Abstract
Objective/Background:
Sleep problems and emotional and behavioral difficulties are highly correlated in community samples of youth and in youth presenting to mental health treatment. However, fewer studies have characterized the associations between sleep and psychopathology symptoms in youth presenting to pediatric sleep clinics. This retrospective, cross-sectional study examined the prevalence of psychopathology symptoms and their associations with sleep disruption in youth presenting to a behavioral sleep medicine clinic.
Participants:
Participants were 373 preschoolers (1.5 to 5 years old) and 300 school age youth (6 to 10 years old) presenting to a pediatric behavioral sleep medicine clinic with a primary insomnia diagnosis.
Methods:
As a part of routine clinical care, parents completed a battery of pre-evaluation measures assessing insomnia severity, sleep disturbance, history of mental health diagnosis, and psychopathology symptoms.
Results:
Both preschool and school age youth had high rates of parent-reported mental health diagnoses (35% and 74%, respectively) and clinically elevated psychopathology symptoms (69% of preschoolers and 77% of school age youth) at initial insomnia evaluation. These symptoms were significantly associated with sleep disruption, with ADHD and affective problems most consistently associated with sleep problems in preschoolers and symptoms of anxiety, affective, and behavioral problems most consistently associated with sleep problems in school age youth.
Conclusions:
Psychopathology symptoms should be regularly assessed in youth presenting to behavioral sleep medicine clinics. Further, the role of psychopathology should be considered in insomnia conceptualization and treatment and, when appropriate, psychopathology symptoms should be targeted in treatment or appropriate referrals should be made.
Keywords: Mental Health, Sleep Disruption, Insomnia Evaluation, Preschool, School Age
The associations between sleep problems and mental health problems in youth have been well established in community samples (Reigstad, Jørgensen, Sund, & Wichstrøm, 2010) and among youth presenting to mental health treatment (Dahl & Harvey, 2007; Ivanenko, Crabtree, Obrien, & Gozal, 2006; Van Dyk, Thompson, & Nelson, 2016). Several studies have examined the prevalence of mental health disorders and symptoms in adults presenting to sleep disorder centers (e.g., Aikens, Vanable, Tadimeti, Caruana-Montaldo, & Mendelson, 1999; Dezee, Hatzigeorgiou, Kristo, & Jackson, 2005) with rates of mental health problems ranging from 22% to 75%. However, few studies have examined mental health symptoms in youth with insomnia and only one study to our knowledge has examined prevalence rates of mental health symptoms in youth specifically presenting to a pediatric sleep clinic (Ivanenko, Barnes, Crabtree, & Gozal, 2004).
In the existing studies examining the relations between mental health and sleep in youth with insomnia, prevalence rates of clinically significant mental health symptoms range from 32% (Velten-Schurian, Hautzinger, Poets, & Schlarb, 2010) to 67% (Ivanenko et al., 2004) with common comorbid disorders including attention-deficit/hyperactivity disorder (ADHD), anxiety, and mood disorders. Preliminary associations between mental health symptoms and severity of sleep problems makes these high prevalence rates particularly concerning for insomnia treatment. In a sample of youth diagnosed with behavioral insomnia, internalizing problems were associated with increased daytime sleepiness and concentration and conduct problems were associated with short sleep duration (Velten-Schurian et al., 2010). In the one study examining mental health symptoms in youth presenting to insomnia treatment, those with a mental health disorder diagnosis were more likely to have parent-reported sleep-onset insomnia. Further, depressive symptoms were positively correlated with sleep onset latency and inversely related to rapid eye movement (REM) sleep latency (Ivanenko et al., 2004).
