Abstract
Context:
Workforce surveillance efforts have long been called for in public health: the Public Health Workforce Interests and Needs Survey (PH WINS) answers that call.
Objective:
To characterize the state of the governmental public health workforce among State Health Agency-Central Office (SHA-CO) staff across the United States.
Design:
The SHA leadership were contacted and invited to have their agency participate in PH WINS 2017 as a census-based fielding. Participating agencies provided staff lists, and staff were then directly invited by e-mail to participate in a Web-based survey. Pearson and Rao-Scott χ2 analyses are employed in descriptive analyses. Balanced repeated replication weights account for design and nonresponse.
Setting and Participants:
SHA-CO staff.
Main Outcome Measures:
The PH WINS focuses on 4 primary domains: perceptions of workplace environment and job satisfaction, training needs, national trends, and demographics. In addition, measures of intent to leave and employee burnout are analyzed.
Results:
The state governmental public health workforce is primarily female (72%), non-Hispanic white (64%), and 46 years of age or older (59%). Nearly one-third (31%) of the workforce is older than 55 years, with 9% aged 30 years or younger. Overall, 74% of respondents indicated that they had at least a bachelor's degree, and 19% indicated having a public health degree of some kind. Seventy-nine percent of the respondents indicated that they were somewhat/very satisfied with their jobs. Approximately 47% of SHA-CO staff say that they are considering leaving or are planning to retire. With respect to training needs, the largest overall gaps for the state health agency workforce were observed in budget and financial management, systems and strategic thinking, and developing a vision for a healthy community.
Conclusions:
PH WINS represents the first nationally representative survey of governmental public health staff in the United States. It holds potential for wide usage from novel workforce research to identifying and helping address practice-based needs.
Keywords: governmental public health workforce, Public Health Workforce Interests and Needs Survey, workforce development
The governmental public health workforce is the cornerstone in the protection and promotion of population health in the United States.1 While the public health workforce plays a critical role in creating positive health outcomes, it is faced with pressing challenges, including funding losses, employee turnover, and emergent threats.2–5 These limit the public health system's ability to operate optimally.6,7 Workforce research was generally conducted at the organizational rather than the individual level until 2014.7,8 Realizing that the individuals working in the nation's state governmental public health agencies were rarely queried, the Association of State and Territorial Health Officials and the de Beaumont Foundation fielded the Public Health Workforce Interests and Needs Survey (PH WINS) in 2014. PH WINS changed the landscape for research and practice related to the State Health Agency (SHA) workforce.9,10 For the first time, the perspectives of more than 10 000 SHA workers, comprising a nationally representative sample of the workforce, were collected including their perceptions of issues related to employee engagement and workplace engagement, self-reported crosscutting training needs, and familiarity with emerging concepts in public health.11 Data supported anecdotes of underrepresentation of Hispanic/Latinos, men, and younger people in the workforce and unveiled that there was an intrinsically motivated staff, but a substantial proportion was considering leaving or retiring.11 By seeking out public health worker perspectives on key issues, PH WINS 2014 captured diverse opinions that provided the field, including agency leadership, with critical data for identifying and informing potential solutions to the workforce challenges faced by the public health system. Workforce development activities that were previously informed by the nonrepresentative or organizational-level research could now reflect the perspectives of the actual individual employees who are often the subject of the workforce development efforts.
Given the success and uptake of PH WINS 2014, as well as the changes in the public sector and in the field of public health specifically, the de Beaumont Foundation and the Association of State and Territorial Health Officials partnered again in 2017 to field an updated PH WINS. Revisions to the instrument and expanded SHA participation made it critical to update and better understand the current state of the workforce in SHAs. This article summarizes the key findings of PH WINS 2017 for SHA respondents and discusses the implications of these findings for policy and practice.
Methods
PH WINS is the largest survey of individual governmental health workers; originally fielded as a nationally representative sample of SHA-Central Office (SHA-CO) staff in 2014,11,12 PH WINS 2017 was expanded with additional state participation and the first nationally representative local health department frame. In its second fielding, PH WINS 2017 was sent to 102 305 staff nationwide, with 47 604 responding and 3764 who had left their position or were otherwise ineligible to participate.13 Potential respondents received an invitation to participate in the Web-based survey directly from Association of State and Territorial Health Officials via Qualtrics and received 5 reminders over 8 weeks on average (Qualtrics LLC, Provo, Utah). After accounting for staff who had left their position and undeliverable e-mails, there was a 47% response rate across all frames, state and local. This article utilizes data from SHA-CO respondents (the “SHA-CO frame”), which accounts for about 39% of all respondents (n = 17 136, 35% response rate). Forty-seven SHAs participated in this frame, which comprises staff who work in a SHA-CO or home office, as opposed to a local office of the SHA. In addition, for decentralized states, district and regional office staff employed by the SHA are included in this frame. In decentralized states, local health departments operate largely independently of the SHA, and so these staff are counted elsewhere in the PH WINS. Complex sampling design was accounted for through the implementation of balanced repeated replication weights.11,14
PH WINS has 4 major domains: workplace engagement, training needs assessment, emerging concepts in public health, and demographics. As in 2014, the workplace engagement domain draws heavily from previously used and validated surveys, especially the Federal Employee Viewpoint Survey.11 These questions relate to respondent perceptions and opinions about their workplace environment and job satisfaction as well as their intent to leave or retire. In addition, the Oldenburg Burnout Inventory (OLBI) was added in 2017 to better measure burnout risk in staff. Burnout is measured in relative terms; the OLBI does not have an absolute scale.15 The training needs section was restructured from 2014. Specifically, display logic was introduced, guiding respondents to a set of approximately 22 training needs, depending on their supervisory status. All respondents answered (1) whether they felt that the item was important in their day-to-day work and (2) how they characterized their ability to perform the item. This section's restructuring is described in detail elsewhere in this supplement.16 The emerging concepts section was modified slightly,14 and a new question was added to gauge respondent perception about the appropriate role of the SHA in other sectors related to health (eg, education, transportation). The demographics section remained unchanged, except in slight modifications to gender, occupation classification, and program area questions.14 Race/ethnicity were combined and analyzed as mutually exclusive categories.
