Abstract
Fracture acetabulum is a grave injury and a challenge for orthopedic surgeons. Anterior and posterior approaches have been described for fixation of acetabulum fractures. The modified Stoppa approach is considered an alternate to anterior approach, which provides access to pelvis from inside the cavity. The purpose of this article is to review the available literature on use of the modified Stoppa approach in acetabulum fractures. The available data suggest that modified Stoppa approach is useful in anterior acetabulum fractures and some posterior acetabulum fractures, especially where buttressing of medial wall is required.
Keywords: acetabulum, fractures bone, fracture fixation, modified stoppa
Introduction
Treatment of acetabular fractures is a challenge for an orthopaedic surgeon. Understanding three dimensional anatomy and fixing the fracture accordingly is the key to treat. After initial work done by Judet 1 and Letournel 2 who described the classification system and approaches, various modifications of approaches have been developed to improve outcome. Ilioinguinal approach was originally described by Letournel 3 in 1961 for fixation of fracture acetabulum. As an intrapelvic approach, it became popular for fixation of anterior wall and column fractures, anterior fractures associated with post hemitransverse fractures and even both column fractures.
Stoppa approach has been used for treatment of inguinal Stoppa approach has been used for treatment of inguinal hernias. 4 5 Hirvensalo et al 6 in 1993 and Cole and Bolhofner 7 in 1994 were the first who independently described intrapelvic extraperitoneal approaches for fixation of pelvic acetabulum fractures which was a modification of stoppa approach.
Modified stoppa approach provides direct access to the pubic bones, the posterior surface of the ramus, the quadrilateral surface, the pubic eminence, and the infrapectineal surface. This approach also provides access as to the sciatic buttress, sciatic notch, and anterior sacroiliac joint. This approach provides mechanical advantage in reduction and fixation of medial displaced fractures as compare to other approaches and claimed to be a viable alternative of ilioinguinal approach for treatment of anterior acetabulum fractures. Though studies are available on use of modified stoppa approach for acetabulum fracture, there is no review article available. For the first time we review the literature on modification of stoppa approach for acetabulum fractures.
Materials and Methods
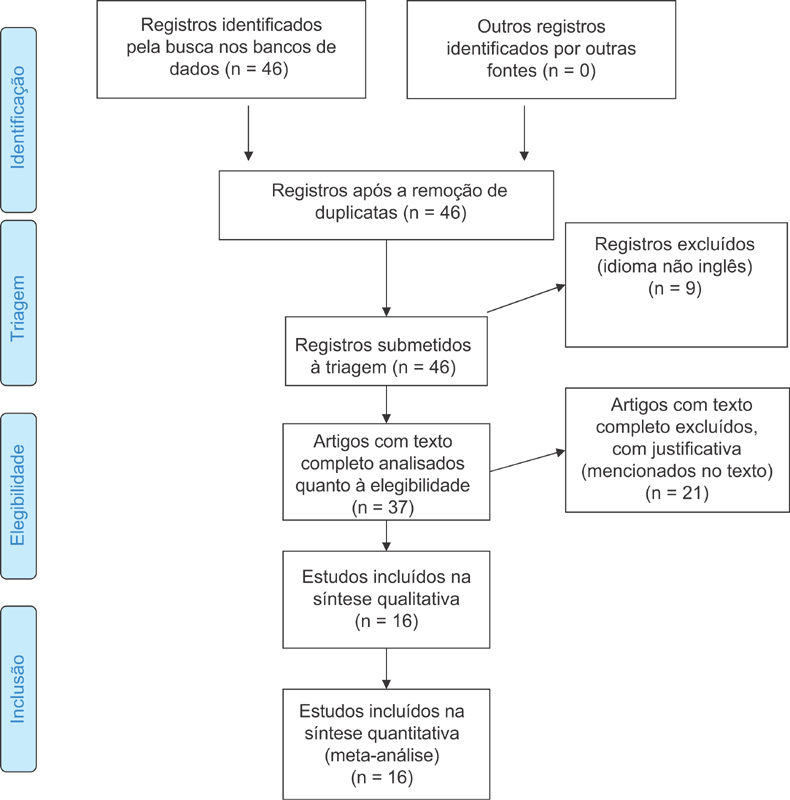
The methodology is described in PRISMA flow diagram ( Fig. 1 ). The Pubmed/Medline and Cochrane database were searched with keywords “modified stoppa,” “anterior intra pelvic,” “anterior intrapelvic,” “extended pfannensteil,” “ilio anterior,” and “third window ilioinguinal” to retrieve the articles in which modified stoppa approach was used to fix acetabulum fractures (on 22 December 2016). The keywords we used were the alternate names by which modified stoppa approach is described in literature. Inclusion criteria were-all articles where modified stoppa approach was used to fix acetabulum fractures. Exclusion criteria were-articles in language other than English, case reports, cadaveric studies, articles without clinical experience, associated pelvic ring injuries and articles where ilioinguinal approach was used. The articles were evaluated for demographic data, mode of injury, classification of fracture, delay in surgery, surgical time, blood loss, additional approaches used, functional and radiological outcome and complications. Total 552 articles were found. 506 articles were not related to modified stoppa approach for acetabulum fractures. Nine article were excluded which were regarding modified stoppa approach for acetabulum fractures but in language other than English. Three cadaveric studies 8 9 10 and two case reports 11 12 were excluded. Nine articles 13 14 15 16 17 18 19 20 21 were excluded in which modified stoppa approach was described as a technique without clinical experience. Three articles were excluded as patients treated for pelvic ring injuries were also included in these studies. 22 23 24 One article by Chesser et al 25 was excluded as patients treated using ilioinguinal approach were also included in this study. One article by Bastian et al 26 was excluded as in 9% of patients in this study modified stoppa approach was changed to ilioinguinal approach intraoperatively and the results were combined for ilioinguinal and modified stoppa approach. Two articles by Keel et al 27 28 were excluded. In these studies the author described pararectus approach where fracture was approached from a plane lateral to rectus muscles. The author himself described their technique different from modified stoppa approach and claimed it to be better than modified stoppa approach.
