Abstract
Overweight children are at risk for poor quality of life (QOL), depression, self-worth, and behavior problems. Exercise trials with children have shown improved mood and self-worth. Few studies utilized an attention control condition, QOL outcomes, or a follow-up evaluation after the intervention ends. The purpose is to test effects of an exercise program versus sedentary program on psychological factors in overweight children. One hundred seventy-five overweight children (87% black, 61% female, age 9.7 ± 0.9 years, 73% obese) were randomized to an 8 month aerobic exercise or sedentary after-school program. Depressive symptoms, anger expression, self-worth, and QOL were measured at baseline and post-test. Depressive symptoms and QOL were also measured at follow-up. Intent-to-treat mixed models evaluated intervention effects, including sex differences. At post-test, QOL, depression, and self-worth improved; no group by time or sex by group by time interaction was detected for QOL or self-worth. Boys’ depressive symptoms improved more and anger control decreased in the sedentary intervention relative to the exercise intervention at post-test. At follow-up, depressive symptoms in boys in the sedentary group decreased more than other groups. Exercise provided benefits to QOL, depressive symptoms, and self-worth comparable to a sedentary program. Sedentary programs with games and artistic activities, interaction with adults and peers, and behavioral structure may be more beneficial to boys’ mood than exercise. Some benefits of exercise in prior studies are probably attributable to program elements such as attention from adults.
Trial Registration: Clinicaltrials.gov, NCT02227095.
Keywords: Aerobic exercise, Obesity, Black, Depressive symptoms, Anger
Children who were overweight or obese (mostly Black) showed similar benefits to their emotional well-being from aerobic and sedentary after-school programs, perhaps due to attention from adults in an organized setting.
Implications.
Practice: Effects of organized exercise programs are largely similar to those of sedentary recreational programs in improving the quality of life, mood, and self-worth of overweight and obese black children.
Policy: Engaging overweight and obese children in quality recreational programs including exercise, games, and arts activities may improve their QOL, mood, and self-worth.
Research: Some of the psychological benefits of exercise programs in prior studies with children are probably attributable to program elements other than exercise, such as adult attention, behavioral structure, and peer interactions.
INTRODUCTION
Alarmingly, child obesity increased eightfold over the past 4 decades worldwide [1]. Black children are more likely to be obese than their white counterparts in the USA [2, 3]. Children who are overweight have worse quality of life (QOL) than their normal-weight peers [4–6]. Buttitta et al. reviewed the literature regarding QOL in children and adolescents who are overweight and obese [7]. Of 34 articles, a majority of studies showed overweight and obesity affect all aspects of QOL, with only two studies failing to find a significant difference in normal weight versus children and adolescents who are overweight or obese. An alarming finding was that not only are children who are overweight or obese likely to have impaired health-related QOL, their level of impairment is similar to those of children and adolescents who have been diagnosed with cancer [8]. Morbidity, mortality, and QOL—but not intermediate biomarkers—are considered important health outcomes by the U.S. Preventive Services Task Force, which determines whether a preventive service can be covered without a co-payment [9].
Overweight status is linked with negative mood and poor self-worth in children. Body mass index (BMI) z-score was linearly related to depression, anxiety, and bullying in children [10]. Parent-reported outcomes show that children with severe obesity were higher on depressive symptoms, anxiety, fatigue, anger, and mobility than their peers [11]. Children and adolescents with metabolic syndrome, who are typically overweight or obese, have higher scores in hostility, hostile affect, and aggressive responding when compared with those without metabolic syndrome [12]. Children who are overweight are at risk of behavior problems [13], and heavier children show more aggression [14]. BMI was inversely associated with children’s self-worth [15].
Physical activity and fitness are associated with health-related QOL and depressed mood in children [16–19]. Mechanisms for exercise benefits on mood have been identified in animal studies [19]. A meta-analysis of eight studies in adolescents with depression found a moderate benefit of exercise interventions on depression [20, 21]. A vigorous physical activity after-school program reduced depressive symptoms in black and white overweight children [22]. The same study showed that the exercise program reduced anger expression and externalized anger, which may reflect dysphoria, and fitness improvements were correlated with reductions in externalized anger [23]. However, there is a lack of research comparing exercise with a sedentary intervention.
Longitudinal, cross-sectional, and quasi-experimental studies of children link physical activity and aerobic fitness with positive self-worth [15, 16]. Two randomized controlled trials of exercise programs in children and adolescents with excess weight found benefits on self-worth [22, 24]. Meta-analyses show a small benefit of exercise programs on self-worth in children, but the evidence is from small, inconsistent trials [25, 26].
No ethnic or sex differences are apparent in QOL among children with obesity [8]. However, degree of obesity was unrelated to global self-worth in black children [14]. Hispanic and white, but not black, girls with obesity report lower self-worth than nonobese peers [27]. An exercise intervention did not improve global self-worth in black children who were overweight, though it did in white peers [22]. Benefits of physical activity on QOL, depression, and self-worth may be less evident in black children than their white peers [22, 24, 25, 28, 29]. There is scant literature relating physical activity to QOL and other psychological factors, especially in children who are overweight, obese, or black.
The purpose of this study was to test the effects of an after-school exercise or sedentary control intervention on QOL and mood in a predominantly black community sample of children who were overweight or obese. Follow-up measures of QOL and depressive symptoms were obtained after the end of the intervention to assess possible lasting effects. This design isolates the effect of exercise per se from other elements of an after-school program. Improvements in the exercise group versus the attention control group would support a biologically based explanation for exercise effects, whereas a null result would support a psychosocial explanation. We hypothesized that the exercise intervention would improve QOL, mood (depressive symptoms and anger expression), and self-worth more than the sedentary control intervention.
