Abstract
Transcatheter therapy for partial anomalous pulmonary venous connection with dual drainage is unique and rarely reported. We report a 69-year-old female with recurrent brain abscess and partial anomalous connection of the left upper pulmonary vein with dual drainage to the vertical vein (VV) and left atrium (LA). Transcatheter occlusion of the VV was done using an 18-mm St. Jude Amplatzer Vascular Plug II, thus redirecting the left-sided pulmonary venous drainage to LA. Careful evaluation of partial anomalous pulmonary venous drainage with cross-sectional imaging is essential to allow the delineation of dual connections, enabling a less invasive transcatheter treatment approach.
Keywords: Anomalous pulmonary venous connection, device occlusion, dual drainage
INTRODUCTION
The usual treatment of left-sided partial anomalous pulmonary venous connection (PAPVC) in the presence of a significant left-to-right shunt is surgical repair.[1] Occasionally, the existence of a dual drainage connecting the PAPVC to the left atrium (LA) has been reported.[2,3,4,5,6,7] In such patients, transcatheter therapy may represent an alternative to surgery. We describe a patient where the presence of dual drainage of left-sided pulmonary veins allowed for a transcatheter treatment approach. Our patient was unique in age, indication, and anatomic subtype of partial anomalous pulmonary venous drainage (PAPVD) with additional connection to the LA.
CASE REPORT
A 69-year-old female was referred for cardiology assessment for recurrent cerebellar abscesses. In the past, she had tissue valve replacement for bicuspid aortic valve stenosis. Cardiovascular examination was unremarkable with normal oxygen saturation. Cardiac imaging including echocardiogram and computed tomography (CT) scan showed the left-sided pulmonary veins were draining to the innominate vein through a vertical vein (VV) and additionally to the LA [Figure 1a]. The right heart was significantly enlarged. The brain abscesses were possibly related to paradoxical embolism.
Figure 1.
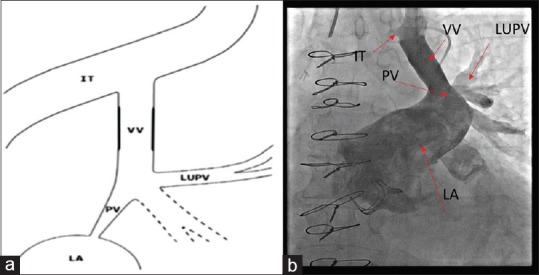
Partial anomalous pulmonary vein connection with dual drainage. (a) Schematic diagram of partial anomalous pulmonary venous connection with dual drainage, (b) Angiogram: Preintervention. VV: Vertical vein, LUPV: Left upper pulmonary vein, LA: Left atrium, IT: Innominate trunk, PV: Pulmonary vein
Cardiac catheterization under general anesthesia with left internal jugular vein access confirmed that all the left-sided pulmonary veins were draining into the VV with additional drainage to LA on angiography [Figure 1b]. Access to the anomalous vein was gained through an 8-Fr sheath and multipurpose diagnostic catheter and then exchanged over an extrastiff exchange wire for a 9-Fr multipurpose guide.
Balloon occlusion of the VV with 34-mm Amplatzer sizing balloon (St Jude Medical, St Paul, MN) above the entry of the pulmonary veins over 10 min showed no change in the mean pressure which remained at 15 mmHg. There was no rise in pressure in the pulmonary vein during balloon occlusion (as measured through transducing the balloon catheter shaft). Subsequently, the VV was occluded using an 18 mm (diameter) × 14 mm (unconstrained length) St. Jude Amplatzer Vascular Plug II. The final position of the device was above the drainage of left-sided pulmonary veins and below the bridging innominate vein without impinging on either structure [Figure 2a]. Postocclusion, the pressure in the VV proximal to the device was a mean of 11 mmHg. The patient recovered uneventfully and was discharged the next day.
Figure 2.
