Fig. 1.
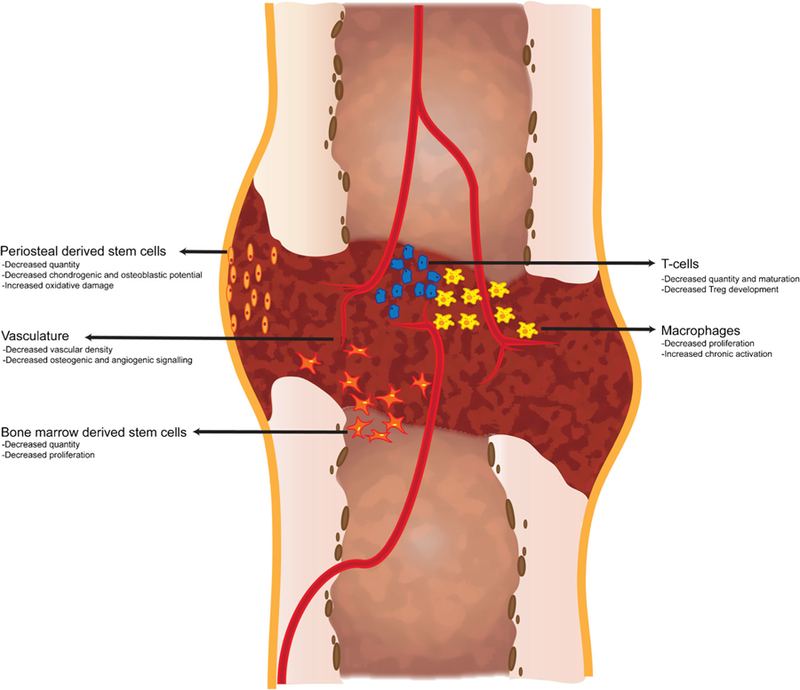
The effect of age on the cellular contribution to fracture healing. Stem cells and immune cells involved in fracture healing demonstrate age-related changes that may negatively affect fracture healing. Osteochondral stem cells arise from the periosteum and bone marrow and demonstrate decreased quantity, increased oxidative damage, and decreased osteoblastic and chondrogenic differentiation potential with age. T-cells contribute to fracture healing and production and maturation of T cells is negatively affected by age-related changes to the bone marrow hematopoietic compartment and to the thymus. Macrophages are important regulators of inflammation during fracture healing. Aged macrophages demonstrate decreased proliferation and increased activation that may contribute to the poorer healing outcomes associated with aged macrophages compared to young. Finally, adequate vascularization is required for successful fracture healing. Aged animals demonstrate decreased vascular density within the callus which is associated with decreased levels of key angiogenic factors required for healing