Data were cleaned, managed, and analyzed in Stata 15.1 (StataCorp LLC, College Station, Texas). Balanced repeated replication weights were used to account for complex sample design. Descriptive statistics were performed, and Fisher exact and Tukey tests for multiple comparisons were employed, as appropriate. Data in this article draw only on the SHA-CO frame.
Results
Who is the state public health workforce?
The state governmental public health workforce is primarily women (72%, 95% confidence interval [CI], 72%-73%), non-Hispanic white (64%, 95% CI: 63%-65%), and 46 years of age or older (58%, 95% CI: 57%-59%) (Table 1). Nearly one-third (31%) of the workforce is older than 55 years, and only 9% are 30 years of age or younger. Staff worked in their current position for an average of 6.0 years (95% CI: 5.8%-6.1%), in their current agency for 9.9 years (95% CI: 9.6%-10.1%), and in public health practice for 13.0 years (95% CI: 12.8%-13.2%). Despite the older age of the workforce, approximately one-third of workers had been in public health practice for 5 years or less. Among those in management roles, 35% (95% CI: 31%-40%) had been in management for 5 years or less. Overall, 74% of respondents indicated that they had at least a bachelor's degree (95% CI: 73%-75%), and 19% indicated having a public health degree of some kind. Having a degree in public health varies considerably by state (state mean 20%, median 20%, interquartile range, 14%-36%). The majority of staff were in a nonsupervisory role (70% CI: 69%-70%), and more staff work in administrative, (44% CI: 43%-45%) as compared with clinical and lab (16%, 95% CI: 15%-16%) or public health sciences roles (37%, 95% CI: 36%-38%). The most commonly identified positions were public health program manager (8%, 95% CI: 7%-9%), epidemiologist (6%, 95% CI: 5%-7%), business/accounting (4%, 95% CI: 3%-5%), and nurse (3%, 95% CI: 2%-4%).
TABLE 1. Demographics of State Governmental SHA-CO Staff in 2017.
| Estimate (95% CI) | |
|---|---|
| Gender | |
| Male | 27% (26%-28%) |
| Female | 72% (72%-73%) |
| Nonbinary/other | 1% (0%-1%) |
| Race/ethnicity | |
| American Indian or Alaskan Native | 0% (0%-1%) |
| Asian | 7% (6%-7%) |
| Black or African American | 14% (13%-14%) |
| Hispanic or Latino | 9% (8%-9%) |
| Native Hawaiian or other Pacific Islander | 1% (0%-1%) |
| White | 64% (63%-65%) |
| Two or more races | 6% (6%-6%) |
| Age, y | |
| ≤20 | 0% (0%-0%) |
| 21-25 | 2% (2%-2%) |
| 26-30 | 7% (7%-8%) |
| 31-35 | 10% (9%-11%) |
| 36-40 | 12% (11%-13%) |
| 41-45 | 11% (10%-12%) |
| 46-50 | 14% (13%-14%) |
| 51-55 | 14% (13%-15%) |
| 56-60 | 16% (15%-16%) |
| 61-65 | 11% (10%-11%) |
| 66-70 | 3% (2%-3%) |
| 71-75 | 1% (0%-1%) |
| ≥76 | 0% (0%-0%) |
Abbreviation: CI, confidence interval.
Are SHA workers satisfied with their jobs?
Seventy-nine percent (95% CI: 79%-80%) of the respondents indicated that they were somewhat/very satisfied with their jobs (Figure 1), though this varied by supervisory status. Seventy-seven percent of nonsupervisors are somewhat/very satisfied with their jobs (95% CI: 77%-78%) compared with 81% of supervisors (95% CI: 80%-83%), 85% of managers (95% CI: 83%-87%), and 91% of executives (95% CI: 87%-94%).
FIGURE 1.
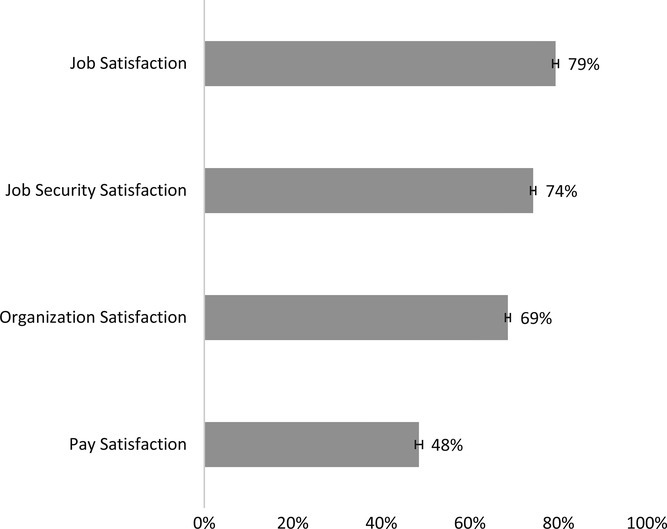
Levels of Satisfaction Among State Health Agency Central Office Staff in 2017
TABLE 2. Workforce Characteristics of State Governmental SHA-CO Staff in 2017.
