Abstract
Background/Aims
Despite the wide use of acupuncture for the management of visceral pain and the growing interest in the pathophysiology of visceral pain, there is no conclusive elucidation of the mechanisms behind the effects of acupuncture on visceral pain. This systematic review aims to provide an integrative understanding of the treatment mechanism of acupuncture for visceral pain.
Methods
Electronic and hand searches were conducted to identify studies that involved visceral pain and acupuncture.
Results
We retrieved 192 articles, out of which 46 studies were included in our review. The results of our review demonstrated that visceral pain behaviors were significantly alleviated in response to acupuncture treatment in groups treated with this intervention compared to in sham acupuncture or no-treatment groups. Changes in the concentrations of β-endorphin, epinephrine, cortisol, and prostaglandin E2 in plasma, the levels of c-Fos, substance P, corticotropin-releasing hormone, P2X3, acetylcholinesterase (AchE), N-methyl-D-aspartate (NMDA) receptors, and serotonin in the gut/spinal cord, and the neuronal activity of the thalamus were associated with acupuncture treatment in visceral pain.
Conclusions
Acupuncture reduced visceral pain behavior and induced significant changes in neuronal activity as well as in the levels of pain/inflammation-related cytokines and neurotransmitters in the brain-gut axis. Further researches on the thalamus and on a standard animal model are warranted to improve our knowledge on the mechanism of acupuncture that facilitates visceral pain modulation.
1. Introduction
Visceral pain, i.e., pain originating from the thoracic, abdominal, or pelvic regions, is a noticeable symptom associated with various clinical conditions [1, 2]. Visceral pain has different characteristics compared to somatic pain. The former is diffusely localized, not evoked by entire viscera, and rarely linked to actual injuries. Although there has been growing interest in the mechanisms and factors that contribute to the pathogenesis of visceral pain, many researches are still more focused on somatic pain [3]. To date, several underlying causes of visceral pain have been proposed, e.g., visceral hypersensitivity due to sensitized visceral nociceptors/afferent fibers, impairments of the brain-gut axis, referred hyperalgesia from viscerosomatic convergence in the spinal cord and central nervous system (CNS), infections, psychological and genetic factors, and hormonal changes [1, 3, 4]. Moreover, a major advance in the understanding of the central mechanisms and the gut environment (e.g., microbiota) of humans has suggested that the brain-gut axis plays a crucial role in visceral nociception in terms of neuronal/chemical signaling between the brain and the gastrointestinal tract [5, 6].
Acupuncture has been used to treat various pain disorders, including visceral pain, and has shown considerable effects on pain relief with only rare cases of adverse events. Many studies have explored the treatment mechanism of acupuncture for pain relief in general, and it is reported that acupuncture alleviates pain mainly by regulating the levels of endogenous opioids, serotonin, and norepinephrine and by inhibiting visceral nociceptors, inflammatory cytokines, and CNS activation [7–9]. Furthermore, acupuncture can decrease visceral sensitivity [10], activate the enteric nervous system (ENS) [11], and modulate the brain-gut axis [12]. However, the treatment mechanism behind the effects of acupuncture on visceral pain is still unclear [4, 9], partially due to the lack of a systematic approach that encompasses a wide range of evidence from basic and clinical researches to analyze this aspect.
In this review, we aimed to provide an integrative understanding of the mechanisms behind the effects of acupuncture therapy on visceral pain in both human and animal subjects, and we suggest directions that can be adopted for future research.
2. Methods
2.1. Search Strategy
We searched through electronic records in PubMed, EMBASE, MEDLINE, and the Cochrane Library using the keywords “visceral,” “pain,” “hyperalgesia,” “algesia,” “acupuncture,” “electroacupuncture,” and “acupoint.” The search terms and strategies were modified for each individual database (Table 1). Hand searching was performed by screening the reference lists of articles that met our inclusion criteria. The literature search was completed in September 2017, and our search strategy was in compliance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines for systematic reviews.
Table 1.
Search terms used in each database.
| Database | Search terms |
|---|---|
| PUBMED | (acupuncture [MeSH Terms] OR acupuncture [All Fields] OR acupoint [All Fields] OR electroacupuncture [MeSH Terms] OR electroacupuncture [All Fields]) AND (“visceral pain” [MeSH Terms] OR “visceral pain” [All Fields] OR (visceral [All Fields] AND (pain [All Fields] OR pain [MeSH Term])) OR (visceral [All Fields] AND (hyperalgesia [All Fields] OR hyperalgesia [MeSH Terms]))) |
| EMBASE | visceral AND (“pain”/exp OR pain OR “hyperalgesia”/exp OR hyperalgesia OR algesia) AND (“acupuncture”/exp OR acupuncture OR “electroacupuncture”/exp OR electroacupuncture OR acupoint) |
| MEDLINE | (visceral and (pain or hyperalgesia or algesia) and (acupuncture or electroacupuncture or acupoint)).mp. |
| Cochrane Library | visceral AND (pain OR hyperalgesia OR algesia) AND (acupuncture OR electroacupuncture OR acupoint) |
2.2. Study Selection
Search results were screened based on the titles and abstracts before full text assessments. We included original studies that investigated the therapeutic effects and/or the mechanisms of acupuncture on visceral pain. Both animal and human studies written in English or Chinese were included. In this review, we considered manual acupuncture (MA), electroacupuncture (EA), transcutaneous electrical nerve stimulation on acupoints (acu-TENS), pharmacopuncture (injection of herbal medicine into acupoints, e.g., sweet bee venom), and laser acupuncture (LA) techniques as the different types of acupuncture.
2.3. Risk of Bias Assessment in the Human Studies
Concerning the studies on human subjects, we evaluated the risk of bias associated with each of them using either the revised Cochrane risk of bias tool for randomized trials (RoB 2.0 [13]) or the Risk Of Bias In Nonrandomized Studies (ROBINS-I [14]) based on each study design, with a focus on the pain-related outcomes. More details on the assessments are described in the footnotes of supplementary Tables 1 and 2.
3. Results
3.1. Search Results
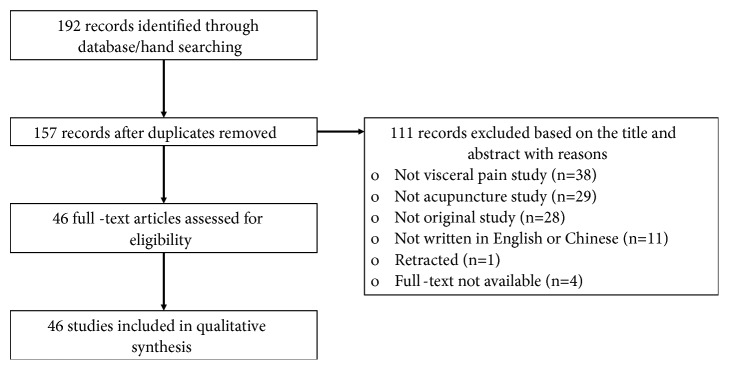
Our search strategy resulted in the retrieval of 192 articles in total. Following this, in addition to removing the duplicates (n=35), 111 studies were excluded based on their titles and abstracts. Among the excluded studies, 67 studies were unrelated to visceral pain or acupuncture, 28 studies were not original, and 11 studies were written in languages other than English or Chinese. Further, full texts corresponding to four studies, each published before 1990, could not be obtained, and one study was retracted. Ultimately, 46 articles were included in this review (Figure 1).
Figure 1.
Flow diagram of article inclusion.
3.2. Visceral Pain Studies on Humans
3.2.1. Visceral Pain Patients and Healthy Participants
There were seven studies with human subjects. Two studies included irritable bowel syndrome (IBS) patients [15, 16], and one study involved primary dysmenorrhea [17] and another study involved chronic pancreatitis patients [18]. Further, a study by Kotani et al. [19] investigated postoperative visceral pain in patients who underwent upper or lower abdominal surgeries [18], and two studies involved healthy participants [20, 21] (Table 2).
Table 2.
Overview of visceral pain studies on humans.
| Author (year) |
Participants group:n(f)/ mean age |
Acupuncture groups | Control groups | Outcomes | Results | ||
|---|---|---|---|---|---|---|---|
| Acupuncture | acupoints number, duration |
Control | acupoints number, duration |
||||
| (1) Thomas et al. (1995) [17] | Primary dysmenorrhea Acu: 17(17)/30.4 Con: 12(12)/27.8 |
(a) MA (b) EA (2Hz) (c) EA (100Hz) (d) Periosteal stimulation (e) acu-TENS (2Hz) (f) acu-TENS (100Hz) |
(a), (b), (c), (d): BL32, CV4, SP6, 9 (e), (f): Spinous processes Thoracic 10-Lumbar 1 2, 20min |
(g) Sham TENS (ns) | Spinous processes Thoracic 10-Lumbar 1 2, 20min |
(1) Blood loss (2) Vomiting (3) Work hours lost (4) Tablet intake (5) Subjective assessment (6) Total pain |
Within group (4), (5), (6) (a), (c), (d) improved (5), (6) (b) improved (4), (5), (6) (e) improved |
| (2) Kotani et al. (2001) [19] | (1) Upper abdominal surgery (A) 50(21)/52 (C) 48(18)/55 (2) Lower abdominal surgery (B) 39(12)/55 (D) 38(13)/55 |
(A) Patient 1 +MA (B) Patient 2 +MA |
(A) BL18, 19, 20, 21, 22, 23, 24 (B) BL20, 21, 22, 23, 24, 25, 26 1, 4 days |
(C) Patient 1+sham MA (ni) (D) Patient 2+sham MA (ni) |
(C) BL18, 19, 20, 21, 22, 23, 24 (D) BL20, 21, 22, 23, 24, 25, 26 1, 4 days |
(1) Incisional, visceral pain (2) Drowsiness (3) Pruritus (4) Nausea/Vomiting (5) Adequacy of pain treatment (6) Morphine intake (7) Adrenal hormone |
Within group (1) (A), (C) improved (6) (A), (B), (C), (D) decreased Between groups (1), (4), (6), (7) (epinephrine, cortisol) (A)<(C), (B)<(D) |
| (3) Xing et al. (2004) [16] | IBS +rectal distention 7(6)/44 |
(a) acu-TENS (5Hz, 250ms) | (a) ST36, PC6 1, - |
(b) TENS (5Hz, 250ms) | (b) non-acupoint 1, - |
(1) Rectal tone (2) Rectal compliance (3) Rectal perception of gas, pain, desire to defecate |
Within group (1) (A), (B) decreased (3) (A) decreased Between groups (3) (A)<(B) |
| (4) Chu et al. (2012) [15] | IBS +rectal distention (A) 15(7)/42.3 (B) 15(8)/44.2 |
(A) EA (10Hz, 0.5ms, 60v) | (A) ST36, 37, SP6 2, 30min |
(B) Sham EA (ns) | (B) ST36, 37, SP6 2, 30min |
(1) fMRI-rectal distention (2) fMRI-A or B +rectal distention (3) fMRI-rectal distention after (2) (4) fMRI-A or B (5) Rectal sensation |
Within group (1) (A), (B): ACC, pgCC, PFC, TH, INS, cerebellum, Temp (A): (1)<(2) pgCC, ACC, PFC, SC, INS, Temp (1)<(3) PFC, SC, Temp (3)<(2) ACC, PFC, TH, INS, Temp (B): (2)>(1) ACC, PFC, SC (3)>(1) PFC, Temp, cerebellum (2)>(3) Temp (3)>(2) PFC Between groups (A)>(B): (2)>(1) in TH, INS Correlation between (5) and brain activation in hypothalamus, TH, INS |
| (5) Leung et al. (2013) [20] | Healthy +rectal distention (A) 20(12)/53.4 (B) 20(12)/53.9 |
(A) acu-TENS (2Hz, 0.2ms) | (A) LI4, PC6, ST36 1, 45min |
(B) Sham TENS (ns) | (B) LI4, PC6, ST36 1, 45min |
(1) Tolerance to rectal sensation (2) Rectal distention pressure (3) Beta-endorphin |
Between groups (1), (2), (3) (B)<(A) |
| (6) Juel et al. (2016) [21] | Healthy +rectal distention 15(8)/27.6 |
(a) MA | (a) CV4, 6, 7, 9, 10, 12, ST25, 26, 37, LI4 +non-acupoints 1, 30min |
(b) Sham MA (ni) | (b) ST37, LI4 1, 30min |
(1) Rectal distention volume (2) Rectal pain (3) EEG |
Within groups (1) (A), (B) increased |
| (7) Juel et al. (2017) [18] | Chronic pancreatitis 15(7)/61.8 |
(a) MA | (a) CV4, 6, 9, 10, 12, ST25, ST36, SP6, 8, 9, 15+non-acupoints 1, - |
(b) Sham MA (ni) | (b) CV4, 6, 9, 10, 12, ST25, ST36, SP6, 8, 9, 15+non-acupoints 1, - |
(1) Reduced pain score (2) EEG |
Between groups (1) (B)<(A) |
Group written in lowercase letters (e.g., (a), (b), and (c)): different treatments in the same population, unless stated otherwise; Group written in capital letters (e.g., (A), (B), and (C)): different treatments in different population
Acu: acupuncture group; ACC: anterior cingulate cortex; BL: Bladder Meridian; Con: control group; CV: Conception Vessel Meridian; EA: electro-acupuncture; EEG: electroencephalography; f: female; fMRI: functional magnetic resonance imaging; IBS: irritable bowel syndrome; INS: insula; LI: Large Intestine Meridian; MA: manual acupuncture; n: number; ni: not inserted; ns: not stimulated; PC: Pericardium Meridian; PFC: prefrontal cortex; pgCC: perigenual cingulate cortex; SC: somatosensory cortex; SP: Spleen Meridian; ST: Stomach Meridian; Temp: temporal lobes; TH: thalamus; (acu-)TENS: Transcutaneous electrical nerve stimulation (on acupoints); min: minutes; ms: milliseconds; v: volts.
