CASE PRESENTATION
A 10-year-old boy was referred to the Ophthalmology service at a paediatric tertiary care centre with a 2-month history of tearing and squinting. In the week prior to assessment, he had experienced what seemed to be a drastic decrease in his visual acuity, suddenly ‘needing to feel his way along the walls’ at home.
Past medical history was significant for autism spectrum disorder (ASD). There was no history of ophthalmologic concerns, and the patient had not had an eye exam previously. Review of systems identified a restricted diet, consisting of chocolate bars, buttered popcorn, french fries, fresh buns, bottled water and soft drinks. The patient’s limited food repertoire had been longstanding and, by parents’ report, had preceded the ASD diagnosis. There had not been regular intake of fruits or vegetables in years. There was no history of oral ulcers, skin rash, diarrhea, steatorrhea or weight loss. The patient was not taking any regular medications, vitamins, herbal products or supplements.
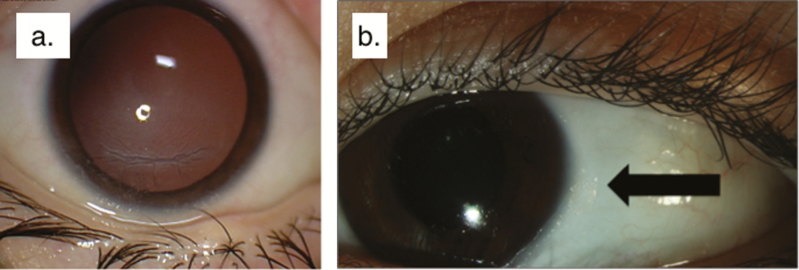
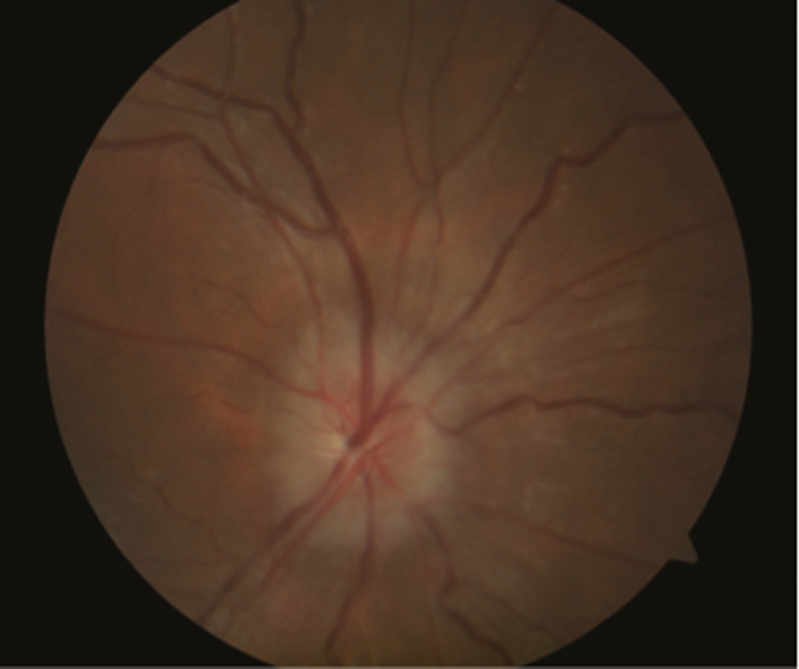
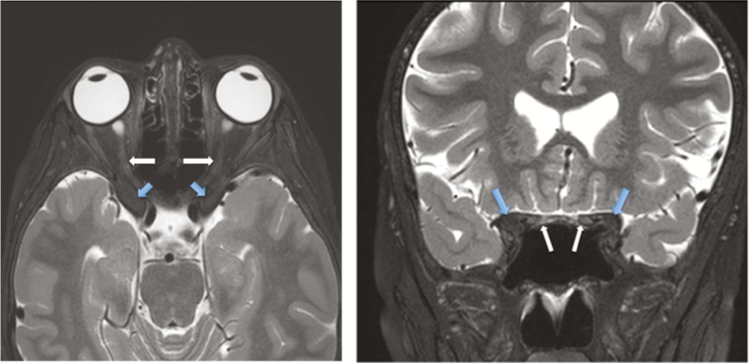
Weight was at the 25th percentile for age. Height could not be obtained because the patient was unable to cooperate. General physical exam was unremarkable. On ophthalmologic exam, the patient had only ‘hand motion’ visual acuity and was not able to fix-and-follow toys, faces or lights. Numerous abnormalities were identified: (1) corneal and conjunctival keratinization with punctate epithelial erosions; (2) dull and irregular light reflex, also indicating abnormal keratinization; (3) scaly, dry patch with foamy appearance and (4) mild optic nerve edema in both eyes (Figures 1 and 2). An MRI head was performed, showing bilateral papilledema with possible narrowing of the optic canals (Figure 3).
