Abstract
Ewing sarcoma family tumors (ESFTs) of the kidney represents less than 1% of all renal tumors. A 45-year-old Japanese woman presented with right abdominal pain. Contrast-enhanced computed tomography showed a 12 × 8-cm right cystic renal mass. The mass was diagnosed as cystic renal cell carcinoma (RCC) and right partial nephrectomy was performed. Immunohistochemical studies showed that the tumor was positive for CD99 (membranous staining in tumoral cells), indicating ESFT. The patient is doing well without further therapy after 1 year of follow-up. To our knowledge, this is the first report of renal ESFT mimicking cystic RCC on diagnostic imaging.
Introduction
Ewing sarcoma family tumors (ESFTs), previously called primitive neuroectodermal tumor, Askin tumor, or Ewing sarcoma, harbor the chromosomal translocation t(11; 22)(q24; q12), which causes the chimeric fusion protein EWS/FLI-1. ESFTs occur most commonly in the bone and soft tissue in children and young adults. ESFTs of the kidney represent less than 1% of all renal tumors1). The imaging findings at the time of diagnosis of ESFT reveal a heterogeneous mass mainly composed of solid components with some hematoma and cystic components. It is difficult to distinguish ESFT from renal cell carcinoma (RCC) by imaging examination alone2). The median size of the tumor at diagnosis is 11.3 cm (range, 5.5–30 cm), and approximately 30% of patients have metastasis at diagnosis1). The treatment strategy is the same as that administered for Ewing sarcoma in the bone. Chemotherapy is effective, with an overall response rate of 66%1), and the median survival of patients with renal ESFT is approximately 2 years. We report a rare patient with ESFT who underwent partial nephrectomy for a large cystic tumor.
Case presentation
A 45-year-old Japanese woman presented with a complaint of episodic right abdominal pain. No remarkable findings were observed on physical examination. Transabdominal ultrasonography (US) showed a 12 × 8-cm cystic renal mass in the right kidney (Fig. 1A). Contrast-enhanced computed tomography (CECT) of the chest and abdomen showed contrast enhancement in the renal parenchyma and cyst wall, without metastasis to the lymph nodes or other organs (Fig. 1B). The mass was diagnosed as right cystic RCC, and the patient underwent robotic-assisted partial nephrectomy (RAPN) using a renal artery clamp. The renal parenchyma around the tumor was bluntly dissected. Hemostasis on the tumor bed was obtained using soft coagulation without renorrhaphy. The warm ischemic time was 18 min, and the estimated blood loss was 800 mL. The macroscopic specimen consisted of hematoma in the thickened cyst wall (Fig. 2A). Microscopic examination of the hematoxylin-eosin-stained sample showed uniform small round blue cells arranged in a rosette fashion (Fig. 2B). Immunohistochemistry (IHC) indicated that the tumor was positive for CD99 (Fig. 2C). Fluorescence in situ hybridization (FISH) analysis was positive for the EWSR1 gene in 90% of cells, which was compatible with a diagnosis of ESFT (Fig. 2D). The patient is alive without further treatment after 1 year of follow-up.
Fig. 1.
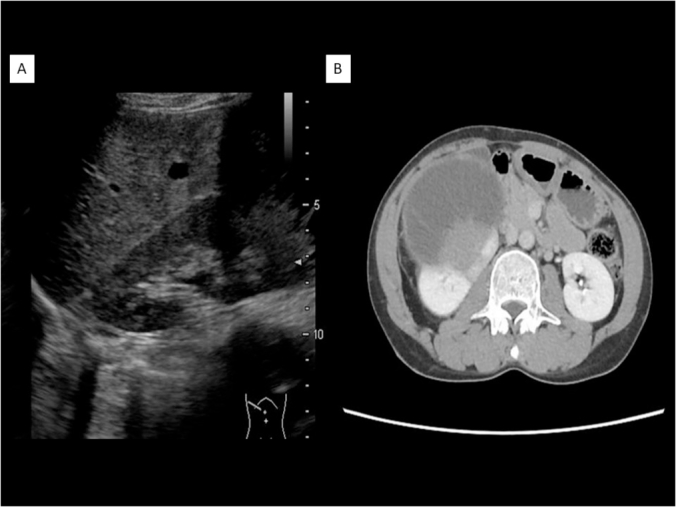
Results of preoperative imaging studies. (A) Transabdominal ultrasonography showed a cystic mass in the right kidney. (B) Contrast-enhanced computed tomography showed a 12 × 8-cm cystic right renal mass with enhanced cystic wall and solid portion.
Fig. 2.