3.2.2. Details of Acupuncture Interventions
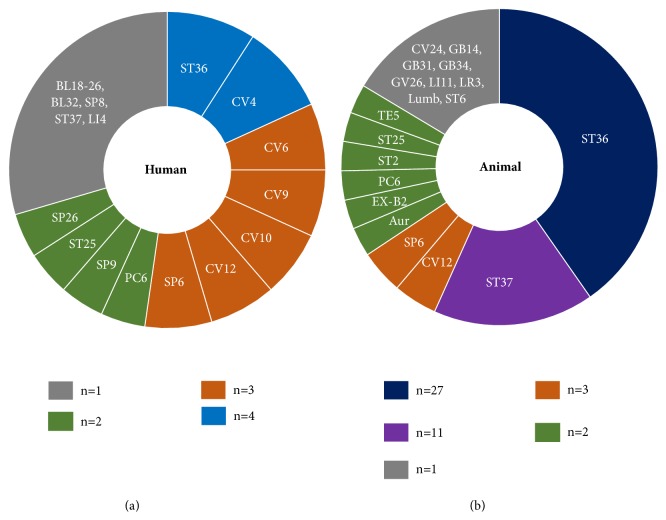
Among the seven studies conducted on humans, the various types of acupuncture techniques that were used are as follows: MA in four studies [17–19, 21], acu-TENS in three studies [16, 17, 20], and EA in two studies [15, 17]. Most of these studies described the stimulation method that was used, the intensity (frequency, voltage, and amperage), and the locations of acupoints. The acupoints that were used in the human studies are summarized in Figure 2(a).
Figure 2.
Frequency distribution of acupuncture points in the human and animal studies on visceral pain. Acupuncture points on Stomach Meridian (ST) and Conception Vessel Meridian (CV) are most frequently selected for visceral pain. Aur: auricular acupoints, Lumb: lumbar acupuncture points, n: number of studies reporting the acupuncture points, BL: Bladder Meridian, GB: Gallbladder Meridian, LI: Large Intestine Meridian, LR: Liver Meridian, PC: Pericardium Meridian, SP: Spleen Meridian, and TE: Triple Energizer Meridian.
3.2.3. Outcomes and Results
(1) Pain Behavioral Outcomes. In human studies, improvements in the pain behavioral outcomes have been consistently observed after acupuncture treatment. Acupuncture treatment showed significantly greater analgesic effects based on subjective pain ratings than sham acupuncture [16, 18, 19], and the maximum tolerable rectal sensation and distention pressure in IBS patients were significantly increased by acu-TENS compared to sham TENS [20] (Tables 2 and 5).
Table 5.
Summary of significant results from the included studies.
| Outcomes | Within acupuncture group (baseline vs post-treatment) |
vs. sham acupuncture group | vs. no treatment group | |
|---|---|---|---|---|
| Behavioral | Human | Intake of analgesics ↓ [17, 19] | Analgesic effect ↑ [16, 18, 19] | |
| Animal | Pain score ↓ Pain threshold ↑ [45, 48] | Pain threshold ↑ [32] | Pain score/behavior ↓ [46, 59] Pain threshold ↑ [29] |
|
| Abdominal withdrawal reflex ↓ [32, 41] | Abdominal withdrawal reflex ↓ [34, 38] | Abdominal withdrawal reflex ↓ [25–27, 33, 38, 39, 42] | ||
| Abdominal muscle activity ↓ [31, 56] | Abdominal muscle activity ↓ [10, 29, 34, 37] | Abdominal muscle activity ↓ [23, 25, 43] | ||
| Writhing response ↓ [50] | Writhing response ↓ [22] | |||
|
| ||||
| Metabolic | Human |
β-endorphin ↑ [20] Adrenal hormones ↓ [19] |
||
| Animal |
β-endorphin ↑ [59] Serotonin/5-HT 3 receptor ↓ [27] |
|||
|
| ||||
| Gut | Animal | c-Fos ↓ [29] | Serotonin ↓ 5-HT4 receptor ↑ [27] Serotonin transporter ↑ [26] c-Fos ↓ p38 ↓ [59] AchE ↓ Leu-enkephalin ↑ [46] Substance P ↓ [46, 59] CRH ↓ [38] P2X3 ↓ [39] |
|
|
| ||||
| Spinal cord | Animal | Neural activity in wide dynamic range neurons ↑ [44, 47]/ ↓ [44] | Serotonin and c-Fos in superficial dorsal horn ↓ [29] | Metabolic rate of glucose in thoracic dorsal horns ↓/lumbar dorsal horns ↑ [48] Neural activity in wide dynamic range neurons ↓ [44] Neural activity in spinal dorsal horn ↓ [24] Action potential in dorsal root ganglion ↓ [10] c-Fos in spinal dorsal horn ↓ [55] P38 in spinal dorsal horn↓ [59] NR2B in spinal dorsal horn, central canal region ↓ [42] CRH ↓ [38] P2X3 ↓ [39] |
|
| ||||
| Brain/brain stem | Human | Perigenual cingulate/prefrontal cortex, temporal lobes, insula, somatosensory cortex ↑ [15] | Thalamus, insula ↑ [15] | |
| Animal | Neural activity in subnucleus reticularis dorsalis ↑ [36] Discharge frequency of thalamus ↑ [40] Activity of thalamus ↓ [54] Pain inhibitory neurons ↑, pain excitation neurons ↓ in ventral posterolateral nucleus (thalamus) [49] Homovanillic acid in the fourth ventricle ↑ [57] |
Neuronal response to colorectal distention in thalamus ↑ [28] Serotonin and c-Fos in dorsal raphe nucleus ↓ [29] |
Glucose metabolic rate in ventral periaqueductal gray, nucleus centralis superior ↓/ periaqueductal gray, gigantocellular reticular nucleus ↑ [48] c-Fos, glial fibrillary acidic protein in medulla ↓ [46] c-Fos in nucleus tractus solitarii ↓ [56] in paratrigeminal nucleus ↑ [23] NMDA receptor 1 in rostral ventromedial medulla ↓ [32] CRH in hypothalamus ↓ [38] P2X3 receptor in prefrontal and anterior cingulated cortex ↓ [39] Homovanillic acid in the fourth ventricle ↑ [57] β-endorphin in hypothalamus ↑ [22, 45] Substance P in hypothalamus ↑ [45] |
|
AChE: acetylcholinesterase; CRH: corticotropin-releasing hormone; NMDA: N-methyl-D-aspartate; NR2B: N-methyl-D-aspartate receptor subunit NR2B; 5-HT: 5-hydroxytryptamine receptor; P2X3: P2X purinoceptor 3.
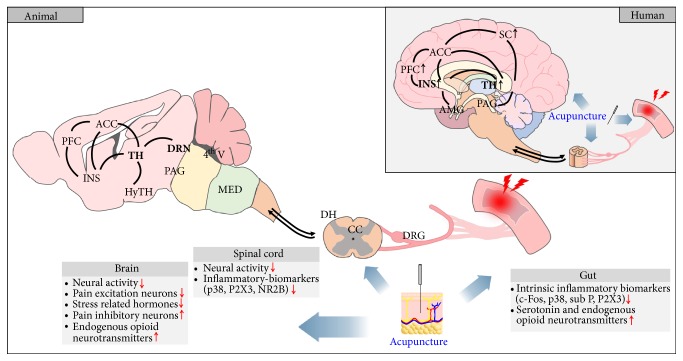
(2) Metabolic Outcomes. In human studies, the secretion of β-endorphin increased after acu-TENS [20], and the levels of adrenal hormones [19] and serum prostaglandin E2 (PGE2) [22] were decreased after MA. The plasma levels of β-endorphin were increased after EA [23] (Tables 2 and 5, Figure 3).
Figure 3.
Schematic illustration of functional and metabolic changes (peptides, proteins, and mRNA) of the brain-gut axis by acupuncture in visceral pain studies. In human, acupuncture consistently enhanced the functional activity in the thalamus and insula, the core brain regions of pain processing. In animal, a great variety of metabolic changes have been reported as well as functional neural activities, demonstrating that acupuncture induces a wide range of changes through the brain-gut axis in visceral pain. ACC: anterior cingulate cortex; AMG: amygdala; CC: central canal; DH: dorsal horn; DRG: dorsal root ganglion; DRN: dorsal raphe nucleus; HyTH: hypothalamus; INS: insula; MED: medulla; NR2B: N-methyl-D-aspartate receptor subunit; PAG: periaqueductal gray; PFC: prefrontal cortex; P2X3: P2X purinoceptor 3; SC: somatosensory cortex; sub P: substance P; TH: thalamus; 4th V: fourth ventricle.
