Abstract
Introduction
From the variety of direct restorative dental materials, composite resins are considered as having the most esthetic and functional properties. The conservative preparation, esthetic results, good mechanical qualities and surface finishing properties of dental composites, combined with the protective properties of fluoride from glass-ionomers, led to a new generation of dental materials: the giomers.
Objective
The purpose is to review the available literature about the giomers, regarding the chemical composition, handling properties and esthetics, adhesion and microleakage, fluoride releasing and protection offered, clinical indications.
Method
The search was carried out using ScienceDirect and PubMed databases with the following keywords: giomer, esthetic properties giomers and fluoride releasing giomers. A total of 232 articles were initially selected, with the following inclusion criteria: full text articles, written in English, with topics on the properties and the clinical implications of giomers. Papers presented as abstract were not included. In the next step, review articles, duplicates, and articles in other languages were removed; as a result, a total of 44 sources published between 2004 and 2017 were selected.
Results
The selected articles referred to the following aspects about the giomers: chemical composition (8 articles), adhesion and microleakage (10 articles), fluoride releasing and pulp protection (15 articles), clinical indications (6 articles), effects of additional treatments and dietary habits (11 articles).
Keywords: giomer, fluoride, dental composites
Introduction
From the variety of direct restorative dental materials, composite resins are considered as having the most esthetic and functional properties, which explains the high frequency of their use [1,2].
S.R. Schricker [1] describes composite resins as a mixture of organic and inorganic particles: the resin, the fillers, the initiator of the chemical reaction and the coupling agent. This is a versatile combination, the properties and indication of a new material being determined by the proportion of the mixed components [1].
Composite resins allow for a conservative preparation of the tooth structure and esthetic results, enabling to build a restoration without the intervention of the dental laboratory. Other advantages include: wear-resistance close to the natural tooth structure, good marginal integrity, they can be repaired intraorally and/or replaced by ceramic or composite indirect restorations and they have low costs [3].
Due to the differences in filler content, composite resins can be used for specific purposes. Low viscosity composites have a much greater contraction and cannot be applied in areas with high functional stress. However the flowing properties make them easy to handle. Conventional composites have lower setting contraction and can be used to restore the posterior teeth. Composites can also be used for core building. Orthodontic devices can be applied using a chemical setting system of two components. For cementation of restorative appliances, a low viscosity composite, with chemical and/or photo- activated curing mechanism is used. Sealing materials have low viscosity, which enable their penetration into the deep pits and fissures and contain a high percentage of activator to be properly light cured [4].
The marginal fit of direct composites might be improved by heating them before application [5]. With modern composites and adequate technique, adhesion to enamel is excellent and to dentine it is increasingly good. The optical properties allow for a close reproduction of color and translucency of natural teeth [6]. According to Rajan [2], all esthetic restorative materials interact with the light, responsible for the intrinsic color; in addition: the optical outcome of the composite restorations is influenced by the thickness of the material, background color, and composition of the materials: matrix component and filler particles, pigments and coupling agents. Titanium oxides, zirconium, aluminum are known as being opaque with refraction indices different from the matrix. They are added in minimal quantities with the purpose of masking discolorations [2].
Another group of direct restorative materials that are known to offer high protection against the development of new carious lesions, by releasing fluoride, are the glass ionomers [3].
Fluoride releasing dental materials benefit from the constant interaction with the oral fluids, which influence the protective properties by release and recharge [7].
The glass-ionomers adhere chemically to the tooth structure and arrest the marginal micro-leakage of the fluids and microorganisms towards the restored surface. However, the mechanical resistance of the glass-ionomers is very weak [8].
Fluoride has the capacity to inhibit the bacterial metabolism of Streptococcus mutans and Streptococcus sobrinus, species associated with carious lesion debut. Glass-ionomers and resin modified glass-ionomers (RMGIC) are highly recommended for direct restorations and sealers for young patients, as well as for orthodontic brackets bonding [9].
