Abstract
BACKGROUND:
Cleft lip and palate CLP is a frequent congenital malformation that manifests in several varieties including unilateral or bilateral anomalies due to either genetic or acquired causes. Alveolar cleft graft ACG remains controversial as regard timing, grafting materials and surgical techniques. The primary goal of alveolar cleft grafting in ACG patients is to provide an intact bony ridge at the cleft site to allow maxillary continuity for teeth eruption, proper orthodontic treatment for dental arch alignment, oronasal fistula closure and providing alar support for nasal symmetry.
AIM:
This study aims to compare different grafting techniques to treat the alveolar cleft defect.
METHODS:
This study included 24 cases divided into three groups of patients: Group A was treated with autogenous iliac crest bone; Group B was treated with nano calcium hydroxyapatite with collagen membrane and Group C was treated with tissue engineering method using bone marrow stem cells extract and PRF membrane.
RESULTS:
According to clinical and radiographic examination measuring bone density in the CT preoperatively compared to six months postoperatively. Group C with bone marrow stem cells extract showed superior results among all followed by group B, while group A with autogenous iliac crest showed resorption in some cases and gave the least values, in addition to its drawbacks as regard donor site affection with pain & scar formation.
CONCLUSION:
Bone substitutes as Nano calcium hydroxyapatite and bone marrow stem cells extract showed to be reliable methods for bone grafting than autogenous iliac crest.
Keywords: Alveolar cleft, Hydroxyapatite, Stem cells, Iliac crest
Introduction
The alveolar cleft is a bony defect present in 75 % of CLP patients. Repair of the alveolar cleft is mandatory for both function and esthetics especially in syndromic patients with genetic malformations. Although secondary ACG is commonly accepted for these patients, controversy remains regarding the surgical technique and type of grafting material used [1], [2], [3]. A primary alveolar cleft repair usually takes place at an early age of life. Secondary alveolar bone grafting for patients with a cleft involving maxillary alveolus was first advocated by Boyne and Sands in 1972 [4]. The grafting procedures are usually taken around the age of 9-12 years by dental development, most notably at the cleft side of permanent canine as stated by Bergland et al., 1986 [5], [6]. Bone grafting can be performed using either autogenous bone or allogenic bone substitutes. Autogenous bone graft harvested from the iliac crest or rib graft with bone morphogenic proteins BMP has shown success rates. It supports the tooth in the alveolar arch and establish nasal bone morphology and ensures the stability of orthodontic treatment [7]. There are several benefits of bone grafting in patients with alveolar clefts, 1: to obtain arch continuity, which is a universal goal in cleft management. 2: to maximise bone support for dentition. 3: to stabilise the maxillary segments after orthodontic treatment, 4: to eliminate the oronasal fistulae. 5: to provide alar cartilage support 6: to establish ideal alveolar morphology and 7: to provide available bone with attached soft tissue for future implant placement in cases where there is residual dental space. In order to achieve these objectives, sufficient height and volume of bone must be provided [8], [9]. The concerns associated with an iliac crest or rib harvesting have focused primarily on the possible effects on growth, gait disturbances, hematoma, and donor site morbidity. Most of these complications can be overcome with a careful surgical technique and using allograft materials [10]. With the advent of new biomaterials, which may include or consist of allogenic bone source such as collagen membranes, hydroxyapatite crystals, tricalcium phosphate powder that has been increased consideration for their placement in the repair of alveolar clefts as well as other dental applications [11], [12]. Recently the technique for tissue engineering using bone marrow stem cells BMSC, mesenchymal stem cells MSC extract seeded on a scaffold as polylactic acid PLA, collagen, fibrin, tri calcium phosphate, calcium carbonate used for ACG [13]. BMSC & MSC are self renew cells isolated from the non hematopoietic compartment of bone marrow that can be induced to differentiate into other cells as osteoblasts, chondroblasts and fibroblasts [14]. Growth factors obtained from platelet rich plasma PRP by Chokroun in 2006 aids in tissue healing and accelerates recovery. PRP seems to enhance bone formation in alveolar clefts mixed with graft materials with less rate of postoperative complications. Its autologous, easy to prepare with a low cost that can be used as a source of growth factors [15], [16]. Orthodontic treatment has a major role in dental preparations preoperatively including maxillary expansion and teeth alignment allowing relief of crowding resulting from arch collapse and hypodontia it also creates space needed for the eruption of missing teeth as well as exposure of impacted teeth resulting from the cleft deformity. Cone beam CT is a low dose and effective method of radiological evaluation of the amount of bone defect at cleft side preoperatively measuring height and faciolingual depth. It measures bone density formed postoperatively to evaluate bone quality & quantity compared to the normal side [17], [18].
