Figure 4. Probability that dapivirine vaginal ring PrEP implementation is cost‐effective at varying thresholds.
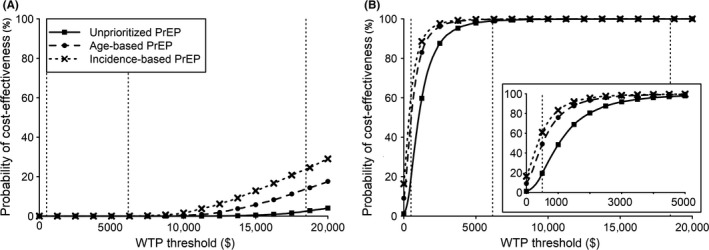
Results are from probabilistic sensitivity analysis. We assessed the cost per life‐year gained, relative to ART implementation without PrEP, in the sexually active population during 2019 to 2030 (A) and over the lifetime of the PrEP‐exposed cohort (B). We assessed unprioritized PrEP implementation among women aged 22 to 45, age‐based PrEP among women aged 22 to 29, incidence‐based PrEP among high‐incidence women aged 22 to 45, or PrEP scaled‐up among FSWs aged 22 to 45. PrEP implementation among FSWs was cost‐saving in >99% of simulations (Table S5). Vertical dotted lines highlight a willingness‐to‐pay threshold of $500 39 and thresholds of about one or threefold South Africa's 2017 per‐capita gross domestic product ($6,200 or $18,500 respectively 40). The inset in (B) highlights the results for willingness‐to‐pay thresholds of $0 to $5000. ART, antiretroviral therapy; FSW, female sex worker; PrEP, pre‐exposure prophylaxis; WTP, willingness‐to‐pay.