For efficient distribution of fluoride, a bioactive nanoparticle is needed. Systemic effects are minimal and this method allows for a higher local concentration of fluoride, and therefor anti-carious effect [10].
By combining the characteristics of the composite resins and glass-ionomers, hybrid products knowns as giomers have been obtained; giomers represent a special class of composites that offer both protection against caries and functional and esthetic results, by incorporating particles of pre-reacted glass filler in the matrix of the composite material.
The objective of this review is to analyze the available literature about the properties, indications, composition of giomers: fluoride-releasing, resin-based, adhesive materials that contain pre-reacted glass fillers.
Materials and method
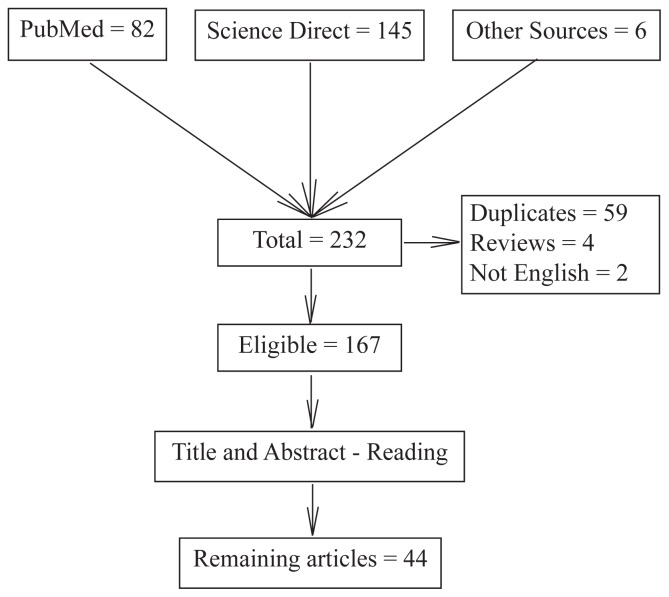
The search was carried out using ScienceDirect and PubMed databases with the following keywords: giomer, esthetic properties giomers and fluoride releasing giomers. A total of 232 articles were initially selected, with the following inclusion criteria: full text articles, written in English, with topics on the properties and the clinical implications of giomers. Papers presented as abstract were not included. In the next step, review articles, duplicates, and articles in other languages were removed; as result, a total of 44 sources published between 2004 and 2017 were selected. The flowchart of the research is presented in Figure 1.
Figure 1.
Flowchart of the selection.
Results
The selected articles referred to the following aspects about the giomers: chemical composition (8 articles), adhesion and microleakage (10 articles), fluoride releasing and pulp protection (15 articles), clinical indications (6 articles), effects of additional treatments and dietary habits (11 articles).
Discussion
Chemical composition of the giomers
New classes of hybrid materials widely used in dentistry are: resin modified glass ionomers (RMGIC), compomers (resin based materials, modified by adding polyacid), ormocers (the matrix is a mix of organic and inorganic polymers), zircomers (composites modified with zirconium particles).
A new class of materials – Giomers - aims to incorporate the best properties of composite resins and glass-ionomers: protection against carious lesion, good mechanical resistance and esthetics. Giomers represent one of the most recent developments in the field of fluoride releasing dental materials, combining esthetics with the possibility to have a finished surface and good mechanical resistance. Clinical studies suggested that the morphology, marginal adaptation and post-operative sensitivity are similar for resin composites and giomers. For giomers, Itota [7], Abdel-Karim [11] and Cury [12] have found that secondary caries are less frequent [7,11,12].
Giomers have a conventional bis-GMA matrix and bioactive glass fillers. The setting reaction is light activated. The consistency is either flow or conventional; the amount of fluoride released is sufficient for antibacterial protection [13].