(3) Brain and Brain Stem. Functional magnetic resonance imaging (fMRI) and electroencephalography (EEG) were used to measure neuronal activity in IBS patients [15] and healthy participants [18, 21]. The fMRI results showed significant increases in the brain activity in the thalamus and insula in the EA group compared to in the sham EA group [15], and there were no significant differences observed in the EEG data between the groups [18, 21] (Tables 2 and 5, Figure 3).
3.2.4. Risk of Bias in the Human Studies
There were three randomized parallel-group trials [15, 19, 20] and two randomized cross-over trials [18, 21] included in our review. One study reported results from two different groups (acupuncture and acu-TENS), and within each group, the assignment of the different interventions to the patients was randomized [17]. Therefore, we treated this study as two randomized cross-over studies and assessed the risk of bias associated with each group separately. Lastly, one study was a nonrandomized trial. The results of the assessments of each domain's risk of bias and the overall risk of bias are presented in Supplementary Tables 1 and 2 for the randomized and nonrandomized studies, respectively.
Out of the seven studies, three studies were classified as having low overall risks of bias. Further, two randomized studies [17, 20] were considered as having high risks of bias due to concerns regarding possible selective reporting. Moreover, there were some concerns regarding three randomized studies [17, 18, 21] with regard to randomization domains because they lacked information regarding either their random sequence generation or their allocation concealment; therefore, we labeled these studies as “some concerns.” Lastly, there were some concerns regarding missing data associated with two studies because they did not provide clear indications on whether the results that were summarized in the texts or figures were from all the study participants.
3.3. Visceral Pain Studies on Animals
3.3.1. Visceral Pain Models
We found 39 studies that examined various visceral pain models in animals. Thirty-one studies used rats [10, 23–51], and the remaining used cats [52–54], mice [22, 55, 56], rabbit [57], or dog [58]. To induce visceral pain, mechanical stimulation by colorectal/rectal/gastric distention was most commonly used (n=19) [10, 24, 25, 28, 29, 32, 33, 35–41, 44, 45, 47, 51, 58]. Other methods included splanchnic nerve stimulation [48, 52–54, 57], acetic acid injections [22, 23, 31, 55, 56] (n=5, respectively), somatic and visceral noxious stimuli [49], formalin injection [23], and antimony potassium tartrate injection [50] (Tables 3 and 4).
Table 3.
Visceral hypersensitivity models in animal studies (visceral hypersensitivity and CRD models).
| Author (year) |
Model (animal, gender, number) |
Acupuncture groups | Control groups | Outcomes | Results | ||
|---|---|---|---|---|---|---|---|
| Acupuncture | acupoints number, duration |
Control | acupoints number, duration |
||||
| (1) Cui et al. (2005) [25] |
Visceral hypersensitivity+CRD (SD rat, m, various) | (A) Model+EA (4/100Hz, 1mA) | (A) ST36, 37 7, 30min |
(B) Control (C) Model (D) Model+Sham EA (ns) |
(A) ST36, 37 7, 30min |
(1) AWR (2) Activity of rectus abdominis |
Between groups (1), (2) (A)<(C), (B)<(C) |
| (2) Tian et al. (2006) [26] |
(1) Colorectal irritation-induced visceral hypersensitivity (SD rat, m, 6/group) (2) Model 1+stress |
(A) Model 1+EA (2Hz, 0.3mA) (B) Model 2+EA (2Hz, 0.3mA) |
(A), (B) ST36, SP6 1, 30min |
(C) Control (D) Model 1 (E) Model 2 |
- | (1) AWR (2) Pain threshold pressure (3) Fecal pellet (4) 5-HT4a receptor in colon (5) Serotonin transporter in colon |
Between groups (1) (A), (C)<(D) (2) (D)<(A), (C) (3) (B), (C), (D)<(E) (4), (5) (B)<(A), (C) (5) (D)<(C) |
| (3) Liu et al. (2009) [27] |
Visceral hypersensitivity (SD rat, m, 8/group) |
(A) Model+EA (2/100Hz, 0.2–0.6ms, 1mA) | (A) ST25, ST37 7, 20min |
(B) Control (C) Model |
- | (1) AWR (2) Concentration of 5-HT (3) Concentration of 5-HT3R (4) Concentration of 5-HT4R |
Between groups (1), (2) (A), (B)<(C) (4) (C)<(A), (B) |
| (4) Xu et al. (2009) [10] |
Visceral hypersensitivity +CRD (SD rat, m, 6-25/group total 74) | (A) Model+EA (2/100Hz, 0.1ms, 1mA) (B) Model+EA+SAL (same as above) |
(A), (B) ST36 5, 40min |
(C) Control (D) Model (E) Model +Sham EA (ns) (F) Model+EA+NAL |
(E), (F) ST36 5, 40min |
(1) VMR (2) Membrane potential of DRG neuron (3) Rheobase of DRG neuron (4) Action potential of DRG neuron |
Within group (1) (D): increased (1) (A), (B): decreased after treatment (effect blocked in (F)) Between groups (2) (A)<(E), (C)<(D) (3) (D)<(C), (E)<(A) (4) (A), (C)<(D) |
| (5) Wu et al. (2010) [29] |
Visceral hypersensitivity +CRD (SD rat, m, 8/group) | (A) Model+EA (10Hz, 0.18ms, ~3mA) | (A) ST36 3, 20min |
(B) Control (C) Model+Sham EA (ns) |
(B) ST36 3, 20min |
(1) Pain threshold to CRD (2) VMR (3) 5-HT in colon, spinal cord, brainstem (4) c-Fos in colon, spinal cord, brainstem |
Between groups (1) (C)<(A), (B) (2), (3), (4) (A), (B)<(C) (except (3) in colon) (B)<(A) (in 40, 60, 80mmHg) |
| (6) Qi et al. (2012) [32] |
Visceral hypersensitivity +CRD (SD rat, m, 8/group) | (A) Model+EA (5/100Hz) | (A) ST36, 37 4, 30min |
(B) Control (C) Model (D) Model+sham EA (ns) |
(D) ST36, 37 4, 30min |
(1) Pain threshold pressure (2) AWR (3) c-Fos in RVM (4) N-methyl-D-aspartate receptor 1 in RVM |
Within group (2) (A): decreased after treatment Between groups (1) (C)<(A), (B) (2) (B)<(C) (3) (A)<(C) (4) (A), (B)<(C) |
| (7) Qi et al. (2012) [33] |
Visceral hypersensitivity +CRD (SD rat, m, 8/group) | (A) Model+EA (5/100Hz) | (A) ST36, 37 4, 30min |
(B) Control (C) Model (D) Model+sham EA (ns) |
(D) ST36, 37 4, 30min |
(1) AWR (2) c-Fos in spinal cord |
Between groups (1), (2) (A), (B)<(C) |
| (8) Zhou et al. (2012) [34] |
Stress-induced visceral hypersensitivity (SD rat, m, 5-8/group total 94) | (A) Model+EA (2/100Hz, 0.1ms, 1mA) | (A) ST36 1, 30min |
(B) Model (C) Control+ Sham EA (ns) (D) Control+EA (E) Model+Sham EA (F) Model+EA (G) Model+EA+SAL (H) Model+EA+NAL (I) Model+EA+NAL methiodide |
(C)-(E), (H)-(J) ST36 (F) BL43 1, 30min |
(1) VMR (2) AWR (3) Distention pressure threshold |
Within group (1), (2) (B): increased (vs baseline) (3) (B): decreased (vs baseline) Between groups (1) (A)<(E), (G)<(I) (40, 60, 80mmHg) (2) (A), (C)<(E) (D)<(E) (60, 80mmHg) (G)<(H) |
| (9) Weng et al. (2015) [39] |
Visceral hypersensitivity +CRD (SD rat, m, 8/group) | (A) Model+EA (2/100Hz, 2mA) | (A) ST25, 37 7, 20min |
(B) Control (C) Model |
- | (1) AWR (2) P2X3 receptor in colonic, DRG, spinal cord, PFC, ACC |
Between groups (1), (2) (A), (B)<(C) |
| (10) Qi et al. (2016) [41] |
Visceral hypersensitivity+CRD (SD rat, m, various/group total 184) | (A) Model+EA (2Hz, 1-3mA) (B) Model+EA (100Hz, 1-3mA) (C) Model+EA (2/100Hz, 1-3mA) |
(A)-(F) ST36, 37 1, 10min |
(D) Model+EA (2Hz, 1-3mA)+NAL (E) Model+EA (100Hz, 1-3mA)+NAL (F) Model+EA (2/100Hz, 1-3mA)+NAL (G) Model+sham EA (ns) (H) Control |
(D)-(G) ST36, 37 1, 10min |
(1) AWR (2) Activity of rectus abdominis |
Within group (1), (2) (A)-(C), (E), (F): increased after CRD, decreased after treatment (D), (G): increased after CRD |
| (11) Liu et al. (2017) [42] |
Visceral hypersensitivity (SD rat, m, 8/group) | (A) Model+EA (5/25Hz, 1mA) | (A) ST36, 37 4, 30min |
(B) Control (C) Model (D) Model+sham EA (ns) |
(C) ST36, 37 4, 30min |
(1) AWR (2) NR2B in spinal cord |
Between groups (1) (A)<(C) (2) (A), (B)<(C), (D) |
| (12) Zhou et al. (2017) [43] |
Visceral hypersensitivity +restraint stress (SD rat, m, 16/8) | (a), (b) Model+EA (100Hz, 1mA) | (a), (b) ST36 (a) 1, 90min (b) 1, 30min |
(C) Control (d) Model (e) Model+sham EA (ns) (f) Model+propranolol (g) Model+phentolamine (h) Model+SAL |
(d) ST36 1, 30min |
(1) Activity of acromiotrapezius (2) ECG |
Within group (2) (d): LF/HF increased after restraint stress Between groups (1) during gastric distention: (C), (a), (b)<(d); (f), (g)<(h) (2) LF/HF, LF: (a)<(d) |
Group written in lowercase letters (e.g., (a), (b), and (c)): different treatments in the same population, unless stated otherwise. Group written in capital letters (e.g., (A), (B), and (C)): different treatments in different population.
ACC: anterior cingulate cortex; AWR: abdominal withdrawal reflex; BL: Bladder Meridian; CRD: colorectal distention; DRG: dorsal root ganglion; EA: electro-acupuncture; ECG: Electrocardiography; f: female; HF: high frequency heart rate variability; LF: low frequency heart rate variability; m:male; mA: milliampere; min: minutes; ms: milliseconds; NR2B: N-methyl-D-aspartate receptor subunit NR2B; NAL: naloxone; ns: not stimulated; PFC: prefrontal cortex; RVM: rostral ventromedia medulla; SAL: saline; SD: Sprague Dawley; ST: Stomach Meridian; VMR: visceral motor response (reflex); 5-HT: 5-hydroxytryptamine (serotonin).
Table 4.