METHOD
Participants
One hundred seventy-five participants (8–11 years old [M = 9.7, SD = 0.9], 87% black, 61% female) who were overweight or obese (BMI ≥ 85th percentile for age and sex) were recruited from public elementary schools in Augusta, GA from 2008 to 2011 for a parallel randomized controlled trial. [30] Children in the study were sedentary (no regular participation in an exercise program more than 1 hr/week) and were excluded if they had any medical conditions or took medications that could affect growth, physical activity, nutritional status, or metabolism. Parents reported child health history and medications. Written informed consent was obtained from parents or guardians and written assent from children. The Human Assurance Committee of the Medical College of Georgia approved the study. Testing and intervention occurred at the Medical College of Georgia in 2008–2013.
Procedure
Individual participants in four cohorts were assigned randomly to one of two conditions: aerobic exercise or sedentary attention control (1:1). After each yearly cohort completed baseline testing and prior to intervention, the study statistician (J.L.W.) assigned a uniform (0, 1) random number to each participant using SAS software, versions 9.3 or 9.4 (SAS Institute Inc.), within their respective race, sex, and school group. If the number was between 0 and 0.5, the child was randomized to the exercise condition, and if the number was above 0.5, to the control condition. The study coordinator informed the families of the child’s assignment. Measures were individually administered at the Georgia Prevention Institute by qualified testers at baseline (during summer, prior to first day of school), post-test (the last 2 months of the school year), and at follow-up (approximately 1 year after completing the intervention, 19 months after baseline). Research staff were available to read questionnaires to children if needed.
Interventions
Participants in both the exercise and control groups were offered an after-school program including a snack and ½ hr of supervised homework time every school day for about 8 months (average number of days offered = 138, SD = 9) in 2008–2012. Participants were transported by bus daily to the Georgia Prevention Institute for the after-school intervention and bused back to their neighborhoods after each session. Lead instructors were rotated between the two groups every 2 weeks, and assistant instructors were rotated between the two groups every week. Both groups could earn points that were redeemed for small prizes weekly for desired behaviors. The reward schedule was periodically calibrated to keep rewards similar between groups.
The groups differed in that they were offered either an exercise or sedentary program. The aerobic exercise group engaged in playful instructor-led aerobic activities for 40 min per day. Each session included vigorous aerobic activities and games (e.g., running games, ball games, and jump rope), interspersed with brief rest periods. Games were selected based on interest and ability to elicit vigorous activity. Children wore heart rate monitors every day (S610i; Polar Electro, Oy, Finland) with which they could monitor their own performance and from which data were collected daily. Points in the exercise group were earned for a daily average heart rate above 150 beats per minute, with more points for higher average heart rates. The attention control group engaged in instructor-led sedentary activities (e.g., board games, puzzles, art, and music). Points in the control group were earned for participation and good behavior.
Measures
Pediatric Quality of Life Inventory
The Pediatric Quality of Life Inventory (PedsQL) [31] is a 23-item instrument designed to measure core dimensions of health and yields a total score. The child rates how much of a problem each item has been for them in the past month on a 0–4 scale, with never (0), almost never (1), sometimes (2), often (3), and almost always (4). The PedsQL was completed at baseline (α = .75), post-test (α = .66), and follow-up (α = .79).
Children’s Depression Inventory
The Children’s Depression Inventory (CDI) [32] is a 27-item self-report questionnaire designed to assess depressive symptoms in children and adolescents that have occurred within 2 weeks of completing the assessment. Each item offers choices for the absence of a symptom (0), mild or probable symptom (1), and definite symptom (2). This instrument includes subscales for measuring negative mood, interpersonal problems, ineffectiveness, anhedonia, and negative self-esteem, in addition to a total score ranging from 0 to 54. A CDI total score ≥19 is the criterion for a positive screen in pediatric nonclinical populations. In the current study, 10% of the sample (17 children) screened positive on this measure at baseline. Also, 21% of the sample (37 children) endorsed self-harm at baseline by selecting either “I think about killing myself but I would not do it” (n = 34) or “I want to kill myself” (n = 3). The study physician offered referrals to families with such concerns. Participants completed this measure at baseline (α = .86), post-test (α = .80), and follow-up (α = .86).
Pediatric Anger Expression Scale
The Pediatric Anger Expression Scale (PAES) [33] is a 15-item self-report measure of anger expression styles. This questionnaire yields an overall Anger Expression score that is comprised of three factor-analytically derived scales: Anger In (holding in or denying anger), Anger Out (openly expressed and potentially aggressive anger), and Anger Control (cognitive resolution of conflict or frustration). The child rates the frequency with which they use a specific manner of anger expression as hardly ever (1), sometimes (2), or often (3). Total inventory scores range from 5 to 15, with normative means from 9.2 to 9.5 (anger-suppression), 8.9 to 9.7 (anger-out), and 9.9 to 10.1 (anger-reflection/control). The overall Anger Expression score is calculated with the following formula: (Anger In + Anger Out) – Anger Control. Children completed this measure at baseline (α = .51) and post-test (α = .45). Higher scores on Anger In and Out and the overall Anger Expression score reflect more anger expression. Higher Anger Control scores indicate better control.