Fig. 1.
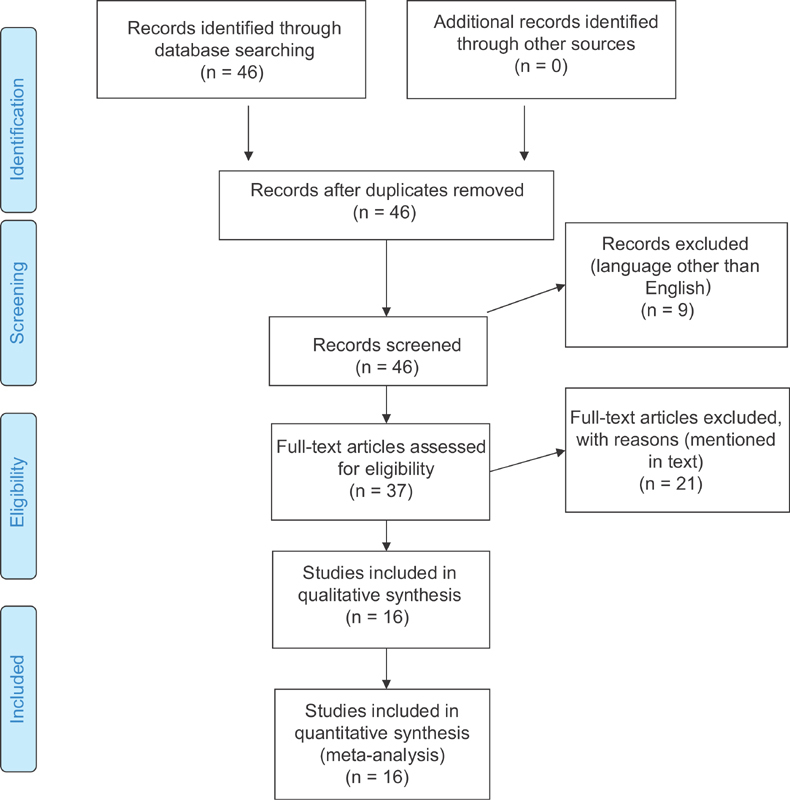
PRISMA flow chart.
Results
Total 16 articles were found to match our selection criteria including one retrospective study by Rocca et al 29 comparing ilioinguinal approach with stoppa approach. The demography of patients was described combined for modified stoppa and ilioinguinal approaches but results were analyzed separately. We included this article in our review while analyzing the outcomes (post op reduction using Matta's method, functional outcome using Matta's modification of Merle d'Aubinne score and Matta's radiological criteria in this study) but excluded it while analyzing the demographic data of patients. References of all 16 articles were manually searched for any missing article. Data are extracted for age, sex ratio, mode of injury, classification of fracture, delay in surgery, surgical time, blood loss, additional approaches used, functional and radiological outcome and complications.
Demography
In 16 studies total 609 patients were treated for fracture acetabulum with modified stoppa approach. 7 30 31 32 33 34 35 36 37 38 39 40 41 42 43 There were 427 males and 139 females. The ratio for male to female was available for 566 patients. 7 30 31 32 33 34 35 36 37 38 39 40 41 42 43 Out of total 609 patients we excluded 34 patients treated by Rocca et al 29 because the demographic data of these patients was described combined with patients treated with ilioinguinal approach. Out of 10 patients treated by Casstevens et al 36 male female ratio was available for eight patients. Out of 57 patients treated by Sagi et al 31 seven patients were skeletally immature and were evaluated only for surgical approach, surgical time, blood loss and complications. In all studies male patients outnumbered females.
In 11 studies (326 patients) age varies between 10–88 years. 7 30 31 32 33 34 35 37 39 41 42 Age was described as mean age by Elmadag et al, 40 Shazar et al 38 and Dailey et al 43 which was 49.3 years, 41.88 ± 15.7 years and 55.88 ± 20.31 years in their respective studies.
Mode of Injury
Mode of injury was evaluated from 6 studies (271 patients). 31 32 33 35 39 42 43 Road traffic accident was the most common mode in 129 patients followed by fall from height in 108 patients, industrial accident in six patients, crush injury in three patients and sports injury in one patient. Cole et al 7 reported road traffic accident as the most common mode of injury in 83% of their 55 patients.
Classification of Fractures
In 14 studies 456 patients were classified according to Judet and Letournel classification. 7 30 31 32 33 34 35 36 37 38 39 40 41 42 There were 128 associated both column, 89 anterior column with posterior hemi-transverse, 84 anterior column, 54 T type, 53 transverse, 29 transverse with posterior wall, 13 anterior column, three anterior column with wall, two anterior wall and one posterior column fractures. The most common fracture pattern was both column fracture in six studies and anterior column in five studies. Dailey et al 43 used anterior intrapelvic approach (AIP) in patients with associated both column fracture and anterior column with posterior hemi-transverse fracture only in 112 patients.