This study aims to compare different grafting techniques to treat the alveolar cleft defect.
Methods
This study included twenty-four patients with unilateral alveolar clefts who were randomly selected from Orodental Genetics clinic at National Research Center and Oral Surgery clinic at Faculty of Oral & Dental Medicine Al Azhar University. The sample was divided into 3 groups with different grafting techniques each containing 8 patients.
Group A: Included 8 patients who were treated with autogenous bone graft harvested from the iliac crest.
Group B: included 8 patients who were treated with GBR graft of nano calcium hydroxylapatite and collagen membrane.
Group C: included 8 patients who were treated with tissue engineering of bone marrow stem cells extract with the addition of PRP growth factors.
All patients were informed about all the details of the surgery & signed consent. Ethical approval of the scientific committee at the National Research Center was obtained. Preoperative patients preparation included clinical photographs intraorally as well as extra orally. Also digital radiographs including panoramic xrays and multi slice CT measuring the size of the defect. Medical history was recorded excluding any systemic diseases. Blood investigations were made prior to each surgery including hemoglobin level, bleeding profile (bleeding time, clotting time & prothrombin time). Kidney functions (Urea & Creatinine), liver functions (SGOT & SGPT), blood sugar, ECG electrocardiogram and chest examination for each patient.
Surgical procedures: Under GA with full aseptic conditions. A full mucoperiosteal flap was reflected from first premolar region to the central incisor. Separation of oral and nasal layers and closure of fistula was done.
Group A: Superior anterior iliac spine approach incision at the pelvis with trocar bone particles harvesting minimal invasive rather than traditional chisels and osteotome method. Bone crushed and placed into the cleft site Figure 1.
Figure 1.

Iliac crest technique (left); Bone marrow stem cells trocar (right)
Group B: 2 gm of hydroxyapatite powder was placed on the collagen membrane and placed into the defect site Figure 2.
Figure 2.
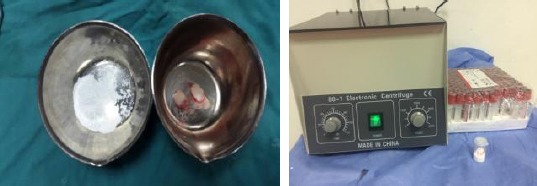
Nano calcium & collagen (left); PRP centrifuge (right)
Group C: Stem cells extracted from bone marrow aspirated from iliac crest using a biopsy needle. PRP obtained by citrated 10 cc syringe after being centrifuged for 15 minutes with 2500 rpm speed to separate the plasma portion rich with growth factors and mixed with bone marrow cells aspirate and packed into cleft site Figure 3.
Figure 3.

Alveolar cleft defect (left); Alveolar cleft grafting (right)
Following the surgery, all patients were prescribed proper antibiotics, analgesics and anti-inflammatory with oral hygiene instructions and soft food diet. Postoperative clinical evaluation (Figure 4) and radiographic evaluation after 6 months with panoramic x rays (Figure 5) and measuring bone density at graft site from CT and comparing it to the normal side (Figure 6). All data were subjected to statistical analysis.
Figure 4.

Preoperative cleft site (left); Postoperative cleft site (right)
Figure 5.

Preoperative panorama (left); Postoperative panorama (right)
Figure 6.