Self-perception profile for children
The Harter Self-Perception Profile for Children [34] is a 36-item self-report inventory that taps children’s perceptions of themselves. This instrument includes a measure of Global Self-Worth. Each question is presented in a “structured alternative format,” in which the child first decides which description is most like him or her, then gauges whether the chosen description is “sort of true” or “really true” for him/her. Each item is scored on a 1–4 scale, with 1 indicating low perceived competence and 4 indicating high perceived competence. This measure was completed at baseline (α = .76) and post-test (α = .82).
Body composition and fitness
Whole-body dual-energy x-ray absorptiometry measured fatness (body fat %), and cardiovascular fitness was determined using a multistage treadmill test (oxygen consumption [VO2] relative to body mass in mL/kg/min) [35–37].
Statistical analysis
The variables analyzed in this paper are secondary outcomes for a randomized controlled trial (Clinical Trials Identifier: NCT02227095). To power for the detection of small group differences in change between baseline and post-test (d = .17) with a correlation between measurement times near 0.5, n = 68/group at post-test was estimated to provide 80% power. Statistical analysis was performed using SAS 9.3 or 9.4, or SPSS 23. Statistical significance was assessed using an alpha level of 0.05. Cronbach’s alpha was calculated.
Repeated measures mixed models were used for each outcome to examine the effects of race, sex, group, and measurement time on the outcome. Two-time point models (baseline and post-test) were done for each outcome, and three-time point models for those outcomes assessed at follow-up. Each model controlled for cohort, race, and sex. Main effects, two- and three-factor interactions of race by group by time or sex by group by time were examined for each outcome measure in separate models. Subject nested within group was the random effect in each model.
Where there were only two measurement times (baseline and post-test), an unstructured covariance structure was assumed. If none of the three-factor interactions were statistically significant, the model was reduced to examine the two-factor interaction of group and time. Final models contained at a minimum cohort, race, sex, the main effects and two-factor interaction between group and time, and any statistically significant three-factor interactions.
For analyses including follow-up data, linear and quadratic effects across the three time points within group or within the cross-classification of race or sex and group were examined using contrasts. Additionally, contrasts were used to examine whether there were differences in the linear or quadratic effects between intervention and control groups overall, or within race or sex levels where appropriate.
A Bonferroni adjustment to the overall alpha level was used to perform post hoc pairwise differences in changes of each measure over time, within group for models with only the two-factor interaction with group and time, or within race and group or within sex and group for models containing three-factor interactions.
RESULTS
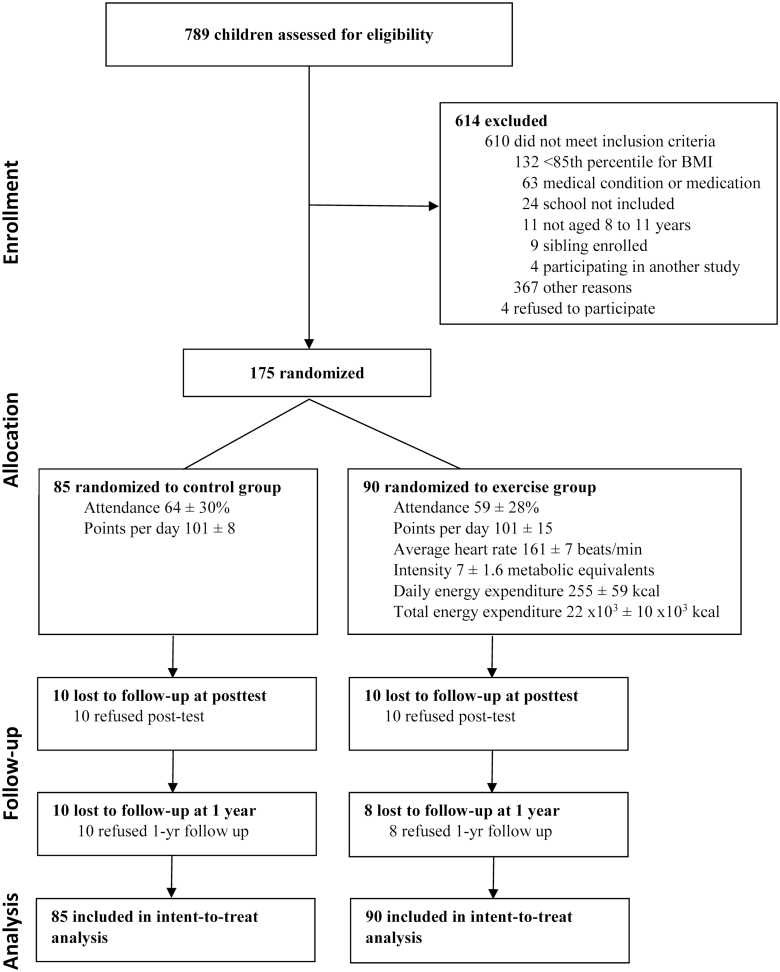
The participant flow diagram is presented in Fig. 1. The two groups were similar at baseline (Table 1). No child was taking antidepressant medication. Few cases of nonblack participants precluded analysis of race differences. Attendance and points earned were similar in control and exercise groups (64% ± 30% vs. 59% ± 28%, 101 ± 15 vs. 101 ± 8 points, p > .20). In the exercise group, daily average heart rates were 161 ± 7 bpm, indicating vigorous activity.
Fig 1.
Flow diagram of study participants.
Table 1.
