrums and temper outbursts, and tonic symptoms of irritability, including touchiness/ease of annoyance and anger/resentment. A frequency of 90 would equal 1 instance of these behaviors per day over the 3 month primary period. | Mean (std): 74.6(128.2) Range:0-889 |
| GI Problems | GI symptoms included abdominal pain,constipation, and diarrhea. Of the 191 children in the follow-up sample, 88 (46%) had at least 1 of these GI symptoms over the 3 month primary period. | Mean (std): 0.7 (0.8) Range:0-3 |
| Food Selectivity | Feeding symptoms included selective eating, food refusal, and food aversion. Of the 191 children in the follow-up sample, 33 (17%) had at least 1 of these feeding symptoms over the 3 month primary period. | Mean (std): 0.2 (0.5) Range:0-2 |
Note. All variables were measured at the follow-up assessment (N=191) when the children were 6 years old using the Preschool Age Psychiatric Assessment (PAPA).
Data Analysis
All models were run in SAS and sampling weights were applied to insure that the results were representative of the population from which the sample was drawn. Unless stated otherwise, all results are reported based on these weighted analyses.
The cross-sectional relationship between sensory over-responsivity (dichotomous present vs. absent variable) and anxiety disorders in the preschool sample (N = 917) was tested using chisquare statistics. Similarly, the proportion of children who met criteria for sensory over-responsivity in the preschool period who also had an impairing anxiety disorder at school-age from the LADB sample (N = 191) was also tested with chi-square statistics.
The predictive, longitudinal relationship between sensory over-responsivity symptoms in the preschool period and school-age anxiety symptoms in the LADB sample of 191 children was tested through regression models using SAS PROC GENMOD. Robust variance (sandwich type) estimates derived from generalized estimating equations were used to account for the stratified design of the study. All outcomes were examined for distribution and AICs were used to determine best fit. A Poisson distribution was found to best match the distribution of school-age anxiety symptoms in our non-clinical sample. The first model (Model 1) tested the direct relationship between symptoms of preschool sensory over-responsivity and school-age anxiety symptoms without adjusting for any covariates. Two adjusted models were also run. The first adjusted model (Model 2) included covariates for age at baseline, sex, race, and poverty status to insure that subject characteristics were not driving the results. The decision to use age at baseline - as opposed to time between baseline and follow-up - was made because age at baseline ranged from 2-5, capturing an important developmental window, and there was little variability in the age at follow-up. The second adjusted model (Model 3) included all covariates in the first adjusted models, plus preschool anxiety symptoms, school-age sensory over-responsivity symptoms, and a dichotomous variable accounting for the presence of other preschool disorders (i.e. ADHD, conduct disorder, depression, and oppositional defiant disorder). Preschool anxiety and school-age sensory over-responsivity symptoms were included in Model 3 to insure that neither concurrent sensory over-responsivity nor early anxiety, rather than early sensory over- responsivity, drove the results. The dichotomous “other preschool disorders” variable was included in Model 3 because of previous literature linking sensory over-responsivity to a number of neurodevelopmental and psychiatric disorders, as well as the significant correlation between preschool sensory over-responsivity and other preschool disorders in our sample. These models were all run with the dependent variable modeled as both a dichotomous variable (i.e. presence of sensory over-responsivity vs. absence) and as a continuous count variable. Findings remained the same regardless of how sensory over-responsivity was modeled. Thus, only the results from the continuous analyses are reported.
In order to fully understand the processes underlying the relationship between anxiety and sensory over-responsivity, we conducted three additional follow-up analyses. First, we used PROC LOGISTIC and all covariates included in Model 3 described above to explore whether the relationship between preschool sensory over-responsivity symptoms and school-age anxiety symptoms was predominantly driven by children meeting criteria for a particular anxiety disorder (i.e. dichotomous variables identifying children with either GAD, SAD, or Social Phobia). Second, to explore whether there was a bidirectional relationship between sensory over-responsivity and anxiety, we repeated Model 3 with school-age sensory over-responsivity symptoms as the outcome and preschool anxiety symptoms as the predictor. Finally, to explore the specificity of our findings to anxiety, we ran Model 3 in PROC LOGISTIC with a dichotomous “other school-age disorders” (i.e. ADHD, conduct disorder, depression, and oppositional defiant disorder) variable as the outcome.
Anxiety as a mediator of the relationship between sensory over-responsivity and behavioral challenges was assessed using the PROCESS macro version 3.0 for SAS (http://www.processmacro.org/; Hayes 2018). Mediation of the path from preschool sensory over-responsivity symptoms to behavioral challenge (e.g. sleep problems) by school-age anxiety symptoms was modeled separately for each behavioral challenge in the follow-up school-age sample (N = 191). Figure 2a depicts the simple mediation model that was tested. For each model, we report the beta coefficient (β) and standard error of the ordinary least squares regressions testing the paths from preschool sensory over-responsivity symptoms to anxiety symptoms (a path), from anxiety symptoms to school-age behavioral challenges (b path), as well as the direct path from preschool sensory over-responsivity symptoms to school-age behavioral challenges when holding anxiety symptoms constant (c1 path). Statistical significance of the indirect effect (i.e. mediation effect) was assessed using a bootstrapping procedure with 10,000 bootstrap samples and 95% confidence intervals estimation. Due to modeling constraints, no sampling weights were applied to the mediation analyses.