Handling properties and esthetics
Working with giomers is considered easy in comparison to composite resins. They have high flexibility and are less likely to be dislocated from areas with high functional stress. Color, fluorescence (property to absorb light and spontaneously emit a higher wavelength, bringing vitality to a restoration) and translucency (property that allows the passage of light), together, essentially contribute to the esthetical integration of a new restoration. Therefore, new materials should imitate the color of natural teeth and all other optical properties [14–17]. Nakamura [13] found esthetic appearance of the fillings at two years after application [13].
Adhesion and micro-leakage
When referring to adhesion in the field of restorative dentistry, a material should ideally achieve an impenetrable bond to the tooth structure. This way, the pulp chamber is sealed from negative stimuli such as bacterial infiltration or chemical injuries. For giomers, a self-etch system is mainly used to obtain the adhesion of the material to the tooth structure.
With the purpose of increasing the antimicrobial protection, the effect of topical fluoridated solutions on the surface of giomers restorations is being tested. The effect of these applications might negatively influence the bond strength between giomer and tooth structure and increase the microleakage [18–21].
Comparative micro-leakage studies have shown that this phenomenon is higher for giomers and lower for glass-ionomers and zircomers (other flouride releasing dental materials). However, the force necessary to displace a giomer filling is higher than for the other two materials [22–24].
A method of avoiding secondary decays is the use of chlorhexidine as disinfectant of the cavity. However, in the case of giomers, when used with a self-etch adhesive system, the supplementary disinfection might negatively influence adhesion quality and therefore increase the risk for micro-leakage [25].
With the purpose of reducing the increase in size for cavities as a consequence of micro-leakage, the possibility to repair a filling is investigated using giomer materials. To accomplish this, a strong bond between the old and the new material is enforced by removing the surface layers of the old filling [8,26].
Fluoride releasing and protection offered by giomers
There is no ideal formula for a dental material that is applicable to all clinical cases [1]. Bioactive glass included in the composition of giomers, dissolves upon contact with biological fluids, allowing for a therapeutic ion release like phosphate, fluoride, calcium, influencing the capacity to form apatite. This approach is a rather new one for the dentistry field. In the field of orthodontics it helps prevent white spots lesions [27].
Clinical indications
Clinical tests conducted by Jyothy and Gordan (periods of 1 year up to 13 years) have shown that giomers have ideal properties for treating cervical non-carious lesions. These lesions remain a challenge because of the lower adhesion quality at cervical level. Clinical trials also indicated both adequate resistance and esthetically acceptable aspect for giomers, years after application [28–30].
Alsayed [31] and Salmerón-Valdés [32] conducted in vitro studies to highlight the preventative properties of giomers as coating materials and pit and fissure sealants [31,32].
Tests conducted by Kimyai [33] show that contamination with hemostatic agents can increase the microleakage and marginal gaps in giomer restorations [33].
Table I shows the available products based on giomer technologies. Manufacturers recommend the use of giomers for all restorations (class I, II, III, IV, V) especially for patients with a high carious index, for direct veneers because of high esthetic properties and chameleon effect, for the proper restoration of pink esthetics in exposed cervical areas (Gingival shades), as pit and fissure sealants, as base materials or liners, for pediatric use, as varnish for hypersensitive exposed areas, for cementation of restorations, and even for collating orthodontic brackets [34].
Table I.