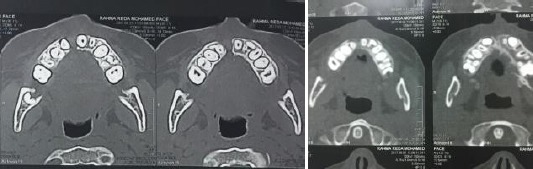
Preoperative CT (left); Postoperative CT (right)
Statistical methodology
All test data was converted and manipulated by using the SPSS software program version 20.0. Data were analysed, mean and standard deviation, range and median were calculated as regarding the three groups (Autogenous graft of iliac crest, Graft with Nano calcium hydroxyapatite and collagen membrane and Graft with bone marrow stem cells extract) in normal and grafted sides and the mean difference between normal and grafted side. Comparisons between normal and grafted results using paired t-test were made as well as a comparison between subjects undergone different methods of grafting using the t-test. P value was established to determine the statistically significant difference between the two groups. The difference between the two groups was considered statistically significant when p < 0.05, and considered highly statistically significant when p < 0.01.
Results
This study included twenty-four patients suffering from unilateral cleft and needed alveolar cleft grafting. Group A patients were grafted by autogenous bone harvested from the iliac crest. Group B patients were grafted by nano calcium hydroxyapatite particles and collagen membrane. Group C patients were grafted by bone marrow mesenchymal stem cells extract with platelet-rich plasma PRP membrane as a scaffold. Group C showed superior results with Mean ± SD 242.4 ± 47.8 with statistically highly significant P value < 0.001** followed by group B with Mean ± SD 144.6 ± 51.6 with statistically highly significant P value < 0.00 ** then group A with Mean ± SD 92.5 ± 35.8 and statistically significant P value 0.033* Table 1. Methods of the evaluation were clinically Figure (7 and 8) and radiographically preoperatively and six months postoperatively Figure (9 and 10) using panoramic x-ray and CT Figure (11 and 12).
Table 1.
Comparison among 24 cases undergone different methods of grafting according to the mean difference of bone densities of grafted side and normal side
| Group A | Group B | Group C | P | |
|---|---|---|---|---|
| Mean ± SD | 92.5 ± 35.8 | 144.6 ± 51.6 | 242.4 ± 47.8 | < 0.001** |
| Range (min-max) | 46-158 | 79-245 | 148-299 | |
| Median | 91.5 | 132 | 251.5 | |
| P value | 0.033l* | < 0.001** | < 0.001** |
p value between group A&B #between B&C between A&C;
statistically significant difference p < 0.05;
statistically highly significant difference p< 0.01.
Bone density was measured in the normal noncleft side and compared to the grafted cleft side in Housefield unit HU. Group C grafted side mean ± SD 618 ± 60.2 compared to normal side mean ± SD 375.6 ± 67.9 with P-value statistically highly significant < 0.001 **. Group B grafted side Mean ± SD 539.9 ± 84.5 compared to normal side with mean ± SD 395.3 ± 65.9 with P-value statistically significant < 0.001* And Group A grafted side mean ± SD 461.0 ± 66.3 compared to normal side mean ± SD 368.5 ± 68.3 with P-value highly significant < 0.001* Table 2. Accordingly, the use of bone substitute materials proved to be a reliable method rather than doner site affecting iliac with scar and pain as well as patient’s gait problems in case of autogenous bone. All grafted patients procedures went uneventful. However, group A showed some bone resorption later on while groups B & C showed bone regeneration due to osteoinductive properties of the graft material used.
Table 2.
Comparison between bone density in the normal side and grafted side in 24 cases
| Grafted area Mean ± SD | Normal side Mean ± SD | P | |
|---|---|---|---|
| Autogenous graft of iliac crets bone | 461.0 ± 66.3 | 368.5 ± 68.3 | < 0.001* |
| Nano Ca hydroxy apatite& collagen membrane | 539.9 ± 84.5 | 395.3 ± 65.9 | < 0.001* |
| Bone marrow stem cells extract with PRF | 618.0 ± 60.2 | 375.6 ± 67.9 | < 0.001** |
Statistically highly significant difference p < 0.01.