| Estimate (95% CI) | |
|---|---|
| Supervisory status | |
| Nonsupervisor | 70% (69%-70%) |
| Supervisor | 16% (16%-17%) |
| Manager | 11% (11%-12%) |
| Executive | 3% (3%-3%) |
| Tenure in current position, y | |
| 0-5 | 66% (65%-67%) |
| 6-10 | 15% (15%-16%) |
| 11-15 | 9% (9%-10%) |
| 16-20 | 5% (4%-5%) |
| ≥21 | 5% (4%-5%) |
| Tenure in current agency, y | |
| 0-5 | 45% (44%-47%) |
| 6-10 | 18% (17%-18%) |
| 11-15 | 14% (13%-15%) |
| 16-20 | 10% (9%-11%) |
| ≥21 | 13% (13%-14%) |
| Tenure in public health practice, y | |
| 0-5 | 32% (31%-33%) |
| 6-10 | 19% (18%-19%) |
| 11-15 | 15% (14%-15%) |
| 16-20 | 13% (12%-13%) |
| ≥21 | 22% (22%-23%) |
| Tenure in management, y | |
| 0-5 | 35% (31%-40%) |
| 6-10 | 22% (19%-25%) |
| 11-15 | 17% (16%-19%) |
| 16-20 | 12% (10%-13%) |
| ≥21 | 14% (13%-15%) |
| Educational attainment | |
| No college degree | 14% (14%-15%) |
| Associates | 11% (11%-12%) |
| Bachelors | 35% (34%-36%) |
| Masters | 31% (31%-32%) |
| Doctoral | 8% (8%-8%) |
| Any degree in public health (any level) | 19% (18%-19%) |
| Job classification | |
| Administrative | 44% (43%-44%) |
| Clinical and lab | 16% (15%-16%) |
| Public health sciences | 37% (36%-38%) |
| Social sciences and all other | 4% (4%-5%) |
Abbreviation: CI, confidence interval.
Respondents reported less satisfaction with their organizations than with their jobs (Figure 1). Sixty-nine percent of respondents (95% CI: 68%-70%) reported satisfaction with their organizations, similar to the percentage of staff who agreed or strongly agreed that they recommend their organization as a good place to work (67%, 95%: CI 66%-68%). Pay satisfaction was modest at 48% somewhat/very satisfied (95% CI: 47%-49%). Pay satisfaction was lowest among nonsupervisors (46%, 95% CI: 45%-47%) but increased with ascending supervisory responsibilities. More than half of all supervisors (50%, 95% CI: 48%-51%) and managers (59%, 95% CI: 57%-62%) were satisfied with their pay as were three-quarters of executives (74%, 95% CI: 70%-77%).
How engaged are state public health agency workers?
Staff were asked to rate their perceptions of 17 components of their workplace environment that are associated with employee engagement (Table 3). With 2 exceptions, the majority of staff said that they agreed or strongly agreed with each statement, with the largest percentages of staff agreeing/strongly agreeing with the statements “the work I do is important” (93%, 95% CI: 93%-94%) and “I am determined to give my best effort at work every day” (94%, 95% CI: 93%-94%). The 2 exceptions with fewer than half of respondents expressing agreement/strong agreement were “creativity and innovation are rewarded” 43%(42%-44%) and “communication between senior leadership and employees is good”) 46%(45%-48%).
TABLE 3. Perceptions of Workplace Environment by Supervisory Status for State Health Agency Central Office Employees.
| Nonsupervisor | Supervisor | Manager | Executive | Total | |
|---|---|---|---|---|---|
| I know how my work relates to the agency's goals and priorities | 86% (85%-86%) | 88% (87%-89%) | 92% (90%-93%) | 96% (95%-98%) | 87% (87%-88%) |
| The work I do is important | 92% (92%-92%) | 96% (95%-96%) | 97% (96%-97%) | 96% (92%-98%) | 93% (93%-94%) |
| Creativity and innovation are rewarded | 41% (40%-42%) | 42% (41%-44%) | 49% (45%-53%) | 67% (57%-75%) | 43% (42%-44%) |
| Communication between senior leadership and employees is good in my organization | 46% (45%-47%) | 42% (40%-44%) | 49% (45%-53%) | 69% (65%-73%) | 46% (45%-48%) |
| Supervisors work well with employees of different backgrounds | 69% (68%-70%) | 75% (73%-76%) | 78% (76%-80%) | 85% (79%-89%) | 71% (71%-72%) |
| Supervisors in my work unit support employee development | 69% (68%-70%) | 75% (73%-76%) | 83% (80%-85%) | 85% (80%-90%) | 72% (71%-73%) |
| My training needs are assessed | 53% (53%-54%) | 48% (47%-50%) | 49% (46%-52%) | 50% (44%-55%) | 52% (51%-53%) |
| Employees have sufficient training to fully utilize technology needed for their work | 52% (51%-53%) | 52% (49%-55%) | 52% (49%-55%) | 50% (46%-54%) | 52% (51%-53%) |
| Employees learn from one another as they do their work | 80% (79%-81%) | 85% (84%-86%) | 89% (88%-90%) | 92% (89%-94%) | 82% (81%-83%) |
| My supervisor provides me with opportunities to demonstrate my leadership skills | 62% (62%-63%) | 76% (75%-78%) | 82% (81%-84%) | 88% (82%-92%) | 68% (67%-69%) |
| I have had opportunities to learn and grow in my position over the past year | 67% (66%-68%) | 74% (71%-76%) | 80% (75%-84%) | 89% (85%-91%) | 70% (70%-71%) |
| I feel completely involved in my work | 78% (77%-79%) | 83% (82%-85%) | 88% (85%-90%) | 93% (91%-95%) | 80% (79%-81%) |
| I am determined to give my best effort at work every day | 93% (92%-93%) | 94% (94%-95%) | 97% (96%-97%) | 98% (96%-99%) | 94% (93%-94%) |
| I am satisfied that I have the opportunities to apply my talents and expertise | 64% (63%-65%) | 71% (68%-73%) | 78% (74%-81%) | 87% (81%-91%) | 67% (67%-68%) |
| My supervisor and I have a good working relationship | 82% (81%-82%) | 84% (82%-86%) | 86% (84%-88%) | 88% (85%-91%) | 83% (82%-83%) |
| My supervisor treats me with respect | 83% (82%-84%) | 86% (83%-87%) | 86% (84%-88%) | 86% (80%-90%) | 84% (83%-84%) |
| I recommend my organization as a good place to work | 65% (64%-66%) | 67% (65%-69%) | 72% (70%-74%) | 84% (78%-89%) | 67% (66%-67%) |
Perceptions were consistent for some items regardless of supervisory status, such as “the work I do is important.” Noteworthy examples where differences were identified by ascending supervisory status include variations in strong agreement/agreement with “creativity and innovation are rewarded” (41% nonsupervisors, 42% supervisors, 49% managers, 67% executives); “I am satisfied that I have the opportunities to apply my talents and expertise” (64% nonsupervisors, 71% supervisors, 78% managers, and 87% executives); and “communication between senior leadership and employees is good in my organization” (46% nonsupervisors, 42% supervisors, 49% managers, and 69% executives).