Commercial products available, according to the producer [34]
| Product | Company | Specifications |
|---|---|---|
| FL-BOND II Adhesive System | Shofu Dental Corporation, Japan | self-etching, fluoride releasing bonding system |
| Beautifil-Bulk Restorative | Shofu Dental Corporation, Japan | For posterior restorations High fill ratio (87.0wt%, 74.5 vol%) reduced polymerization shrinkage increased compressive and flexural strength sustained fluoride release |
| Beautifil-Bulk Flowable | Shofu Dental Corporation, Japan | High filler ratio (73.wt %) reduced volumetric shrinkage increased compressive and flexural strength fluoride release and recharge Self-leveling and easy adaptation 10 second cure time |
| Beautifil Flow Plus, Beautifil Flow | Shofu Dental Corporation, Japan | Base, liner and restorative material |
| Beautifil II | Shofu Dental Corporation, Japan | A fluoride releasing, highly aesthetic dental material for all classes of restorations appropriate for patients with high caries index |
| Beautifil II LS (Low Shrinkage) | Shofu Dental Corporation, Japan | Low volumetric shrinkage Chameleon effect Easy to handle Sustained fluoride release and recharge |
| Beautifil II Gingiva Shades | Shofu Dental Corporation, Japan | fluoride-releasing intended for the cervical area, specifically the aesthetic correction of gingival recession, wedge-shaped defects, exposed cervical areas, splinting, and re-balancing of pink aesthetics |
| Beautifil II Enamen Shades | Shofu Dental Corporation, Japan | chameleon-like optical characteristics for enamel direct veneers |
| BeautiSealant | Shofu Dental Corporation, Japan | Fluoride Releasing Pit and Fissure Sealant System |
| PRG Barrier Coat | Shofu Dental Corporation, Japan | light-cured giomer varnish for prolonged hypersensitivity relief Seals and protects exposed dentinal tubules to prevent pain for patients experiencing loss of enamel, gingival recession or temporary sensitivity due to whitening |
| BeautiCem SA | Shofu Dental Corporation, Japan | Self-etching, self-adhesive resin cement No primer required for all substrates (except porcelain) Low film thickness (12 μm) |
Effects of additional treatments/ dietary habits
Currently, an often required procedure is teeth whitening. The substances used have the capacity to modify the surface structure of the enamel and of direct restoration materials.
The changes in color after the use of whiting method are clinically acceptable. Microscopically, micro-fissures and a higher bacterial adhesion can be detected. For other materials, such as microfilled composite resins, replacing the filling is imperative after the whitening procedure because of visible color differences [35,36].
Lately an important increase in the number of erosive lesions with both intrinsic and external causes has been observed. A great part of the external erosion is caused by the increased consumption of acidic beverages, which modify also the surface of restorative materials, including giomers [37–39]. Another important factor for surface modifications in giomer restorations is represented by prophylaxis methods like air-powder polishing, pumice and brushes used to remove dental plaque. Increased surface roughness favored staining, bacterial retention and gingival inflammation [14,40,41].
Giomers prove to be useful in the process of collating orthodontic brackets with mechanical properties similar to composite resins. They offer protection against carious lesions, but the orthodontic bond-strength of giomer materials proves to be lower than that of RMGIC [42–44].
Conclusions
Giomers have been proved to incorporate the mechanical and esthetic qualities of composite resins and carious protection through fluoride release from the glass-ionomers component. They have a wide range of clinical indications and are easily used them for restorations of cervical lesions, where adhesion is less efficient.
Giomers are affected by dietary habits and dental procedures, such as acidic beverage consumption, teeth whitening or prophylaxis methods.
In some cases, other materials have improved performances: RMGIC and Nano-Ionomers have a better marginal adaptation when compared to giomers and RMGIC have a stronger bond-strength than giomer materials when attaching metal brackets to enamel.
New research investigates the usage of giomers in the field of orthodontics, for the prevention and treatment of white spots.
Acknowledgement
This study was supported by the Iuliu Hatieganu University of Medicine and Pharmacy, Cluj-Napoca, by the internal Project: Nr. 1680/75, of 19 January 2018.