Group A: Autogenous graft of iliac crest bone.
Group B: Graft with Nano calcium hydroxylapatite and collagen membrane.
Group C: Graft with bone marrow stem cells extract and PRF.
Discussion
Cleft lip and palate is a congenital problem that happens for 1:700 child at birth according to UK studies. The alveolar cleft is a bony defect present in 75 % of CLP patients [1]. Repair of the alveolar cleft is mandatory for both function and esthetics. A primary alveolar cleft repair usually takes place at an early age of life. Secondary alveolar bone grafting for patients with a cleft involving maxillary alveolus was first advocated by Boyne and Sands in 1972 [4]. Secondary Alveolar bone grafting between the ages of 9-11 years is a routine procedure for children with cleft involving the alveolus [19]. The main advantages can be summarised as follows: stabilisation of the maxillary arch, allowing eruption of the canine and sometimes the lateral incisor, providing bony support for adjacent teeth, oroantral fistula closure and raising the alar base [20]. Von Eisenberg in 1901 & Lexer in 1908 was the first to use autogenous bone graft in the maxillary alveolar cleft. Iliac crest donor site seems to be the most preferred by surgeons however there are possible complications from the iliac crest as excessive blood loss, haematoma, delayed wound healing, pain lasting for two weeks to two months, and painful scars under belts or clothing and hypoesthesia or anaesthesia as observed by patients in the first group A. Radiographic evaluation showed that after 6 months of follow up bone volume loss in some cases. According to Masashi et al., [21] who compared the use of autogenous bone grafting versus using hydroxyl appetite bone combined with collagen membrane in 15 patients and observed that the there was no difference in radiographic results as regard the bone volume formed postoperatively while after 6 months postoperatively he concluded that the group grafted with iliac crest resulted in bone resorption while the group grafted with hydroxylapatite particles resulted in bone formation with no doner site complications with matching results to our current research in the second group B patients. The present study also concluded that using nano hydroxyl apatite on collagen sponge in alveolar cleft grafting was more successful and the same finding occurred with Al Ahmady HH et al., [22] who studied the merits of nano calcium hydroxyapatite with 90% success rate over the autologous iliac crest bone grafting with 70 % success rate in 20 patients divided into two groups during a period of 12 months follow up radiographically. The third group C in this study that was treated with bone marrow mesenchymal stem cells along with PRF membrane showed promising outcome according to its osteoinductive and osteoconductive properties in addition to overcoming the draw backs of standard autogenous method of bone grafting. Bajestan MN et al., [23] also proved that stem cell therapy with bone marrow derived cells can promote regeneration of bone in 18 cleft and trauma patients. He showed that the ability of stem cells to treat large alveolar cleft defects is safe. Our findings in the present study showed the best outcome in group C patients who were treated with tissue engineering technology combined with PRF method [1] as Choukran [15] who stated all the merits of the platelet-derived growth factors.