Results
Sensory Over-Responsivity is Common in Preschool Children
Overall rates with weighted percentages of sensory over-responsivity in the full preschool anxiety study sample (N = 917) at baseline are included in Table 1. Twenty percent of parents reported over-responsivity at least one sensory domain in our preschool sample. The most commonly reported sensory over-responsivity was to tactile experiences (18%), followed by auditory experiences (4%). Of the children with sensory over-responsivity at preschool who were assessed again at school-age, 56% of them still had a parent-reported sensory over-responsivity at school-age. Of children for whom their parents did not endorse any sensory over-responsivity as a preschooler, 16% of children’s parents endorsed at least one sensory over-responsivity by school-age. The demographic characteristics of the sample based on the presence or absence of a sensory over-responsivity are described in Table 1. There were no significant differences in the rates of preschool sensory over-responsivity based on the age of the child or the race of the child. However, the proportion of females for whom parents endorsed at least one sensory over responsivity in the preschool period was higher than the proportion of boys (χ2 (1, N = 917) = 5.41, p = .02, φ = −0.08). Sensory over-responsivity was also more common in children who fell below the federal poverty line (χ2(1, N = 917) = 9.63, p < .002, φ = 0.11).
Children with Sensory Over-Responsivity as Preschoolers Have Higher Rates of Concurrent Anxiety Disorders
We first explored the cross-sectional relationship between sensory over-responsivity and anxiety in the full Preschool Anxiety Study sample (N = 917), weighted back to the original screening sample of 3,433 children. Frequency of anxiety disorders in children with sensory over-responsivity as preschoolers is summarized in Table 1. There was a significant relationship between the presence of sensory over-responsivity (dichotomous variable; absent vs. present) and any anxiety diagnosis in the preschool period (χ2(1, N = 917) = 85.59, p < .0001, < = 0.23), with 152 (43%) of preschool-age children whose parents endorsed a sensory over-responsivity also meeting criteria for an impairing anxiety disorder. The relationship between preschool sensory over-responsivity and preschool anxiety was true for each individual anxiety disorder when tested separately, including GAD (χ2(1, N = 917) = 32.33, p < .0001, φ = 0.19), SAD (χ2 (1, N = 917) =92.90, p < .0001, φ = 0.32), and social phobia (χ2(1, N = 917) = 16.28, p < .0001, φ = 0.13). This relationship was not unique to anxiety as there was also a significant association between preschool sensory over-responsivity and other disorders (e.g. ADHD) in the preschool period (χ2(1, N = 917) = 24.27, p < .0001, < = 0.13).
Preschool Sensory Over-Responsivity Symptoms Predict Anxiety Symptoms at School-age
We next assessed the longitudinal relationship between sensory over-responsivity and anxiety in the LADB sample (N = 191). Preschool sensory over-responsivity symptoms significantly and positively predicted anxiety symptoms at age six (Model 1, Table 4 Column 1, β (SE) = 0.37 (0.05), p < .0001, 95% CIs: 0.27-0.47). The relationship also remained significant when other potential confounding variables (sex, age, race, and poverty status) were added to the model (Model 2, Table 4 Column 2, β (SE) = 0.38, (0.05), p < .0001, 95% CIs: 0.28-0.48). Finally, the significant relationship remained when adding school-age sensory over-responsivity symptoms, preschool anxiety symptoms, and diagnosis with other preschool disorders to the models (Model 3, Table 4 Column 3, β (SE) = 0.13 (0.07), p = .04, 95% CIs: 0.01-0.26). This suggests that concurrent sensory over-responsivity, nor the correlation between these variables in the preschool period, nor other disorders during the preschool period account for this relationship.
Table 4.
Long-Term Association Between Symptoms of Sensory Over-Responsivity in the Preschool Period and Overall Anxiety Symptoms at School-Age.
| Model 1: Simple Association β(SE) 95% Cl |
Model 2: Adjusted Model 1 β (SE) 95% Cl |
Model 3: Adjusted Model 2 β (SE) 95% Cl |
|
|---|---|---|---|
| Preschool Sensory Over-Responsivity Symptoms | 0.37 (0.05) § 0.27-0.47 |
0.38 (0.05) § 0.28-0.48 |
0.13 (0.07) † 0.01-0.26 |
| Gender | - | 0.28 (0.12) † 0.04-0.52 |
0.33 (0.13) ‡
0.09-0.58 |
| Poverty Status | - | 0.07 (0.17) −0.28-0.41 |
0.29 (0.18) −0.05-0.64 |
| Race | - | −0.16 (0.13) −0.42-0.09 |
−0.17 (0.13) −0.42-0.08 |
| Age at Baseline PAPA Assessment | - | 0.15 (0.06) † 0.03-0.27 |
0.12 (0.06) −0.004-0.24 |
| School-Age Sensory Over-Responsivity Symptoms | - | - | 0.09 (0.06) −0.04-0.21 |
| Preschool Anxiety Symptoms | - | - | 0.15 (0.02) § 0.12-0.20 |
| Other Preschool Mental Health Disordersa | - | - | 0.025 (0.16) −0.30-0.35 |
Note. All models tested the predictive, longitudinal relationship between sensory over-responsivity in the preschool period and school-age anxiety symptoms through regression models using SAS PROC GENMOD.