References
- 1.Schricker SR. Composite resin polymerization and relevant parameters. In: Eliades T, Brantley W, editors. Orthodontic Applications of Biomaterials. 1 ed. Woodheah Publishing; 2016. pp. 153–170. [Google Scholar]
- 2.Rajan G, Shouha P, Ellakwa A, Bhowmik K, Xi J, Prusty G. Evaluation of the physical properties of dental resin composites using optical fiber sensing technology. Dent Mater. 2016;32:1113–1123. doi: 10.1016/j.dental.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 3.Itota T, Carrick TE, Yoshiyama M, McCabe JF. Fluoride release and recharge in giomer, compomer and resin composite. Dent Mater. 2004;20:789–795. doi: 10.1016/j.dental.2003.11.009. [DOI] [PubMed] [Google Scholar]
- 4.Dionysopoulos D, Tolidis K, Gerasimou P, Koliniotou-Koumpia E. Effect of preheating on the film thickness of contemporary composite restorative materials. J Dent Sci. 2014;9:313–319. [Google Scholar]
- 5.Randolph LD, Palin WM, Leloup G, Leprince JG. Filler characteristics of modern dental resin composites and their influence on physico-mechanical properties. Dent Mater. 2016;32:1586–1599. doi: 10.1016/j.dental.2016.09.034. [DOI] [PubMed] [Google Scholar]
- 6.Xu X, Ling L, Wang R, Burgess JO. Formulation and characterization of a novel fluoride-releasing dental composite. Dent Mater. 2006;22:1014–1023. doi: 10.1016/j.dental.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 7.Itota T, Al-Naimi OT, Carrick TE, Yoshiyama M, McCabe JF. Fluoride release and neutralizing effect by resin-based materials. Oper Dent. 2005;30:522–527. [PubMed] [Google Scholar]
- 8.Harhash AY, ElSayad II, Zaghloul AGS. A comparative in vitro study on fluoride release and water sorption of different flowable esthetic restorative materials. Eur J Dent. 2017;11:174–179. doi: 10.4103/ejd.ejd_228_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nguyen S, Escudero C, Sediqi N, Smistad G, Hiorth M. Fluoride loaded polymeric nanoparticles for dental delivery. Eur J Pharm Sci. 2017;104:326–334. doi: 10.1016/j.ejps.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 10.McCabe JF, Rusby S. Water absorption, dimensional change and radial pressure in resin matrix dental restorative materials. Biomaterials. 2004;25:4001–4007. doi: 10.1016/j.biomaterials.2003.10.088. [DOI] [PubMed] [Google Scholar]
- 11.Abdel-karim UM, El-Eraky M, Etman WM. Three-year clinical evaluation of two nano-hybrid giomer restorative composites. Tanta Dent J. 2014;11:213–222. [Google Scholar]
- 12.Cury JA, de Oliveira BH, dos Santos AP, Tenuta LM. Are fluoride releasing dental materials clinically effective on caries control? Dent Mater. 2016;32:323–333. doi: 10.1016/j.dental.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 13.Nakamura N, Yamada A, Iwamoto T, Arakaki M, Tanaka K, Aizawa S, et al. Two-year clinical evaluation of flowable composite resin containing pre-reacted glass-ionomer. Pediat Dent J. 2009;19:89–97. [Google Scholar]
- 14.Condò R, Cerroni L, Pasquantonio G, Mancini M, Pecora A, Convertino A, et al. A Deep Morphological Characterization and Comparison of Different Dental Restorative Materials. Biomed Res Int. 2017;2017 doi: 10.1155/2017/7346317. 7346317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ilie N, Stawarczyk B. Evaluation of modern bioactive restoratives for bulk-fill placement. J Dent. 2016;49:46–53. doi: 10.1016/j.jdent.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 16.Yu B, Lee YK. Differences in color, translucency and fluorescence between flowable and universal resin composites. J Dent. 2008;36:840–846. doi: 10.1016/j.jdent.