Delay in Surgery
Time delay for surgery was mentioned in eight studies (260 patients) ranges from 0 day to 30 days. 7 31 32 33 34 35 39 40 41 Mean time from injury to surgery was 4.83 + /-3.74 in study by Dailey et al. 43
Surgical Time
Surgical time ranges from 80 minutes to 568 minutes in seven studies (250 patients). 7 30 33 35 39 41 42 Anderson et al 30 described surgical time as time which includes breaking down the sterile field, obtaining postoperative radiographs, and having the attending physician review the radiographs after they are developed, a process that takes at least 30 minutes. In their study the time ranges from three hours to eight hours 48 minutes. Casstevens et al 36 described surgical time as median surgical time which was 232 minutes for their 10 patients. Shazar et al, 38 Laflamme et al 32 and Dailey et al 43 described surgical time as mean surgical time which was 240.5 minutes, 167 ± 41 minutes and 276.59 ± 103.66 for their 103 patients, 21 patients and 112 patients respectively.
Blood Loss
Estimated blood loss in 9 studies (299 patients) ranges from 100 ml – 5000 ml. 7 29 30 32 33 35 39 40 41 Casstevens et al, 36 Laflamme et al 32 and Dailey et al 43 described blood loss as mean blood loss which was 1270 mL, 1376 ± 608 mL and 1159.73 ± 1072.5 mL in 10 patients, 21 patients and 112 patients respectively.
Approach
Modified stoppa approach was combined with kocher langenbeck, lateral window and medial window of ilio inguinal approach in various studies ( Table 1 ).
Table 1. Approaches used by authors.
| Sr no | No of patients | Approach | |
|---|---|---|---|
| 1 | Elmadag et al 33 | 36 | MS |
| 2 | Hammad et al 42 | 21 | MS ± LW 14% requires KL |
| 3 | Kim et al 34 | 22 | MS – 13 MS + KL – 9 (5 ACPHT, 4 Trans + PW) MS + LW – 2 |
| 4 | Rocca et al 29 | 34 | MS + LW (Ace approach) |
| 5 | Elmadag et al 40 | 17 | MS |
| 6 | Shazar et al 38 | 103 | MS – 32 MS + LW – 57 MS + KL – 11 MS + MW + LW - 2 MS + SP - 1 |
| 7 | Laflamme and Herbert-Davies 37 | 9 | MS + LW |
| 8 | Casstevens et al 36 | 10 | MS |
| 9 | Liu et al 35 | 29 | MS + LW (Newly modified stoppa approach) |
| 10 | Ma et al 39 | 30 | MS – 8 MS + LW – 22 |
| 11 | Anderson et al 30 | 17 | MS + Post app – excluded from study MS + LW – included Exact no not mentioned |
| 12 | Sagi et al 31 | 57 (7 sklt immature) |
MS – 23 MS + LW – 34 (additional SM in 2 pt) (AIP approach) |
| 13 | Isaacson et al 41 | 36 | MS + LW – 23 MS + KL – 3 |
| 14 | Laflamme et al 32 | 21 | MS + LW |
| 15 | Cole and Bolhofner 7 | 55 | Only MS – 32 MS + KL – 18 primarily anterior approach) (6 patients required lateral Avila approach in addition to primarily anterior approach) |
| 16 | Dailey and Archdeacon 43 | 112 | AIP approach (as described by Sagi HC et al 9 ) |
Abbreviations: ACPHT, Anterior column posterior hemitransverse fracture; KL, Kocher Langenbech; LW, Lateral window of ilioinguinal; MS, modified Stoppa; MW, Medial window of ilioinguinal; SP, Smith Peterson; Trans + PW, Transverse with posterior wall fracture.
Outcome
Post op reduction – Matta's method
Post operatively fracture reduction was evaluated in 12 studies (408 patients) by using scoring system described by Matta 44 in 1996. 30 31 32 33 34 35 37 38 39 41 42 Reduction was anatomic (≤ 1 mm) in 290 patients, imperfect (> 1 to < 3 mm) in 77 patients and poor (≥ 3 mm) in 34 patients. Seven patients had either anatomic or imperfect reductions. Hammad et al 42 found that out of 10 patients with poor outcome six had type B fracture acetabulum and 10 patients with anatomical reduction, 6 had type C fracture. Sagi et al 31 found that poor fracture reductions occurred most frequently (75%) with associated both column fractures. In their results percentage of excellent reduction was maximum (92%) in anterior column fracture whereas percentage of excellent reduction was minimum (67%) in transverse fractures. Similarly the lowest percentage of excellent reduction (75%) was found in transverse fractures by Shazar et al 38 but in their study highest percentage (92.9%) of anatomical reduction was achieved in anterior column with posterior hemi-transverse fractures.
Harris Hip Score
Harris hip score was evaluated by four studies. 32 35 37 40 In three studies (82 patients) Harris hip score was 35 excellent, 34 good, eight fair and five poor. 32 35 40 Laflamme et al 37 found mean Harris hip score 81 (range 51–100) in a series of 9 patients.