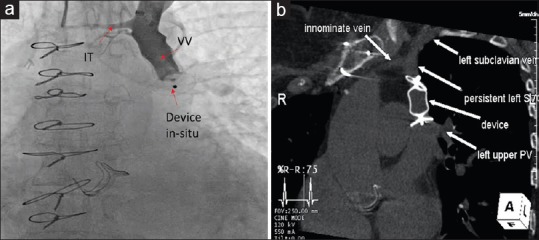
Transcatheter intervention of partial anomalous pulmonary vein connection with dual drainage. (a) Vertical vein angiogram shows Amplatzer Vascular Plug II device in good position with no significant residual flow into the left atrium. (b) Computed tomography scan 1-year postdevice occlusion shows the device in good position and redirecting pulmonary venous flow to the left atrium
At follow-up, 2 years later, the patient remains asymptomatic, with no further embolic events. No systemic desaturation was noted. She has no evidence of right heart dilation on echocardiogram. A repeat CT scan showed the device in satisfactory position above the entry point of the left upper pulmonary vein [Figure 2b], thus redirecting the left-sided pulmonary venous drainage to the LA.
DISCUSSION
PAPVC describes an abnormal connection of one or more, but not all, pulmonary veins, usually to a systemic vein or directly to the right atrium. The connections can be supracardiac (usually the right upper pulmonary vein to superior caval vein or left pulmonary vein to VV and innominate vein), cardiac (to coronary sinus or directly to the right atrium), or infracardiac (to inferior caval vein or hepatic veins).
The VV has also been termed as the levoatrio or levoatrial cardinal vein in some reports. However, the levoatrial cardinal vein is a vein that communicates both with the LA and with the left superior cardinal vein. In other words, this is a left pulmonary vein that has an abnormal persisting anastomosis with the left superior cardinal vein. It is often associated with severe pulmonary venous and left atrial obstruction caused by mitral atresia or severe stenosis. In this hemodynamic situation, the levoatrial cardinal vein helps to decompress the hypertensive pulmonary veins and LA.[8]
The incidence of PAPVC cases with dual drainage is difficult to estimate, especially in VV type, since patients are often asymptomatic and may escape detection. Echocardiographic signs of right ventricular volume overload should raise suspicion, as well as an enlarged superior caval vein. These defects have the same physiological effect as any long-standing left-to-right shunt at atrial level, as they combine drainage of PV to the right side and free drainage of the LA to the right atrium. Moreover, any connection between a systemic vein and the LA may allow paradoxical embolism.[5,9] Two of the previously published patients with a VV type presented with stroke-like symptoms. Although there was no significant left-to-right shunt, transcatheter correction was recommended and successfully performed.[4,7,10]
PAPVC of the left upper lobe can mimic left-sided superior caval vein (LSVC) on cross-sectional imaging, so care is required to make the correct diagnosis. In the former, blood drains cranially through a “VV” into the left innominate vein. Other differentiating imaging features include dilated coronary sinus and LSVC manifesting as two vessels anterior to the left main bronchus on axial imaging, whereas in PAPVD, there will be no aberrant vessel or superior pulmonary vein evident.[11] Absence of an innominate vein is inconsistent with the left upper lobe PAPVC, although the presence of this vessel is not a helpful discriminator.
Transcatheter closure of the abnormal venous connection is certainly the treatment of choice for PAPVC with dual drainage, although successful surgical ligation of the VV has been reported. Interventional catheterization also offers the possibility of performing an occlusion test.[10] Pulmonary vein pressure is monitored during balloon occlusion (transduce balloon shaft) as a marker for unobstructed flow to the LA through the dual connections. The absolute increase in pulmonary venous pressure (in mm Hg) is more informative than a percentage increase in pressure. Closure is avoided if a pulmonary venous pressure rise of ≥10 mmHg was documented.[10] Risks associated with occlusion of the VV type anomalous vein in the absence of adequate alternative drainage could include either a rise in pulmonary venous pressure on that side or central venous pressure should the bridging innominate vein be inadequate.
