Abstract
Background and Aims
Facial rejuvenation has become an increasingly patient-driven procedure with speedy but significant results and minimal downtime being the holy grail of both patient and practitioners. Fractional techniques with both laser and radiofrequency sources have attracted attention with some good results, but still with some downtime. Combination therapy could offer the best points of the separate techniques to give synergistic results with minimal downtime. The present pilot mini-study investigated the safety and efficacy of facial rejuvenation with a combination of microneedling fractional radiofrequency (MFR) and fractional minimally-invasive thulium laser (FTL) treatment.
Subjects and Methods
Four Korean females, ages from 53–63 yr (mean age 58.25), Fitzpatrick skin type Ⅲ-Ⅳ with mild to moderate photoaging-related sequelae participated in the study. On the first pass an MFR system was used with insulated microneedles to deliver a single pass of RF energy to a depth of 1.5 mm-1 mm in the dermis (7.5 W, 30 ms exposure). This was immediately followed by an FTL (5 W, 10 mJ) with 2–3 passes over the whole face, and a further 4–5 passes over the target wrinkles. This was repeated for 6 treatment sessions with 2-weekly intervals, and with a follow-up of 16 weeks after the final session. An analytical digital clinical imaging system captured gross and analytical images, and an independently-scored Physician Global Assessment (PGA) scale was used to assess efficacy in addition to patient satisfaction.
Results
Apparent smoothing of wrinkles and general improvement in skin condition was seen following the 3rd to 4th sessions. At the 16-week assessment very clear improvement was seen both with the naked eye and with specific analytical software from the imaging system. The total mean PGA score was 3.35 (out of 4), and all patients were extremely satisfied with the results. No adverse events were reported and pain was minimal.
Conclusions
The combination of MFR and FTL was safe and effective, and produced synergistic results in skin rejuvenation in the Asian skin type which were judged to be better than either system used on its own. Further larger population, split-face and controlled trials are warranted to confirm these optimistic results.
Keywords: High-intensity focused RF, thulium laser, fractional approach, combination fractional treatment, synergistic treatment
Introduction
Facial rejuvenation is now a very highly patient-driven procedure, with many patients requiring ‘more for less’, i.e., more efficacy with less downtime. In other words particularly those patients with only mild to moderate photoageing sequelae now look for ‘good gain with little pain’, rather than the accepted ‘no pain, no gain’ approach with even minimally invasive approaches which satisfied the requirements of the moderate to severely photodamaged patient.
The so-called ‘nonablative laser resurfacing’ phase for facial rejuvenation which appeared at the turn of the New Millennium attempted to give at least some of the benefits of full-face ablative CO2 and Er:YAG laser resurfacing, 1) but without the really heavy burden and prolonged downtime imposed by the severe sequelae of the fully ablative approach. 2, 3) The theory was that laser energy would create controlled coagulation in the dermis under a fairly aggressively chilled epidermis: unfortunately in practice the results were extremely disappointing, despite the reported very good dermal histology, and patient satisfaction was rather dismal. The major problem was that the chilling of the epidermis prevented any renovation and restructuring of that layer, 4) and it is the epidermis that patients see when they look in the mirror, not the dermis.
Fractional laser resurfacing for facial rejuvenation went through a non-ablative stage before ablative fractional resurfacing showed very good results, but still with some downtime which could last for several days. 5, 6) That was, however, orders of magnitude better than the fully ablative approach, and fractional laser rejuvenation has become very popular, especially for the rejuvenation of moderate to severe photoaged skin. More recently, two novel approaches to facial rejuvenation have attracted attention. The first was with a non-laser energy-based device, microneedling fractional radiofrequency (MFR), 5) using insulated microneedles which deliver the RF energy directly to the dermis with no electrothermal damage to the epidermis, since the needle shafts are insulated. Mild mechanical microneedling of the epidermis is also achieved which goes some way to encouraging rejuvenation of the epidermis as well. 6) There is downtime associated with MFR, but it was found to be less than with ablative fractional CO2 skin rejuvenation, and the efficacy and safety have been high. MFR is painful, however, and requires pretreatment with a topical anesthetic. Because of the downtime and the pain, MFR is particularly associated with treatment of moderate to severe skin conditions, The second novel approach has been the use of a fractional thulium fiber laser (FTL) at 1927 nm. 7) With water absorption more than the Er:glass laser at 1540–1550 nm, but less than the CO2 and Er:YAG lasers, FTL treatment could deliver intermediate, controlled subablative and minimally invasive tissue damage, with temporary disruption of both the stratum corneum and stratum spinosum and controlled coagulation of the superficial dermis to achieve rejuvenation both of the epidermis and dermis with minimal downtime. Anesthesia is required with more aggressive settings. With limited coagulation damage and short downtime, the FTL approach is particularly suited for correction of very mild to moderate skin conditions.