How many workers intend to leave or retire?
More than one-third of respondents say that they are considering leaving their organization in the coming year for any reason, including retirement. About 5% were considering leaving to retire (95% CI: 5%-6%), 7% to take another job in governmental public health (95% CI: 6%-8%), and 22% to take another job not in governmental public health (95% CI: 21%-23%). Overall, 23% of staff say that they plan to retire by 2023 (95% CI: 22%-24%); the importance of this statistic is compounded by the fact that fully 18% of the workforce is 60 years of age or older (95% CI: 17%-19%), and 33% is 55 years of age or older (95% CI: 32%-34%).
Staff who indicated that they were considering leaving were asked for how long they had been considering leaving, and if they had taken any active steps to do so, such as applying or interviewing for a new position outside their organization. Twenty percent (95% CI: 18%-21%) said that they had been considering leaving for less than 3 months, 26% (95% CI: 23%-25%) said that they had been thinking about it for 3 to 6 months, and 57% said that they had been considering leaving for more than 6 months (95% CI: 55%-58%). Sixty-one percent of staff who indicated plans to leave (95% CI: 60%-63%) said that they had taken steps to do so.
Staff were also asked to identify reasons they were considering leaving. Pay was selected by 46% of respondents (95% CI: 45%-47%), followed by lack of opportunities for advancement (42%, 95% CI: 40%-44%), workplace environment (33%, 95% CI; 32%-35%), and job satisfaction (29%, 95% CI: 27%-30%). Higher proportions of staff with lower levels of supervisory responsibility reported pay, lack of opportunities for advancement, lack of acknowledgment/recognition, and lack of training compared with managers and executives (Table 4). Change in leadership was more commonly cited by managers than by those lower in the hierarchy, although this difference was not statistically significant (21% vs 15%, P = .052). Managers cited stress and work overload/burnout more than their colleagues with lower levels of supervisory responsibility (32% vs 22%, P < .001)(Figure 2).
TABLE 4. Reasons for Considering Leaving, by Supervisory Status Among State Health Agency Central Office Staff.
| Reason for Considering Leaving | Nonsupervisor | Supervisor | Manager | Executive | Total |
|---|---|---|---|---|---|
| Lack of acknowledgment/recognition | 26% (25%-28%) | 24% (21%-27%) | 20% (16%-25%) | 15% (7%-24%) | 25% (24%-27%) |
| Job satisfaction | 30% (28%-32%) | 27% (23%-31%) | 23% (20%-26%) | 15% (6%-24%) | 29% (27%-30%) |
| Lack of opportunities for advancement | 46% (44%-48%) | 36% (33%-39%) | 26% (21%-31%) | 22% (12%-31%) | 42% (40%-44%) |
| Lack of training | 16% (14%-17%) | 10% (8%-12%) | 10% (7%-13%) | 6% (2%-10%) | 14% (13%-15%) |
| Leadership changeover | 15% (14%-16%) | 17% (12%-21%) | 21% (15%-26%) | 23% (6%-39%) | 16% (15%-17%) |
| Other opportunities outside agency | 18% (17%-19%) | 18% (15%-20%) | 16% (11%-22%) | 14% (7%-22%) | 18% (17%-19%) |
| Pay | 49% (48%-50%) | 43% (38%-47%) | 36% (32%-40%) | 26% (19%-33%) | 46% (45%-47%) |
| Retirement | 3% (2%-3%) | 3% (2%-3%) | 5% (3%-7%) | 4% (0%-8%) | 3% (2%-3%) |
| Satisfaction with supervisor | 20% (19%-21%) | 21% (17%-24%) | 18% (14%-23%) | 22% (12%-31%) | 20% (19%-21%) |
| Stress | 21% (20%-22%) | 28% (22%-33%) | 31% (25%-37%) | 23% (14%-33%) | 23% (22%-24%) |
| Lack of flexibility (flex hours/telework) | 15% (14%-16%) | 14% (12%-17%) | 12% (9%-15%) | 10% (4%-16%) | 15% (13%-16%) |
| Weakening of benefits | 13% (11%-14%) | 13% (10%-17%) | 12% (9%-15%) | 4% (1%-7%) | 12% (12%-13%) |
| Work overload/burnout | 21% (20%-22%) | 27% (25%-30%) | 32% (28%-35%) | 24% (14%-34%) | 23% (22%-24%) |
| Workplace environment | 34% (32%-36%) | 35% (31%-39%) | 29% (25%-32%) | 23% (13%-33%) | 33% (32%-35%) |
| Lack of support | 27% (25%-29%) | 31% (28%-34%) | 25% (19%-31%) | 31% (15%-47%) | 27% (25%-30%) |
| Other | 19% (17%-20%) | 17% (14%-20%) | 11% (8%-13%) | 18% (10%-27%) | 17% (16%-19%) |
FIGURE 2.