Figure 1.
Pretreatment images of the patient’s eyes. (a) Corneal and conjunctival keratinization with punctate epithelial erosions. Dull and irregular light reflex, also indicating abnormal keratinization. (b) Scaly, dry patch with foamy appearance on temporal aspect of the conjunctiva (Bitot’s spot), as indicated by black arrow.
Figure 2.
Pretreatment funduscopic image. Mild optic nerve edema, as demonstrated here, was observed in both eyes.
Figure 3.
T2-weighted MRI images. Bony hypertrophy of the anterior clinoid (blue arrow) encroaching upon the optic nerves (white arrow) in the optic canal.
DIAGNOSIS: VITAMIN A DEFICIENCY AND XEROPHTHALMIA: DISCUSSION
Worldwide, vitamin A deficiency represents an important public health problem, affecting approximately 250 million children (1,2). In developed countries, vitamin A deficiency is uncommon; however, rare cases have been described secondary to malabsorption syndromes (3), cholestatic liver disease (4) and certain types of bariatric surgery (5). Cases of vitamin A deficiency in children with ASD have also been reported in developed countries including Japan, Ireland, the USA and Australia (6–10). Here, we report the unusual case of a Canadian child with ASD and restricted diet who presented with vision loss secondary to vitamin A deficiency and xerophthalmia.
Vitamin A deficiency was presumed based on ophthalmologic exam findings and was confirmed when vitamin A level was ultimately found to be low (<0.1 μmol/L; reference 0.9 to 1.7). Also low were zinc (8.6 μmol/L; reference 11.6 to 15.4), vitamin D (34 nmol/L; reference 70 to 250), total protein (63 g/L; reference 68 to 85) and albumin (35 g/L; reference 37 to 50). Hemoglobin, vitamin B12, vitamin E, ferritin, calcium and red cell folate were all within normal limits. Empiric treatment was initiated prior to the patient’s vitamin A level being available as per World Health Organization (WHO) guidelines (11); two doses of vitamin A were immediately given on consecutive days and a third dose was given on day 14. Each dose was 200,000 international units. Sedation was required for insertion of a nasogastric tube and administration of the first dose of vitamin A. The patient was able to take the second and third doses mixed with water.
Reassessment 1 week after the first doses of vitamin A showed a significant improvement in visual acuity (20/40 in the right eye and 20/30 in the left eye). Xerosis and punctate epithelial erosions of the cornea had also improved. Approximately 3 months after treatment, the patient continued on daily vitamin A supplementation. Corneal changes had resolved and there was complete resolution of previous disc edema with residual optic nerve atrophy. The patient was able to fix and follow with both eyes. Visual acuity was at least 20/500, but could not be further assessed because of the patient’s inability to cooperate with examination.
Because vitamin A is required to maintain the epithelium of the ocular surface, deficiency results in replacement of the normal epithelium by an abnormal, keratinized epithelium (12). Xerophthalmia—the spectrum of ophthalmologic disease caused by vitamin A deficiency—is characterized by dryness of the cornea and conjunctiva. It typically manifests as areas of desquamated epithelium and keratinization of the conjunctiva (Bitot’s spots), progressing to corneal xerosis (keratinization of the cornea). In severe vitamin A deficiency, the stroma of the cornea can soften and liquefy (keratomalacia). As vitamin A has a role in photoreception at the retina, vitamin A deficiency is known to also cause night blindness and retinopathy.
Vitamin A deficiency has systemic effects on hematopoiesis (leading to anemia), immune function (via effects on humoral and cell-mediated immunity) and bone growth (via postulated effects on osteoblast activity (13)). Vitamin A deficiency causing bony overgrowth has been reported in animal studies (13, 14) but has only been described in one previous case report (6). We propose that vitamin A deficiency led to optic canal narrowing in our patient, accounting for the initial optic disc swelling and subsequent optic nerve atrophy.
The WHO has published protocols for treatment of xerophthalmia, in which three age-specific doses of vitamin A are given (11). The oral route is preferred to the intramuscular route, except in the case of severe malabsorption (11). Practically, however, the oral administration of vitamin A may be difficult because of the restricted intake that initially led to vitamin A deficiency, as was the case in our patient. Because the advanced stages may be irreversible, xerophthalmia should be treated as a medical emergency and treatment initiated promptly (11). Delayed recognition of nutritional deficiencies may lead to worse outcomes, emphasizing the importance of vigilance in this context.