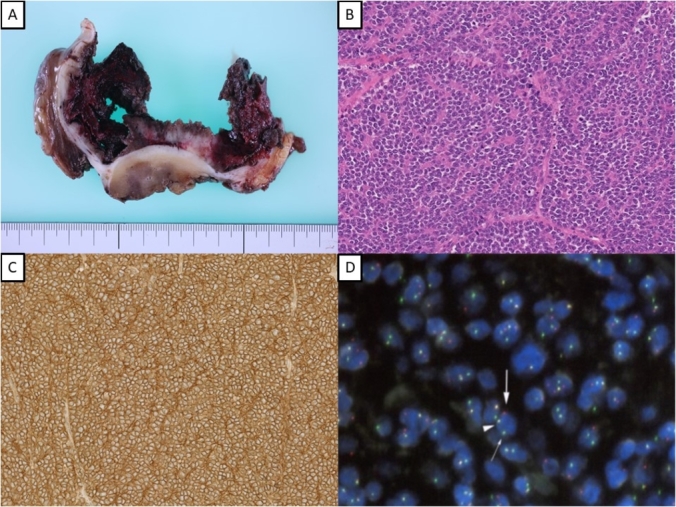
(A) The macroscopic specimen showed hematoma in the thickened cyst wall. (B) Microscopic examination of the hematoxylin-eosin-stained sample showed uniform small round blue cells arranged as a rosette fashion ( × 400). (C) Immunohistochemistry was positive for CD99 ( × 400). (D) Fluorescence in situ hybridization analysis was positive for the EWSR1 gene in 90% of cells.
Discussion
ESFT of the kidney is a relatively rare tumor. Since its first description in 1975, more than 120 cases have been published in the medical literature1). The differential diagnoses include RCC, Wilms tumor, neuroblastoma, malignant lymphoma, metastatic renal involvement from sarcoma elsewhere in the body, and renal involvement by a primary retroperitoneal sarcoma. ESFT is generally diagnosed by IHC and FISH analysis. The IHC pattern of renal ESFT is CD99 staining on the cell membrane3). ESFTs can be particularly difficult to diagnose by imaging alone, as no specific signs of ESFT in transabdominal US, CECT, or magnetic resonance imaging have been described. The imaging characteristics of most renal sarcomas are indistinguishable from those of RCC2). Generally, the imaging findings indicate a heterogeneous mass mainly composed of solid components with mixed hematoma and cystic components. To our knowledge, there are no other reports of renal ESFT mimicking cystic RCC on diagnostic imaging.
The 5-year survival rate of ESFT is only 20-30% in patients with metastasis. The most common metastatic sites are the lung (60%), liver (37%), abdominal lymph nodes (20%), and bone (16%)1). Patients are treated using the strategy for Ewing sarcoma in the bone, namely, a combination of surgery, radiation therapy, and chemotherapy, depending on the primary site and stage. The most commonly administered chemotherapy is vincristine-doxorubicin-cyclophosphamide, followed by etoposide-ifosfamide. Eighty-nine percent of patients with ESFT of the kidney undergo surgery for the primary tumor1). Among these patients, 95% undergo nephrectomy, and the remaining patients undergo open biopsy. Half of the patients receive neoadjuvant or adjuvant chemotherapy for the primary tumor1). Most patients undergo combined total resection and chemotherapy. Excessive chemotherapy should be avoided in patients with ESFT in the skin if complete resection of the tumor is possible4). Our patient underwent no further treatment because complete resection of the tumor was obtained by RAPN with negative surgical margins. As a result, the patient is alive without relapse for 1 year.
Conclusion
We report a case of a large cystic ESFT of the kidney that was completely resected by RAPN.
Conflicts of interest
We have no conflicts of interest with regard to this case report.
References
- 1.Risi E., Iacovelli R., Altavilla A. Clinical and pathological features of primary neuroectodermal tumor/Ewing sarcoma of the kidney. Urology. 2013;82:382–386. doi: 10.1016/j.urology.2013.04.015. [DOI] [PubMed] [Google Scholar]; Risi E, Iacovelli R, Altavilla A, et al. Clinical and pathological features of primary neuroectodermal tumor/Ewing sarcoma of the kidney. Urology. 82(2013), pp. 382-386. [DOI] [PubMed]
- 2.Almeida M.F., Patnana M., Korivi B.R. Ewing sarcoma of the kidney: a rare entity. Case Rep Radiol. 2014;2014:283902. doi: 10.1155/2014/283902. [DOI] [PMC free article] [PubMed] [Google Scholar]; Almeida MF, Patnana M, Korivi BR, et al. Ewing sarcoma of the kidney: a rare entity. Case Rep Radiol. 2014(2014), pp. 283902. [DOI] [PMC free article] [PubMed]
- 3.Celli R., Cai G. Ewing sarcoma/primitive neuroectodermal tumor of the kidney: a rare and lethal entity. Arch Pathol Lab Med. 2016;140:281–285. doi: 10.5858/arpa.2014-0367-RS. [DOI] [PubMed] [Google Scholar]; Celli R and Cai G. Ewing sarcoma/primitive neuroectodermal tumor of the kidney: a rare and lethal entity. Arch Pathol Lab Med. 140(2016), pp. 281-285. [DOI] [PubMed]
- 4.Omori M., Ueno M., Ogawa M. Primary cutaneous extraskeletal Ewing's sarcoma/PNET: possibility of better prognosis than deep ES/PNET. Eur J Dermatol. 2014;24:126–127. doi: 10.1684/ejd.2013.2247. [DOI] [PubMed] [Google Scholar]; Omori M, Ueno M, Ogawa M, et al. Primary cutaneous extraskeletal Ewing's sarcoma/PNET: possibility of better prognosis than deep ES/PNET. Eur J Dermatol. 24(2014), pp. 126-127. [DOI] [PubMed]