Participant characteristics
| Control (n = 85) | Exercise (n = 90) | |||
|---|---|---|---|---|
| Baseline | Post | Baseline | Post | |
| % or mean ± SD | % or mean ± SD | % or mean ± SD | % or mean ± SD | |
| Age (yr) | 9.7 ± 0.88 | 10.4 ± 0.89 | 9.6 ± 0.88 | 10.4 ± 0.87 |
| Black | 84.7 | – | 90.0 | – |
| Female | 55.3 | – | 66.7 | – |
| Body fat (%) | 36.7 ± 7.3 | 36.2 ± 8.0 | 38.3 ± 6.9 | 36.2 ± 7.7 |
| VO2 peak (mL/kg/min) | 30.0 ± 5.1 | 31.2 ± 5.8 | 28.9 ± 5.7 | 31.6 ± 5.6 |
| Quality of Life | 77.3 ± 14.8 | 81.0 ± 11.9 | 78.8 ± 13.6 | 80.4 ± 12.5 |
| Depressive Symptoms | 8.1 ± 7.5 | 6.8 ± 5.9 | 7.6 ± 6.6 | 6.3 ± 5.2 |
| Positive screen | 12 | 5 | 8 | 3 |
| Self-harm | 21 | 15 | 21 | 10 |
| Anger Expression | 7.1 ± 4.4 | 7.6 ± 3.7 | 7.5 ± 3.9 | 7.3 ± 3.1 |
| Anger In | 10 ± 2 | 10 ± 3 | 10 ± 2 | 10 ± 2 |
| Anger Out | 8 ± 3 | 9 ± 2 | 9 ± 2 | 8 ± 2 |
| Anger Control | 11 ± 2 | 11 ± 2 | 11 ± 2 | 11 ± 2 |
| Global Self-Worth | 3.2 ± 0.69 | 3.3 ± 0.53 | 3.2 ± 0.63 | 3.4 ± 0.63 |
There was one Pacific Islander and one other race participant in the control group. All other participants were black or white race. There were three Hispanic black participants in the exercise group, and two black Hispanic and two white Hispanic participants in the control group. There were no group differences at baseline for any of the variables reported in this table.
No sex by group by time or group by time interactions were detected for any QOL scale, Global Self-Worth, or any anger expression scale. Adjusted least square means and 95% confidence intervals are reported in Table 2. However, there were main effects of time such that scores improved from baseline to post-test on QOL (p = .03), CDI (p = .02), and Global Self-Worth (p = .02). No main effect of time was found for anger measures. Participants in the exercise group were found to have lost body fat and be fitter at post-test than baseline when compared with the control group (−1.8% vs. −0.8%, 2.7 vs. 1.3 mL/kg/min, both p = .04) [37].
Table 2.
Means (95% CI) by measurement time and adjusted change from baseline to post-test by group
| Outcome variable | Interaction variable | Control adjusted Δ | Exercise adjusted Δ | p for ΔControl Vs. ΔExercise |
|---|---|---|---|---|
| Quality of Life | 3.7 (0.7, 6.7)* | 1.1 (−1.8, 3.9) | .22 | |
| Depressive Symptomsa | Female | −0.4 (−2.4, 1.5) | −2.0 (−3.7, −0.3)* | .24 |
| Male | −3.1 (−5.3, −1)** | 0.5 (−1.8, 2.8) | .03 | |
| Anger Expressiona | Female | 0.1 (0.0, 0.3) | −0.1 (−0.2, 0.1) | .06 |
| Male | −0.1 (−0.3, 0.1) | 0.1 (−0.1, 0.3) | .07 | |
| Anger In | 0.4 (−0.3, 1.0) | −0.1 (−0.8, 0.5) | .32 | |
| Anger Out | 0.1 (−0.5, 0.7) | −0.4 (−1.0, 0.1) | .19 | |
| Anger Controla | Female | −0.5 (−1.2, 0.3) | 0.1 (−0.5, 0.7) | .23 |
| Male | 0.6 (−0.1, 1.4) | −1.1 (−2.0, −0.3)** | .003 | |
| Global Self-worth | 0.2 (0.0, 0.3) | 0.1 (0.0, 0.3) | .84 |
aSex by group by time interaction p < .05, *within-group change p < .05, **within-group change p < .01.
Bold value indicates between-group change, p < .05.