The present pilot study was designed based on the premise that the use of lower parameters of the MFR approach could limit pain and downtime but deliver controlled coagulation to the upper reticular layer of the dermis under a minimally damaged epidermis, followed immediately in the same session by controlled subablative alterations to the epidermal architecture with mild coagulation in the superficial dermis. The synergy between these two approaches, namely a ‘top-down’ (laser) approach and ‘bottom up (RF) approach whereby the range of tissue effects would cover from the epidermis down to the upper reticular dermis, might encourage renovation and rejuvenation of all these tissues through induction of the wound healing process and thus deliver a total result superior to either of these approaches used separately, but with minimal downtime. This might therefore satisfy the ‘Good Gain with Little Pain’ requirement of patients with only mild to moderately aged facial skin.
Subjects and Methods
Subjects
Four Korean females participated in the study, ages from 53–63 yr (mean age 58.25), Fitzpatrick skin type Ⅲ–Ⅳ with mild to moderate photoaging-related wrinkles, enlarged pores, rough skin and dyschromia. Having had the study protocol explained to them, including potential side effects, all four subjects gave written informed consent to participate in the pilot study, and for the use of their clinical photography. The study was carried out under the principles of the Declaration of Helsinki (2011).
Microneedling Fractional Radiofrequency (MFR) System
The system used was the INFINI® MFR system (Lutronic Corporation, Goyang, South Korea). This RF device has a handpiece equipped with single-use disposable tips containing a 1 cm2 matrix of 49 microneedles. The needles are insulated except for the 300 µm at the very tip, which acts as the RF electrode, and delivery and return needles are paired as a bipolar RF device. The depth of the needles in the dermis can be selected (0.5 mm −3.5 mm, 0.5 mm increments). Power level (1–20, 2.5–50 W) and exposure time (10 ms −1000 ms) can also be selected. Needle insertion and retraction is automatic and controlled by a footswitch or finger switch. This technique is also referred to as high-intensity focused radiofrequency (HiRF), as the RF energy is focused between the needle tips as elctrodes.
Fractional Thulium Laser (FTL)
The FTL device was the LaseMD® system (also from Lutronic Corporation). This is a thulium fiber-based system emitting laser energy at 1927 nm, and delivered via a fractionating handpiece. The microbeams (100 µm in diameter) can be delivered in a stamping or a dynamic mode. In dynamic mode, the laser is fired by a magnetic tracking system linked to two rollers in the handpiece tip: the faster the handpiece is moved across the tissue, the faster the laser is fired, and vice versa. It is therefore impossible to overlap microbeams during each pass. The system offers two treatment modes, a preset mode and an advanced mode with power adjustable from 1 to 5 W in 1 W increments, and beam energy adjustable from 1 to 20 mJ in 1 mJ increments.
Treatment Protocol
The subjects' faces were cleaned, and a topical anesthetic was applied (lidocaine cream, 9.6%) and left to incubate for at least 30 min under cling film occlusion. The occlusive film was removed and all traces of anesthetic cream were removed. The MFR treatment was indicated first over the whole face using a single pass with no overlap. Needle depth was from 1.0 to 1.5 mm to target the mid reticular -upper dermis, depending on the severity of the skin condition, intensity 3 (7.5 W) and an exposure time per shot of 30 ms: these were very conservative settings. In each MFR treatment the total shot count was 200 to 300.
In all subjects, the MFR treatment was immediately followed by the FTL treatment with 2–3 passes over the entire face, and a further 4–5 passes over the deeper wrinkles. Dynamic mode was selected with 5 W and 10 mJ as the laser parameters. The endpoint was mild to moderate diffuse erythema, with a feeling of heat in the skin. Skin cooling was performed with ice packs post treatment, and a simple moisturizing cream was applied. Patients could gently wash their face after treatment, but avoid scrubbing the skin for 48 hr. Use of a gentle moisturizer and a daily UVA/B sunscreen regimen was recommended, SPF > 30. Six treatment sessions were given at two-weekly intervals. The final assessment was 16 weeks after the last treatment session.
Assessments
Digital clinical photography was captured under standardized settings and lighting conditions using a single lens reflex (SLR) digital camera for full face and profile images (CANON 80D, Canon Camera, Tokyo, Japan), and the ANTERA-3D® system (Miravex, Dublin, Ireland) for macrophotography and capture of specific skin characteristics. The camera illuminates the skin with multiple wavelengths of LED light from different angles, and an onboard computer uses the reflected light to develop a 3-dimensional image of the skin which can then be manipulated via built-in filters to capture specific aspects of the skin, including wrinkles, redness and pigmentation, The macro-images in the present study were analyzed using the ANTERA3D wrinkle, roughness, pore, redness and pigmentation filters. All clinical photography was captured at baseline, before and after each treatment session, and at the 16-week assessment point.
