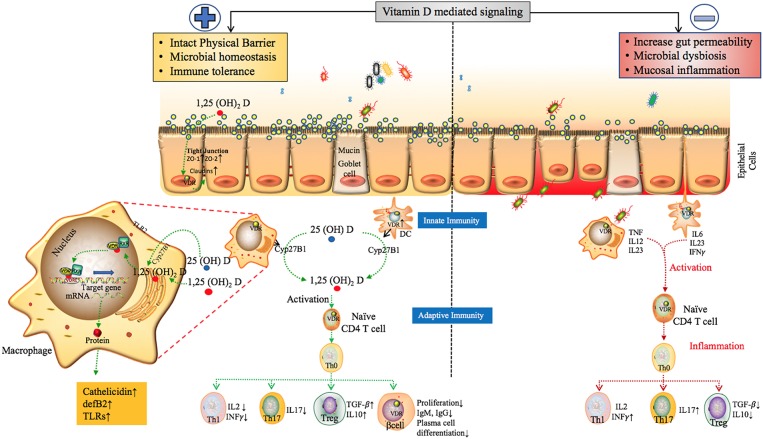
Figure 6.
The proposed role of Vitamin D mediated signaling in epithelial cell barrier function, Gut microbial hemostasis and modulation of Innate and adaptive immune responses. VDR regulates the level of tight junction proteins ZO1, ZO2 via claudin2 and 12 (39, 118) and helps maintain the structural integrity of epithelial barrier. Vitamin D deficiency have also been shown to disrupt gut homeostasis leading to systemic inflammation (119). Effects of Vitamin D on different players of the innate and adaptive immune system. In response to an antigenic challenge, macrophages, dendritic cells, and lymphocytes express the Vitamin D receptor (VDR), thereby becoming targets for the active Vitamin D metabolite, 1,25(OH)2D (120). Macrophages and dendritic cells also express the CYP27B1 that synthesizes 1,25(OH)2D leading to intra and paracrine responses such as stimulates enhancing the phagocytotic responses of macrophages and production of antimicrobial proteins such as cathelicidin (49, 121, 122). Active Vitamin D also modulates adaptive immunity. At the level of the APCs (like DCs), 1,25(OH)2D inhibits the surface expression of MHC-II-complexed antigen. In addition, 1,25(OH)2D directly affects T cell responses, by inhibiting the production of Th1 cytokines (IL-2 and IFN-γ), Th17 cytokines (IL-17 and IL-21), and by stimulating Th2 cytokine production (IL-4) and Treg cell development (123–129). Finally, 1,25(OH)2D blocks plasma-cell differentiation, IgG and IgM production and B-cell proliferation (130). The above factors can trigger inflammatory immune responses such as TNF-α and IFN-γ leading to intestinal permeability and susceptibility to pathogenic infections, microbial dysbiosis and manifestation of immune related inflammatory diseases (19).