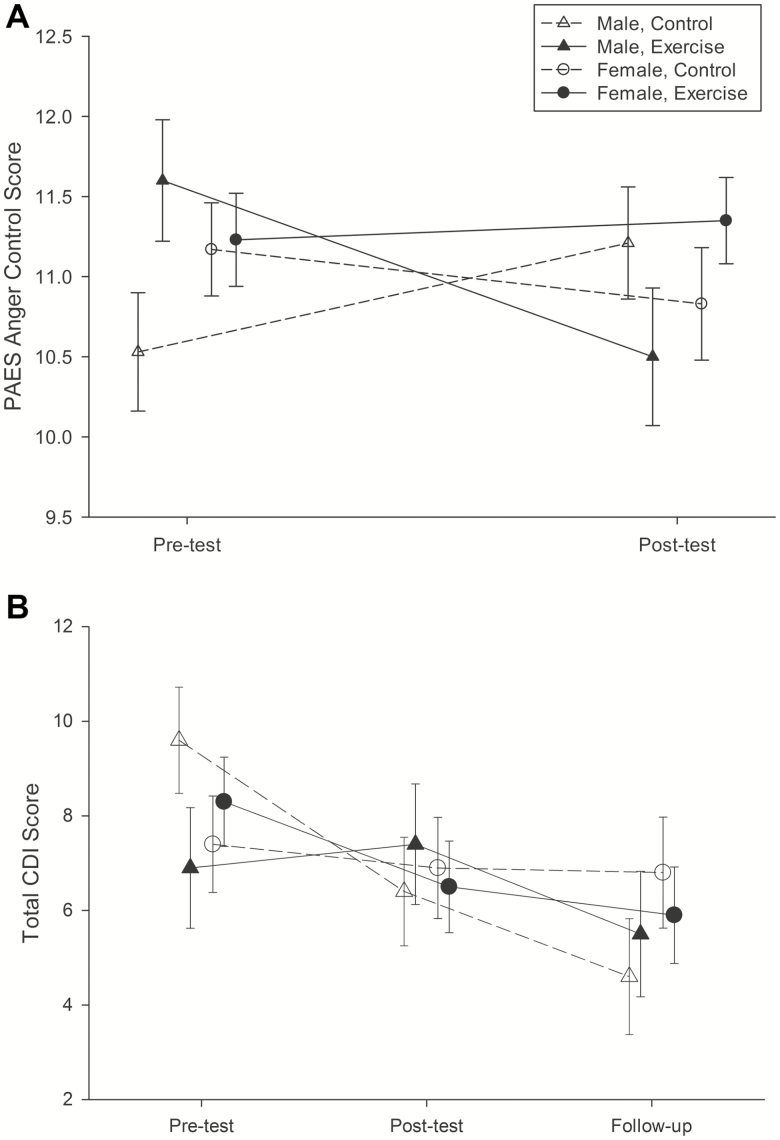
Three-factor interactions with sex, group, and time were found for total CDI score and Anger Control (Fig. 2), indicating that the changes over time were different in the sex by exercise groups. On the CDI, boys benefited from the sedentary intervention (−3.1 vs. 0.5 in male exercise only, p = .03). Girls’ CDI scores decreased after exercise but this was not different from the change in controls (−2.0 female exercise vs. −0.4 in female control, p = .24).
Fig 2.
Adjusted means and standard error for interactions with sex. (A) Anger Control scores from the PAES from baseline to post-test. (B) CDI total scores from baseline to follow-up.
A significant three-factor interaction of sex by group by time was detected for overall Anger Expression from the PAES with increases in the male exercise and decreases in male controls and females in both control and exercise groups, but there were no statistically significant post hoc pairwise differences. The changes from baseline to post within males and females were not different between exercise and control groups. On the Anger Control scale, males assigned to exercise reduced their anger control (−1.1 exercise vs. 0.6 control, p < .01), with no changes in the girls (0.1 exercise, −0.5 control, respectively).
Analyses of follow-up data showed a statistically significant group three-factor interaction with sex, group, and time for CDI total score (Fig. 2b). Males in the sedentary control group reported decreased depressive symptoms over time (p = .01) when compared with males in the exercise group (−5.0, −1.4, respectively) or females in either condition (−2.4 vs. −0.6 in control). No other group by time effects were found at follow-up testing.
DISCUSSION
This study examined exercise-specific effects of an 8 month after-school intervention on QOL, mood measures, and self-worth in a predominantly black community sample of children who are overweight and obese. The exercise intervention resulted in a reduction in body fat and improved fitness, demonstrating a training effect. Compared with a sedentary attention control group, the exercise intervention showed no advantage on QOL, internalized, externalized, or overall anger expression, or self-worth. Boys appeared to benefit more from the sedentary intervention than the exercise intervention for depressive symptoms, whereas depressive symptoms were equally improved by exercise and sedentary interventions in girls. Both intervention programs showed improved QOL, depressive symptoms, and self-worth from baseline to post-test. Based on these results, we concluded that some of the benefits of exercise on QOL factors in prior studies may be due to program elements such as attention from caring adults who provide behavioral structure (e.g., rules and routines), socializing with peers, snacks, or watching less television. Results apply to children with overweight or obesity, particularly black children.
Although there were no group by time effects for QOL in the current study, both intervention groups did show improved QOL from baseline to post-test. This result is consistent with previous research [16, 17] indicating that QOL improves with increased physical activity. One study using step-tracking in a majority-black sample of children showed a positive relationship between steps taken and health-related QOL [28]. A cross-sectional study in low-income children found that depression moderated the relationship between physical activity and QOL such that physical activity was not related to QOL in children with more depressive symptoms [20]. Ra and Gang [11] suggest that a combination of physical activity encouragement and social support may be beneficial for improved health-related QOL in at-risk pediatric populations. Social support elements in the interventions may have contributed to improvements in both groups in the current study. This study is a contribution to the scant literature relating physical activity to QOL in children, especially in black children and/or children who are overweight.
In the current study, there were no differential effects of the exercise or sedentary interventions on depressive symptoms among girls. This may be because the sample in the current study is predominantly black. Duncan and colleagues [29] found that being more physically active was related to being less depressed in Latina and white girls, but not in black girls. A meta-analysis of physical activity trials in depressed adolescents found that physical activity reduced depression symptoms, but sex and race of participants were not analyzed [21].
Boys in the current study improved more on depressive symptoms in the sedentary intervention than the exercise intervention. A previous study in children who were overweight showed a dose–response effect such that more exercise reduced depressive symptoms, with no moderation by sex or race [22]. However, that study compared an exercise intervention with a no-intervention control condition, whereas in the current study, an exercise and a sedentary intervention were compared to isolate the effect of the exercise component. Children in the Petty et al. study may have been more responsive to intervention due to having worse symptoms of depression; however, this is difficult to compare because a different measure was used. In both samples, only a few children screened positive for depression at baseline (4% Petty et al., 10% here). Although there were no significant differences at baseline between the exercise and control groups, the control group (esp. boys) in the current study endorsed slightly more depressive symptoms at baseline than the exercise group (Fig. 2b). We suspect that this may have masked exercise-induced improvements in depressive symptoms, due to regression to the mean in the control group. Nonetheless, in the current study, depression symptoms improved in children in both groups after the interventions, suggesting that nonspecific factors such as reduced time watching television, provision of snacks, positive interactions with peers and adults, and contingent rewards from adults during the interventions may be responsible.