The clinical photography was assessed at baseline and at the 16-week follow-up by two independent dermatologists to score improvement on a quintile Physician Global Assessment (PGA) scale: 0 points, 0–10% improvement; 1, 11–25%; 2, 26–50%; 3, 51–75%; and 4, 75–100%. The assessing clinicians reached a consensus following discussion where required. Patients were asked to grade their satisfaction with the treatment at the 16-week assessment as follows: totally dissatisfied (0% improvement or the condition deteriorated); a little satisfied (1–20% improvement); fairly satisfied (21–50%); satisfied (51%–75%); and highly satisfied (76%–100%).
Apart from the anticipated degree of erythema, the appearance of any adverse events, including but not restricted to unwanted pigmentary and textural changes, was noted during and after treatment, and during the 16-week followup. Patients were asked to rate their discomfort during the MFR and FLT procedures for each session using an 11-point visual analog scale (VAS) where zero was no pain and 10 was the worst possible pain.
Results
The four subjects completed all treatment sessions and the 16-week follow-up. Diffuse and even erythema post-treatment almost always lasted up to 12 hr before spontaneously evolving. No other adverse events were noted during or after treatment by the subjects or the investigator. Some degree of pain was noted during treatment, more so for the MFR than the FTL approach (Table 1). The scores for the former ranged from 2 to 4 (mean ± SD: 3.38 ± 0.61), and for the latter 0–2 (mean 0.71 ± 0.40). A trend towards a lower pain score was seen as treatment sessions progressed, possibly indicating an increasing degree of tolerance.
Table 1: Pain scores during microneedling fractional RF (MFR) and fractional thulium laser (FTL) treatment.
| Patient No | Session numbers | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1st | 2nd | 3rd | 4th | 5th | 6th | |||||||
| MFR | FTL | MFR | FTL | MFR | FTL | MFR | FTL | MFR | FTL | MFR | FTL | |
| 1 | 4 | 2 | 3 | 0 | 4 | 1 | 3 | 0 | 3 | 1 | 3 | 1 |
| 2 | 3 | 1 | 4 | 1 | 3 | 0 | 4 | 1 | 3 | 0 | 3 | 0 |
| 3 | 4 | 2 | 3 | 1 | 3 | 1 | 2 | 0 | 3 | 1 | 2 | 0 |
| 4 | 3 | 1 | 4 | 1 | 3 | 0 | 4 | 1 | 3 | 0 | 3 | 1 |
| Averages | 3.5 | 1.5 | 3.5 | 0.75 | 3.25 | 0.5 | 3.25 | 0.5 | 3 | 0.5 | 2.75 | 0.5 |
The mean PGA scores for improvement in dyschromia, skin roughness, enlarged pores and wrinkles at the 16-week assessment were, respectively, 4.0, 4.0, 2.5 and 3.0 (Table 2), giving an overall mean PGA of 3.35 out of the possible 4 and indicating a high degree of overall improvement in the facial skin condition. All four subjects subjectively rated the improvement in their skin condition at the 16-week assessment as highly satisfactory, and would be very happy to return for further treatments when necessary.
Table 2: Scores for Physician Global Assessment (PGA) of improvement from baseline to the 16-week assessment.
| Patient No | Item | |||
|---|---|---|---|---|
| Dyschromia | Skin roughness | Enlarged pores | Wrinkles | |
| 1 | 4 | 4 | 3 | 3 |
| 2 | 4 | 4 | 2 | 3 |
| 3 | 4 | 4 | 3 | 3 |
| 4 | 4 | 4 | 2 | 3 |
| Means | 4.0 | 4.0 | 2.5 | 3.0 |
| Total mean PGA: 3.35 | ||||
Clinical photography
In the use of the clinical photography for the PGA scoring, the assessors correctly identified in every case the ‘after’ image from the before and after images.