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Dede DÖ, Sahin O, Özdemir OS, Yilmaz B, Celik E, Köroğlu A. Influence of the color of composite resin foundation and luting cement on the final color of lithium disilicate ceramic systems. J Prosthet Dent. 2017;117:138–143. doi: 10.1016/j.prosdent.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 18.Tarasingh P, Reddy JS, Suhasini K, Hemachandrika I. Comparative Evaluation of Antimicrobial Efficacy of Resin-Modified Glass Ionomers, Compomers and Giomers – An Invitro Study. J Clin Diagn Res. 2015;9:ZC85–ZC87. doi: 10.7860/JCDR/2015/14364.6237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dhull KS, Nandlal B. Effect of low-concentration daily topical fluoride application on fluoride release of giomer and compomer: an in vitro study. J Indian Soc Pedod Prev Dent. 2011;29:39–45. doi: 10.4103/0970-4388.79930. [DOI] [PubMed] [Google Scholar]
- 20.Mousavinasab SM, Meyers I. Fluoride release by glass ionomer cements, compomer and giomer. Dent Res J (Isfahan) 2009;6:75–81. [PMC free article] [PubMed] [Google Scholar]
- 21.Naoum S, O’Regan J, Ellakwa A, Benkhart R, Swain M, Martin E. The effect of repeated fluoride recharge and storage media on bond durability of fluoride rechargeable Giomer bonding agent. Aust Dent J. 2012;57:178–183. doi: 10.1111/j.1834-7819.2012.01681.x. [DOI] [PubMed] [Google Scholar]
- 22.Walia R, Jasuja P, Verma KG, Juneja S, Mathur A, Ahuja L. A comparative evaluation of microleakage and compressive strength of Ketac Molar, Giomer, Zirconomer, and Ceram-x: An in vitro study. J Indian Soc Pedod Prev Dent. 2016;34:280–284. doi: 10.4103/0970-4388.186746. [DOI] [PubMed] [Google Scholar]
- 23.Bollu IP, Hari A, Thumu J, Velagula LD, Bolla N, Varri S, et al. Comparative evaluation of microleakage between nano-ionomer, giomer and resin modified glass ionomer cement in class V cavities- CLSM study. J Clin Diagn Res. 2016;10:66–70. doi: 10.7860/JCDR/2016/18730.7798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alsayed EZ, Hariri I, Sadr A, Nakashima S, Bakhsh TA, Shimada Y, et al. Optical coherence tomography for evaluation of enamel and protective coatings. Dent Mater J. 2015;34:98–107. doi: 10.4012/dmj.2014-215. [DOI] [PubMed] [Google Scholar]
- 25.Kimyai S, Pournaghi-Azar F, Naser-Alavi F, Salari A. Effect of disinfecting the cavity with chlorhexidine on the marginal gaps of Cl V giomer restorations. J Clin Exp Dent. 2017;9:e202–e206. doi: 10.4317/jced.53193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arami S, Kimyai S, Oskoee PA, Daneshpooy M, Rikhtegaran S, Bahari M, et al. Reparability of giomer using different mechanical surface treatments. J Clin Exp Dent. 2017;9:e520–e526. doi: 10.4317/jced.53591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Al-Eesa NA, Wong FSL, Johal A, Hill RG. Fluoride containing bioactive glass composite for orthodontic adhesives – ion release properties. Dent Mater. 2017;33:1324–1329. doi: 10.1016/j.dental.2017.08.185. [DOI] [PubMed] [Google Scholar]
- 28.Jyothi K, Annapurna S, Kumar AS, Venugopal P, Jayashankara C. Clinical evaluation of giomer- and resin-modified glass ionomer cement in class V noncarious cervical lesions: An in vivo study. J Conserv Dent. 2011;14:409–413. doi: 10.4103/0972-0707.87214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gordan V, Mondragon E, Watson RE, Garvan C, Mjör IA. A clinical evaluation of a self-etching primer and a giomer restorative material: results at eight years. J Am Dent Assoc. 2007;138:621–627. doi: 10.14219/jada.archive.2007.0233. [DOI] [PubMed] [Google Scholar]
- 30.Gordan VV, Blaser PK, Watson RE, Mjör IA, McEdward DL, Sensi LG, et al. A clinical evaluation of a giomer restorative system containing surface prereacted glass ionomer filler: results from a 13-year recall examination. J Am Dent Assoc. 2014;145:1036–1043. doi: 10.14219/jada.2014.57. [DOI] [PubMed] [Google Scholar]