In the current study, no group differences on self-worth effects of intervention were found, but there were within-group main effects for improved global self-worth from baseline to post-test. Daley et al. [24] compared exercise therapy (combination aerobic training and counseling), versus a stretching condition that had the same amount of face-to-face contact as the exercise therapy, versus usual care in a predominantly white sample. They reported similar short-term benefits to physical self-worth in the exercise therapy and stretching interventions. This along with the current results suggests that supportive attention from adults can be as effective as physical activity in improving self-worth in children who are overweight.
Black children’s self-worth appears to be less responsive to a physical activity intervention than that of white children. Improved self-worth as a result of physical activity may be more evident in predominantly white samples of children and adolescents. Petty et al. [22] showed that a 3 month physical activity program increased self-worth about physical appearance and increased global self-worth only in white children. A randomized controlled trial involving a predominantly white sample of adolescents found that an 8 week exercise intervention improved perceived self-worth [24]. The meta-analysis conducted by Liu et al. [25], including studies conducted primarily in the USA, Australia, and the UK, found a beneficial effect of physical activity programs on self-worth. Sutter et al. [38] found that, for black adolescents, BMI z-score did not predict changes in self-worth over time, whereas it did significantly predict decreases in self-worth for white adolescents. In a sample of inner-city minority children, Wong et al. [39] showed that weight status was unrelated to self-worth.
In the current study, exercise provided similar improvements on internalized, externalized, or overall anger expression when compared with a sedentary attention control group. However, among boys, anger control was reduced more in the exercise condition compared with the sedentary condition, an unexpected result. In contrast, a prior study [23] with a 3 month exercise intervention and a no-intervention control group found that participation in an after-school exercise program resulted in reduced anger expression and that fitness improvements and adherence to the program were correlated with decreased externalized anger. In another study, depressive symptoms in boys were predicted by more sedentary time [40].
It could be that structured sedentary programs that include games and artistic activities and interaction with adults and peers might be more beneficial to boys’ mood than exercise, perhaps because boys may feel pressured to participate in athletic activities more typical of their gender role [41] rather than more artistic activities which are preferred by children this age [42–45]. Posner and Vandell [43] conducted an in-depth analysis of how black and white children spend their time. Television watching was the most common after-school activity, which was associated with maladjustment and offset by structured programs. Girls were more likely to spend time on academic and social activities, whereas boys spent time in coached sports. However, the children in their study were more likely to choose socializing (“just talking”) as their main activity by the time they reached 5th grade. The sedentary group in the current study had more opportunities to talk among themselves during their time in the intervention. Structured sedentary programs (e.g., positive youth development programs) may provide children with opportunities to improve social skills (e.g., communication, cooperation, conflict resolution, and teamwork) and develop friendships in an environment where there is little pressure on their performance [42, 46–48]. Boys may feel more comfortable in such a setting than in physical activity which they associate with competition [42].
Alternatively, the interaction in the current study could reflect that arts and crafts are a means of personal expression and creativity or even that these activities are more conducive to collaborative play and interpersonal communication among boys [49]. Previous research has linked sport participation to more aggressive behavior in boys [50]. Reduced anger control might be an unwanted side effect of exercise intervention in boys, even with behavioral structure. In this study, this is more likely regression to the mean and Type 1 error due to the slightly higher baseline level of anger control in boys in the exercise group, though this difference was not statistically significant (Fig. 2a). Also, the anger scale was not very reliable in this sample.
A limitation of this study was that participants and measurement staff were not blinded to intervention condition. We did not have enough nonblack participants to test for race differences. The study was not powered to detect 3-way interactions; therefore, those results may be sample-specific. There was not a no-intervention control group. Questionnaires were read to some children if needed; this was not adjusted in the analyses.
The current study tested the effect of exercise or sedentary recreational interventions on QOL, negative mood, and self-worth of predominantly black children who are overweight. Although exercise did result in health benefits to the children that were not seen in the sedentary group, the overall benefits of both interventions on psychological factors were largely similar. In conclusion, some of the psychological benefits of exercise programs in prior studies with children are probably attributable to program elements other than exercise, such as adult attention, behavioral structure (rules, routines, and adult-led activities), interaction with peers, and reduction in television watching and similar pursuits. Afterschool programs are beneficial to child development, and a major component of successful afterschool programs is the staff leading them [44]. Having a structured environment and supportive staff can help children in afterschool programs improve academically and socially, and keep them from engaging in risky behaviors [44]. Positive adult-child relationships are a major factor in a child’s cognitive development, social skills learning, and academic advancement [47]. Although physical activity programs are certainly needed to support physical health, provision of quality adult-led after-school programs may be more essential for psychosocial health in children.
Acknowledgments
This work was supported by the National Institutes of Health (grant R01 HL087923) to Augusta University (Principal Investigator, C. L. Davis). The content is solely the responsibility of the authors and does not necessarily represent the views of the National Institutes of Health.
Compliance with Ethical Standards
Authors’ Contributions: C. F. Williams drafted the manuscript, and assisted with statistical analyses and quality control. E. E. Bustamante contributed to drafting the manuscript. J. L. Waller assisted with design of the study and conducted intent to-treat statistical analyses. C. L. Davis conceived the study, contributed to drafting the manuscript and oversaw data collection and analysis. All authors reviewed the manuscript prior to submission.