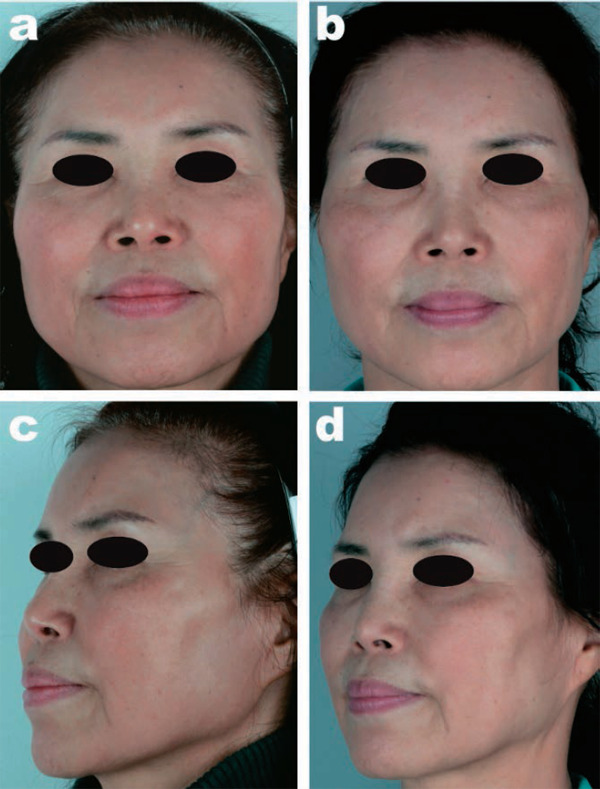
Figures 1 to 4 show the findings for the four subjects at baseline and at the 16-week follow-up, Cases 1 to 4 respectively. Figure 5 illustrates the nose of Case 1 at baseline (5a,c) and at 2 weeks after the 6th session (5b,d) in normal close-up mode and in the analytical mode of the camera system set to highlight pores/rough skin. Note the clear progress in the skin quality. Improvement in melanin dyschromia is shown in Figure 6a,b on the left cheek of Case 1, whereas improvement in atrophic areas on the right cheek at baseline and 16 weeks after the 6th session can be seen in 6 c,d. Clear amelioration of periorbital wrinkles and skin condition at 16 weeks after the final session compared with baseline in Case 2 is seen in Figure 7, while Figure 8 shows improvement in the overall smoothness of the skin condition on the right cheek of case 3 (baseline, Figure 8a,c), with smoothing seen at 16 weeks after the final treatment (Figure 8b,d). The ANTERA camera system can also highlight hemoglobin-related dyschromia, such as potential facial flushing or early stage rosacea, as seen at baseline in the right cheek of Case 4 in Figure 9a, c, with good improvement at the 16 week-assessment (Figure 9b,d).
Figure 1:
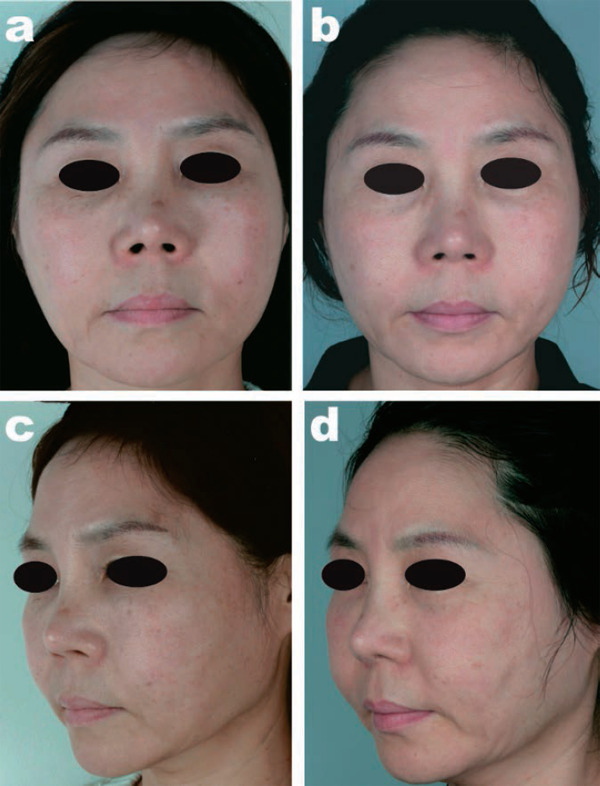
Case 1, a 56-year-old Korean female at baseline (a, full face; c three-quarter profile) and at the final assessment (b,d), 16 weeks after the final treatment session.
Figure 2:
Case 2, a 63-year-old Korean female at baseline (a, full face; c three-quarter profile) and at the final assessment (b,d), 16 weeks after the final treatment session.
Figure 3:

Case 3, a 61-year-old Korean female at baseline (a, full face; c three-quarter profile) and at the final assessment (b,d), 16 weeks after the final treatment session.
Figure 4:

Case 4, a 53-year-old Korean female at baseline (a, full face; c three-quarter profile) and at the final assessment (b,d), 16 weeks after the final treatment session.
Figure 5:
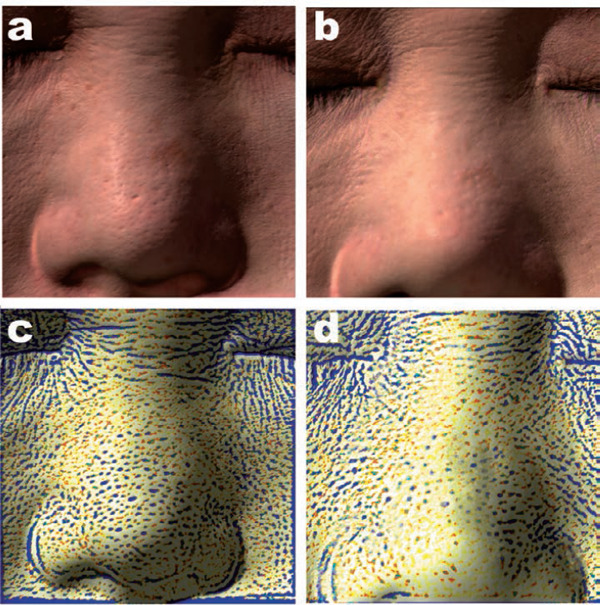
Improvement in pores / rough skin assessed with the ANTERA™ system in Case 1 at baseline and at the 16-week final assessment (a): Baseline with Macro 3D setting. (c): Baseline with Pores setting. (b & d): Baseline and final assessment in the Macro 3D and Pores settings, respectively. Clear improvements are recorded.