Visceral hypersensitivity models in animal studies (other models).
| Author (year) |
Model (animal, gender, number) |
Acupuncture groups | Control groups | Outcomes | Results | ||
|---|---|---|---|---|---|---|---|
| Acupuncture | Acupoints number, duration |
Control | Acupoints number, duration |
||||
| (1) Du et al. (1976) [52] | Splanchnic nerve stimulation (cat, -,-) | (A) Model+EA (25/70/100Hz) | (A) GB31, 34, LI11, TE5 - |
- | - | (1) VSR | Within group (1) (A): inhibited |
| (2) Zhang et al. (1989) [53] | Splanchnic nerve stimulation (cat, -, total 35) | (A) Model+EA (5Hz) | (A) PC6 1,3-5min |
(B) Model+Morphine (C) Model+EA+NAL |
(C) PC6 1, 3-5min |
(1) C-CEPs (2) A-CEPs |
Within group (1) (A), (B): reduced amplitudes (2) (A), (B): reduced amplitude of late component |
| (3) Guoxi (1991) [54] | Splanchnic nerve stimulation (cat, m, total 219) | (A) Model+EA | (A) ST36 - |
- | - | (1) Electrical activities in thalamus | Within group (1) (A): inhibited in 45 out of 48 neurons |
| (4) Shu et al. (1994) [48] | Splanchnic nerve stimulation (Wistar rat, m, 3/4/4) | (A) Model+EA | (A) ST36, SP6 - |
(B) Control (C) Model |
- | (1) Pain threshold (2) Glucose metabolic rate |
Within group (1) (A): increase after treatment Between groups (2) (A)<(C): TDH, LC, ventral PAG, CPC, HL, Hippo, CP, NRD, NCS, TPV, ACC, accumbens, NSL, SC (C)<(A): LDH, NRM, NRG, PAG (B)<(C): NRM, PGL, LC, NRG, HA, CCGM |
| (5) Cai et al. (1994) [57] | Splanchnic nerve stimulation (rabbit, m/f, 8/4/6/6/7/9/6/6) | (A) Model+EA (25Hz)+SAL | (A) EX-B2 (T12,L1,L2) 1, 30min |
(B) Model+SAL (C) Model+ MCP (D) Model+EA (25Hz)+MCP (E) Model+EA+MCP+SAL (F) Model+EA+MCP+APO (G) Model+EA+MCP+SKF38393 (H) Model+EA+MCP+LY171555 |
(D)-(H) EX-B2 1, 30min |
(1) Pain threshold (2) DA in CSF (3) DOPAC in CSF (4) HVA in CSF |
Within group (1) (A), (C), (D), (F): elevated compared to baseline (4) (A), (C): elevated compared to baseline Between groups (1) (A), (C)<(D); (B)<(C); (F), (G), (H)<(E) (4) (A),(C)>(B) |
| (6) Kwon et al. (2001) [56] | Acetic acid injection (ICR mice, m, 10-20/group) | (A) Model+BV (B) Model+BV+NAL (C) Model+BV+Yo |
(A) CV12 1, - |
(D) Model+BV (E) Model+SAL |
(D) non-acupoint 1, - |
(1) Abdominal stretches (2) c-Fos in spinal cord, NTS |
Between groups (1) (A), (D)<(E) (2) (A)<(E) |
| (7) Yu et al. (2008) [55] |
Acetic acid injection (mice, m/f, 12/group) | (A) WT Model+MA (B) Connexin 43 gene knockout HT Model+MA |
(A),(B) CV12, ST36 1, 30min |
(C) WT control (D) HT control (E) WT model (F) HT model |
- - |
(1) c-Fos in the spinal dorsal horn | Between groups (1) (A)<(E), (A)<(B) |
| (8) Yu et al. (2008) [22] |
Acetic acid injection (mice, m/f, 18/group) | (A) Model+WT MA (B) Connexin 43 gene knockout HT ++Model+MA |
(A),(B) CV12, ST36 1, 30min |
(C) WT control (D) HT control (E) WT model (F) HT model |
- - |
(1) Latency of writhing response (2) Number of writhing response (3) β-endorphin in hypothalamus (4) Plasma PGE2 |
Between groups (1), (3) (A)>(E), (A)>(B) (2), (4) (A)<(E), (A)<(B) |
| (9) Liu et al. (2010) [23] | Acetic acid injection (SD rat, m/f, 6/group) | (A) Model+EA (2/20Hz) (B) Model+EA+Snake venom (C) Modal+EA+SAL |
(A)-(C) ST2 1, 20 min |
(D) Control (E) Model (F) Model+EA+ION transection |
(F) ST2 1, 20 min |
(1) Abdominal muscular contractions (2) c-Fos expression in the NTS (3) c-Fos expression in the PTN |
Between groups (1), (2) (A),(E)>(D); (A),(B),(C)<(E), (A)<(F) (3) (A),(B),(C)>(E), (A),(B),(C)>(F) |
| (10) Liu et al. (2011) [31] | Acetic acid injection (SD rat, -, -) | (A) Model+EA (2/20Hz, 1.0mA) (B) Model+EA (2/20Hz, 2.0mA) (C) Model+ EA (2/20Hz, 4.5mA) (D) EA (2/20Hz) (E)-(G) Model+EA (2/20Hz) |
(A)-(E) ST2 (F) GB14 (G) ST6 1, 20min |
(H) Control (I) Model (J) Model+Sham EA (ns) (K) Model+EA (2/20Hz) |
(J) ST2 (K) non-acupoint 1, 20min |
(1) c-Fos (2) Abdominal contractions |
Within group (1) (D): in the NTS, CPTN, PTN, postrema, DMN of the vagus, RF (blocked by infraorbital nerves transaction pretreatment in PTN) (1) (B), (C), (E), (G), (K): inhibited in NTS (1) (B)-(E), (G), (K): increased in PTN (1), (2) (E): infraorbital nerves transaction and capsaicin pretreatment inhibited the effect of EA on reduced (1) and (2) Between groups (2) (D), (E), (G), (H), (K)<(I) (B), (C)<(A), (I), (K) |
| (11) Gong et al. (1992) [50] |
Antimonium potassium tartrate injection (Wistar rat, m/f, 15/10/7/-/12/8/9/8/6/6/10/8/15/15) | (A) Model+EA (45/12.5Hz) (B) Model+EA (45/12.5Hz) +electrical stimulation of PVN |
GV26, CV24 1, 20min |
(C) Control (D) Model (E) Model+Sham EA (ns) (F) Model+EA+sham stimulation of PVN (G) Model+EA+lesion of PVN (H) Model+EA+sham lesion of PVN (I) Model+EA+vasopressin antagonist (J) Model+EA+SAL (K) Model+EA+vasopressin antiserum (L) Model+EA+normal serum (M) Model+EA+vasopressin antagonist (N) Model+EA+SAL |
(E)-(N) GV26, CV24 1, 20min |
(1) Writhing response | Between groups (1) (A)<(E), (B)<(F), (G)>(H), (I)>(J), (K)>(L) |
| (12) Xu et al. (2010) [59] | Formalin injection (SD rat, m, 8/group) | (A) EA (20Hz, ~1mA) (B) Model+EA (20Hz, ~1mA) |
(A), (B) EX-B2 (L3, 6) 1, 20min |
(C) Control (D) Model |
- | (1) Visceral pain behavior (2) p38 in colon, spinal dorsal horn (3) c-Fos in colon, spinal dorsal horn (4) Plasma β-endorphin (5) SP in colon |
Between groups (1) (B)<(D) (2), (3), (5) (B), (C)<(D) (4) (C)<(D)<(B) |
| (13) Rong et al. (2005) [44] |
CRD (SD rat, m, total 67) | (A) Model+non receptive field MA (2-3Hz) (B) Model+receptive field MA |
(A) ST36 (contr) (B) ST36 (ips) 1, 30s |
(C) Model (D) Model+non receptive field pinch (E) Model+ receptive field pinch (F) Model+hot water on tail (non receptive filed) (G) Model+ non receptive field MA+acute freeze of spinal cord (H) Model+acute freeze of spinal cord |
(G) ST36 (contralateral) 1, 30s |
(1) Electrical activities of spinal dorsal horn WDR neurons of L1-L3 | Within groups (1) (A), (D): decreased (B), (G), (H): increased Between groups (1) (A),(D)<(C); (A)<(G) |
| (14) Rong et al. (2005) [24] |
CRD (SD rat, -, 17/17/9/15/9) | (A), (B) Model+MA (2Hz) | (A) ST36 (contr) (B) ST36 (ips) 1, 30s |
(C) Pinch (contr) (D) Pinch (ips) (E) Model |
- | (1) Electrical activities in spinal dorsal horn | Between groups (1) (A), (C)<(E) ((A)<(E) effect blocked after spinalization) |
| (15) Zhang et al. (2009) [28] | CRD (SD rat, m, 58) | (a), (b) Model+EA (2Hz, 1mA) | (a) ST36 (contr) (b) ST36 (ips) 1, 320s |
(c) Model (d) Model+EA (2Hz, 1mA, 0.5ms) (e) Model+EA (100Hz, 1mA, 0.5ms) |
(c)-(e) center of receptive field 1, 320s |
(1) Electrical activities in thalamus | Between groups (1) (d), (e)<(c) (e)<(d) (d)<(a), (b) |
| (16) Chen et al. (2010) [51] | CRD (Wistar rat, m, 9/group) | (A) Model+EA (B) Model+EA (C) Model+EA (2/15Hz, 2mA) |
(A) ST36 (B) PC6 (C) LR3 1, 15min |
(D) Control (E) Model+Sham EA (non-acupoint, 2/15Hz, 2mA) |
(E) non-acupoint 1, 15min |
(1) MAP (2) HR (3) HRV HF (4) LF (5) LF/HF |
Within group (2) (A), (B) decreased Between groups (1) (A),(B)<(C),(D),(E) (4) (A),(B),(C)<(D) (5) (A),(B)<(D) |
| (17) Liu et al. (2014) [35] | CRD (SD rat, m, 62) | (a)-(c) Model+EA (10Hz, 2mA) | (a) ST36 (b) PC6 (c) Auricular acupoint (heart) 1, 30s |
- | - | (1) Electrical activities in NTS | Within group (1) (a), (b), (c): reduced in 5-10 neurons and increased in 2 neurons among 21 excited neurons by CRD reversed in 9-15 neurons among 24 inhibited neurons by CRD |
| (18) Yu et al. (2014) [36] | CRD (SD rat, m, 10-11/group) | (a) Model+EA (15Hz, 1.5mA) (b) Model+EA (15Hz, 6mA) (c) Model+EA (15Hz, 4mA) |
(a)-(c) ST36, 37 2, 30s |
(d) Model | - | (1) Electrical activities of wide dynamic range neurons (2) Electrical activities of SRD neurons |
Within group (1) (a), (b): increased after treatment and CRD (d): increased (2) (c), (d): significant responses (a), (b): increased after CRD |
| (19) Li et al. (2014) [37] | CRD (SD rat, f, 8/7/7/7) | (A) Model+auricular EA (25Hz, 0.8mA) | (A) Auricular acupoints (stomach, small intestine) 1, 30min |
(B) Control (C) Model (D) Model+sham EA |
(D) no vagal innervation points 1, 30min |
(1) VMR (2) mRNA of 5-HT1a receptor in colon (3) mRNA of 5-HT1a receptor in raphe nuclei |
Within group (1) (C): increased Between groups (1) (B)<(A), (C), (D) (1), (2) (A)<(C) (3) (A)<(C), (D) |
| (20) Yu et al. (2014) [47] | CRD (SD rat, m, 22) | (a) preEA+Model+EA (15Hz, 1mA) (b) preEA+Model+EA (15Hz, 4mA) (c) preEA+Model+EA (15Hz, 7mA) (d) preEA+Model+EA (15Hz, 10mA) |
(a)-(d) ST36 (ips) 2, 30s |
- | - - |
(1) Electrical activities of WDR in lumbar spinal cord | Within group (1) (a), (b), (c), (d): increased |
| (21) Liu et al. (2015) [38] | CRD (SD rat, m, 8/group) | (A) Model+EA (2/100Hz) | (A) ST37 7, 20min |
(B) Control (C) Model (D) Model+sham EA (ns) |
(D) ST37 7, 20min |
(1) AWR (2) CRH in colon (3) CRH in spinal cord, hypothalamus (4) mRNA of CRH in colon, spinal cord, hypothalamus |
Between groups (1) (A), (B)<(C); (A)<(D) (2) (A), (B), (D)<(C) (3) (A), (B)<(C),(D) (except (A)<(D) in the spinal cord) (4) (A), (B)<(C); (B)<(D)<(C) (only in hypothalamus) |
| (22) Rong et al. (2015) [40] | CRD (SD rat, m, 26) | (a) Model+EA (20Hz) | (A) ST36, 37 2, 30s |
(b) Model | - | (1) Discharge frequency of VPL neurons in thalamus | Within group (1) (a): increased after CRD (b): increased |
| (23) Iwa et al. (2005) [58] |
Rectal distension (Dog, f 4, 6/group) | (A) Model+EA (10Hz) | (A) ST36 1, 30min |
(B) Model+EA (C) Model+EA+NAL (D) Model+EA+NAL methiodide |
(B) BL21 (C), (D) ST36 1, 30min |
(1) Arterial blood pressure |
Within group (1) (A), (D): decreased after treatment |
| (24) Lin et al. (2009) [45] | Gastric distension (SD rat, m, 10/group) | (A) Model+EA (2Hz, 1-3mA) (B) Model+EA (100Hz, 1-3mA) |