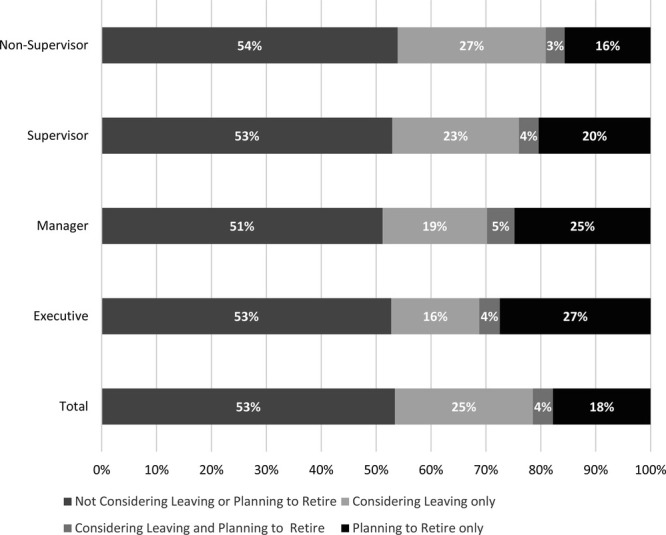
Intent to Leave by Supervisory Status Among State Health Agency Central Office Staffa
aMargin of error is ±0.5%. “Considering leaving” represents proportion of staff who say that they are considering leaving their organization in the next year for reasons other than retirement. “Planning to retire” represents the proportion of staff who say that they are planning to retire within 5 years.
Are SHA workers experiencing burnout?
The PH WINS 2017 added the Oldenburg Burnout Index, a validated measure of burnout, exhaustion, and disengagement (Figure 3). Because the OLBI is a relative measure, we examined which agencies were experiencing higher levels of burnout than the national average. Nationally, the OLBI shows a relatively normal distribution, with a slight skew toward lower burnout for SHA workers. Nine states have 55% or more of their staff rating above the national average on burnout. Four states have 45% or lower of their staff rating below the national average on burnout.
FIGURE 3.
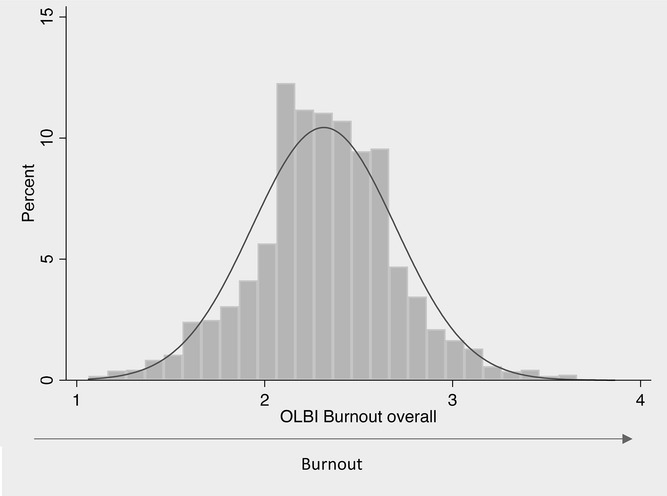
Distribution of Employee Burnout for State Health Agency Staff
Abbreviation: OLBI, Oldenburg Burnout Inventory.
What are the top training needs and gaps of SHA workers?
The PH WINS 2017 training needs assessment was organized into tiers based on supervisory status, with skills aligned with 8 focus areas (Table 5). A training need or skill gap was identified if a respondent indicated 2 things: (1) that it was somewhat or very important in their day-to-day work; and (2) that they were unable to perform the skill or considered themselves a beginner in the skill. Gaps at the focus area level are identified when any 1 skill item in that focus area has a skill gap.
TABLE 5. Training Needs: Percentage of State Health Agency Central Office Staff Who Identify as High Importance/Low Skill by Skill Domain.
| Nonsupervisors | Supervisors/Managers | Executives | Total | Significant Differencesa | |
|---|---|---|---|---|---|
| Effective communication | 19% (18-20%) | 14% (12-16%) | 5% (3-7%) | 17% (16%-18%) | 1, 2, 3 |
| Data for decision making | 25% (24-26%) | 22% (21-24%) | 23% (18-27%) | 24% (24%-25%) | 1 |
| Cultural competency | 30% (29-31%) | 36% (33-38%) | 34% (30-38%) | 32% (31%-33%) | 1 |
| Budget and financial management | 53% (51-55%) | 49% (48-50%) | 47% (41-53%) | 52% (50%-53%) | 1, 2 |
| Change management | 40% (39-42%) | 35% (33-38%) | 25% (19-32%) | 38% (38%-39%) | 1, 2, 3 |
| Systems and strategic thinking | 44% (42-45%) | 49% (48-51%) | 41% (36-47%) | 45% (45%-46%) | 1, 3 |
| Develop a vision for a healthy community | 40% (38-42%) | 44% (41-46%) | 36% (31-40%) | 41% (40%-42%) | 1, 3 |
| Cross-sectoral partnerships | 34% (33-36%) | 35% (33-38%) | 26% (21-30%) | 34% (33%-35%) | 2, 3 |
an ranges: 12 618 to 16 529; estimates shown as estimate (95% confidence interval); 1: Statistically significant difference at P < .05 between nonsupervisors and supervisors/mangers; 2: Statistically significant difference at P < .05 between nonsupervisors and executives; 3: Statistically significant difference at P < .05 between supervisors/managers and executives. High importance/low skill identified as those who have at least 1 skill per category identified both as somewhat/very important in their day-to-day work and as unable to perform/beginner in said skill.