In conclusion, bone substitutes as Nano calcium hydroxyapatite and bone marrow stem cells extract showed to be reliable methods for bone grafting than autogenous iliac crest.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Seifeldin S. Is alveolar cleft reconstruction still controversial?(Review of literature) Saudi Dental J. 2016;28(1) doi: 10.1016/j.sdentj.2015.01.006. https://doi.org/10.1016/j.sdentj.2015.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xiao WL, Zhang DZ, Chen XJ, Xue LF. Osteogenesis effect of guided bone regeneration combined with alveolar cleft grafting, assessement of cone beam computed tomography. Int J Oral Maxillofac Surg. 2016;45(6):683. doi: 10.1016/j.ijom.2016.01.013. https://doi.org/10.1016/j.ijom.2016.01.013 PMid:26876144. [DOI] [PubMed] [Google Scholar]
- 3.Cho-Lee GY, García-Díez EM, Nunes RA, Martí-Pagès C, Sieira-Gil R, Rivera-Baró A. Review of secondary alveolar cleft repair. Annals of maxillofacial surgery. 2013;3(1):46. doi: 10.4103/2231-0746.110083. https://doi.org/10.4103/2231-0746.110083 PMid:23662259 PMCid:PMC3645611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boyne PJ. Secondary bone grafting of residual alveolar and palatal clefts. J Oral Surg. 1972;30:87–92. [PubMed] [Google Scholar]
- 5.Bergland O, Semb G, Abyholm FE. Elimination of the residual alveolar cleft by secondary bone grafting and subsequent orthodontic treatment. The Cleft palate journal. 1986;23(3):175–205. [PubMed] [Google Scholar]
- 6.Francis CS, Mobin SS, Lypka MA, Rommer E, Yen S, Urata MM, Hammoudeh JA. rhBMP-2 with a demineralized bone matrix scaffold versus autologous iliac crest bone graft for alveolar cleft reconstruction. Plastic and reconstructive surgery. 2013;131(5):1107. doi: 10.1097/PRS.0b013e3182865dfb. https://doi.org/10.1097/PRS.0b013e3182865dfb PMid:23385986. [DOI] [PubMed] [Google Scholar]
- 7.Wahaj A, Hafeez K, Zafar MS. Role of bone graft materials for cleft lip and palate patients:A systematic review. The Saudi Journal for Dental Research. 2016;7(1):57–63. https://doi.org/10.1016/j.sjdr.2015.02.001. [Google Scholar]
- 8.Horswell BB, Henderson JM. Secondary osteoplasty of the alveolar cleft defect1. Journal of oral and maxillofacial surgery. 2003;61(9):1082. doi: 10.1016/s0278-2391(03)00322-7. https://doi.org/10.1016/S0278-2391(03)00322-7. [DOI] [PubMed] [Google Scholar]
- 9.Le BT, Woo I. Alveolar cleft repair in adults using guided bone regeneration with mineralized allograft for dental implant site development:a report of 2 cases. Journal of Oral and Maxillofacial Surgery. 2009;67(8):1716. doi: 10.1016/j.joms.2009.04.012. https://doi.org/10.1016/j.joms.2009.04.012 PMid:19615587. [DOI] [PubMed] [Google Scholar]
- 10.Sadove AM, Nelson CL, Eppley BL, Nguyen B. An evaluation of calvarial and iliac donor sites in alveolar cleft grafting. Cleft Palate Journal. 1990;27(3):225–9. doi: 10.1597/1545-1569(1990)027<0225:aeocai>2.3.co;2. https://doi.org/10.1597/1545-1569_1990_027_0225_aeocai_2.3.co_2 PMid:2372971. [DOI] [PubMed] [Google Scholar]
- 11.Kraut RA. The use of allogeneic bone for alveolar cleft grafting. Oral surgery, oral medicine, oral pathology. 1987;64(3):278–82. doi: 10.1016/0030-4220(87)90003-x. https://doi.org/10.1016/0030-4220(87)90003-X. [DOI] [PubMed] [Google Scholar]
- 12.Peamkaroonrath C, Godfrey K, Chatrchaiwiwatana S. New clinical method for alveolar bone graft evaluation in cleft patients:a pilot study. The Cleft Palate-Craniofacial Journal. 2011;48(3):286–92. doi: 10.1597/09-222. https://doi.org/10.1597/09-222 PMid:20572777. [DOI] [PubMed] [Google Scholar]