(A),(B) ST36 7, 30min |
(C) Control (D) Model (E) Sham model |
- - |
(1) Pain score (2) β-endorphin in hypothalamus (3) SP in hypothalamus |
Within group (1) (A), (B) decreased Between groups (1) (B)>(A)>(D)>(C),(E) (2),(3) (A)>(B)>(D)>(C),(E) |
| (25) Sun et al. (1991) [49] | Somatic and visceral noxious stimuli (Wistar rat, m/f, 23/28/-/16) | (A) Model+EA (6v, 8Hz) | (A) ST36 1, 15min |
(B) Model (C) Model+Morphine (D) Model+Morphine+NAL |
- - |
(1) Discharge of PEN in VPN (2) Discharge of PIN in VPN |
Within group (1) (A): reduced (2) (A): enhanced |
| (26) Lorenzini et al. (2010) [30] | Cystitis (SD rat, m, total 48) | (A) Cystitis+PWL | (A)-(F) ST36, TE5 Various |
(B) Cystitis | - | (1) Urinary bladder weight, mucosal erosion, ulceration, edema, petechial hemorrhages, thickness of bladder wall (2) Visceral pain behavior |
Within group (1), (2) (A), (B): increased |
| (27) Yang et al. (2010) [46] | Visceral traction (SD rat, m, 10/group) | (A) Model+ LA (650nm, 10mW) | (A) ST36 1, 30min |
(B) Sham model (C) Model (D) Model+Moxa |
(D) ST36 1, 30min |
(1) Pain score (2) Systolic pressure (3) AChE (4) SP (5) LEK (6) Positive index of c-Fos protein (7) Positive index of GFAP |
Between groups (1), (3) (A),(B),(D)<(C) (2) (A),(B)<(C) (4) (B)<(A)<(D)<(C) (5) (A)>(B),(C),(D) (6), (7) (B)<(A),(D)<(C) |
Group written in lowercase letters (e.g., (a), (b), and (c)): different treatments in the same population, unless stated otherwise. Group written in capital letters (e.g., (A), (B), and (C)): different treatments in different population.
ACC: anterior cingulate cortex; A-CEPs: cortical evoked potentials of A-fibers; AChE: acetylcholinesterase; APO: apomorphine; AWR: Abdominal withdrawal reflex; BL: Bladder Meridian; BV: bee venom; C-CEPs: cortical evoked potentials of C-fibers; CCGM: centralis corpus geniculatum medialis; contr: contralateral; CP: caudate putamen; CPTN: caudal spinal trigeminal nucleus; CRD: colorectal distension; CRH: corticotropin-releasing hormone; CSF: cerebrospinal fluid; CV: Conception Vessel Meridian; DA: dopamine; DMN: dorsal motor nucleus; DOPAC: dopaceticacid; EA: electro-acupuncture; f: female; GB: Gall Bladder Meridian; GFAP: glial fibrillary acidic protein; GV: Governing Vessel Meridian; HA: hypothalamic arcuatus; HF: high frequency heart rate variability; Hippo: hippocampus; HL: habenulae lateralis; HR: heart rate; HRV: heart rate variability; HT: heterozygote; HVA: homovanillic acid; ION: infraorbital nerve; ips: ipsilateral; IT: intrathecal injection; L: lumbar vertebrae; LA: laser acupuncture; LC: locus coeruleus; LDH: lumbar dorsal horns; LEK: leu-enkephalin; LF: low frequency heart rate variability; LI: Large Intestine Meridian; LR: Liver Meridian; m:male; MA: manual acupuncture; mA: milliampere; MAP: mean arterial pressure; MCP: metoclopramide; min: minutes; Moxa: moxibustion; mRNA: messenger ribonucleic acid; ms: milliseconds; NAL: naloxone; NCS: nucleus centralis superior; NRD: nucleus raphe dorsalis; NRG: nucleus reticular gigantocellularis; NRM: nucleus raphe magnus; ns: not stimulated; NSL: nucleus septal lateralis; NTS: nucleus tractus solitarii; PAG: periaqueductal gray; PC: Pericardium Meridian; CPC: centromedian-parafascicula; PEN: pain-excitation neurons; PGE2: prostaglandin E2; PGL: paragigantocellularis lateralis, PIN: pain-inhibitory neurons; PTN: paratrigeminal nucleus; PVN: paraventricular nucleus; PWL: pulsed wave laser; RF: reticular formation; SAL: saline; s: seconds; SC: somatosensory cortex; SD: Sprague Dawley; SP: substance P; SRD: subnucleus reticularis dorsalis; ST: Stomach Meridian; T: thoracic vertebrae; TDH: thoracic dorsal horns; TE: Triple Energizer Meridian; TPV: thalamic posterior ventralis; VMR: visceral motor response (reflex); VPL: ventralis posterior lateralis; VPN: ventral posterolateral nucleus; VSR: viscerosomatic reflex discharges; WDR: wide dynamic range; WT: wild type; Yo: yohimbine; 5-HT: 5-hydroxytryptamine receptor.
3.3.2. Details of Acupuncture Interventions
Further, concerning the animal studies, EA was the intervention that was used in most of them [10, 23, 25–29, 31–43, 45, 47–54, 57, 58] (n=32), and the others involved MA [22, 24, 44, 55], LA [30, 46], or pharmacopuncture techniques using bee venom [56] or snake venom [23]. The acupoints that were used in the animal studies are summarized in Figure 2(b).
3.3.3. Outcomes and Results
(1) Behavioral Outcomes. In the animal studies, the abdominal withdrawal reflex [25–27, 32–34, 38, 39, 41, 42], abdominal muscle activities, writhing responses in the abdomen and leg, and other pain-related behaviors significantly decreased after administering EA [29, 45, 48, 50] (Tables 3–5).
(2) Metabolic Outcomes. Liu et al. found that EA treatment applied at the ST25 and ST37 points reduced the concentrations of 5-hydroxytryptamine (5-HT) when compared to the concentrations observed in the no-treatment visceral hypersensitivity group [27]. Xu et al. also showed increased β-endorphin levels in the EA treatment group compared to in the no-treatment formalin injection model [59] (Figure 3).
(3) Gut. The concentration levels of serotonin-related factors, hormones, neurotransmitters, and other molecular signaling factors in the colon were observed in the animals before and after acupuncture. The expression levels of serotonin and c-Fos dropped significantly after EA treatment [26, 29]. The expression levels of serotonin transporter (additional water avoidance stress model) [26], c-Fos [23], p38 [23], substance P [23, 46], corticotropin-releasing hormone (CRH) [38], P2X3 receptor [39], acetylcholinesterase (AchE) [46], and the serotonin concentration [27] were significantly lowered after EA. The expression levels of the serotonin transporter (colorectal irritation model) [26], 5-HT4 receptor [27], and leu-enkephalin [46] significantly increased after EA and LA (Tables 3–5, Figure 3).
(4) Spinal Cord. In the spinal cords of the studied animals, neuronal activities, glucose metabolic rates, hormones, serotonin-related factors, and pain-related molecules were observed before and after acupuncture. The glucose metabolic rates were significantly decreased in the thoracic dorsal horns and increased in the lumbar dorsal horns and in the periaqueductal gray matter after EA [48]. In the lumbosacral spinal cord, the expression levels of serotonin and c-Fos decreased significantly after EA compared to after sham EA [29]. The c-Fos expression levels also decreased in various regions of the spinal cord after EA [23, 31–33] and MA [55]. The neuronal activity of the dorsal root ganglion significantly decreased after EA [10] and that of the spinal dorsal horn significantly decreased after MA [24]. The expression levels of p38 in the spinal dorsal horn [40], CRH [38], P2X3 receptor [39], and the NR2B subunit of the N-methyl-D-aspartate (NMDA) receptor [42] decreased further after EA (Tables 3–5, Figure 3).
(5) Brain and Brain Stem. In the animal studies, the glucose metabolic rates, the levels of serotonin-related neurotransmitters, hormones, and neuronal activity along with the levels of molecular signaling associated with this activity were measured. After EA, the glucose metabolic rates significantly decreased in many regions, e.g., in the thalamus, anterior cingulate cortex (ACC), nucleus accumbens, and somatosensory cortex, and they increased in the nucleus raphe magnus [48]. A significantly increased thalamic neuronal response to colorectal distention was found after EA (versus nonacupoint EA) [28]. CRH concentrations in the hypothalamus were significantly decreased after EA [38], and β-endorphin levels in the hypothalamus were significantly elevated after MA [22]. β-endorphin and substance P levels in the hypothalamus showed significant increases after EA [45]. The P2X3 receptor expression levels in the prefrontal cortex (PFC) and in the ACC significantly decreased after EA [39] (Tables 3–5, Figure 3).
4. Discussion
To our knowledge, this is the first study to systematically review the mechanisms behind the effects of acupuncture on visceral pain studied in both humans and animals through the brain-gut axis. In the 46 included studies in our review, significant improvements in pain-related behaviors were consistently reported in both humans and animals included in the acupuncture treatment groups compared to those included in the sham acupuncture or no-treatment groups. Increased secretion of β-endorphin and decreased epinephrine, cortisol, and PGE2 levels may be involved in the acupuncture mechanisms at the systemic level that are responsible for the modulation of visceral pain. Acupuncture treatment reduced c-Fos, substance P, CRH, P2X3, AchE, serotonin, and NMDA receptor expression levels and elevated serotonin receptor/transporter and leu-enkephalin expression levels in the gut and spinal cord. Studies reporting on the functional neuronal activity showed that EA increased the activity of the thalamus more than sham EA during colorectal distention. The effects of acupuncture were blocked by spinalization [24], acute freezing of the spinal cord [44], naloxone [10, 41], capsaicin [31], and infraorbital nerve transection [23, 31, 41], indicating the requirements for acupuncture to have an effect. Moreover, it is conceivable that the mechanisms underlying the effects of EA may differ depending on the frequency of EA administrations. Qi et al. [41] reported that the administration of naloxone inhibited the effects of 2 Hz EA but not those of 100 Hz or 2/100 Hz EA (alternate stimulation at 2 Hz and 100 Hz frequencies).