The largest overall gaps for the SHA workforce were observed in budget and financial management, systems and strategic thinking, and developing a vision for a healthy community. Statistically significant differences were observed across almost every domain, especially between nonsupervisors and others. Among nonsupervisors, who constitute the vast majority of the workforce 70%(69%-70%), the biggest gaps were also in the budget and financial management focus area 53%(51%-55%) and systems and strategic thinking (44%, 95% CI: 42%-45%). The focus area with the fewest self-reported gaps among executives was effective communication (5%, 95% CI: 3%-7%).
Are SHA workers aware of emerging public health concepts?
Respondents were asked to reflect on 6 emerging public health concepts, first identifying whether they had heard of the concept and then identifying how much the concept impacts their day-to-day work (Table 6). The concepts that the largest percentage of the workforce was aware of were fostering a culture of quality improvement (82%, 95% CI: 81%-83%) and evidence-based public health practice (77%, 95% CI: 76%-79%). The concepts that the smallest percentage of the workforce was aware of were health in all policies (55%, 95% CI: 54%-56%) and multisectoral collaboration (66% 95% CI: 65%-66%).
TABLE 6. Perceptions of Emerging Concepts in Public Health Among the State Health Agency Central Office Workforcea.
| Heard of Trend | Trend Impacts Day-to-Day Work Fair Amount/Great Deal | |
|---|---|---|
| Cross-jurisdictional sharing of public health services | 69% (68%-70%) | 49% (48%-50%) |
| Fostering a culture of quality improvement | 82% (81%-83%) | 68% (67%-69%) |
| Public health and primary care integration | 73% (72%-74%) | 46% (44%-48%) |
| Evidence-based public health practice | 77% (76%-79%) | 60% (60%-61%) |
| Health in all policies | 55% (54%-56%) | 43% (42%-44%) |
| Multisectoral collaboration | 66% (65%-66%) | 57% (56%-58%) |
aEstimate shown as estimate (95% confidence interval). Heard of trend defined as all those who had said that they heard of trend “not much,” “a little bit,” or “a lot.” It excludes those who said that they had heard “nothing at all” about trend.
Like awareness, the concept that the largest percentage of staff thought impacted their work a fair amount/a great deal was fostering a culture of quality improvement (68%, 95% CI: 67%-69%), and the concept that the smallest percentage thought impacted their work a fair amount/a great deal was health in all policies (43%, 95% CI: 42%-44%). Interestingly, among those staff who were aware of the 6 concepts, a smaller proportion of the workforce thought that the concepts impacted their day-to-day work a fair amount or great deal compared to the percent of staff that had heard of the concept.
Respondents were also asked to identify how involved they felt their agency ought to be in effecting change in a set of specific social determinants of health. Reasonably substantial disagreement was observed in national aggregates. Eighty-three percent of respondents (95% CI: 82%-84%) thought that their agency should be somewhat/very involved in addressing health equity, compared with 46% (95% CI: 45%-47%) who thought their agency should be somewhat/very involved in affecting the quality of transportation in their jurisdiction.
Discussion
PH WINS 2017 generated the second nationally representative dataset of SHA employees and built upon the first iteration of the survey to further grow the knowledge base about the SHA workforce. These data should directly inform workforce strategies to ensure that the workforce and SHAs in which they work can optimally function to address emerging health challenges and improve community health outcomes.
In the SHA workforce, over 3 times as many employees are older than 55 years than are younger than 31 years. Despite the small percentage of the workforce younger than 31 years, nearly one-third of the overall workforce reports having fewer than 5 years of experience in public health practice. This suggests that many come to work at governmental SHAs later in their professional careers. The mobility in the workforce is also worth noting when considering the aging workforce, with two-thirds of the workforce having been in their current position for 5 years or less. While the workforce is generally well educated, less than 20% of the workforce has a degree at any level in public health. This finding, coupled with the aging of the workforce and the large proportion of the workforce with 5 years or fewer in public health practice, points to potential challenges in the workforce pipeline for state governmental public health agencies. Greater engagement with the nation's schools and programs of public health is needed to recruit younger people into the SHA workforce to address the need for a more robust pipeline and increase the proportion of the workforce with public health training.
The pipeline is of critical importance, given the potential for turnover in state governmental public health agencies.4,17 Despite relatively high levels of job and organizational satisfaction in the workforce, more than one-third of the workforce is considering leaving their position in the next year, the majority of whom have already taken steps toward leaving. While pay is a considerable factor in deciding to leave, and pay satisfaction is relatively low compared with job and organizational satisfaction, other factors related to employee engagement clearly contribute to considering leaving. Potential employee departure should be of increased concern among the state governmental public health leadership. When employees leave state health agencies, there is no guarantee that the position will be refilled at the same position level with the same salary or experience level, if it is refilled at all. The SHA workforce never recovered the positions lost in 2008.18,19 Leaders in state health agencies should prioritize retention to maintain an effective workforce. While compensation is rarely within the control of individual managers in an SHA, other factors that could impact retention may be including opportunities to promote staff and grow within a position, assessing and satisfying training needs, improving communication between leadership and staff, and rewarding creativity and innovation in the workplace.