CLINICAL PEARLS
Vitamin A deficiency and xerophthalmia are relatively rare in developed countries but may be seen in certain medical conditions and in the context of restricted diet
Because advanced xerophthalmia may be irreversible, vitamin A deficiency impacting vision is a nutritional and medical emergency that should be treated immediately as per WHO guidelines
For patients at risk of micronutrient deficiencies, such as children with ASD and restricted diet, health care providers should (1) employ appropriate anticipatory guidance and preventive strategies, and (2) maintain a low threshold for referral and assessment if concerning signs and symptoms develop
Funding source: The work on which this manuscript is based did not receive funding from any agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest: None of the authors has a conflict of interest to declare. None of the authors has a financial relationship relevant to this article to disclose.
ACKNOWLEDGEMENTS
The authors would like to thank Drs. Nasrin Tehrani and Asim Ali (Ophthalmology, The Hospital for Sick Children) for their assistance with ophthalmologic photographs and their interpretation. The authors are also indebted to Dr. Manohar Shroff and Dr. Pradeep Krishnan (Diagnostic Imaging, The Hospital for Sick Children) for their invaluable assistance with MRI images.
References
- 1. World Health Organization. Global prevalence of vitamin A deficiency. MDIS Working Paper #2. Geneva, Switzerland: World Health Organization, 1995. [Google Scholar]
- 2. Underwood BA, Arthur P. The contribution of vitamin a to public health. Faseb J 1996;10(9):1040–8. [PubMed] [Google Scholar]
- 3. Chiu M, Dillon A, Watson S. Vitamin a deficiency and xerophthalmia in children of a developed country. J Paediatr Child Health 2016;52(7):699–703. [DOI] [PubMed] [Google Scholar]
- 4. Feranchak AP, Gralla J, King R, et al. Comparison of indices of vitamin a status in children with chronic liver disease. Hepatology 2005;42(4):782–92. [DOI] [PubMed] [Google Scholar]
- 5. Surapaneni KR, Koreishi A, Phelps PO. Bitot’s spots in gastric bypass patient. Ophthalmology 2016;123(3):521. [DOI] [PubMed] [Google Scholar]
- 6. Chiu M, Watson S. Xerophthalmia and vitamin A deficiency in an autistic child with a restricted diet. BMJ Case Rep 2015;2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tanoue K, Matsui K, Takamasu T. Fried-potato diet causes vitamin a deficiency in an autistic child. JPEN J Parenter Enteral Nutr 2012;36(6):753–5. [DOI] [PubMed] [Google Scholar]
- 8. Duignan E, Kenna P, Watson R, Fitzsimon S, Brosnahan D. Ophthalmic manifestations of vitamin a and d deficiency in two autistic teenagers: Case reports and a review of the literature. Case Rep Ophthalmol 2015;6(1):24–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McAbee GN, Prieto DM, Kirby J, Santilli AM, Setty R. Permanent visual loss due to dietary vitamin a deficiency in an autistic adolescent. J Child Neurol 2009;24(10):1288–9. [DOI] [PubMed] [Google Scholar]
- 10. Steinemann TL, Christiansen SP. Vitamin a deficiency and xerophthalmia in an autistic child. Arch Ophthalmol 1998;116(3):392–3. [DOI] [PubMed] [Google Scholar]
- 11. WHO/UNICEF/IVACG Task Force., World Health Organization., UNICEF., International Vitamin A Consultative Group. Vitamin A supplements: A guide to their use in the treatment and prevention of vitamin A deficiency and xerophthalmia. Geneva: World Health Organization; WHO Publication Center, 1988:24. [Google Scholar]
- 12. Sommer A. Xerophthalmia and vitamin a status. Prog Retin Eye Res 1998;17(1):9–31. [DOI] [PubMed] [Google Scholar]
- 13. Hayes KC, Nielsen SW, Eaton HD. Pathogenesis of the optic nerve lesion in vitamin a-deficient calves. Arch Ophthalmol 1968;80(6):777–87. [DOI] [PubMed] [Google Scholar]
- 14. Gallina AM, Helmboldt CF, Frier HI, Nielsen SW, Eaton HD. Bone growth in the hypovitaminotic a calf. J Nutr 1970;100(1):129–41. [DOI] [PubMed] [Google Scholar]