4.1. Plasma
Pain commonly causes hyperactivity of the hypothalamic-pituitary-adrenal system resulting in elevated plasma hormone levels such as those of cortisol, epinephrine, and adrenocorticotropin [60]. In their review, Kotani et al. reported that the increased levels of epinephrine and cortisol in plasma after abdominal surgeries were significantly reduced by MA than by sham acupuncture [19]. Previous studies have also reported that acupuncture attenuated the epinephrine [61] and cortisol [62, 63] levels in plasma. With regard to how EA normalized the increased low-frequency/high-frequency ratio caused due to stress in the functional dyspepsia model [43], the results we have discussed demonstrate the modulatory effects of acupuncture on acute stress caused by visceral pain via sympathetic activity and the hypothalamic-pituitary-adrenal axis.
4.2. Gut
Since visceral pain originates in the gastrointestinal tract and its peripheral regions, changes in the immune and nervous systems and changes in the microbial environment of the gut have been investigated. β-endorphin is an endogenous opioid neuropeptide that has an analgesic effect [64], and PGE2 is a hormone-like substance that participates in a wide range of bodily functions such as muscle activity, blood pressure control, pain sensation, and inflammation [65]. Neurotransmitter substance P, the levels of which decreased after acupuncture [23, 46], is also involved in inflammation and plays an important role in the mechanisms of acupuncture related to pain modulation [66]. Serotonin, another important neurotransmitter in the CNS and gastrointestinal tract, regulates various functions of the digestive tract. Serotonin and its receptors are extensively distributed in the myenteric nerve plexus and participate in the regulation of abnormal symptoms in the GI tract [67, 68]. It has been reported that the levels of serotonin and the activities of various types of its receptors are found to be increased in the intestinal mucosa of visceral pain patients [69]. Serotonin induces and maintains visceral hyperactivity by modulating the activation of the transient receptor potential vanilloid 1 (TRPV1) [70]; thus, serotonin receptor agonists or antagonists have been investigated for the treatment of IBS patients [71, 72]. In our review, three studies reported that serotonin levels were lower in the EA groups compared to in the sham EA [29] or no treatment groups [27] or in the model groups [26] while 5-HT4 receptor and serotonin transporter levels significantly increased after EA treatment in visceral pain models [26, 27] and decreased after EA treatment in visceral pain groups that received additional stress conditions [26]. These results suggest that changes in neuropeptide concentrations may vary depending on the type of visceral pain model and the stress levels and that acupuncture has bidirectional effects on diverse systems in order to modulate pain.
4.3. Spinal Cord
The spinal cord is the first region in which incoming pain signals are transmitted to the central nerves. The spinal cord receives sensory information from the whole body and transmits this information to several regions of the brain that are responsible for processing pain [73]. In this review, the studies reported that the action potential, c-Fos, serotonin, p38, and NMDA receptor levels in the spinal dorsal horn were all significantly decreased after EA [10, 29]. C-Fos is commonly used as a marker to measure neuronal activity [74]; thus, increased c-Fos activation in response to the spinal cord signals represents the excitement of the CNS, similar to the effects of an increased action potential. Serotonin, p38, and NMDA receptors are involved in the development of visceral pain [75] and the central sensitization of visceral pain [76]. In addition, the effects of acupuncture were inhibited by spinalization [24]. These results indicate that the spinal cord plays a critical role in the analgesic mechanism of acupuncture for visceral pain. However, conflicting results among electrical or chemical measurements associated with various nuclei hinder the development of an integrative understanding.
4.4. Brain
A set of brain regions, collectively called the “visceral pain network,” are the core of the perception and modulation of internal and external stimuli in the gut [77, 78]. An fMRI study found that the activities of the thalamus and insula significantly increased during EA treatment compared to during sham EA stimulation when the participants underwent visceral distention [15]. Complementary to fMRI measurements in humans, which could not distinguish between the excitatory and inhibitory neurons, Sun et al. [49] reported that EA significantly reduced the discharge of pain excitation neurons and enhanced the discharge of pain inhibition neurons in the thalamus of rats. This bidirectional influence of acupuncture (to inhibit or enhance neuronal activity) might have led to the inconsistent results in the evaluations of the thalamic activity during/after acupuncture in the animal studies. In other visceral pain network regions, P2X3 receptor activity was decreased more in the PFC and ACC in the EA group (versus no-treatment IBS model group) during colorectal distention [39]. The thalamus receives signals from its periphery and relays them to the hypothalamus, insula, PFC, and motor and somatosensory cortex—the so-called visceral pain network [79–81]. The insula integrates sensory information received from visceral and motor activities with inputs from the limbic system [77, 80]. The thalamus is mainly associated with the first-order processing of sensory information, whereas the PFC, insula, and ACC tend to be associated with the higher-order processing of cognitive evaluation, attention, sensory-motor integration, and affective responses [77]. This observation implies that acupuncture treatment influences higher-level cortical activity along with the primary visceral sensory processing regions.
4.5. Quality Assessment of the Included Studies
We only assessed the quality of the human studies and found that only three studies were classified as having low overall risks of bias while two studies were considered as having high risks of bias. A few assessment tools have been developed for assessing the quality of animal studies, but they are not widely accepted nor validated in the field yet. Moreover, since most of the animal studies included in our review did not report on having employed ways to minimize the risk of bias, such as the blinding of the outcome assessor or randomization methods, we could only assume that they were at high risks of bias.
It is also important to assess the reporting quality of the acupuncture interventions. There are well-known guidelines, the STRICTA guidelines (STandards for Reporting Interventions in Clinical Trials of Acupuncture [82, 83]), for clinical studies that use acupuncture treatment. However, there are no such guidelines that have been designed specifically for reporting acupuncture interventions in animal studies. For these reasons, we evaluated the quality of reporting on acupuncture interventions according to the STRICTA guidelines in a separate paper [84]. To improve our understanding of the underlying mechanisms of acupuncture that are involved in the treatment of visceral pain, studies conducted according to well-validated guidelines with detailed reports on the acupuncture intervention employed are warranted.
4.6. Summary
Based on these results, we found that acupuncture induces analgesic effects on visceral pain via multiple pathways from the peripheral organs (gut) to the CNS (brain). Visceral organs are where visceral pain occurs, and acupuncture directly regulates visceral pain by reducing the levels of intrinsic inflammatory biomarkers and increasing the levels of serotonin and endogenous opioid neurotransmitters. The neural signals induced by acupuncture are also transmitted to the brain through the spinal cord, and it attenuates the peripheral neural activity and concentrations of the inflammatory-biomarkers such as p38, P2X3, and NR2B in the spinal cord. In the brain, acupuncture attenuates the levels of neural activity and pain excitation neurons in the thalamus and reduces stress-related hormone levels in the hypothalamus, which suggests that the neural and hormonal changes in the thalamus and hypothalamus are involved in the pain modulatory effects of acupuncture on visceral pain. Moreover, acupuncture induces an increase in the levels of β-endorphin and pain inhibitory neurons that are also related to pain inhibition.
With this review, we were able to present the broad outline of the acupuncture signal-transduction system from the gut to the CNS, but the acupuncture signaling pathways from the spinal cord to the intestine or the gut-brain signal-transduction system are still unclear. Further experimental studies are needed to elucidate the entire signaling mechanism of acupuncture from the peripheral to the central organs.
5. Conclusion
This review summarizes the findings from previous studies associated with the neural and chemical changes that take place through the brain-gut axis in both humans and animals in order to reveal the underlying mechanisms behind the effects of acupuncture treatment on visceral pain. The results of this review demonstrated significant improvements in visceral pain following acupuncture treatments. However, achieving an integrative understanding of the mechanism of acupuncture on visceral pain remains a long-term endeavor. High heterogeneity among the included studies (various visceral pain conditions and models along with diverse outcome measures and heterogeneous results) and the lack of detailed descriptions outlining the treatment methods also raise concerns.
In future studies, the thalamus and the brain-gut axis could be considered as targets or markers of the visceral pain that is modulated by acupuncture. Furthermore, studies on changes in the levels of neurotransmitters or neuropeptides in the gut and the brain may improve our knowledge of visceral pain modulation by acupuncture treatment.
Acknowledgments
This work was supported only by the Daejeon University Research Grants (2016).
Conflicts of Interest
The authors declared no conflicts of interest.
Authors' Contributions
This review was conceived and designed by Ji-Yeun Park and In-Seon Lee. Ji-Yeun Park and In-Seon Lee developed the search strategy, and In-Seon Lee conducted the database search. Ji-Yeun Park, In-Seon Lee, and Soyeon Cheon assessed studies for inclusion and extracted and analyzed the data. Ji-Yeun Park, In-Seon Lee, and Soyeon Cheon prepared the manuscript draft. All the authors approved the final version of the manuscript for publication. In-Seon Lee is currently supported by the Intramural Research Program of the National Center for Complementary and Integrative Health, National Institutes of Health.
Supplementary Materials
Two supplementary tables reporting the risk of bias of included clinical studies regarding the quality of the included studies. We assessed the risk of bias with RoB 2.0 tool for randomized controlled trials (n=6, supplementary Table 1) and ROBINS-I tool for non-randomized clinical trial (n=1, supplementary Table 2).