The St Jude Amplatzer Vascular Plug II is well suited for occluding such venous structures. It can be easily delivered through the left internal jugular vein and deployed just above the anomalous connection.[4,10]
CONCLUSION
“Dual drainage” of the left-sided pulmonary veins to both a VV and the LA made it possible to successfully reroute the anomalous left-sided PAPVC.
Diligent evaluation of partial anomalous left-sided pulmonary venous drainage is essential to delineate dual connections, hence allowing a less invasive transcatheter approach for therapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ward KE, Mullins CE. Anomalous pulmonary venous connections, vein stenosis, and atresia of the common vein. In: Garson A, Bricker JT, Fisher DJ, Neish SR, editors. The Science and Practice of Pediatric Cardiology. Baltimore, Md: Williams and Wilkins; 1998. pp. 1431–61. [Google Scholar]
- 2.Forbess LW, O’Laughlin MP, Harrison JK. Partially anomalous pulmonary venous connection: Demonstration of dual drainage allowing nonsurgical correction. Cathet Cardiovasc Diagn. 1998;44:330–5. doi: 10.1002/(sici)1097-0304(199807)44:3<330::aid-ccd19>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 3.Dähnert I, Riede FT, Kostelka M. Partial anomalous pulmonary venous drainage of the left upper pulmonary vein – Catheter interventional treatment is sometimes possible. Clin Res Cardiol. 2007;96:511–3. doi: 10.1007/s00392-007-0518-8. [DOI] [PubMed] [Google Scholar]
- 4.Gomez J, Soledispa C. Redirection of anomalous venous pulmonary flow to left atrium using a vascular plug II. J Invasive Cardiol. 2012;24:E96–8. [PubMed] [Google Scholar]
- 5.Recto MR, Sadlo H, Sobczyk WL. Rare case of persistent left superior vena cava to left upper pulmonary vein: Pathway for paradoxical embolization and development of transient ischemic attack and subsequent occlusion with an amplatzer vascular plug. J Invasive Cardiol. 2007;19:E313–6. [PubMed] [Google Scholar]
- 6.Kasarala G, Fiore A, Schowengerdt K, Jureidini S. Partial anomalous pulmonary venous return: Transcatheter repair. Pediatr Cardiol. 2011;32:1238–40. doi: 10.1007/s00246-011-0075-9. [DOI] [PubMed] [Google Scholar]
- 7.Kobayashi D, Forbes TJ, Delius RE, Aggarwal S. Amplatzer vascular plug for transcatheter closure of persistent unligated vertical vein after repair of infracardiac total anomalous pulmonary venous connection. Catheter Cardiovasc Interv. 2012;80:192–8. doi: 10.1002/ccd.23497. [DOI] [PubMed] [Google Scholar]
- 8.Cullen EL, Breen JF, Rihal CS, Simari RD, Ammash NM. Levoatriocardinal vein with partial anomalous venous return and a bidirectional shunt. Circulation. 2012;126:e174–7. doi: 10.1161/CIRCULATIONAHA.111.085555. [DOI] [PubMed] [Google Scholar]
- 9.Saremi F, Vojdani E, Vorobiof G, Shavelle D, Wilcox A, Madanipour S, et al. Right to left shunting through communications between the left superior intercostal vein tributaries and the left atrium: A potential cause of paradoxical embolism. Int J Cardiol. 2013;167:2867–74. doi: 10.1016/j.ijcard.2012.07.024. [DOI] [PubMed] [Google Scholar]
- 10.Wilson W, Horlick E, Benson L. Successful transcatheter occlusion of an anomalous pulmonary vein with dual drainage to the left atrium. Catheter Cardiovasc Interv. 2015;85:1212–6. doi: 10.1002/ccd.25734. [DOI] [PubMed] [Google Scholar]
- 11.Dillon EH, Camputaro C. Partial anomalous pulmonary venous drainage of the left upper lobe vs. duplication of the superior vena cava: Distinction based on CT findings. AJR Am J Roentgenol. 1993;160:375–9. doi: 10.2214/ajr.160.2.8424355. [DOI] [PubMed] [Google Scholar]