Merle d'Aubinne score
In four studies 30 32 39 40 (133 patients) Merle d'Aubinne score 45 46 was 58 excellent, 59 good, eight fair, eight poor. Isaacson et al 41 in their study described 12 very good, two good, four medium, one fair and three poor results according to Merle d'Aubinne score. 45
Matta modification of Merle d'Aubinne score
Matta's modification of Merle d'Aubinne score 44 47 was used to evaluate the functional results three studies 33 34 42 (72 patents). 15 patients had excellent, 30 had good, 11 had fair, 16 had poor results. Cole et al 7 in their study described functional results according to Matta modification of Merle d'Aubinne score 47 in percentage. The authors had 47% excellent, 42% good, 9% fair and 2% poor results.
Matta's Radiological Criteria
In three studies 34 36 39 (70 patients) radiological results were classified according to Matta. 44 47 45 excellent, 14 good, 6 fair and 5 poor results were found. Cole et al 7 in their study described radiological score according to Matta's radiological criteria 47 in percentage. The authors had 64% excellent, 25% good, 7% fair and 4% poor results. Laflamme et al 32 evaluated the functional results of internal fixation of osteopenic acetabular fractures involving quadrilateral plate in 19 elderly patients. 31 He found (mean ± SD) SF-12 PCS – 45.3 ( ± 12.1), SF-12 MCS – 55.9 ( ± 8.5), PMA – 16.8 ( ± 1.3), HHS (Harris Hip Score) – 86.2 ( ± 13.9), WOMAC (pain) – 3.4 ( ± 3.5), WOMAC (stiffness) – 1.3 ( ± 1.5), WOMAC (ADL) – 11.7 ( ± 12.2).
Complications
Obturator nerve injury was the most frequent complication whereas hip joint arthritis was the most frequent late complication ( Table 2 ).
Table 2. Complications.
| Complications | No of patients | Management |
|---|---|---|
| Intra operative complications | ||
| Corona mortis injury | 2 | Packing and ligation in 1 patient Details of 1 patient not mentioned |
| Obturator artery injury | 1 | Packing and ligation |
| External iliac vein injury | 1 | Primary repair |
| Superior gluteal artery injury | 1 | Packing and embolization |
| Post-operative complications | ||
| Obturator nerve injury | 21 | Recovered in 3–6 months in 20 patients Partial recovery in 1 patient |
| Deep infection | 13 | Debridement and antibiotics in 11 patients Debridement, antibiotics and plate removal in 1 patient Hip joint fusion in 1 patient |
| Lateral femoral cutaneous nerve palsy | 8 | Recovered in 3–6 months in 5 patients Details not mentioned for 2 patients |
| Foot drop | 5 | Recovered in 6–12 months |
| Superficial infection | 5 | Dressing and antibiotics |
| Deep vein thrombosis | 7 | Chemical prophylaxis in 1 patient |
| Details not mentioned for 3 patients | ||
| Intra articular screw | 2 | Removed |
| Sciatic nerve palsy | 1 | Recovered in 6 weeks |
| Seroma at operative site | 1 | Treated operatively, no infection was found |
| Peritoneum breach | 1 | Wound was closed without sequelae |
| Wound dehiscence | 1 | Surgical closure done |
| Delayed wound healing | 1 | Healed in 3 weeks with infra-red heat lamp treatment |
| Late complications | ||
| Hip joint arthritis | 15 | |
| Ectopic bone formation | 9 | Conservative in 3 patients with full range of motion Details not mentioned for 6 patients |
| Avascular necrosis femur head | 5 | |
| Loss of reduction | 4 | THR done in 2 patients Details not mentioned for 2 patients |
| Rectus atrophy without hernia | 2 | |
| Lateral inguinal hernia | 4 | Repair done |
| Non-union | 1 | Fixation and bone grafting at 10 months |
| Other complications | ||
| Fatal pulmonary embolism | 2 | |
| Non-fatal pulmonary embolism | 1 | |
| Stroke | 1 | |
| Common iliac artery thrombosis | 1 | |
| Fatal liver cirrhosis | 1 | |
Discussion
Judet et al 48 described acetabulum as a socket surrounded and supported by an arch formed by two columns of bones, anterior and posterior, and roof of the acetabulum as keystone of this arch. He emphasised on the importance of these columns saying that in order to fix acetabulum fracture these columns should be restored.
The classical approach to fix posterior and anterior column fracture is kocher langenback and ilioinguinal approach respectively. However with time other approaches were developed for anterior acetabulum.
Hirvensalo et al 6 in 1993 and Cole et al 7 in 1994 were the first to describe the use of preperitoneal space to fix the pelvic fractures. Hirvensalo et al 6 treated 18 pelvic ring injuries using low Pfannensteil approach. Rectus abdominis and pectineus muscles were detached from the rami and subperiosteal discetion was done along the inner surface of pelvic brim up to sacroiliac joint. Iliopectineal fascia, external iliac vessels, femoral nerve and psoas muscle were undisturbed. Obturator vessels, nerves and corona mortis were protected. The approach was termed as “the ilioanterior approach”. The lateral window of ilioinguinal approach was used along with this ilioanterior approach when fracture extended to that region. Since this study included pelvic ring injuries, we excluded this study from our review. Cole and Bolhofner 7 treated 55 acetabular fractures with intrapelvic approach which they termed as “Extended Pfennensteil” but after further discussion and research it was later termed as “modified Stoppa” approach, quit similar to Stoppa approach used to repair hernia. The authors extended the stoppa approach posteriorly along the brim elevating the iliopectinel and obturator fascia. The authors concluded that this new approach may offer improved reduction and fixation of certain types of acetabular fractures and may decrease the rate of complications associated with extrapelvic extensile approaches.