References
- 1.Sikandar S., Dickenson A. H. Visceral pain: the ins and outs, the ups and downs. Current Opinion in Supportive and Palliative Care. 2012;6(1):17–26. doi: 10.1097/SPC.0b013e32834f6ec9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cervero F. Pathophysiology of visceral pain. Revista DOR. 2014;15(2):133–138. doi: 10.5935/1806-0013.20140032. [DOI] [Google Scholar]
- 3.Gebhart G. F., Bielefeldt K. Physiology of visceral pain. Comprehensive Physiology. 2016;6(4):1609–1633. doi: 10.1002/cphy.c150049. [DOI] [PubMed] [Google Scholar]
- 4.Zhang F., Wu L., Zhao J., et al. Neurobiological mechanism of acupuncture for relieving visceral pain of gastrointestinal origin. Gastroenterology Research and Practice. 2017;2017:11. doi: 10.1155/2017/5687496.5687496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bonaz B. Visceral sensitivity perturbation integration in the brain-gut axis in functional digestive disorders. Journal of Physiology and Pharmacology. 2003;54 Suppl 4:27–42. [PubMed] [Google Scholar]
- 6.Moloney R. D., Johnson A. C., O'Mahony S. M., Dinan T. G., Greenwood-Van Meerveld B., Cryan J. F. Stress and the microbiota-gut-brain axis in visceral pain: relevance to irritable bowel syndrome. CNS Neuroscience & Therapeutics. 2016;22(2):102–117. doi: 10.1111/cns.12490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takagi J., Yonehara N. Serotonin receptor subtypes involved in modulation of electrical acupuncture. Japanese Journal of Pharmacology. 1998;78(4):511–514. doi: 10.1254/jjp.78.511. [DOI] [PubMed] [Google Scholar]
- 8.Andersson S., Lundeberg T. Acupuncture—from empiricism to science: functional background to acupuncture effects in pain and disease. Medical Hypotheses. 1995;45(3):271–281. doi: 10.1016/0306-9877(95)90117-5. [DOI] [PubMed] [Google Scholar]
- 9.Chen S., Wang S., Rong P., et al. Acupuncture for visceral pain: neural substrates and potential mechanisms. Evidence-Based Complementary and Alternative Medicine. 2014;2014:12. doi: 10.1155/2014/609594.609594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu G. Y., Winston J. H., Chen J. D. Electroacupuncture attenuates visceral hyperalgesia and inhibits the enhanced excitability of colon specific sensory neurons in a rat model of irritable bowel syndrome. Neurogastroenterology & Motility. 2009;21(12):1302–e125. doi: 10.1111/j.1365-2982.2009.01354.x. [DOI] [PubMed] [Google Scholar]
- 11.Hu S., Zhao Z.-K., Liu R., et al. Electroacupuncture activates enteric glial cells and protects the gut barrier in hemorrhaged rats. World Journal of Gastroenterology. 2015;21(5):1468–1478. doi: 10.3748/wjg.v21.i5.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li H., He T., Xu Q., et al. Acupuncture and regulation of gastrointestinal function. World Journal of Gastroenterology. 2015;21(27):8304–8313. doi: 10.3748/wjg.v21.i27.8304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgins J., Sterne J., Savović J., et al. A revised tool for assessing risk of bias in randomized trials. Cochrane Database of Systematic Reviews. 2016;10(Suppl 1):p. CD201601. [Google Scholar]
- 14.Sterne J. A., Hernán M. A., Reeves B. C., et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:p. i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chu W. C. W., Wu J. C. Y., Yew D. T. W., et al. Does acupuncture therapy alter activation of neural pathway for pain perception in irritable bowel syndrome?: a comparative study of true and sham acupuncture using functional magnetic resonance imaging. Journal of Neurogastroenterology and Motility. 2012;18(3):305–316. doi: 10.5056/jnm.2012.18.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xing J., Larive B., Mekhail N., Soffer E. Transcutaneous electrical acustimulation can reduce visceral perception in patients with the irritable bowel syndrome: a pilot study. Alternative Therapies in Health and Medicine. 2004;10(1):38–42. [PubMed] [Google Scholar]
- 17.Thomas M., Lundeberg T., Bjork G., Lundstrom-Lindstedt V. Pain and discomfort in primary dysmenorrhea is reduced by preemptive acupuncture or low frequency TENS. European Journal of Physical Medicine & Rehabilitation. 1995;5(3):71–76. [Google Scholar]
- 18.Juel J., Liguori S., Liguori A., et al. Acupuncture for pain in chronic pancreatitis: a single-blinded randomized crossover trial. Pancreas. 2017;46(2):170–176. doi: 10.1097/MPA.0000000000000749. [DOI] [PubMed] [Google Scholar]
- 19.Kotani N., Hashimoto H., Sato Y., et al. Preoperative intradermal acupuncture reduces postoperative pain, nausea and vomiting, analgesic requirement, and sympathoadrenal responses. Anesthesiology. 2001;95(2):349–356. doi: 10.1097/00000542-200108000-00015. [DOI] [PubMed] [Google Scholar]
- 20.Leung W.-W., Jones A. Y., Ng S. S., Wong C. Y., Lee J. F. Acupuncture transcutaneous electrical nerve stimulation reduces discomfort associated with barostat-induced rectal distension: a randomized-controlled study. World Journal of Gastroenterology. 2013;19(3):381–388. doi: 10.3748/wjg.v19.i3.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Juel J., Liguori S., Liguori A., et al. A new method for sham-controlled acupuncture in experimental visceral pain – a randomized, single-blinded study. Pain Practice. 2016;16(6):669–679. doi: 10.1111/papr.12309. [DOI] [PubMed] [Google Scholar]
- 22.Yu W.-C., Huang G.-Y., Zhang M.-M. Influence of connexin 43 gene knockout on the analgesic effect of acupuncture in visceral pain mice. Acupuncture Research. 2008;33(1):3–6. [PubMed] [Google Scholar]
- 23.Liu J.-H., Fu W.-B., Xu Z.-H., Liao Y., Li X.-R. Effect of transection or pretreatment of the infraorbital nerve with snake venom on the analgesia induced by electroacupuncture of "Sibai" (ST 2) acupoint in visceral pain rats. Acupuncture Research. 2010;35(4):281–286. [PubMed] [Google Scholar]
- 24.Rong P.-J., Zhu B., Huang Q.-F., Gao X.-Y., Ben H., Li Y.-H. Acupuncture inhibition on neuronal activity of spinal dorsal horn induced by noxious colorectal distention in rat. World Journal of Gastroenterology. 2005;11(7):1011–1017. doi: 10.3748/wjg.v11.i7.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cui K. M., Li W. M., Gao X., Chung K., Chung J. M., Wu G. C. Electro-acupuncture relieves chronic visceral hyperalgesia in rats. Neuroscience Letters. 2005;376(1):20–23. doi: 10.1016/j.neulet.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 26.Tian X. Y., Bian Z. X., Hu X. G., Zhang X. J., Liu L., Zhang H. Electro-acupuncture attenuates stress-induced defecation in rats with chronic visceral hypersensitivity via serotonergic pathway. Brain Research. 2006;1088(1):101–108. doi: 10.1016/j.brainres.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 27.Liu H.-R., Wang X.-M., Zhou E.-H., et al. Acupuncture at both ST25 and ST37 improves the pain threshold of chronic visceral hypersensitivity rats. Neurochemical Research. 2009;34(11):1914–1918. doi: 10.1007/s11064-009-9972-1. [DOI] [PubMed] [Google Scholar]
- 28.Zhang J. L., Zhang S. P., Zhang H. Q. Effect of electroacupuncture on thalamic neuronal response to visceral nociception. European Journal of Pain. 2009;13(4):366–372. doi: 10.1016/j.ejpain.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 29.Wu J. C., Ziea E. T., Lao L., et al. Effect of electroacupuncture on visceral hyperalgesia, serotonin and fos expression in an animal model of irritable bowel syndrome. Journal of Neurogastroenterology and Motility. 2010;16(3):306–314. doi: 10.5056/jnm.2010.16.3.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lorenzini L., Giuliani A., Giardino L., Calzà L. Laser acupuncture for acute inflammatory, visceral and neuropathic pain relief: an experimental study in the laboratory rat. Research in Veterinary Science. 2010;88(1):159–165. doi: 10.1016/j.rvsc.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 31.Liu J., Fu W., Yi W., et al. Extrasegmental analgesia of heterotopic electroacupuncture stimulation on visceral pain rats. Brain Research. 2011;1373:160–171. doi: 10.1016/j.brainres.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 32.Qi D.-B., Li W.-M. Effects of electroacupuncture on expression of c-fos protein and N-methyl-D-aspartate receptor 1 in the rostral ventromedial medulla of rats with chronic visceral hyperalgesia. Journal of Chinese Integrative Medicine. 2012;10(4):416–423. doi: 10.3736/jcim20120410. [DOI] [PubMed] [Google Scholar]
- 33.Qi D.-B., Li W.-M. Effects of electroacupuncture on expression of c-fos protein in the spinal dorsal horn of rats with chronic visceral hyperalgesia. Journal of Chinese Integrative Medicine. 2012;10(12):1490–1496. doi: 10.3736/jcim20121224. [DOI] [PubMed] [Google Scholar]
- 34.Zhou Y.-Y., Wanner N. J., Xiao Y., et al. Electroacupuncture alleviates stress-induced visceral hypersensitivity through an opioid system in rats. World Journal of Gastroenterology. 2012;18(48):7201–7211. doi: 10.3748/wjg.v18.i48.7201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu K., Gao X. Y., Li L., et al. Neurons in the nucleus tractus solitarius mediate the acupuncture analgesia in visceral pain rats. Autonomic Neuroscience: Basic and Clinical. 2014;186:91–94. doi: 10.1016/j.autneu.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 36.Yu L.-L., Li L., Rong P.-J., et al. Changes in responses of neurons in spinal and medullary subnucleus reticularis dorsalis to acupoint stimulation in rats with visceral hyperalgesia. Evidence-Based Complementary and Alternative Medicine. 2014;2014:8. doi: 10.1155/2014/768634.768634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li H., Hu S., Zhang J., et al. Effects and mechanisms of auricular electroacupuncture on visceral pain induced by colorectal distension in conscious rats. Acupuncture in Medicine. 2014;32(6):472–477. doi: 10.1136/acupmed-2014-010575. [DOI] [PubMed] [Google Scholar]
- 38.Liu H.-R., Fang X.-Y., Wu H.-G., et al. Effects of electroacupuncture on corticotropin-releasing hormone in rats with chronic visceral hypersensitivity. World Journal of Gastroenterology. 2015;21(23):7181–7190. doi: 10.3748/wjg.v21.i23.7181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weng Z. J., Wu L. Y., Zhou C. L., et al. Effect of electroacupuncture on P2X3 receptor regulation in the peripheral and central nervous systems of rats with visceral pain caused by irritable bowel syndrome. Purinergic Signalling. 2015;11(3):321–329. doi: 10.1007/s11302-015-9447-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rong P.-J., Zhao J.-J., Yu L.-L., et al. Function of nucleus ventralis posterior lateralis thalami in acupoint sensitization phenomena. Evidence-Based Complementary and Alternative Medicine. 2015;2015:6. doi: 10.1155/2015/516851.516851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Qi D., Wu S., Zhang Y., Li W. Electroacupuncture analgesia with different frequencies is mediated via different opioid pathways in acute visceral hyperalgesia rats. Life Sciences. 2016;160:64–71. doi: 10.1016/j.lfs.2016.06.025. [DOI] [PubMed] [Google Scholar]
- 42.Liu H., Zhang Y., Qi D., Li W. Downregulation of the spinal NMDA receptor NR2B subunit during electro-acupuncture relief of chronic visceral hyperalgesia. The Journal of Physiological Sciences. 2017;67(1):197–206. doi: 10.1007/s12576-016-0456-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhou J., Li S., Wang Y., et al. Inhibitory effects and mechanisms of electroacupuncture via chronically implanted electrodes on stress-induced gastric hypersensitivity in rats with neonatal treatment of iodoacetamide. Neuromodulation: Technology at the Neural Interface. 2017;20(8):767–773. doi: 10.1111/ner.12602. [DOI] [PubMed] [Google Scholar]