Other mental health disorders is a dichotomous variable that included whether the child met criteria for any of the following: ADHD, conduct disorder, depression, and/or oppositional defiant disorder. β=Parameter Estimate; SE=Standard Error; CI= Confidence Intervals;
p≤0.05;
p≤0.01;
p≤0.001
Follow-up analyses explored the relationship between having preschool sensory over-responsivity and each individual anxiety disorder (i.e. GAD, SAD, and Social Phobia) at school- age. This analysis revealed that the relationship between preschool sensory over-responsivity and anxiety was predominantly driven by children who met criteria for GAD (β (SE) = 0.97 (0.40), p = .02, OR = 2.64; 95% CIs: 1.20-5.80) and was not associated with either SAD (β (SE) = 0.22 (0.42), p = .61, OR = 1.24; 95% CIs: 0.54-2.85) or social phobia (β (SE) = 0.04 (0.39), p = .90, OR = 1.04, 95% CIs: 0.49-2.22).
To test the specificity of the relationship between preschool sensory over-responsivity symptoms and school-age anxiety symptoms, we conducted two additional analyses. First, we tested the hypothesis that the relationship between symptoms of sensory over-responsivity and anxiety symptoms was bidirectional. Although preschool sensory over-responsivity significantly predicted school-age anxiety in the models described above, the opposite was not the case. Preschool anxiety symptoms did not significantly predict school-age sensory over-responsivity symptoms (β (SE) = 0.003 (0.06), p = .96).
Second, we tested the hypothesis that preschool sensory over-responsivity predicts school-age psychiatric disorders generally and thus is not specific to anxiety symptoms. There was not a significant relationship between preschool sensory over-responsivity symptoms and other non-anxiety disorders at school-age (β (SE) = −0.47 (0.30), p = .11). This suggests that the predictive longitudinal relationship from preschool sensory over-responsivity symptoms to school-age psychiatric disorders is specific to anxiety.
School-age Anxiety Symptoms Mediate the Relationship between Preschool Sensory Over-Responsivity Symptoms and Other Behavioral Challenges at School-Age
Mediation models from the longitudinal LADB study (N = 191) demonstrated that school-age anxiety symptoms significantly mediate the relationship between preschool sensory over-responsivity symptoms and behavioral challenges at school-age. As can be seen in Figure 2b-c, children with higher levels of sensory over-responsivity as preschoolers also have higher levels of school-age anxiety symptoms (a path; β (SE) = 0.55 (0.17), t(189)=3.30, p = .001, 95% CIs: 0.22-0.88). Further, children with higher levels of school-age anxiety symptoms have more difficulties with irritability (b path, Figure 2b: β (SE) = 16.02 (3.99), t(l89) = 4.01, p = .0.0001, 95% CIs: 8.15-23.89) and sleep problems (b path, Figure 2c: β (SE) = 0.34 (0.06), t(l89) = 5.94, p < .0001, 95% CIs: 0.23-0.46) at school-age. Bootstrap confidence intervals for the indirect effects suggest that there was a statistically significant positive indirect effect of preschool sensory over-responsivity symptoms through school-age anxiety symptoms to levels of both irritability (indirect path ab, Figure 2b; Effect (SE) = 8.81 (4.8), 95% CIs = 1.09-19.66) and sleep problems (indirect path ab, Figure 2c; Effect (SE) = 0.19 (0.07), 95% CIs = 0.05-0.33) at school- age. In other words, children who have higher levels of sensory over-responsivity symptoms as preschoolers, also have higher levels of anxiety symptoms at school-age, which in turn is associated with increased levels of irritability and sleep problems at school-age. There was no significant relationship between preschool sensory over-responsivity symptoms, school-age anxiety symptoms, and either GI symptoms (indirect path: β (SE) = 0.02 (0.02), 95% CIs = −0.01−0.06) or food selectivity (indirect path: β (SE) = 0.01 (0.01), 95% CIs = −0.004−0.03) at school-age.
Because we only have data from two time points, it is possible that sensory over-responsivity is mediating the relationship between anxiety and both irritability and sleep problems, as opposed to the alternative explanation tested above. To test this alternative model, we ran models with preschool anxiety symptoms as the predictor and school-age sensory over-responsivity symptoms as the mediator. Mediation models did not support school-age sensory over-responsivity symptoms as a mediator of the relationship between preschool anxiety symptoms and either irritability (indirect path: Effect (SE) = −0.50 (0.84), 95% CIs = −2.36–1.15) or sleep problems (indirect path: Effect (SE) = 0.02 (0.02), 95% CIs = −0.01−0.05) at school-age.