Alternate to Ilioinguinal Approach
Modified stoppa approach along with or without other approaches provides alternate to ilioinguinal approach for fixation of anterior acetabulum fractures, 30 32 33 34 35 39 Elmadag et al 33 concluded in their retrospective study of 36 patients that modified stoppa approach is a good alternative to ilioinguinal approach even for many complex acetabular fractures despite a steep learning curve due to proximity of neurovascular structure. Kim et al 34 in their study of 22 patients concluded that modified stoppa approach can be an alternative to classic ilioinguinal approach with excellent and good results though comminution of acetabular fracture was important factor leads to non anatomic reduction and unsatisfactory clinical results.
Access to Quadrilateral Plate
Modified stoppa approach provides access to acetabulum from inside the pelvis making easy to address the fractures involving quadrilateral plate. 30 31 34 35 42 Laflamme et al 32 stated that quadrangular plate can be fixed so well using this approach that it can be a viable alternate to arthroplasty in old patients or patients having osteoporosis with certain fracture acetabulum. The author treated 21 patients, more than 60 year of age or with established osteoporosis, with acetabular fractures involving quadrilateral plate. Modified stopaa approach along with lateral window was used to fix acetabular fractures and buttress the quadrilateral plate. The authors concluded that the initial treatment of osteoporotic acetabular fracture involving anterior column and quadrilateral plate, fixation of fracture using modified stoppa approach to butteress the quadrilateral plate should be considered as a viable alterantive to total hip artrhoplasty.
Access to Posterior Column
Modified stoppa approach when combined with lateral window of ilioinguinal approach provides access to posterior column also. This helps in fixation of fracture anterior acetabulum extending into posterior acetabulum. 29 30 41 Using modified stoppa approach along with lateral window of ilioinguinal, Anderson RC et al treated 17 young patients (age < 60 years) having acetabular fractures with anterior and posterior column displaced. 29 The authors concluded that in certain fractures involving displaced anterior and posterior columns (even with more than 5 mm displacement of posterior column), anatomic or imperfect reduction can be achieved using modified stoppa approach along with lateral window of ilioinguinal approach. Isaacson et al in their prospective study of 36 patients reported good functional outcome with minimal complication rates using modified stoppa approach for acetabular fractures including fractures extending into and displacing posterior column. 41 Though, author highlighted the difficulty but feasibility of treating posterior column displacement by anterior approach alone.
Variations of the Approach
Though many authors combine modified stoppa approach with other approaches ( Table 2 ), certain modifications of the approach have also been described. 30 34 35 Rocca et al 29 combined modified stoppa approach, as described by Cole and Bolhofner, with proximal and lateral window of ilioinguinal approach and termed it as Anterior Combined Endopelvic (ACE) approach. Sagi et al 31 described modification of Rives-Stoppa approach as Anterior Intra-Pelvic (AIP) approach. Lateral window of ilioinguinal approach was used along with if required. Excellent visualization and access to the quadrilateral plate and posterior column was reported. Good to excellent reduction in majority of cases was achieved with complication rates comparable to ilioinguinal approach. The authors found the approach helpful when comminution of quadrilateral plate and posterior column exists and recommended this technique as a potential alternative to the ilioinguinal approach for anterior exposure of acetabulum. Instead of using midline incision, Liu et al 35 treated 29 acetabular fractures through the inner two-third of the line 2 cm above the inguinal ligament and parallel to it. Rectus fascia was split, inferior epigastric artery was ligated and transversalis fascia was incised just superior to the symphysis pubis. this anterior approach was combined with lateral approach on the iliac crest. The approach was termed as ‘Newly modified Stoppa approach’. The authors concluded that this approach provides excellent access to anterior column, quadrilateral surface and scitic notch, permits excellent reduction, fixation and good postoperative outcomes and is a viable alternative to ilioinguinal approach. The complication rates were found to be comparable to ilioinguinal approach.
Different Technical Tricks
Since operating surgeon can approach acetabulum from inside the pelvis using modifies stoppa approach, different technical tips were described utilising this advantage. Casstevens et al 36 in 10 patients described a technical trick using modifies stoppa approach to reduce and buttress screw fixation of impacted dome of acetabulum. Similarly Laflamme et al, 37 in nine patients described technical trick of direct reduction of superomedial dome impaction in geriatric acetabular fractures using modified stoppa approach.
Timing of Surgery
We found only one study evaluating the effect of timing of surgery using modified ilioinguinal approach. Dailey et al 43 evaluated influence of timing of surgery on blood loss and surgery time in patients with fracture acetabulum. 176 patients having posterior wall fracture acetabulum were treated with kocher langenbeck approach. 112 patients having associated both column fracture or anterior column with posterior hemi-transverse fracture were treated with anterior intrapelvic approach. We included in our study 112 patients treated with anterior intrapelvic approach. The author did not find any difference in terms of blood loss or operative time for early (< 48 hours) or late (> 48 hours) fixation of fractures, either posterior wall or associated both column/ anterior column with posterior hemi-transverse.