Conflicts of Interest: The authors declare that they have no conflicts of interest.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Institutional Review Board of the Medical College of Georgia approved the study. This article does not contain any studies with animals.
Informed Consent: Informed consent or assent was obtained from all participants included in the study.
References
- 1. N. C. D. Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–2642. doi: 10.1016/S0140-6736(17)32129-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in us youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA. 2018;319(16):1723–1725. doi: 10.1001/jama.2018.3060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics. 2018;141(3). pii: e20173459. doi:10.1542/peds.2017–3459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Williams J, Wake M, Hesketh K, Maher E, Waters E. Health-related quality of life of overweight and obese children. JAMA. 2005;293(1):70–76. [DOI] [PubMed] [Google Scholar]
- 5. Wynne C, Comiskey C, Hollywood E, Quirke MB, O’Sullivan K, McGilloway S. The relationship between body mass index and health-related quality of life in urban disadvantaged children. Qual Life Res. 2014;23(6):1895–1905. [DOI] [PubMed] [Google Scholar]
- 6. Ottova V, Erhart M, Rajmil L, Dettenborn-Betz L, Ravens-Sieberer U. Overweight and its impact on the health-related quality of life in children and adolescents: results from the European KIDSCREEN survey. Qual Life Res. 2012;21(1):59–69. [DOI] [PubMed] [Google Scholar]
- 7. Buttitta M, Iliescu C, Rousseau A, Guerrien A. Quality of life in overweight and obese children and adolescents: a literature review. Qual Life Res. 2014;23(4):1117–1139. [DOI] [PubMed] [Google Scholar]
- 8. Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289(14):1813–1819. [DOI] [PubMed] [Google Scholar]
- 9. Wolff TA, Krist AH, LeFevre M, et al. . Update on the methods of the U.S. preventive services task force: linking intermediate outcomes and health outcomes in prevention. Am J Prev Med. 2018;54(1S1):S4–S10. [DOI] [PubMed] [Google Scholar]
- 10. Bell LM, Byrne S, Thompson A, et al. . Increasing body mass index z-score is continuously associated with complications of overweight in children, even in the healthy weight range. J Clin Endocrinol Metab. 2007;92(2):517–522. [DOI] [PubMed] [Google Scholar]
- 11. Selewski DT, Collier DN, MacHardy J, et al. . Promising insights into the health related quality of life for children with severe obesity. Health Qual Life Outcomes. 2013;11:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Räikkönen K, Matthews KA, Salomon K. Hostility predicts metabolic syndrome risk factors in children and adolescents. Health Psychol. 2003;22(3):279–286. [DOI] [PubMed] [Google Scholar]
- 13. Lumeng JC, Gannon K, Cabral HJ, Frank DA, Zuckerman B. Association between clinically meaningful behavior problems and overweight in children. Pediatrics. 2003;112(5):1138–1145. [DOI] [PubMed] [Google Scholar]
- 14. Young-Hyman D, Schlundt DG, Herman-Wenderoth L, Bozylinski K. Obesity, appearance, and psychosocial adaptation in young African American children. J Pediatr Psychol. 2003;28(7):463–472. [DOI] [PubMed] [Google Scholar]
- 15. Reddon H, Meyre D, Cairney J. Physical activity and global self-worth in a longitudinal study of children. Med Sci Sports Exerc. 2017;49(8):1606–1613. [DOI] [PubMed] [Google Scholar]
- 16. Strong WB, Malina RM, Blimkie CJ, et al. . Evidence based physical activity for school-age youth. J Pediatr. 2005;146(6):732–737. [DOI] [PubMed] [Google Scholar]
- 17. Morales PF, Sánchez-López M, Moya-Martínez P, et al. . Health-related quality of life, obesity, and fitness in schoolchildren: the Cuenca study. Qual Life Res. 2013;22(7):1515–1523. [DOI] [PubMed] [Google Scholar]
- 18. Brown HE, Pearson N, Braithwaite RE, Brown WJ, Biddle SJ. Physical activity interventions and depression in children and adolescents: a systematic review and meta-analysis. Sports Med. 2013;43(3):195–206. [DOI] [PubMed] [Google Scholar]
- 19. Dishman RK, Berthoud HR, Booth FW, et al. . Neurobiology of exercise. Obesity. 2006;14(3):345–356. [DOI] [PubMed] [Google Scholar]
- 20. Ra JS, Gang M. Depression moderates between physical activity and quality of life in low-income children. Appl Nurs Res. 2016;29:e18–22. doi: 10.1016/j.apnr.2015.06.004 [DOI] [PubMed] [Google Scholar]
- 21. Radovic S, Gordon MS, Melvin GA. Should we recommend exercise to adolescents with depressive symptoms? A meta-analysis. J Paediatr Child Health. 2017;53(3):214–220. [DOI] [PubMed] [Google Scholar]
- 22. Petty KH, Davis CL, Tkacz J, Young-Hyman D, Waller JL. Exercise effects on depressive symptoms and self-worth in overweight children: a randomized controlled trial. J Pediatr Psychol. 2009;34(9):929–939. doi: 10.1093/jpepsy/jsp007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tkacz J, Young-Hyman D, Boyle CA, Davis CL. Aerobic exercise program reduces anger expression among overweight children. Pediatr Exerc Sci. 2008;20(4):390–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Daley AJ, Copeland RJ, Wright NP, Roalfe A, Wales JK. Exercise therapy as a treatment for psychopathologic conditions in obese and morbidly obese adolescents: a randomized, controlled trial. Pediatrics. 2006;118(5):2126–2134. [DOI] [PubMed] [Google Scholar]