Figure 6:

Melanin and atrophic skin findings in Case 1 assessed with the ANTERA system at baseline (a: melanin, c: atrophic areas) and at the 16-week assessment (b & d). Particular improvent is noted in the filling out of the atrophic areas.
Figure 7:
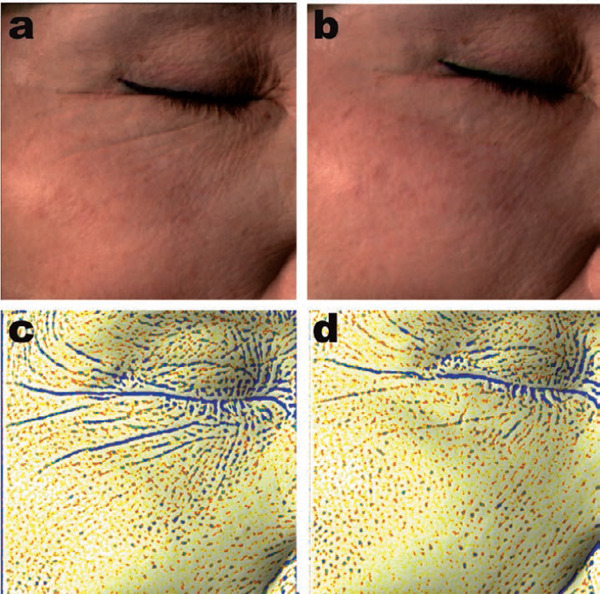
ANTERA 3D images showing improvement in Case 2 with the Macro 3D setting (a: baseline, b: 16-week assessment) and the Rough Skin setting (c, baseline: d, 16-week assessment).
Figure 8:
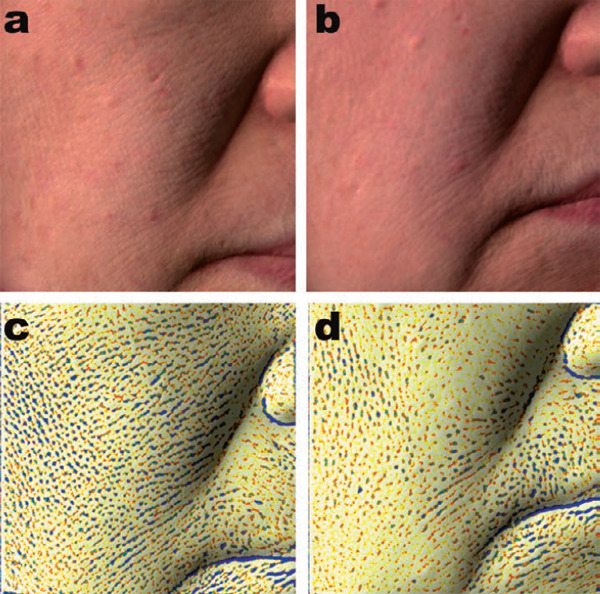
Smoothing out of rough skin can be seen compared with baseline following treatment in Case 3. (a): Baseline Macro 3D. (c): Baseline Rough Skin. (b & d) 16-week assessments.