Discussion
The current study had two primary findings. First, this is the first study to demonstrate that sensory over-responsivity symptoms during the preschool period is predictive of school-age anxiety symptoms in a non-referred primary care sample of children. Importantly, this finding held even after controlling for school-age sensory over-responsivity, preschool anxiety symptoms, and other preschool psychiatric diagnoses. As such, this suggests that sensory over-responsivity symptoms in the preschool period uniquely predicted school-age anxiety symptoms over-and-above preschool anxiety, concurrent sensory sensitivities, and other preschool psychiatric diagnoses. Second, our results support the hypothesis that school-age anxiety symptoms mediate the relationship between preschool sensory over-responsivity symptoms and school-age behavioral challenges. Specifically, children with high levels of sensory over-responsivity symptoms as preschoolers have higher levels of anxiety symptoms at school-age. This in turn is associated with higher levels of both irritability and sleep problems at school-age. Together, these results underscore the importance of considering sensory over-responsivity when identifying and treating anxiety in young children, as well as suggest that sensory over-responsivity may serve as a marker for anxiety disorders.
Our findings support previous studies suggesting that parent reported sensory over-responsivity is common in typically-developing children (C. Van Hulle et al. 2015; Ben-Sasson et al. 2017; Yochman et al. 2004; Ben-Sasson et al. 2009; Carter et al. 2003; Carter et al. 2011; C. A. Van Hulle et al. 2012). In our representative sample of children, 20% of parents of our preschool-age children endorsed at least one sensory over-responsivity. Thus, our estimate falls within, but at the higher end, of the ranges reported in previous studies. Our prevalence may trend towards the higher end of previous estimates for a number of reasons. First, several studies focused solely on tactile and/or auditory sensory over-responsivity (Ben-Sasson et al. 2009; Carter et al. 2011; C. Van Hulle et al. 2015). Although these were the two most commonly reported sensitivities in our sample, a small subset of our children were reported to have other sensitivities (e.g. to visual stimulation), which likely increased our overall prevalence. Second, it is possible that the differences in prevalence estimates are due to differences in the way that sensory over-responsivity is measured and defined in other studies. In the current study, we defined sensory over-responsivity as meeting criteria for over-responsivity in at least one sensory domain assessed on the PAPA. As such, the inclusion criteria for having sensory over-responsivity in our study may have been more lenient than in previous studies.
Almost half of preschool-age children with a sensory over-responsivity also met criteria for a concurrent impairing anxiety disorder in our sample. This replicates a number of studies that have demonstrated correlations between sensory challenges, including sensory over-responsivity, and anxiety in typically developing individuals across the lifespan (Carter et al. 2011; Ben-Sasson et al. 2009; C. A. Van Hulle et al. 2012; Farrow and Coulthard 2012; Hopkins et al. 2013; Kinnealey and Fuiek 1999; Conelea et al. 2014; Goldsmith et al. 2006; Meredith et al. 2016; Engel-Yeger and Dunn 2011; Bart et al. 2017; Horder et al. 2014; Neil et al. 2016). The cooccurrence of sensory over-responsivity and anxiety across studies has led Green and Ben-Sasson to postulate that sensory over-responsivity precedes and is an early risk factor for the development of generalized anxiety through context conditioning (Green and Ben-Sasson 2010). While this group has demonstrated that sensory over-responsivity precedes anxiety in children with autism (Green et al. 2012), the current study is the first to support this relationship in a representative, non-clinical sample of young children. Importantly, our results also suggest that the predictive longitudinal relationship from preschool sensory over-responsivity symptoms to school-age anxiety symptoms is specific to anxiety in our sample.
Although our results support sensory over-responsivity as an early risk factor for the development of generalized anxiety disorder in children, not all children with sensory over-responsivity will develop anxiety. Indeed, only 52% of children who had at least one sensory sensitivity as preschoolers in our sample went on to meet criteria for an anxiety disorder at school-age. Additionally, of the subset of children who did not exhibit any sensory over-responsivity in preschool, 15% had an anxiety disorder at school-age. These results have important implications for both researchers and clinicians. For researchers, it suggests that we need to explore other moderating variables that predisposes children with sensory over-responsivity to the development of anxiety, while others are spared. For clinicians, it means that sensory over-responsivity is not, in and of itself, a sufficient marker for risk of anxiety.
Even though not all children with sensory over-responsivity develop anxiety, those who have sensory over-responsivity and/or anxiety are at increased risk for a number of challenging comorbid symptoms. The results of our mediation analyses suggest that when children have higher levels of sensory over-responsivity symptoms as preschoolers, they also have higher levels of school-age anxiety symptoms, which in turn is associated with increased levels of irritability and sleep problems at school-age. Importantly, the alternative model (i.e. when children have higher levels of anxiety symptoms as preschoolers, they also have higher levels of school-age sensory over-responsivity, which is in turn associated with increased levels of irritability and sleep problems at school-age) was not supported. This has important clinical implications in that, in children with sensory over-responsivity who do have an anxiety disorder, treatment of both the anxiety and sensory over-responsivity may have downstream effects on the child’s levels of irritability and sleep problems.