- 25. Liu M, Wu L, Ming Q. How does physical activity intervention improve self-esteem and self-concept in children and adolescents? Evidence from a meta-analysis. PLoS One. 10(8):e0134804. doi: 10.1371/journal.pone.0134804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ekeland E, Heian F, Hagen K, Coren E. Can exercise improve self esteem in children and young people? a systematic review of randomised controlled trials. Br J Sports Med. 2005;39(11):792–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Strauss RS. Childhood obesity and self-esteem. Pediatrics. 2000;105(1):e15. [DOI] [PubMed] [Google Scholar]
- 28. Staiano AE, Beyl RA, Hsia DS, et al. . Step tracking with goals increases children’s weight loss in behavioral intervention. Child Obes. 13(4):283–290. doi: 10.1089/chi.2017.0047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Duncan SC, Strycker LA, Chaumeton NR. Sports participation and positive correlates in African American, Latino, and white girls. Appl Dev Sci. 2015;19(4):206–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Krafft CE, Schwarz NF, Chi L, et al. . An 8-month randomized controlled exercise trial alters brain activation during cognitive tasks in overweight children. Obesity (Silver Spring). 2014;22(1):232–42. Epub 2013/06/22. doi:10.1002/oby.20518. PubMed PMID: 23788510; PMCID: PMC4077546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3(6):329–341. [DOI] [PubMed] [Google Scholar]
- 32. Kovacs M. Children’s Depression Inventory Manual. North Tonawanda, NY: Multi-Health Systems Inc.; 1992. [Google Scholar]
- 33. Jacobs GA, Phelps M, Rohrs B. Assessment of anger expression in children: the pediatric anger expression scale. Pers Individ Dif. 1989;10(1):59–65. [Google Scholar]
- 34. Harter S. The Self-perception Profile for Children: Revision of the Perceived Competence Scale for Children. Denver, CO: University of Denver; 1985. [Google Scholar]
- 35. Rowland TW. Aerobic Exercise Testing Protocols. Champaign, IL: Human Kinetics; 1993. [Google Scholar]
- 36. American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription. 6th ed Baltimore, MD: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 37. Davis CL, Litwin SE, Pollock NK, et al. . Effects of aerobic training on arterial stiffness and cardiovascular risk in overweight minority children: The SMART randomized controlled trial. Under review, Sept. 2018. [Google Scholar]
- 38. Sutter C, Nishina A, Adams RE. How you look versus how you feel: associations between BMI z-score, body dissatisfaction, peer victimization, and self-worth for African American and white adolescents. J Adolesc. 2015;43:20–28. [DOI] [PubMed] [Google Scholar]
- 39. Wong WW, Mikhail C, Ortiz CL, et al. . Body weight has no impact on self-esteem of minority children living in inner city, low-income neighborhoods: a cross-sectional study. BMC Pediatr. 2014;14:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sund AM, Larsson B, Wichstrøm L. Role of physical and sedentary activities in the development of depressive symptoms in early adolescence. Soc Psychiatry Psychiatr Epidemiol. 2011;46(5): 431–441. [DOI] [PubMed] [Google Scholar]
- 41. Martínez-Andrés M, Bartolomé-Gutiérrez R, Rodríguez-Martín B, Pardo-Guijarro MJ, Martínez-Vizcaíno V. “Football is a boys’ game”: children’s perceptions about barriers for physical activity during recess time. Int J Qual Stud Health Well-Being. 2017;12(sup2): 1379338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wright R, John L, Ellenbogen S, Offord DR, Duku EK, Rowe W. Effect of a structured arts program on the psychosocial functioning of youth from low-income communities: findings from a Canadian longitudinal study. J Early Adolesc. 2006;26(2):186–205. [Google Scholar]
- 43. Posner JK, Vandell DL. After-school activities and the development of low-income urban children: a longitudinal study. Dev Psychol. 1999;35(3):868–879. [DOI] [PubMed] [Google Scholar]
- 44. Little P, Wimer C, Weiss HB.. After School Programs in the 21st Century: Their Potential and What it Takes to Achieve it. Issues and Opportunities in Out-of-School Time Evaluation, Brief No. 10. Cambridge, MA: Harvard Family Research Project; 1–12; 2008. [Google Scholar]
- 45. Larson RW, Verma S. How children and adolescents spend time across the world: work, play, and developmental opportunities. Psychol Bull. 1999;125(6):701–736. [DOI] [PubMed] [Google Scholar]
- 46. Blair C, Raver CC. Child development in the context of adversity: experiential canalization of brain and behavior. Am Psychol. 2012;67(4):309–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Power TJ. Promoting Children’s Health: Integrating School, Family, and Community. New York: Guilford Press; 2003. [Google Scholar]
- 48. Catalano RF, Berglund ML, Ryan JA, Lonczak HS, Hawkins JD. Positive youth development in the United States: research findings on evaluations of positive youth development programs. Ann Am Acad Pol Soc Sci. 2004;7(1), 98–124. [Google Scholar]
- 49. Bouffard SM, Caronongan P, Little P, Dearing E, Simpkins SD. Demographic differences in patterns of youth out-of-school time activity participation. J Youth Dev. 2006;1(1):24–40. [Google Scholar]
- 50. Endresen IM, Olweus D. Participation in power sports and antisocial involvement in preadolescent and adolescent boys. J Child Psychol Psychiatry. 2005;46(5):468–478. [DOI] [PubMed] [Google Scholar]