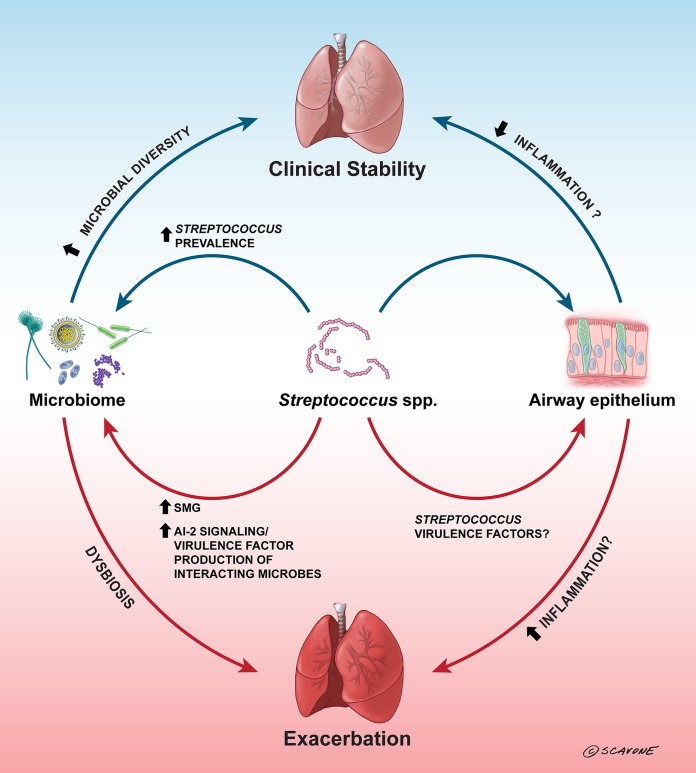
FIG 1.
Streptococci can influence cystic fibrosis airway disease. In CF airways, an increased prevalence of Streptococcus spp. has been correlated with clinical stability, lower inflammation, and/or less severe outcomes (2, 9, 12, 21, 29), but it is unclear whether this is due to direct interactions with the airway epithelium, is due to interactions between the streptococci and the microbiome that lead to increased microbial diversity, or is a consequence of less damage to the airway. Oral streptococci have been demonstrated to inhibit P. aeruginosa growth through the production of hydrogen peroxide and reactive nitrogenous intermediates (49–51); by inhibiting P. aeruginosa, streptococci could open up niches for increased microbial diversity in the lung, which could aid clinical stability. In contrast, the predominance of SMG isolates has been correlated with exacerbation (1, 7, 17, 30), and this may be due to interactions between the SMG isolates and other CF pathogens, such as P. aeruginosa. Oral streptococci have been demonstrated to stimulate increased virulence factor production by P. aeruginosa (43–45) through AI-2 signaling (43), and this could lead to dysbiosis in the lung and eventual exacerbation. The arrows indicate both direct and indirect interactions that are suggested to occur in the CF airways. The blue arrows indicate generally positive effects, the red arrows indicate generally negative effects, and the arrows are labeled with the factors (if known) involved in these effects. (Copyright William Scavone, Kestrel Studio; reproduced with permission.)