While it may be challenging to create opportunities for advancement on a career ladder within an SHA, leaders can offer stretch assignments, mentoring opportunities, and other programs to help staff grow and practice their skills and develop their leadership abilities. Such programs can also contribute to succession planning, an area of needed investment given the aging workforce, as nonsupervisory staff learn and grow in their positions and demonstrate their leadership skills. Approximately 70% of the workforce agreed or strongly agreed with related statements of “I have had opportunities to learn and grow in my position over the past year,” “I am satisfied that I have the opportunities to apply my talents and expertise,” and “my supervisor provides me with opportunities to demonstrate my leadership skills.” However, there tend to be lower levels of agreement with these statements among nonsupervisory staff as compared to higher levels of supervisory status. Participating departments should assess their own results to consider possible employee development programs. In addition, with only slightly more than half of the workforce agreeing or strongly agreeing that their training needs were assessed, assessing and meeting training needs may be another opportunity to improve worker engagement, which in turn can benefit retention.
While more than 80% of the workforce agreed/strongly agreed that they have good working relationships with their supervisors and that their supervisors treat them with respect, the percentage that agree/strongly agree with the notion that communication between senior leaders and employees is good was much lower. Except for executives, fewer than half of all employees agreed/strongly agreed with this statement. The difference between executives who agreed/strongly agreed and all other staff was more than 20%, indicating that the most senior leaders in state health agencies may be unaware of this challenge and its potential impact on the workplace environment. This finding should serve as a call to all executives working in SHAs to consider strategies to improve their communications with staff throughout the agency.
PH WINS 2017 data also confirm that creativity and innovation are not flourishing in SHAs. This lack of creativity and innovation will make it difficult for SHAs to attract and retain highly educated and skilled individuals who seek to apply their talents to the nation's most pressing social challenges. Promoting creativity and innovation in the workplace and its effect on employee engagement are well described.20–25 However, the strategies to do this—for example, promoting experimentation and supporting failure, creating environments that allow all ideas to be expressed and explored, or creating space for teams to work without assuming that the identified organizational leader must lead discussions and assume responsibility—may run counter to what typically is expected in a governmental work environment and from staff's own degree of risk aversion in the public sector.26 Funding mechanisms may inadvertently reinforce this lack of creativity and innovation by focusing on delivery of a specific service rather than allowing for the proposal of solutions to specific communities' problems. The SHA leaders who want to attract and retain talent should work actively to create workplace engagement and support workforce development strategies that are supportive of creativity and innovation.
Interesting findings have also emerged from PH WINS 2017 data related to staff awareness of and perceived impact of emerging concepts in public health and perceptions of levels of agency involvement in sectors outside of public health. There was greater awareness of concepts that inform the operational practice of public health, such as quality improvement and evidence-based public health, but lower awareness of health in all policies and forming multisectoral partnerships, which are both part of a fundamental shift in the conceptualization of the role of public health and its practice.27 These are critical approaches through which state public health agencies can accomplish their goals of advancing population and community health. However, training and promotion strategies are needed to translate these concepts that appear to be relatively removed from practitioners on the ground into something where staff can understand and relate them to their functional practice.
State health agencies and their leaders are often held accountable for community-level health outcomes measures, and while agencies tackle complex challenges (eg, rising rates of sexually transmitted diseases, opioid use, and obesity rates), little focus is placed on the essential role of the workforce in successfully changing these rates. Healthy communities are dependent upon healthy state governmental public health agencies, with sufficiently trained and engaged staff. While many of the activities within SHAs require external funding, there are opportunities to improve retention and engagement of the workforce with internal initiatives that may not require additional funding.
Implications for Policy & Practice
Almost half of governmental public health staff in SHA-COs say that they are considering leaving their job in the next year or are planning to retire by 2023. This represents a profound challenge to workforce development and means succession planning and the transfer of institutional knowledge ought to be critical components of any workforce plan.
Several of the top reasons for leaving might be somewhat immutable within an organization—pay, opportunities for advancement—but many are ripe for intervention, including perceived lack of support, burnout, and lack of acknowledgment/recognition. These are important reasons staff say they are considering leaving that are suited to amelioration by leadership-led change.
Job satisfaction remains high among public health staff—this appears to be tied to employee engagement, satisfaction with one's supervisor, and organizational support. Leaders can continue to bolster these positive feelings, even while other correlates of job satisfaction (eg, pay) may be less positive and harder to change.
Skill gaps are prevalent and not merely among nonsupervisors but also for supervisors, managers, and executives. Agencies and support institutions, such as public health training centers, ought to tailor high-quality distance training to address these needs by the supervisory tier.
Limitations
This study has several limitations. First, 47 of 50 states responded. While states that did not participate do not appear materially different from their peers who did, this form of bias—where staff in nonparticipating states versus participating states are different—remains possible. Moreover, if respondents are different from nonrespondents, nonresponse bias may be a problem. Balanced repeated replication weights were used to account for sample design and nonresponse. Another limitation is the self-reported nature of the data; this is especially worthy of consideration in analyzing training needs and skill gaps. Finally, these data should be viewed as generalizable only to SHA-CO staff; analyses of local health department staff are conducted elsewhere in this supplement.28,29
Footnotes
PH WINS was funded by the de Beaumont Foundation. Any opinions expressed herein are the authors alone and do not necessarily reflect the position of their respective organizations.
The authors declare no conflicts of interest.