Figure 9:
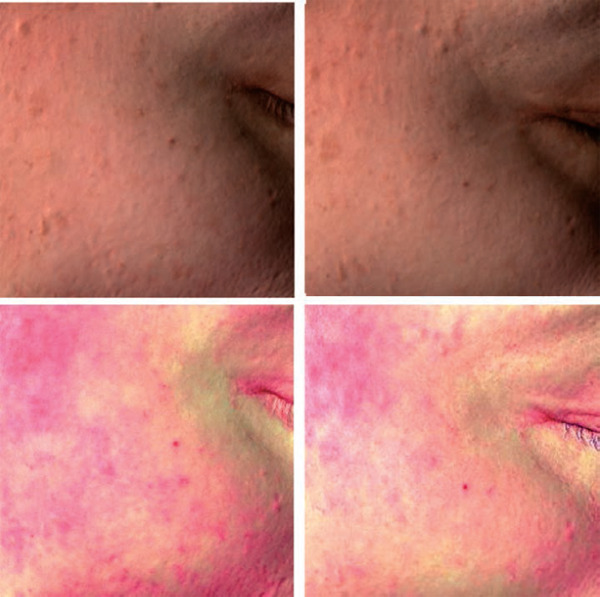
Improvement in potential flushing seen with the ANTERA Macro 3D and Hemoglobin settings respectively at baseline (a,c) and 16-week assessment (b,d)
Discussion
Rejuvenation of aging facial skin is one of the fastest-growing fields in aesthetic and cosmetic dermatological practice. The power of social media now means that this arena is fast becoming highly patient-driven, with specific protocols searched for, or even clinics identified with specific laser systems or energy-based devices which are rightly or wrongly seen as ‘the best’. Foremost among the goals of the patient looking for skin rejuvenation is the ability to get the best result possible, as quickly as possible and with as little downtime as possible. In the case of moderate to severely aged skin, this minimalistic approach becomes less realistic. For the woman, or man, with very mild to moderately-aged skin the ‘no pain, no gain’ maxim is unattractive and inappropriate, and they actively desire a ‘good gain with no (or little) pain’ approach.
Industry has cooperated with the patient requiring the minimally aggressive approach and systems have been developed which offer non- or subablative, minimally- or noninvasive approaches. The development of the fractionation principle was the first real practical step towards achieving these goals, to achieve limited damage in the treated area leaving large percentages of untreated skin to assist with the wound healing process and to limit the downtime. However, for the ablative fractional laser, such as the CO2 and to a lesser extent, the Er:YAG, even the limited damage can be associated with downtime which, though orders of magnitude better than the fully ablative approach, can still be as long as a week to 10 days in cases where aggressive parameters are required in the treatment of severely aged or compromised skin.
The fractional delivery of RF with insulated microneedles, MFR, took a large step towards offering laser-like efficacy with much less downtime than the fractional ablative laser, although pain was still an issue. Real efficacy could be offered with safety, and the results could be truly dramatic, for example, in correcting neck and jowl laxity. 5) The MFR protocol normally used requires 2 to 3 passes at decreasing needle depths in the dermis, with fairly aggressive power level and exposure time settings. Pain is definitely an issue, and downtime lasts 2–4 days. One of the main advantages of this approach is that the epidermis is spared because the needles are insulated, so all the electrothermal effect is limited to the area in the dermis around the needle tips. When thinking of the typical patient looking for the ‘good gain with no pian’ approach, the author surmised that a single MFR pass at a depth of 1–1.5 mm would deposit a controlled layer of coagulation in the upper and fine reticular dermis, sufficient to start the wound healing process, and would at the same time minimize the downtime associated with the more aggressive depth and energy settings (Figure 10). However, it would not be enough to improve the Grenz layer in the papillary dermis, and the mechanical microneedling might not be enough to stimulate regeneration of the epidermis, as seen in the intact condition of the epidermis and superficial dermis in Figure 10. That is where the addition of the fractional thulium laser came into the picture.
Figure 10:
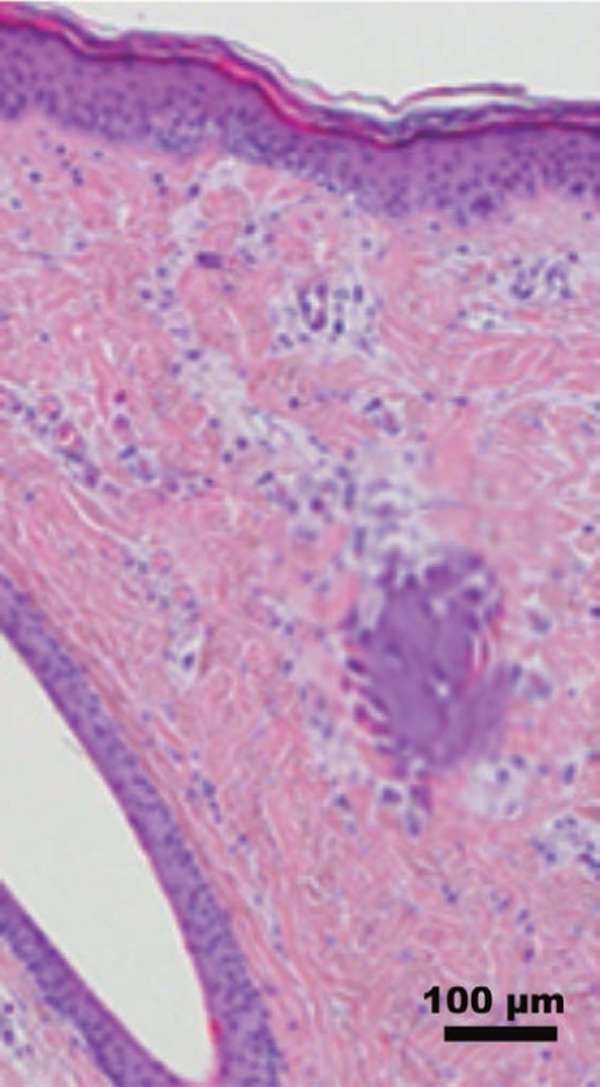