Comparison with Ilioinguinal Approach
Five studies compared the results of stoppa approach vs ilioinguinal approach in fixation of fracture acetabulum. 34 38 39 40 42 Rocca et al 29 treated 34 patients using ACE approach (modified stoppa approach combined with lateral window of ilioinguinal approach) and compared it with 42 patients treated with ilioinguinal approach for fracture acetabulum. It was concluded that ACE technique is an easier and viable alternative to ilioinguinal approach to expose anterior acetabulum and quadrilateral plate with slightly better clinical outcome and comparable complication rates. Hammad AS et al concluded that reduction accuracy and clinical scores were similar with both approaches. 42 The stoppa approach might be more advantageous in direct buttressing of quadrilateral plate and associated both column fractures whereas middle window of ilioinguinal approach better exposes anterior wall and transversly oriented fractures. Elmadag et al 40 concluded that there is no advantage of stoppa approach over ilioinguinal in term of complications and bleeding except the former has cosmetically better scar. Also with stoppa approach bilateral fractures can be treated with single incision and better visualization is provided in lateral compression injuries. Shazar et al 38 concluded that AIP approach provides higher rate of anatomical reduction as compare to ilioinguinal approach in lesser surgical time with comparable complications rates. Ma et al 39 concluded that there was no significant difference in reduction quality, imaging follow-up results, clinical outcomes and complications between modified stoppa approach and ilioinguinal approach in acetabular fracture fixation. However operative time, blood loss, wound drainage and blood transfusion is less with stoppa approach. The author recommended stoppa approach for anterior exposure of acetabulum, especially for fracture involving quadrilateral plate.
The present studies on modified stoppa approach for treating acetabulum fractures are highly variable in term of their study design. Different methods of result assessments were used by different authors. Different modifications and technical tricks have also been described with different aims and objectives using this approach. Moreover associated pelvic ring fractures and additional use of other approaches for acetabulum fractures makes it difficult to evaluate the results of modified stoppa approach in acetabulum fractures.
Conclusion
Though there is high variability of study design in past studies, the available literature suggests that modified stoppa approach is useful anterior approach for fixation of fracture acetabulum especially for buttressing the quadrilateral plate. Posterior column fractures can be addressed with this approach or it can be fixed with combined KL approach. For fractures extending to the iliac crest, a lateral window can be made without exposing the neurovascular bundle as done in ilioinguinal approach. Good reduction is achieved with acceptable complication rates with this approach.
Conflitos de Interesse Os autores declaram não haver conflitos de interesse.
Estudo conduzido no Department of Orthopedics, Government Medical College and Hospital, Chandigarh, Índia.
Study conducted at Department of Orthopedics, Government Medical College and Hospital, Chandigarh, India. Publishied originally by Elsevier Editora Ltda.
References
- 1.Judet R, Judet J, Letournel E. [Surgical treatment of recent fractures of the acetabulum. (Apropos of 46 operated cases)] Mem Acad Chir (Paris) 1962;88:369–377. [PubMed] [Google Scholar]
- 2.Letournel E, Judet R. New York: Springer-Verlag; 1974. Fractures of the acetabulum. 2nd. [Google Scholar]
- 3.Letournel E. Fractures of the cotyloid cavity, study of a series of 75 cases] J Chir (Paris) 1961;82:47–87. [PubMed] [Google Scholar]
- 4.Rives J, Stoppa R, Fortesa L, Nicaise H. [Dacron patches and their place in surgery of groin hernia. 65 cases collected from a complete series of 274 hernia operations] Ann Chir. 1968;22(03):159–171. [PubMed] [Google Scholar]
- 5.Stoppa R E, Rives J L, Warlaumont C R, Palot J P, Verhaeghe P J, Delattre J F. The use of Dacron in the repair of hernias of the groin. Surg Clin North Am. 1984;64(02):269–285. doi: 10.1016/s0039-6109(16)43284-6. [DOI] [PubMed] [Google Scholar]
- 6.Hirvensalo E, Lindahl J, Böstman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res. 1993;(297):28–32. [PubMed] [Google Scholar]
- 7.Cole J D, Bolhofner B R. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994;(305):112–123. [PubMed] [Google Scholar]
- 8.Bastian J D, Savic M, Cullmann J L, Zech W D, Djonov V, Keel M J. Surgical exposures and options for instrumentation in acetabular fracture fixation: Pararectus approach versus the modified Stoppa. Injury. 2016;47(03):695–701. doi: 10.1016/j.injury.2016.01.025. [DOI] [PubMed] [Google Scholar]