These studies are useful in their description of mental health symptoms in youth with insomnia and more specifically in youth presenting to sleep treatment. However, research is needed to address several gaps that have implications for evidenced-based assessment and treatment of pediatric insomnia. First, prior studies identified subjects with insomnia based on varying research definitions as opposed to using International Classification of Sleep Disorders diagnostic criteria. Secondly, the limited research in this area used samples that are not representative of the clinical heterogeneity of children that present for insomnia treatment. For example, Ivanenko et al. (2004) excluded children with comorbid sleep disorders such as sleep disordered breathing, abnormal movements during sleep, and/or parasomnias. Accordingly, examining mental health symptoms in youth presenting to insomnia treatment, regardless of comorbidity, is warranted since this represents the heterogeneity that occurs in real-world settings. Including these youth also acknowledges the high comorbidity of organic and behavioral sleep concerns in youth (Byars, Apiwattanasawee, Leejakpai, Tangchityongsiva, & Simakajornboom, 2011; Byars & Simon, 2014; Owens, Opipari, Nobile, & Spirito, 1998). Third, it would be useful to examine the relations between mental health and sleep within specific age groups (e.g., preschool, school age). Youth often present differently to sleep treatment across the developmental spectrum and also may have unique emotional and behavioral concerns. It is possible that certain mental health symptoms are more clearly associated with sleep at varying developmental levels. Specific mental health symptoms or patterns of symptoms that relate to sleep disruption prior to insomnia treatment have yet to be identified, and this may be due in part to limitations of existing research and the need to consider developmental differences.
In sum, by addressing gaps in the extant literature, we may better understand the prevalence and sleep-related correlates of mental health symptoms in youth presenting to insomnia evaluation. This is an important step in considering how mental health symptoms manifest in children with insomnia. Further, determining which symptoms are most consistently related to sleep problems will inform assessment efforts and offer a potential avenue of intervention with the opportunity to target emotional and behavioral problems in addition to insomnia symptoms. The present study aims to build on existing literature by providing an update on the prevalence of mental health symptoms and their associations with sleep disruption, specifically focusing on preschool and school age youth presenting to a behavioral sleep medicine clinic. It was hypothesized that, in general, mental health problems would be highly prevalent and related to measures of insomnia symptoms.
Method
Participants
Participants included preschool (n=373; 1.5–5 years old) and school age (n=300, 6–10 years old) children presenting with their caregiver to an outpatient pediatric behavioral sleep medicine clinic (BSMC) for evaluation between June 2009 to March 2015. All youth were referred to the BSMC based on a primary complaint of sleep disruption. Inclusion criteria included a primary insomnia diagnosis according to International Classification of Sleep Disorders criteria (ICSD; AASM 2005, 2014) and complete data on the Child Behavior Checklist (Achenbach & Rescorla, 2001). Participants were excluded if their primary behavioral sleep medicine diagnosis was not insomnia (i.e., delayed sleep phase disorder, adjustment sleep disorder, parasomnia, rhythmic movement disorder, nocturnal enuresis, idiopathic hypersomnia, and narcolepsy). This excluded relatively few youth (n=18 for preschoolers and n=29 for school age youth). To best represent the heterogeneity of youth presenting to insomnia treatment in “real-world” settings, participants were not excluded if they had a comorbid organic sleep disorder or secondary behavioral sleep medicine diagnosis (e.g., parasomnia). Participants’ insomnia symptoms were not better explained by their comorbid sleep-related diagnoses.
Procedures
Participants were presenting for an evaluation at a BSMC housed within an accredited sleep disorders center located in a tertiary-care pediatric hospital. Patients were either self-referred or referred by a health care provider for primary concerns related to sleep. Of note, only 3.5% of preschoolers and 10.6% of school age youth were referred from a mental health care provider. Based on the referral question and caregiver-reported history obtained through an intake survey, patients referred to the sleep disorders center were triaged to be seen by a board-certified sleep physician in the sleep disorders clinic and/or a licensed psychologist certified in behavioral sleep medicine in the BSMC. For patients referred to the BSMC, a battery of pre-evaluation screening measures were completed by the caregiver as a part of routine clinical care. Pre-evaluation measures were incorporated into the comprehensive evaluation which also included a clinical interview and review of sleep diary (when available). At the initial BSMC evaluation, the purpose of the study was explained and all families were invited to participate. For those agreeing, the primary caregiver provided written informed consent. Ten preschool families and five school age families declined to participate (97% and 98% participation rate, respectively). Characteristics and reasons for decline were not collected from these families. Although consent was prospectively obtained, data was not collected with the specific intent to complete the current study, thus this is a retrospective, cross-sectional study. The overarching goal of the original study was to create a clinic-based data registry whereby data collected as part of standard care could be leveraged for future, unspecific research questions. Study procedures were approved by the hospital’s institutional review board (approval #2010–0001).
Measures
Demographics.
Demographic information (i.e., age, sex, race, and income) was reported by caregivers on a pre-evaluation form.
Sleep Diagnoses and Symptoms.