Our results need to be considered in light of several limitations. First, we only have data from two time points and thus were are unable to fully meet the criteria for temporal precedence which is ideally needed for mediation. As such, we are unable to completely assess whether there is a causal relationship between sensory over-responsivity, anxiety, and behavioral challenges. This will need to be explored in future prospective and longitudinal studies that can assess the progressive impact of symptoms of sensory over-responsivity over time on anxiety symptoms, and the subsequent action of the anxiety symptoms on behavioral challenges.
Second, sensory over-responsivity was measured within the context of a comprehensive parent interview about a number of psychopathologies, as opposed to using a measure designed to assess sensory over-responsivity specifically. Replication of our results in additional longitudinal studies using parent report measures, such as the Sensory Experience Questionnaire (Baranek et al. 2006) or the Sensory Over-Responsivity Inventory (SensOR) (Schoen et al. 2008), which are specialized for the study of sensory response patterns, is warranted. Similarly, we were surprised not to replicate previous findings of a relationship between both sensory over-responsivity and anxiety with picky eating or GI problems. As researchers learn more about GI sensitivity and feeding issues, there is increasing consensus there are subtypes within these categories. By collapsing the various sub-symptoms into gross dimensions of both GI sensitivity and food selectivity, we may be losing the ability to detect nuanced differences between these variables and sensory sensitivities. Future research will need to look at specific GI and feeding symptoms in relationship to sensory over-responsivity.
Third, all of the results presented here were based on a single parent report measure of child behavior and mental health. As such, it is possible that the relationship between sensory over-responsivity and anxiety may be inflated in our study. Additionally, previous research has demonstrated a relationship between maternal affective symptoms and an increased rate of reporting of child symptomatology (Briggs-Gowan et al. 1996). Thus, it is possible that parental characteristics, such as parental anxiety or depression, may contribute to the relationship between sensory over-responsivity and anxiety in our sample. Furthermore, although there was evidence for sensory over-responsivity and anxiety being separable constructs in the current study, teasing apart these constructs in parent report measures can be prove to be challenging. As such, additional research focused on biological or observational assessments of both anxiety and sensory challenges, using measures such as the Sensory Processing Assessment (Baranek 1999) and the Anxiety Dimensional Observation Schedule (Mian et al. 2015), will greatly strengthen our understanding of these relationships.
Fourth, of the 309 families who were contacted to participate in the LADB study, only 208 (67%) enrolled. As such, our attrition was higher than anticipated. Additionally, although test retest reliability statistics for all of the variables used in the current analyses were within the range reported for other variables in the PAPA, as well as in line with similar measures from other instruments (Egger et al. 2006), the reliabilities for some variables were still low. This reflects the work that still needs to be done both in defining the nosology of psychopathology in early childhood and in assessing psychopathology in the preschool and early school-age period.
Finally, although sensory over-responsivity is the focus of the current study, previous research has demonstrated a correlation between other sensory response patterns, namely sensory under-responsivity and sensory seeking, and anxiety (Ben-Sasson et al. 2008; Lidstone et al. 2014). Future research will need to explore whether these other sensory response patterns are also predictive of anxiety in non-clinical groups of young children.
In summary, the present study suggests that sensory over-responsivity in the preschool period is a risk factor for the development of anxiety disorders. Furthermore, school-age anxiety symptoms mediate the relationship between preschool sensory over-responsivity symptoms and later behavioral challenges. Specifically, when children have higher levels of sensory over-responsivity during preschool it is associated with higher levels of anxiety symptoms and subsequently greater impairment for the child at school-age. As the field moves towards intervening with children at risk for anxiety before the child progresses to a full-blown anxiety disorder (Chronis-Tuscano et al. 2018), identifying early factors, such as sensory over-responsivity, that confer such risk is critical. In support of sensory over-responsivity as one such potential target, treatment of sensory defensiveness in adults has been shown to decrease anxiety (Pfeiffer and Kinnealey 2003) and early treatment in children with autism has been shown to decrease sensory challenges in that population (Baranek et al. 2015). Thus, treating sensory over-responsivity may represent a preventive approach that could have lasting impacts on behavior, functioning, and long-term outcomes.