Typical histological pattern 1 hr following treatment with an MFR system at approximately the same parameters as used in the presents study (1 mm depth, level 5, 100 ms). Discrete coagulation in the fine reticular dermis is seen under an intact epidermis. (H&E, Facial skin, scale bar as shown. Courtesy Medicoscientific Affairs, Lutronic, South Korea)
With fractional delivery of the thulium fiber laser 1927 nm energy, coupled with water absorption at less than the Er:YAG and CO2 lasers, but more than the nonablative Er:glass lasers at 1450 nm-1550 nm, it became possible to deliver highly controlled subablative damage to the epidermis with very superficial coagulation in the papillary and superficial dermis. Figure 11 shows a hematoxylin and eosin stained specimen of a typical FTL impact, delivered with the system used in the present study. The stratum corneum is disrupted but not destroyed; the stratum spinosum is denatured, temporarily disabling the tight desmosomal cell-cell adhesion of the upward moving daughter keratinocytes; there is mild vacuolation at the dermoepidermal junction, and the stratum basale, though stimulated by the laser energy, is left intact; and there is am area of mild coagulation in the very superficial dermis. Figure 12 is a scanning electron photomicrograph of skin treated with the laser used in the present study, showing clearly that the plates of the stratum corneum are intact with fully subablative damage, The epidermal disruption returns very quickly to normal with restoration of the skin barrier function within 1 to 2 hours, but enough of a stimulus has been delivered to the epidermis to regenerate and improve its overall condition. Efficacy for skin rejuvenation and pigmented lesions including melasma has been reported with FTL treatment. 7) This FTL stimulation is also coupled with the stimulus exerted by the mechanical microneedling delivered to the epidermis and superficial dermis by the insulated microneedles during the MFR process. A recent review of microneedling concluded that it clearly offered both cosmetic and therapeutic benefits, and could help with pigmentation problems including melasma. 6) The importance of repeated sessions was stressed.
Figure 11:
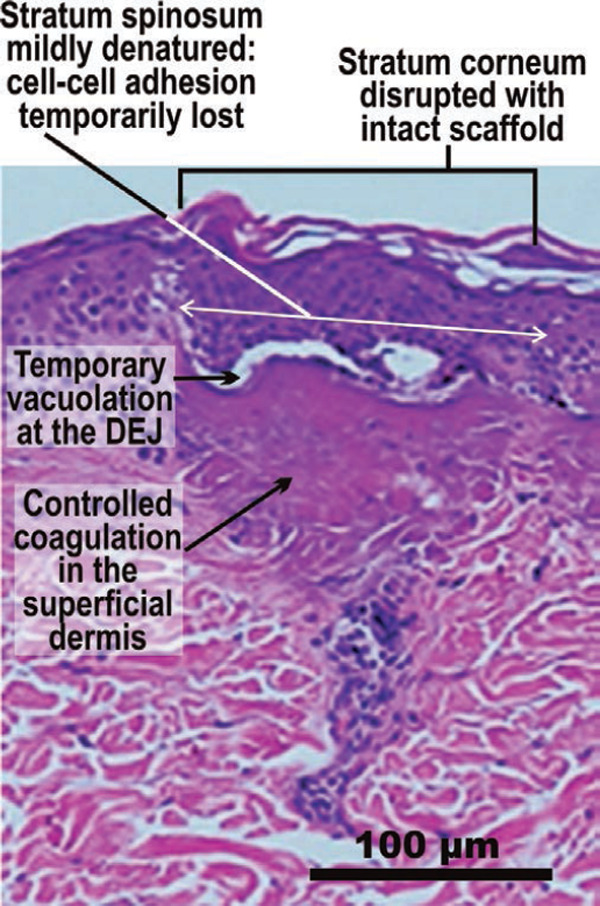
Hematoxylin and eosin stained specimen of a typical FTL impact at 5 W, 20 mJ. The changes in the epidermis and at the DEJ are mild and very transient, allowing for controlled side effects and shorter downtime, but with good restoration of the epidermis. The controlled dermal coagulation is sufficent to ensure induction of the wound healing process with collagenesis and elastinogenesis in the superficial dermis, followed by ECM remodelling. (Human skin, H&E stain, scale bar as shown. Courtesy BC Goo MD, South Korea)
Figure 12:
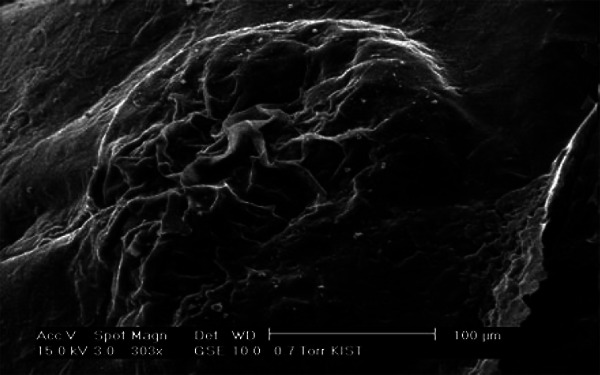
Scanning electron photomicrograph of an FTL microbeam impact in human skin, 5 W, 20 mJ. No ablation but mild disruption of the stratum corneum keratin scaffold is seen. (Scale bar as shown. Courtesy BC Goo MD, South Korea)
The author therefore added FTL to the MFR in the present study, delivered during the same session, immediately after the latter was completed. The parameters chosen delivered the maximum power (5 W) with the energy set to one-half of the maximum 20 mJ available (10 mJ) to limit the volume of damage, especially in the epidermis, and hence the downtime. The higher the energy setting, the longer the exposure time required to achieve it, and the longer the exposure time for a given output power, the greater is the damage volume. The author hypothesized that the combination of the upper dermal damage associated with the MFR treatment would ‘marry’ with the much more superficial damage from the FTL, and double stimulus of the epidermis by the mechanical microneedling followed by the subablative FTL energy would work on the epidermis. However, the level of damage in the epidermis should not be enough to trigger inflammation at the DEJ, which would certainly lead to the risk of PIH in the Korean skin type Ⅲ-Ⅳ. The good results achieved safely certainly bore out the author's hypothesis, and the end result offered a synergistic tissue response which gave greater efficacy than the sum of results of the two components had they been used individually.