- 9.Bible J E, Choxi A A, Kadakia R J, Evans J M, Mir H R. Quantification of bony pelvic exposure through the modified Stoppa approach. J Orthop Trauma. 2014;28(06):320–323. doi: 10.1097/BOT.0000000000000032. [DOI] [PubMed] [Google Scholar]
- 10.Kacra B K, Arazi M, Cicekcibasi A E, Büyükmumcu M, Demirci S. Modified medial Stoppa approach for acetabular fractures: an anatomic study. J Trauma. 2011;71(05):1340–1344. doi: 10.1097/TA.0b013e3182092e8b. [DOI] [PubMed] [Google Scholar]
- 11.Murcia-Asensio A, Ferrero-Manzanal F, Lax-Pérez R, Fernández-Fairén M. Stoppa approach for intrapelvic damage control and reconstruction of complex acetabular defects with intra-pelvic socket migration: A case report. Int J Surg Case Rep. 2016;25:143–148. doi: 10.1016/j.ijscr.2016.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elmadag M, Acar M A. A modified stoppa (technique) approach for treatment of pediatric acetabular fractures. Case Rep Orthop. 2013;2013:478131. doi: 10.1155/2013/478131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Archdeacon M T, Kazemi N, Guy P, Sagi H C. The modified Stoppa approach for acetabular fracture. J Am Acad Orthop Surg. 2011;19(03):170–175. doi: 10.5435/00124635-201103000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Archdeacon M T. Comparison of the ilioinguinal approach and the anterior intrapelvic approaches for open reduction and internal fixation of the acetabulum. J Orthop Trauma. 2015;29 02:S6–S9. doi: 10.1097/BOT.0000000000000270. [DOI] [PubMed] [Google Scholar]
- 15.Collinge C A, Lebus G F. Techniques for reduction of the quadrilateral surface and dome impaction when using the anterior intrapelvic (modified Stoppa) approach. J Orthop Trauma. 2015;29 02:S20–S24. doi: 10.1097/BOT.0000000000000271. [DOI] [PubMed] [Google Scholar]
- 16.Guy P. Evolution of the anterior intrapelvic (Stoppa) approach for acetabular fracture surgery. J Orthop Trauma. 2015;29 02:S1–S5. doi: 10.1097/BOT.0000000000000269. [DOI] [PubMed] [Google Scholar]
- 17.Hagen J E, Weatherford B M, Nascone J W, Sciadini M F. Anterior intrapelvic modification to the ilioinguinal approach. J Orthop Trauma. 2015;29 02:S10–S13. doi: 10.1097/BOT.0000000000000266. [DOI] [PubMed] [Google Scholar]
- 18.Khoury A, Weill Y, Mosheiff R.The Stoppa approach for acetabular fracture Oper Orthop Traumatol 201224(4-5):439–448. [DOI] [PubMed] [Google Scholar]
- 19.Kistler B J, Sagi H C. Reduction of the posterior column in displaced acetabulum fractures through the anterior intrapelvic approach. J Orthop Trauma. 2015;29 02:S14–S19. doi: 10.1097/BOT.0000000000000267. [DOI] [PubMed] [Google Scholar]
- 20.Qureshi A A, Archdeacon M T, Jenkins M A, Infante A, DiPasquale T, Bolhofner B R. Infrapectineal plating for acetabular fractures: a technical adjunct to internal fixation. J Orthop Trauma. 2004;18(03):175–178. doi: 10.1097/00005131-200403000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Sagi H C, Bolhofner B. Osteotomy of the Anterior Superior Iliac Spine as an Adjunct to Improve Access and Visualization Through the Lateral Window. J Orthop Trauma. 2015;29(08):e266–e269. doi: 10.1097/BOT.0000000000000283. [DOI] [PubMed] [Google Scholar]
- 22.Vikmanis A, Vikmanis A, Jakusonoka R, Jumtins A, Pavare Z. Mid-term outcome of patients with pelvic and acetabular fractures following internal fixation through a modified Stoppa approach. Acta Orthop Belg. 2013;79(06):660–666. [PubMed] [Google Scholar]
- 23.Jakob M, Droeser R, Zobrist R, Messmer P, Regazzoni P. A less invasive anterior intrapelvic approach for the treatment of acetabular fractures and pelvic ring injuries. J Trauma. 2006;60(06):1364–1370. doi: 10.1097/01.ta.0000208139.97474.f7. [DOI] [PubMed] [Google Scholar]
- 24.Ponsen K J, Joosse P, Schigt A, Goslings J C, Luitse J S.Internal fracturefixation using the Stoppa approach in pelvic ring and acetabular fractures: technical aspects and operative results J Trauma 20066103662–667.. Erratum in. J Trauma 2007;62(6):1490 [DOI] [PubMed] [Google Scholar]
- 25.Chesser T J, Eardley W, Mattin A, Lindh A M, Acharya M, Ward A J. The modified ilioinguinal and anterior intrapelvic approaches for acetabular fracture fixation: indications, quality of reduction, and early outcome. J Orthop Trauma. 2015;29 02:S25–S28. doi: 10.1097/BOT.0000000000000268. [DOI] [PubMed] [Google Scholar]
- 26.Bastian J D, Tannast M, Siebenrock K A, Keel M J. Mid-term results in relation to age and analysis of predictive factors after fixation of acetabular fractures using the modified Stoppa approach. Injury. 2013;44(12):1793–1798. doi: 10.1016/j.injury.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 27.Keel M J, Tomagra S, Bonel H M, Siebenrock K A, Bastian J D. Clinical results of acetabular fracture management with the Pararectus approach. Injury. 2014;45(12):1900–1907. doi: 10.1016/j.injury.2014.10.040. [DOI] [PubMed] [Google Scholar]