Acknowledgements:
This work was supported by awards from the National Institute of Mental Health (R01-MH-081025 and R01-MH-075766, PI: Egger), a NARSAD Young Investigator Grant from the Brain & Behavior Research Foundation (#23807, PI: Carpenter), and by the Office of the Assistant Secretary of Defense for Health Affairs through the Autism Research Program (Award# W81XWH-14-1-0526, PIs: Dawson/Carpenter/Baranek). The sponsors had no role in the study design, in the collection, analysis, or interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
References Cited
- Baranek GT (1999). Sensory Processing Assessment for Young Children (SPA). Unpublished. [Google Scholar]
- Baranek GT, David FJ, Poe MD, Stone WL, & Watson LR (2006). Sensory Experiences Questionnaire: discriminating sensory features in young children with autism, developmental delays, and typical development. J Child Psychol Psychiatry, 47(6), 591–601, doi: 10.1111/j.1469-7610.2005.01546.x. [DOI] [PubMed] [Google Scholar]
- Baranek GT, Watson LR, Turner-Brown L, Field SH, Crais ER, Wakeford L, et al. (2015). Preliminary efficacy of adapted responsive teaching for infants at risk of autism spectrum disorder in a community sample. Autism Res Treat, 2015, 386951, doi: 10.1155/2015/386951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bart O, Bar-Shalita T, Mansour H, & Dar R (2017). Relationships among Sensory Responsiveness, Anxiety, and Ritual Behaviors in Children with and without Atypical Sensory Responsiveness. Phys Occup Ther Pediatr, 37(3), 322–331, doi: 10.1080/01942638.2016.1185504. [DOI] [PubMed] [Google Scholar]
- Ben-Sasson A, Carter AS, & Briggs-Gowan MJ (2009). Sensory over-responsivity in elementary school: prevalence and social-emotional correlates. J Abnorm Child Psychol, 37(5), 705–716, doi: 10.1007/s10802-008-9295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Sasson A, Carter AS, & Briggs-Gowan MJ (2010). The development of sensory over-responsivity from infancy to elementary school. J Abnorm Child Psychol, 38(8), 1193–1202, doi: 10.1007/s10802-010-9435-9. [DOI] [PubMed] [Google Scholar]
- Ben-Sasson A, Cermak SA, Orsmond GI, Tager-Flusberg H, Kadlec MB, & Carter AS (2008). Sensory clusters of toddlers with autism spectrum disorders: differences in affective symptoms. J Child Psychol Psychiatry, 49(8), 817–825, doi: 10.1111/j.1469-7610.2008.01899.x. [DOI] [PubMed] [Google Scholar]
- Ben-Sasson A, Soto TW, Heberle AE, Carter AS, & Briggs-Gowan MJ (2017). Early and Concurrent Features of ADHD and Sensory Over-Responsivity Symptom Clusters. J Atten Disord, 21(10), 835–845, doi: 10.1177/1087054714543495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Sasson A, Soto TW, Martinez-Pedraza F, & Carter AS (2013). Early sensory over-responsivity in toddlers with autism spectrum disorders as a predictor of family impairment and parenting stress. J Child Psychol Psychiatry, 54(8), 846–853, doi: 10.1111/jcpp.12035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitsika V, Sharpley CF, & Mills R (2016). How are Sensory Features associated with seven anxiety disorders in boys with Autism Spectrum Disorder? Int J Dev Neurosci, 50, 47–54, doi: 10.1016/j.ijdevneu.2016.03.005. [DOI] [PubMed] [Google Scholar]
- Bittner A, Egger HL, Erkanli A, Jane Costello E, Foley DL, & Angold A (2007). What do childhood anxiety disorders predict? J Child Psychol Psychiatry, 48(12), 1174–1183, doi:JCPP1812 [pii] 10.1111/j.1469-7610.2007.01812.x. [DOI] [PubMed] [Google Scholar]
- Boyd BA, Baranek GT, Sideris J, Poe MD, Watson LR, Patten E, et al. (2010). Sensory features and repetitive behaviors in children with autism and developmental delays. Autism Res, 3(2), 78–87, doi: 10.1002/aur.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, & Schwab-Stone M (1996). Discrepancies among mother, child, and teacher reports: examining the contributions of maternal depression and anxiety. J Abnorm Child Psychol, 24(6), 749–765. [DOI] [PubMed] [Google Scholar]
- Carter AS, Ben-Sasson A, & Briggs-Gowan MJ (2011). Sensory over-responsivity, psychopathology, and family impairment in school-aged children. J Am Acad Child Adolesc Psychiatry, 50(12), 1210–1219, doi: 10.1016/j.jaac.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter AS, Briggs-Gowan MJ, Jones SM, & Little TD (2003). The Infant-Toddler Social and Emotional Assessment (ITSEA): factor structure, reliability, and validity. J Abnorm Child Psychol, 31(5), 495–514. [DOI] [PubMed] [Google Scholar]