- 31.Alsayed EZ, Hariri I, Nakashima S, Shimada Y, Bakhsh T, Tagami J, et al. Effects of coating materials on nanoindentation hardness of enamel and adjacent areas. Dent Mater. 2016;32:807–816. doi: 10.1016/j.dental.2016.03.023. [DOI] [PubMed] [Google Scholar]
- 32.Salmerón-Valdés EN, Scougall-Vilchis RJ, Alanis-Tavira J, Morales-Luckie RA. Comparative study of fluoride released and recharged from conventional pit and fissure sealants versus surface prereacted glass ionomer technology. J Conserv Dent. 2016;19:41–45. doi: 10.4103/0972-0707.173197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kimyai S, Pournaghi-Azar F, Mohammadi N, Babri M. Effect of hemostatic agent on marginal gaps of class V giomer restorations. J Clin Exp Dent. 2017;9:e672–e676. doi: 10.4317/jced.53704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shofu Dental. Composites [Google Scholar]
- 35.Kimyai S, Bahari M, Naser-Alavi F, Behboodi S. Effect of two different tooth bleaching techniques on microhardness of giomer. J Clin Exp Dent. 2017;9:e249–e253. doi: 10.4317/jced.53290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mohammadi N, Kimyai S, Abed-Kahnamoii M, Ebrahimi-Chaharom ME, Sadr A, Daneshi M. Effect of 15% carbamide peroxide bleaching gel on color stability of giomer and microfilled composite resin: an in vitro comparison. Med Oral Patol Oral Cir Bucal. 2012;17:e1082–e1088. doi: 10.4317/medoral.17916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hotwani K, Thosar N, Baliga S. Comparative in vitro assessment of color stability of hybrid esthetic restorative materials against various children’s beverages. J Conserv Dent. 2014;17:70–74. doi: 10.4103/0972-0707.124154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rajavardhan K, Sankar A, Kumar M, Kumar K, Pranitha K, Kishore K. Erosive potential of cola and orange fruit juice on tooth colored restorative materials. Ann Med Health Sci Res. 2014;4(Suppl 3):S208–S212. doi: 10.4103/2141-9248.141960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tanthanuch S, Kukiattrakoon B, Siriporananon C, Ornprasert N, Mettasitthikorn W, Likhitpreeda S, et al. The effect of different beverages on surface hardness of nanohybrid resin composite and giomer. J Conserv Dent. 2014;17:261–265. doi: 10.4103/0972-0707.131791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kimyai S, Lotfipour F, Pourabbas R, Sadr A, Nikazar S, Milani M. Effect of two prophylaxis methods on adherence of Streptococcus mutans to microfilled composite resin and giomer surfaces. Med Oral Patol Oral Cir Bucal. 2011;16:e561–e567. doi: 10.4317/medoral.16.e561. [DOI] [PubMed] [Google Scholar]
- 41.Kimyai S, Savadi-Oskoee S, Ajami AA, Sadr A, Asdagh S. Effect of three prophylaxis methods on surface roughness of giomer. Med Oral Patol Oral Cir Bucal. 2011;16:e110–e114. doi: 10.4317/medoral.16.e110. [DOI] [PubMed] [Google Scholar]
- 42.Suzuki M, Yamada A, Saito K, Hino R, Sugawara Y, Ono M, Naruse M, Arakaki M, Fukumoto S. Application of a tooth-surface coating material containing pre-reacted glass-ionomer fillers for caries prevention. Pediatr Dent J. 2015;25:72–78. [Google Scholar]
- 43.Yoshihara K, Nagaoka N, Maruo Y, Sano Y, Yoshida Y, Van Meerbeek B. Bacterial adhesion not inhibited by ion-releasing bioactive glass filler. Dent Mater. 2017;33:723–734. doi: 10.1016/j.dental.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 44.Chitnis D, Dunn WJ, Gonzales DA. Comparison of in-vitro bond strengths between resin-modified glass ionomer, polyacid-modified composite resin, and giomer adhesive systems. Am J Orthod Dentofacial Orthop. 2006;129:e11–e16. doi: 10.1016/j.ajodo.2005.11.011. [DOI] [PubMed] [Google Scholar]