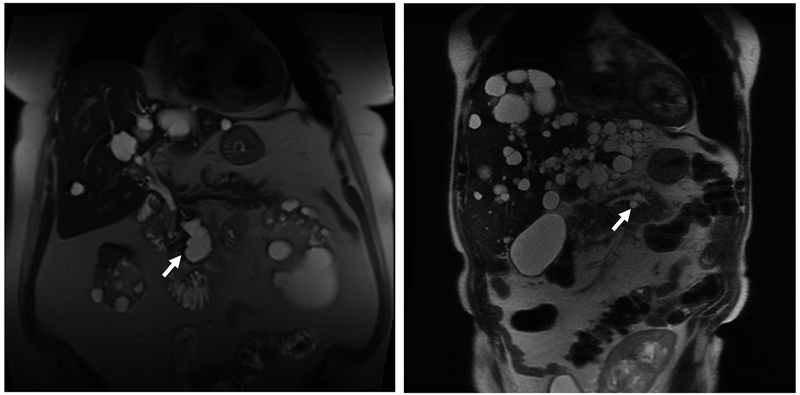
FIGURE 3.
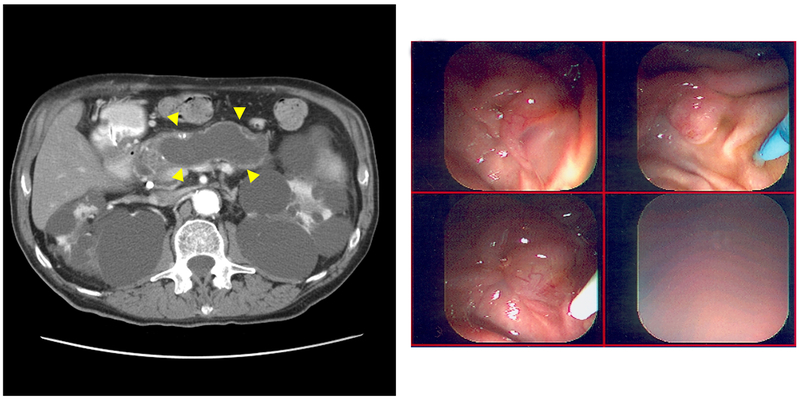
Magnetic Resonance Imaging (MRI) Scans of Branch Duct (BD) Intraductal Papillary Mucinous Neoplasm (IPMN). A, Axial T2-weighted MRI showing a BD-IPMN (arrow) of a 69-year-old woman (case 1) with autosomal dominant polycystic kidney disease (ADPKD). Seven cysts were noted in the head of the pancreas (maximum diameter, 30 mm). The main pancreatic duct (MPD) measured 3 mm. The patient has not had follow-up imaging at this institution to evaluate any increase in size of BD-IPMN. B, Coronal single-shot fast-spin echocardiography (SSFSE) MRI of 58-year-old patient with PKD1 (case 2) with polycystic liver and bilateral nephrectomies with BD-IPMN based on endoscopic ultrasonography showing clear communication (arrow), seen with 3-mm MPD. The patient had 2 pancreatic cystic lesions (maximum diameter, 20 mm) that increased in size over 124 months but has had no indication for surgical intervention to date. C, A 72-year-old man (case 3) with ADPKD diagnosed with MPD-IPMN on presentation with abdominal pain. Abdominal computed tomography shows grossly dilated MPD (arrowheads on sagittal section) and polycystic kidneys. D, On endoscopic retrograde cholangiopancreatography, major and minor papillae were identified easily by the profuse thick mucus coming through widely patent orifices from an irregular and dilated pancreatic duct. The patient declined surgical management and succumbed to bowel obstruction secondary to the mucus at 56 months after diagnosis.