- Cermak SA, Curtin C, & Bandini LG (2010). Food selectivity and sensory sensitivity in children with autism spectrum disorders. [Research Support, N.I.H., Extramural Research Support, U.S. Gov't, P.H.S. Review]. J Am Diet Assoc, 110(2), 238–246, doi: 10.1016/j.jada.2009.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Danko CM, Rubin KH, Coplan RJ, & Novick DR (2018). Future Directions for Research on Early Intervention for Young Children at Risk for Social Anxiety. J Clin Child Adolesc Psychol, 47(4), 655–667, doi: 10.1080/15374416.2018.1426006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conelea CA, Carter AC, & Freeman JB (2014). Sensory over-responsivity in a sample of children seeking treatment for anxiety. J Dev Behav Pediatr, 35(8), 510–521, doi: 10.1097/dbp.0000000000000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Brotman MA, & Costello EJ (2015). Normative Irritability in Youth: Developmental Findings From the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry, 54(8), 635–642, doi: 10.1016/j.jaac.2015.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Costello EJ, & Angold A (2009). Childhood and adolescent psychiatric disorders as predictors of young adult disorders.[Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't]. Arch Gen Psychiatry, 66(7), 764–772, doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Egger HL, & Angold A (2005). The developmental epidemiology of anxiety disorders: phenomenology, prevalence, and comorbidity. Child Adolesc Psychiatr Clin N Am, 14(4), 631–648, vii, doi:S1056-4993(05)00061-1 [pii] 10.1016/j.chc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Dougherty LR, Tolep MR, Bufferd SJ, Olino TM, Dyson M, Traditi J, et al. (2013). Preschool anxiety disorders: comprehensive assessment of clinical, demographic, temperamental, familial, and life stress correlates. J Clin Child Adolesc Psychol, 42(5), 577–589, doi: 10.1080/15374416.2012.759225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger HL, & Angold A (2006). Common emotional and behavioral disorders in preschool children: presentation, nosology, and epidemiology. J Child Psychol Psychiatry, 47(3-4), 313–337. [DOI] [PubMed] [Google Scholar]
- Egger HL, Erkanli A, Keeler G, Potts E, Walter BK, & Angold A (2006). Test-Retest Reliability of the Preschool Age Psychiatric Assessment (PAPA). J Am Acad Child Adolesc Psychiatry, 45(5), 538–549, doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- Engel-Yeger B, & Dunn W (2011). Exploring the relationship between affect and sensory processing patterns in adults. British Journal of Occupational Therapy, 74(10), 456–464, doi:. [DOI] [Google Scholar]
- Farrow CV, & Coulthard H (2012). Relationships between sensory sensitivity, anxiety and selective eating in children. Appetite, 58(3), 842–846, doi: 10.1016/j.appet.2012.01.017. [DOI] [PubMed] [Google Scholar]
- Franz L, Angold A, Copeland W, Costello EJ, Towe-Goodman N, & Egger H (2013). Preschool anxiety disorders in pediatric primary care: prevalence and comorbidity. J Am Acad Child Adolesc Psychiatry, 52(12), 1294–1303 e1291, doi: 10.1016/j.jaac.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith HH, Van Hulle CA, Arneson CL, Schreiber JE, & Gernsbacher MA (2006). A population-based twin study of parentally reported tactile and auditory defensiveness in young children. J Abnorm Child Psychol, 34(3), 393–407, doi: 10.1007/s10802-006-9024-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green SA, & Ben-Sasson A (2010). Anxiety disorders and sensory over-responsivity in children with autism spectrum disorders: is there a causal relationship? J Autism Dev Disord, 40(12), 1495–1504, doi: 10.1007/s10803-010-1007-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green SA, Ben-Sasson A, Soto TW, & Carter AS (2012). Anxiety and sensory over-responsivity in toddlers with autism spectrum disorders: bidirectional effects across time. J Autism Dev Disord, 42(6), 1112–1119, doi: 10.1007/s10803-011-1361-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallett V, Lecavalier L, Sukhodolsky DG, Cipriano N, Aman MG, McCracken JT, et al. (2013). Exploring the manifestations of anxiety in children with autism spectrum disorders. J Autism Dev Disord, 43(10), 2341–2352, doi: 10.1007/s10803-013-1775-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2018). Introduction to Mediation, Moderation, and Conditional Process Analysis (Metholodology in the Social Sciences). New York: Guilford Press. [Google Scholar]
- Hopkins J, Lavigne JV, Gouze KR, LeBailly SA, & Bryant FB (2013). Multidomain models of risk factors for depression and anxiety symptoms in preschoolers: evidence for common and specific factors. J Abnorm Child Psychol, 41(5), 705–722, doi: 10.1007/s10802-013-9723-2. [DOI] [PubMed] [Google Scholar]
- Horder J, Wilson CE, Mendez MA, & Murphy DG (2014). Autistic traits and abnormal sensory experiences in adults. J Autism Dev Disord, 44(6), 1461–1469, doi: 10.1007/s10803-013-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinnealey M, & Fuiek M (1999). The relationship between sensory defensiveness, anxiety, depression and perception of pain in adults. Occupational Therapy International, 6(3), 195–206, doi: 10.1002/oti.97. [DOI] [Google Scholar]