- 44.Rong P.-J., Zhu B., Huang Q.-F., Gao X.-Y., Ben H., Li Y.-H. Acupuncture inhibiting responses of spinal dorsal dorsal horn neurons induced by noxious dilation rectum and colon. Chinese Acupuncture & Moxibustion. 2005;25(9):645–650. [PubMed] [Google Scholar]
- 45.Lin Y.-P., Peng Y., Yi S.-X., Tang S. Effect of different frequency electroacupuncture on the expression of substance P and beta-endorphin in the hypothalamus in rats with gastric distension-induced pain. Acupuncture Research. 2009;34(4):252–257. [PubMed] [Google Scholar]
- 46.Yang H.-Y., Guo T.-T., Ma Y.-N., Liu T.-Y., Gao M. Effects of 650 nm laser and moxibustion pretreatment on enteric nervous system and medullary visceral zone in rats with visceral traction pain. Chinese Acupuncture & Moxibustion. 2010;30(9):745–751. [PubMed] [Google Scholar]
- 47.Yu L.-L., Li L., Qin Q.-G., Ben H., Rong P.-J., Zhu B. Colorectal nociceptive signal input facilitates impact of acupoint stimulation of "Zusanli" (ST 36) on electrical activities of wide dynamic range neurons in lumbar spinal cord in rats. Acupuncture Research. 2014;39(5):390–395. [PubMed] [Google Scholar]
- 48.Shu J., Li K.-Y., Huang D.-K. The central effect of electro-acupuncture analgesia on visceral pain of rats: a study using the [3H] 2-deoxyglucose method. Acupuncture & Electro-Therapeutics Research. 1994;19(2-3):107–117. doi: 10.3727/036012994816357330. [DOI] [PubMed] [Google Scholar]
- 49.Sun M., Li Y., Zhang J., Bian J. Effects of noxious stimuli on the discharges of pain-excitation neurons and pain-inhibition neurons in the nucleus ventralis posterolalis of thalamus in the rat and a modulating action of electroacupuncture on its electric activities. Acupuncture Research. 1991;16(1):19–22. [PubMed] [Google Scholar]
- 50.Gong S., Yin W.-P., Yin Q.-Z. Involvement of vasopressinergic neurons of paraventricular nucleus in the electroacupuncture-induced inhibition of experimental visceral pain in rats. Acta Physiologica Sinica. 1992;44(5):434–441. [PubMed] [Google Scholar]
- 51.Chen S.-P., Gao Y.-H., Yu X.-C., Liu J.-L. Effects of electroacupuncture of different acupoints on changes of blood pressure and autonomic nerve system after colorectal distension in rats. Acupuncture Research. 2010;35(5):335–341. [PubMed] [Google Scholar]
- 52.Du H. J., Chao Y. F. Localization of central structures involved in descending inhibitory effect of acupuncture on viscero-somatic reflex discharges. SCIENCE CHINA Chemistry. 1976;19(1):137–148. [PubMed] [Google Scholar]
- 53.Zhang J. M., Guo L. N., Chen P. X. The effect of electro-acupuncture of "neiguan" acupoint on cortical potential evoked by stimulating C-fibers of splanchnic nerve. Acupuncture Research. 1989;14(4):410–413. [PubMed] [Google Scholar]
- 54.Guoxi T. The action of the visceronociceptive neurons in the posterior group of thalamic nuclei: possible mechanism of acupuncture analgesia on visceral pain. The Kitasato Archives of Experimental Medicine. 1991;64(1):43–55. [PubMed] [Google Scholar]
- 55.Yu W.-C., Huang G.-Y., Zhang M.-M., Wang W. Effect of connexin 43 knockout on acupuncture-induced down-regulation of c-fos expression in spinal dorsal horn in visceral pain mice. Acupuncture Research. 2008;33(3):179–182. [PubMed] [Google Scholar]
- 56.Kwon Y.-B., Kang M.-S., Han H.-J., Beitz A. J., Lee J.-H. Visceral antinociception produced by bee venom stimulation of the Zhongwan acupuncture point in mice: Role of α2 adrenoceptors. Neuroscience Letters. 2001;308(2):133–137. doi: 10.1016/S0304-3940(01)01989-9. [DOI] [PubMed] [Google Scholar]
- 57.Cai B., Huang X., Wang G., Mo W. Potentiation of electroacupuncture analgesia on visceral pain by metoclopramide and its mechanism. Acupuncture Research. 1994;19(1):66–70, 74. [PubMed] [Google Scholar]
- 58.Iwa M., Strickland C., Nakade Y., Pappas T. N., Takahashi T. Electroacupuncture reduces rectal distension-induced blood pressure changes in conscious dogs. Digestive Diseases and Sciences. 2005;50(7):1264–1270. doi: 10.1007/s10620-005-2770-y. [DOI] [PubMed] [Google Scholar]
- 59.Xu K. D., Liang T., Wang K., Tian D. A. Effect of pre-electroacupuncture on p38 and c-Fos expression in the spinal dorsal horn of rats suffering from visceral pain. Chinese Medical Journal. 2010;123(9):1176–1181. doi: 10.3760/cma.j.issn.0366-6999.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 60.Tennant F. The physiologic effects of pain on the endocrine system. Pain and Therapy. 2013;2(2):75–86. doi: 10.1007/s40122-013-0015-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yang J.-W., Ye Y., Wang X.-R., et al. Acupuncture attenuates renal sympathetic activity and blood pressure via beta-adrenergic receptors in spontaneously hypertensive rats. Neural Plasticity. 2017;2017:9. doi: 10.1155/2017/8696402.8696402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ahsin S., Saleem S., Bhatti A. M., Iles R. K., Aslam M. Clinical and endocrinological changes after electro-acupuncture treatment in patients with osteoarthritis of the knee. PAIN. 2009;147(1–3):60–66. doi: 10.1016/j.pain.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 63.Harbach H., Moll B., Boedeker R., et al. Minimal immunoreactive plasma β-endorphin and decrease of cortisol at standard analgesia or different acupuncture techniques. European Journal of Anaesthesiology. 2007;24(4):370–376. doi: 10.1017/S0265021506001906. [DOI] [PubMed] [Google Scholar]
- 64.Hartwig A. C. Peripheral beta-endorphin and pain modulation. Anesthesia Progress. 1991;38(3):75–78. [PMC free article] [PubMed] [Google Scholar]
- 65.Kawahara K., Hohjoh H., Inazumi T., Tsuchiya S., Sugimoto Y. Prostaglandin E2-induced inflammation: relevance of prostaglandin e receptors. Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 2015;1851(4):414–421. doi: 10.1016/j.bbalip.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 66.Karatay S., Okur S. C., Uzkeser H., Yildirim K., Akcay F. Effects of acupuncture treatment on fibromyalgia symptoms, serotonin, and substance P levels: a randomized sham and placebo-controlled clinical trial. Pain Medicine. 2018;19(3):615–628. doi: 10.1093/pm/pnx263. [DOI] [PubMed] [Google Scholar]
- 67.Huang R., Zhao J., Wu L., et al. Mechanisms underlying the analgesic effect of moxibustion on visceral pain in irritable bowel syndrome: a review. Evidence-Based Complementary and Alternative Medicine. 2014;2014:7. doi: 10.1155/2014/895914.895914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ma X.-P., Hong J., An C.-P., et al. Acupuncture-moxibustion in treating irritable bowel syndrome: how does it work? World Journal of Gastroenterology. 2014;20(20):6044–6054. doi: 10.3748/wjg.v20.i20.6044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kanazawa M., Hongo M., Fukudo S. Visceral hypersensitivity in irritable bowel syndrome. Journal of Gastroenterology and Hepatology. 2011;26 Suppl 3:119–121. doi: 10.1111/j.1440-1746.2011.06640.x. [DOI] [PubMed] [Google Scholar]
- 70.Qin H.-Y., Luo J.-L., Qi S.-D., Xu H.-X., Sung J. J. Y., Bian Z.-X. Visceral hypersensitivity induced by activation of transient receptor potential vanilloid type 1 is mediated through the serotonin pathway in rat colon. European Journal of Pharmacology. 2010;647(1–3):75–83. doi: 10.1016/j.ejphar.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 71.Binienda A., Storr M., Fichna J., Salaga M. Efficacy and safety of serotonin receptor ligands in the treatment of irritable bowel syndrome: a review. Current Drug Targets. 2018;19(15) doi: 10.2174/1389450119666171227225408. [DOI] [PubMed] [Google Scholar]
- 72.Steadman C. J., Talley N. J., Phillips S. F., Zinsmeister A. R. Selective 5-hydroxytryptamine type 3 receptor antagonism with ondansetron as treatment for diarrhea-predominant irritable bowel syndrome: a pilot study. Mayo Clinic Proceedings. 1992;67(8):732–738. doi: 10.1016/s0025-6196(12)60797-6. [DOI] [PubMed] [Google Scholar]
- 73.Todd A. J. Neuronal circuitry for pain processing in the dorsal horn. Nature Reviews Neuroscience. 2010;11(12):823–836. doi: 10.1038/nrn2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bullitt E. Expression of c-fos-like protein as a marker for neuronal activity following noxious stimulation in the rat. Journal of Comparative Neurology. 1990;296(4):517–530. doi: 10.1002/cne.902960402. [DOI] [PubMed] [Google Scholar]
- 75.Kondo T., Sakurai J., Miwa H., Noguchi K. Activation of p38 MAPK through transient receptor potential A1 in a rat model of gastric distension-induced visceral pain. NeuroReport. 2013;24(2):68–72. doi: 10.1097/WNR.0b013e32835c7df2. [DOI] [PubMed] [Google Scholar]
- 76.Luo X.-Q., Cai Q.-Y., Chen Y., et al. Tyrosine phosphorylation of the NR2B subunit of the NMDA receptor in the spinal cord contributes to chronic visceral pain in rats. Brain Research. 2014;1542:167–175. doi: 10.1016/j.brainres.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 77.Moisset X., Bouhassira D., Denis D., Dominique G., Benoit C., Sabaté J.-M. Anatomical connections between brain areas activated during rectal distension in healthy volunteers: a visceral pain network. European Journal of Pain. 2010;14(2):142–148. doi: 10.1016/j.ejpain.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 78.Lelic D., Olesen S. S., Valeriani M., Drewes A. M. Brain source connectivity reveals the visceral pain network. NeuroImage. 2012;60(1):37–46. doi: 10.1016/j.neuroimage.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 79.Aziz Q., Schnitzler A., Enck P. Functional neuroimaging of visceral sensation. Journal of Clinical Neurophysiology. 2000;17(6):604–612. doi: 10.1097/00004691-200011000-00006. [DOI] [PubMed] [Google Scholar]
- 80.Olesen A. E., Farmer A. D., Olesen S. S., Aziz Q., Drewes A. M. Management of chronic visceral pain. Pain Management. 2016;6(5):469–486. doi: 10.2217/pmt-2015-0011. [DOI] [PubMed] [Google Scholar]
- 81.Al-Chaer E. D., Lawand N. B., Westlund K. N., Willis W. D. Visceral nociceptive input into the ventral posterolateral nucleus of the thalamus: a new function for the dorsal column pathway. Journal of Neurophysiology. 1996;76(4):2661–2674. doi: 10.1152/jn.1996.76.4.2661. [DOI] [PubMed] [Google Scholar]
- 82.MacPherson H., White A., Cummings M., Jobst K. A., Rose K., Niemtzow R. C. Standards for reporting interventions in controlled trials of acupuncture: the STRICTA recommendations. The Journal of Alternative and Complementary Medicine. 2002;8(1):85–89. doi: 10.1089/107555302753507212. [DOI] [PubMed] [Google Scholar]
- 83.MacPherson H., Altman D. G., Hammerschlag R., et al. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. Journal of Evidence-Based Medicine. 2010;3(3):140–155. doi: 10.1111/j.1756-5391.2010.01086.x. [DOI] [PubMed] [Google Scholar]
- 84.Lee I.-S., Cheon S., Park J.-Y. A review on reporting quality of acupuncture intervention for visceral pain: assessment with STRICTA. Korean Journal of Acupuncture. 2019;36(1):19–35. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Two supplementary tables reporting the risk of bias of included clinical studies regarding the quality of the included studies. We assessed the risk of bias with RoB 2.0 tool for randomized controlled trials (n=6, supplementary Table 1) and ROBINS-I tool for non-randomized clinical trial (n=1, supplementary Table 2).