References
- 1.Gebbie KM, Rosenstock L, Hernandez LM. Who Will Keep the Public Healthy? Educating Public Health Professionals for the 21st Century. Washington, DC: The National Academies Press; 2002. [PubMed] [Google Scholar]
- 2.Erwin PC, Brownson RC. Macro trends and the future of public health practice. Annu Rev Public Health. 2017;38:393–412. [DOI] [PubMed] [Google Scholar]
- 3.Leider JP, Coronado F, Beck AJ, Harper E. Reconciling supply and demand for state and local public health staff in an era of retiring baby boomers. Am J Prev Med. 2018;54(3):334–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yeager VA, Beitsch LM, Hasbrouck L. A mismatch between the educational pipeline and public health workforce: can it be reconciled? Public Health Rep. 2016;131(3):507–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Health and Human Services. Public Health 3.0: A Call to Action to Create a 21st Century Public Health Infrastructure. Washington, DC: US Department of Health & Human Services Office of the Assistant Secretary for Health; 2016. [Google Scholar]
- 6.Coronado F, Koo D, Gebbie K. The public health workforce: moving forward in the 21st century. Am J Prev Med. 2014;47(5, suppl 3):S275–S277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beck AJ, Boulton ML. Building an effective workforce: a systematic review of public health workforce literature. Am J Prev Med. 2012;42(5, suppl 1):S6–S16. [DOI] [PubMed] [Google Scholar]
- 8.Hilliard TM, Boulton ML. Public health workforce research in review: a 25-year retrospective. Am J Prev Med. 2012;42(5, suppl 1):S17–S28. [DOI] [PubMed] [Google Scholar]
- 9.Tilson H. When we have data we can count on, everyone WINS. J Public Health Manag Pract. 2015;21(suppl 6):S173–S174. [DOI] [PubMed] [Google Scholar]
- 10.Ehlinger E. Public health wins when we use data to drive decision making. J Public Health Manag Pract. 2015;21(suppl 6):S170–S172. [DOI] [PubMed] [Google Scholar]
- 11.Sellers K, Leider JP, Harper E, et al. The public health workforce interests and needs survey: the first national survey of state health agency employees. J Public Health Manag Pract. 2015;21(suppl 6):S13–S27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leider JP, Bharthapudi K, Pineau V, Liu L, Harper E. The methods behind PH WINS. J Public Health Manag Pract. 2015;21(suppl 6):S28–S35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leider J, Pineau V, Bogaert K, Ma Q. The methods of PH WINS 2017: approaches to refreshing nationally-representative state-level estimates and creating nationally-representative local-level estimates of public health workforce interests and needs. J Public Health Manag Pract. 2019;25(suppl 2):S49–S57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leider JP, Pineau V, Bogaert K, Ma Q. The methods of PH WINS 2017: approaches to refreshing nationally-representative state-level estimates and creating nationally-representative local-level estimates of public health workforce interests and needs. J Public Health Manag Pract. 2019;25(suppl 2):S49–S57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jonathon RBH, Demerouti E. The construct validity of an alternative measure of burnout: investigating the English translation of the Oldenburg Burnout Inventory. Work Stress. 2005;19(3):208–220. [Google Scholar]
- 16.Bogaert K, Castrucci B, Gould E, Rider N, Whang C, Corcoran E. Top training needs of governmental public health departments. J Public Health Manag Pract. 2019;25(suppl 2):S134–S144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yeager VA, Wisniewski JM, Amos K, Bialek R. Why do people work in public health? Exploring recruitment and retention among public health workers. J Public Health Manag Pract. 2016;22(6):559–566. [DOI] [PubMed] [Google Scholar]
- 18.Association of State and Territorial Health Officials. Profile of State and Territorial Public Health. Arlington, VA: Association of State and Territorial Health Officials; 2017. [Google Scholar]
- 19.Young G. State and Local Government Workforce; 2018 Data and 10 Year Trends. Washington, DC: Center for State and Local Governmental Excellence; 2018. [Google Scholar]
- 20.Zhou J, Hoever IJ. Research on workplace creativity: a review and redirection. Annu Rev Organ Psychol Organ Behav. 2014;1(1):333–359. [Google Scholar]
- 21.Froese FJ, Peltokorpi V, Varma A, Hitotsuyanagi–Hansel A. Merit–based rewards, job satisfaction and voluntary turnover: moderating effects of employee demographic characteristics [published online February 27, 2018]. Br J Manage. 10.1111/1467-8551.12283 [Google Scholar]
- 22.Lang J, Kern M, Zapf D. Retaining high achievers in times of demographic change. The effects of proactivity, career satisfaction and job embeddedness on voluntary turnover. Psychology. 2016;7(13):1545. [Google Scholar]
- 23.Maier C, Laumer S, Eckhardt A, Weitzel T. Who really quits?: a longitudinal analysis of voluntary turnover among IT personnel. ACM SIGMIS Database. 2015;46(4):26–47. [Google Scholar]
- 24.Coomber B, Barriball KL. Impact of job satisfaction components on intent to leave and turnover for hospital-based nurses: a review of the research literature. Int J Nurs Stud. 2007;44(2):297–314. [DOI] [PubMed] [Google Scholar]
- 25.Griffeth RW, Hom PW, Gaertner S. A meta-analysis of antecedents and correlates of employee turnover: update, moderator tests, and research implications for the next millennium. J Manage. 2000;26(3):463–488. [Google Scholar]
- 26.Bellante D, Link AN. Are public sector workers more risk averse than private sector workers? Ind Labor Relat Rev. 1981;34(3):408–412. [Google Scholar]
- 27.DeSalvo KB, O'Carroll PW, Koo D, Auerbach JM, Monroe JA. Public health 3.0: time for an upgrade. Am J Public Health. 2016;106(4):621–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robin N, Castrucci BC, McGinty M, Edmiston A, Bogaert K. The First nationally representative benchmark of the local governmental public health workforce: findings from the 2017 public health workforce interests and needs survey. J Public Health Manag Pract. 2019;25(suppl 2):S26–S37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Juliano C, Castrucci B, Leider JP, McGinty M, Bogaert K. The governmental public health workforce in 26 cities: PH WINS results from big cities health coalition members. J Public Health Manag Pract. 2019;25(suppl 2):S38–S48. [DOI] [PMC free article] [PubMed] [Google Scholar]