- 13.Fujihara K, Kotaki M, Ramakrishna S. Guided bone regeneration membrane made of polycaprolactone/calcium carbonate composite nano-fibers. Biomaterials. 2005;26(19):4139–47. doi: 10.1016/j.biomaterials.2004.09.014. https://doi.org/10.1016/j.biomaterials.2004.09.014 PMid:15664641. [DOI] [PubMed] [Google Scholar]
- 14.Ratajczak MZ, Zuba-Surma EK, Wysoczynski M, Ratajczak J, Kucia M. Very small embryonic-like stem cells:characterization, developmental origin, and biological significance. Experimental hematology. 2008;36(6):742–51. doi: 10.1016/j.exphem.2008.03.010. https://doi.org/10.1016/j.exphem.2008.03.010 PMid:18474305 PMCid:PMC2430762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Choukroun J, Diss A, Simonpieri A, Girard M-O, Dohan SL. Platelet rich fibrin a second generation of platelet concentrate. Oral Surg Med Oral Path Oral Radiol Endo. 2006;101:56. doi: 10.1016/j.tripleo.2005.07.011. https://doi.org/10.1016/j.tripleo.2005.07.011 PMid:16504852. [DOI] [PubMed] [Google Scholar]
- 16.Hernández P, Cortina L, Artaza H, Pol N, Lam RM, Dorticós E, Macías C, Hernández C, Del Valle L, Blanco A, Martínez A. Autologous bone-marrow mononuclear cell implantation in patients with severe lower limb ischaemia:a comparison of using blood cell separator and Ficoll density gradient centrifugation. Atherosclerosis. 2007;194(2):e52–6. doi: 10.1016/j.atherosclerosis.2006.08.025. https://doi.org/10.1016/j.atherosclerosis.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 17.Ehrenfest M. In search of consensus terminology in the field of platelet concentrates for surgical use:Platelet rich Plasma PRP, platelet rich fibrin PRF. 2015;13:1131. doi: 10.2174/138920112800624328. https://doi.org/10.2174/138920112800624328. [DOI] [PubMed] [Google Scholar]
- 18.Zhou WN, Xu Jiang HB, Du YF. Accurate evaluation of Cone beam CT to volumetrically asses alveolar cleft patients. 2015;26:535. doi: 10.1097/SCS.0000000000002034. https://doi.org/10.1097/SCS.0000000000002034. [DOI] [PubMed] [Google Scholar]
- 19.Gillgras TJ, MacDonald JP, Mossey PA, Welbury RR. The impact of alveolar bone grafting on cleft lip and palate:a literature review. South European journal of orthodontics and dentofacial research. 2014;1(1):19–22. https://doi.org/10.15538/sejodr-2014-21992. [Google Scholar]
- 20.Jan Lilja. Alveolar Bone grafting. Indian Journal of Plastic Surgery. 2014;42 https://doi.org/10.4103/0970-0358.57200. [Google Scholar]
- 21.Masaahi T, Teru S, Yoshaiki S, Kazuo K. Assessement of bioabsorbable hydroxyapatite for secondary bone grafting in unilateral alveolar cleft. J Plastic Reconstructive & Aesthetic Surgery. 2015;69:4. doi: 10.1016/j.bjps.2015.10.040. https://doi.org/10.1016/j.bjps.2015.10.040. [DOI] [PubMed] [Google Scholar]
- 22.Al-Ahmady HH, Elazeem AF, Ahmed NE, Shawkat WM, Elmasry M, Abdelrahman MA, Abderazik MA. Combining autologous bone marrow mononuclear cells seeded on collagen sponge with Nano Hydroxyapatite, and platelet-rich fibrin:Reporting a novel strategy for alveolar cleft bone regeneration. Journal of Cranio-Maxillofacial Surgery. 2018;46(9):1593–600. doi: 10.1016/j.jcms.2018.05.049. https://doi.org/10.1016/j.jcms.2018.05.049 PMid:30196860. [DOI] [PubMed] [Google Scholar]
- 23.Bajestan MN, Rajan A, Edwards SP, Aronovich S, Cevidanes LH, Polymeri A, Travan S, Kaigler D. Stem cell therapy for reconstruction of alveolar cleft and trauma defects in adults:A randomized controlled, clinical trial. J Clin Implant Dent Relat Res. 2017;19(5):793–801. doi: 10.1111/cid.12506. https://doi.org/10.1111/cid.12506 PMid:28656723. [DOI] [PubMed] [Google Scholar]