- 28.Keel M J, Ecker T M, Cullmann J L, Bergmann M, Bonel H M, Büchler L et al. The Pararectus approach for anterior intrapelvic management of acetabular fractures: an anatomical study and clinical evaluation. J Bone Joint Surg Br. 2012;94(03):405–411. doi: 10.1302/0301-620X.94B3.27801. [DOI] [PubMed] [Google Scholar]
- 29.Rocca G, Spina M, Mazzi M. Anterior Combined Endopelvic (ACE) approach for the treatment of acetabular and pelvic ring fractures: A new proposal. Injury. 2014;45 06:S9–S15. doi: 10.1016/j.injury.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 30.Andersen R C, O'Toole R V, Nascone J W, Sciadini M F, Frisch H M, Turen C W. Modified stoppa approach for acetabular fractures with anterior and posterior column displacement: quantification of radiographic reduction and analysis of interobserver variability. J Orthop Trauma. 2010;24(05):271–278. doi: 10.1097/BOT.0b013e3181b2b4ca. [DOI] [PubMed] [Google Scholar]
- 31.Sagi H C, Afsari A, Dziadosz D. The anterior intra-pelvic (modified rives-stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010;24(05):263–270. doi: 10.1097/BOT.0b013e3181dd0b84. [DOI] [PubMed] [Google Scholar]
- 32.Laflamme G Y, Hebert-Davies J, Rouleau D, Benoit B, Leduc S. Internal fixation of osteopenic acetabular fractures involving the quadrilateral plate. Injury. 2011;42(10):1130–1134. doi: 10.1016/j.injury.2010.11.060. [DOI] [PubMed] [Google Scholar]
- 33.Elmadag M, Guzel Y, Aksoy Y, Arazi M. Surgical Treatment of Displaced Acetabular Fractures Using a Modified Stoppa Approach. Orthopedics. 2016;39(02):e340–e345. doi: 10.3928/01477447-20160222-07. [DOI] [PubMed] [Google Scholar]
- 34.Kim H Y, Yang D S, Park C K, Choy W S. Modified Stoppa approach for surgical treatment of acetabular fracture. Clin Orthop Surg. 2015;7(01):29–38. doi: 10.4055/cios.2015.7.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu Y, Yang H, Li X, Yang S H, Lin J H. Newly modified Stoppa approach for acetabular fractures. Int Orthop. 2013;37(07):1347–1353. doi: 10.1007/s00264-013-1920-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Casstevens C, Archdeacon M T, dʼHeurle A, Finnan R. Intrapelvic reduction and buttress screw stabilization of dome impaction of the acetabulum: a technical trick. J Orthop Trauma. 2014;28(06):e133–e137. doi: 10.1097/BOT.0000000000000005. [DOI] [PubMed] [Google Scholar]
- 37.Laflamme G Y, Hebert-Davies J. Direct reduction technique for superomedial dome impaction in geriatric acetabular fractures. J Orthop Trauma. 2014;28(02):e39–e43. doi: 10.1097/BOT.0b013e318298ef0a. [DOI] [PubMed] [Google Scholar]
- 38.Shazar N, Eshed I, Ackshota N, Hershkovich O, Khazanov A, Herman A. Comparison of acetabular fracture reduction quality by the ilioinguinal or the anterior intrapelvic (modified Rives-Stoppa) surgical approaches. J Orthop Trauma. 2014;28(06):313–319. doi: 10.1097/01.bot.0000435627.56658.53. [DOI] [PubMed] [Google Scholar]
- 39.Ma K, Luan F, Wang X, Ao Y, Liang Y, Fang Y et al. Randomized, controlled trial of the modified Stoppa versus the ilioinguinal approach for acetabular fractures. Orthopedics. 2013;36(10):e1307–e1315. doi: 10.3928/01477447-20130920-25. [DOI] [PubMed] [Google Scholar]
- 40.Elmadağ M, Güzel Y, Acar M A, Uzer G, Arazi M. The Stoppa approach versus the ilioinguinal approach for anterior acetabular fractures: a case control study assessing blood loss complications and function outcomes. Orthop Traumatol Surg Res. 2014;100(06):675–680. doi: 10.1016/j.otsr.2014.05.020. [DOI] [PubMed] [Google Scholar]
- 41.Isaacson M J, Taylor B C, French B G, Poka A. Treatment of acetabulum fractures through the modified Stoppa approach: strategies and outcomes. Clin Orthop Relat Res. 2014;472(11):3345–3352. doi: 10.1007/s11999-014-3460-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hammad A S, El-Khadrawe T A. Accuracy of reduction and early clinical outcome in acetabular fractures treated by the standard ilio-inguinal versus the Stoppa/iliac approaches. Injury. 2015;46(02):320–326. doi: 10.1016/j.injury.2014.10.053. [DOI] [PubMed] [Google Scholar]
- 43.Dailey S K, Archdeacon M T. Open reduction and internal fixation of acetabulum fractures: does timing of surgery affect blood loss and OR time? J Orthop Trauma. 2014;28(09):497–501. doi: 10.1097/BOT.0000000000000153. [DOI] [PubMed] [Google Scholar]
- 44.Matta J M. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78(11):1632–1645. [PubMed] [Google Scholar]
- 45.D'Aubigne R M, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36-A(03):451–475. [PubMed] [Google Scholar]
- 46.Merle D'Aubigné R. [Numerical classification of the function of the hip. 1970] Rev Chir Orthop Repar Appar Mot. 1990;76(06):371–374. [PubMed] [Google Scholar]
- 47.Matta J M, Anderson L M, Epstein H C, Hendricks P. Fractures of the acetabulum. A retrospective analysis. Clin Orthop Relat Res. 1986;(205):230–240. [PubMed] [Google Scholar]
- 48.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction Preliminary report. J Bone Joint Surg Am. 1964;46:1615–1646. [PubMed] [Google Scholar]