- Lidstone J, Uljarevic M, Sullivan J, Rodgers J, McConachie H, Freeston M, et al. (2014). Relations among restricted and repetitive behaviors, anxiety and sensory features in children with autism spectrum disorders. Research in Autism Spectrum Disorders, 8(2), 82–92, doi: 10.1016/j.rasd.2013.10.001. [DOI] [Google Scholar]
- Mangeot SD, Miller LJ, McIntosh DN, McGrath-Clarke J, Simon J, Hagerman RJ, et al. (2001). Sensory modulation dysfunction in children with attention-deficit-hyperactivity disorder. Dev Med Child Neurol, 43(6), 399–406. [DOI] [PubMed] [Google Scholar]
- Mazurek MO, & Petroski GF (2015). Sleep problems in children with autism spectrum disorder: examining the contributions of sensory over-responsivity and anxiety. Sleep Med, 16(2), 270–279, doi: 10.1016/j.sleep.2014.11.006. [DOI] [PubMed] [Google Scholar]
- Mazurek MO, Vasa RA, Kalb LG, Kanne SM, Rosenberg D, Keefer A, et al. (2013). Anxiety, sensory overresponsivity, and gastrointestinal problems in children with autism spectrum disorders. J Abnorm Child Psychol, 41(1), 165–176, doi: 10.1007/s10802-012-9668-x. [DOI] [PubMed] [Google Scholar]
- Meredith PJ, Bailey KJ, Strong J, & Rappel G (2016). Adult Attachment, Sensory Processing, and Distress in Healthy Adults. Am J Occup Ther, 70(1), 7001250010p7001250011–7001250018, doi: 10.5014/ajot.2016.017376. [DOI] [PubMed] [Google Scholar]
- Merwin RM, Moskovich AA, Wagner HR, Ritschel LA, Craighead LW, & Zucker NL (2013). Emotion regulation difficulties in anorexia nervosa: Relationship to self-perceived sensory sensitivity. Cogn Emot, 27(3), 441–452, doi: 10.1080/02699931.2012.719003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mian ND, Carter AS, Pine DS, Wakschlag LS, & Briggs-Gowan MJ (2015). Development of a novel observational measure for anxiety in young children: The Anxiety Dimensional Observation Scale. J Child Psychol Psychiatry, 56(9), 1017–1025, doi: 10.1111/jcpp.12407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neil L, Olsson NC, & Pellicano E (2016). The Relationship Between Intolerance of Uncertainty, Sensory Sensitivities, and Anxiety in Autistic and Typically Developing Children. J Autism Dev Disord, 46(6), 1962–1973, doi: 10.1007/s10803-016-2721-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Donnell S, Deitz J, Kartin D, Nalty T, & Dawson G (2012). Sensory processing, problem behavior, adaptive behavior, and cognition in preschool children with autism spectrum disorders. Am J Occup Ther, 66(5), 586–594, doi: 10.5014/ajot.2012.004168. [DOI] [PubMed] [Google Scholar]
- Pfeiffer B, & Kinnealey M (2003). Treatment of sensory defensiveness in adults. Occup Ther Int, 10(3), 175–184. [DOI] [PubMed] [Google Scholar]
- Pfeiffer B, Kinnealey M, Reed C, & Herzberg G (2005). Sensory modulation and affective disorders in children and adolescents with Asperger's disorder. Am J Occup Ther, 59(3), 335–345, doi: 10.5014/ajot.59.3.335. [DOI] [PubMed] [Google Scholar]
- Pickles A, Dunn G, & Vazquez-Barquero J (1995). Screening for stratification in two-phase (‘two-stage’) epidemiological surveys. Statistical Methods in Medical Research, 4(1), 73–89. [DOI] [PubMed] [Google Scholar]
- Reynolds S, & Lane SJ (2009). Sensory overresponsivity and anxiety in children with ADHD. Am J Occup Ther, 63(4), 433–440. [DOI] [PubMed] [Google Scholar]
- Schoen SA, Miller LJ, & Green KE (2008). Pilot study of the Sensory Over-Responsivity Scales: assessment and inventory. Am J Occup Ther, 62(4), 393–406. [DOI] [PubMed] [Google Scholar]
- Shanahan L, Copeland WE, Angold A, Bondy CL, & Costello EJ (2014). Sleep problems predict and are predicted by generalized anxiety/depression and oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry, 53(5), 550–558, doi: 10.1016/j.jaac.2013.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towe-Goodman NR, Franz L, Copeland W, Angold A, & Egger H (2014). Perceived family impact of preschool anxiety disorders. J Am Acad Child Adolesc Psychiatry, 53(4), 437–446, doi: 10.1016/j.jaac.2013.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hulle C, Lemery-Chalfant K, & Goldsmith HH (2015). Trajectories of Sensory Over-Responsivity from Early to Middle Childhood: Birth and Temperament Risk Factors. PLoS One, 10(6), e0129968, doi: 10.1371/journal.pone.0129968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hulle CA, Schmidt NL, & Goldsmith HH (2012). Is sensory over-responsivity distinguishable from childhood behavior problems? A phenotypic and genetic analysis. J Child Psychol Psychiatry, 53(1), 64–72, doi: 10.1111/j.1469-7610.2011.02432.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yochman A, Parush S, & Ornoy A (2004). Responses of preschool children with and without ADHD to sensory events in daily life. Am J Occup Ther, 58(3), 294–302. [DOI] [PubMed] [Google Scholar]
- Zucker N, Copeland W, Franz L, Carpenter K, Keeling L, Angold A, et al. (2015). Psychological and Psychosocial Impairment in Preschoolers With Selective Eating. Pediatrics, 136(3), e582–590, doi: 10.1542/peds.2014-2386. [DOI] [PMC free article] [PubMed] [Google Scholar]