The present study has limitations. The small patient population is obviously the main one, but this was a pilot study. No histology was taken immediately after treatment to quantify the damage delivered by the two approaches, separately and in combination: this needs to be added to any future study. The study would be enhanced by a split face component, perhaps with MFR or fractional CO2 laser used alone on one side at the usual parameters for rejuvenation of milder skin damage, and the combination used on the contralateral side to show at the very least its noninferiority with less pain and shorter downtime to the more aggressive approach with more pain and more downtime.
Conclusions
The present pilot study in a short case series used a combination of microneedle fractional RF followed immediately by fractional thulium laser over 6 treatment sessions, both used at less-aggressive parameters than usual when used alone, for facial rejuvenation of mild to moderately damaged skin in Korean patients. This combination approach gave high efficacy and safety with a short downtime, and high satisfaction for the patients at a 16-week followup. The degree of efficacy achieved indicated the possible synergistic results of this combination approach. Further larger and controlled studies are required to validate the optimistic results achieved in the present study.
Conflict of Interest
The author declares no conflict of interest regarding either of the systems used in the present study, and confirms that he received no incentive, financial or otherwise, from the manufacturer of these systems.
References
- 1: Trelles MA, García-Solana L, Calderhead RG. Skin Resurfacing Improved with a New Dual Wavelength Er:YAG / CO2 Laser System: A Comparative Study. J Clin Laser Med Surg, 1999; 17: 99-104. [DOI] [PubMed] [Google Scholar]
- 2: Menaker GM, Wrone DA, Williams RM, Moy RL: Treatment of facial Rhytides with a nonablative laser: a clinical and histological study. Dermatol Surg, 1999; 25: 440-444. [DOI] [PubMed] [Google Scholar]
- 3: Trelles MA, Allones I, Luna R: Facial rejuvenation with a nonablative 1320 nm Nd:YAG laser: a preliminary clinical and histologic evaluation. Dermatol Surg, 2001; 27: 111-116. [DOI] [PubMed] [Google Scholar]
- 4: Goldberg DJ: Non-ablative subsurface remodeling: clinical and histological evaluation of a 1320 nm Nd:YAG laser. J Cutan Las Ther, 1999; 1: 153-157. [DOI] [PubMed] [Google Scholar]
- 5: Clementoni MT, Munavalli GS: Fractional high intensity focused radiofrequency in the treatment of mild to Moderate laxity of the lower face and neck: A pilot study. Lasers Surg Med, 2016; 48: 461-470. [DOI] [PubMed] [Google Scholar]
- 6: Iriarte C, Awosika O, Rengifo-Pardo M, Ehrlich A: Review of applications of microneedling in dermatology. Clin Cosmet Investig Dermatol, 2017; 10: 289-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7: Lee HM, Haw S, Kim JK, Chang SE, Lee MW: Split-face study using a 1,927-nm thulium fiber fractional laser to treat photoaging and melasma in Asian skin. Dermatol Surg, 2013; 39: 879-888. [DOI] [PubMed] [Google Scholar]