Sleep disorders were diagnosed following a comprehensive evaluation conducted by a licensed clinical psychologist certified in behavioral sleep medicine. All participants had a primary insomnia diagnosis according the ICSD criteria (AASM, 2005, 2014). Accordingly, behavioral insomnia of childhood was broadly defined as difficulty initiating or maintaining sleep with subsequent daytime impairment (e.g., fatigue, difficulty with concentration or behavior). For youth, this sleep disruption is thought to result from the child’s reliance on a specific stimuli (often parental presence) to initiate or return to sleep after waking (i.e., sleep-onset association type), is characterized by inadequate limit setting by the caregiver at bedtime (i.e., limit-setting type), or is a combination of these two types. Patients were categorized by insomnia subtype according to ICSD-2 nosology. Organic sleep disorders, when present, were diagnosed by a board-certified sleep physician.
Pediatric Insomnia Severity Index (PISI).
The PISI (Byars & Simon, 2014; Byars, Simon, Peugh, & Beebe, 2017) was a primary sleep outcome completed at the initial evaluation session. It is a six question, parent-report measure of insomnia severity that includes difficulty falling asleep, difficulty maintaining sleep, daytime sleepiness, and sleep duration. Parents are asked to think about the past week when answering questions. Scores range from 0 to 30 with higher scores indicating greater severity. The PISI has been shown to be sensitive to change in youth being treated for insomnia and has demonstrated adequate reliability and validity in preliminary studies for youth ages 0 to 10 (Byars & Simon, 2014; Byars et al., 2017).
Child Sleep Habits Questionnaire (CSHQ).
The CSHQ (Owens, Spirito, & McGuinn, 2000) was another primary sleep outcome completed as part of the pre-evaluation assessment. It is a 33-item, parent-report of sleep patterns and problems validated in youth ages 2.5 to 10 years (Lewandowski, Toliver-Sokol, & Palermo, 2011). The CSHQ consists of eight subscales including bedtime resistance, sleep onset delay, sleep duration, sleep anxiety, night wakings, parasomnias, sleep-disordered breathing, and daytime sleepiness. The measure is well-established with strong psychometric properties in youth ages 2.5 to 10 (Lewandowski et al., 2011; Owens et al., 2000).
Given the PISI’s preliminary validation in younger youth and that the CSHQ has not yet been validated in children under age 2.5, we examined correlations of these measures with the CBCL sleep subscale as a preliminary test of convergent validity to support our use of these measures in young children. Both the CSHQ and PISI demonstrated good convergent validity with the CBCL sleep subscale (rs = .60 and .42, respectively).
Emotional and Behavioral Functioning.
As a part of the pre-evaluation clinical history form, parents reported on any mood or behavioral diagnoses previously given to their child by a medical/psychological professional. Parent-reported diagnoses were organized into the following categories: anxiety and related disorders (i.e., anxiety, obsessive compulsive disorder, post-traumatic stress disorder), depression and mood disorders (i.e., depression, mood disorder, bipolar disorder), ADHD, behavior disorders (i.e., oppositional defiant disorder, disruptive behavior disorder, impulse control disorder, intermittent explosive disorder), pervasive developmental disorders (i.e., autism spectrum disorder, Asperger’s disorder), adjustment disorder, and an “other” category including psychotic disorder, Tourette’s disorder, tic disorder, conversion disorder, reactive attachment disorder, and eating disorders.
Child Behavior Checklist (CBCL).
Parents completed the full version of the CBCL (Achenbach & Rescorla, 2001) which is a broadband measure of mental health symptoms in children. Parents of preschool youth completed the 1.5- to 5-year-old form and parents of school age youth completed the 6- to 18-year-old form. The DSM-oriented subscales were used in the present study given their direct correspondence with psychiatric nosology. The DSM-oriented subscales have strong psychometric properties for both the preschool (Rescorla, 2005) and school age forms (Nakamura, Ebesutani, Bernstein, & Chorpita, 2009). These subscales are comparable with the CBCL syndrome scales in regards to demonstrating adequate internal consistency, test-retest reliability, and cross-informant agreement (Achenbach, Dumenci, & Rescorla, 2003) and also have been shown to have adequate correspondence with mental health disorders diagnosed using semi-structured interviews (Ebesutani et al., 2010).
Sleep-related items were removed from CBCL DSM-oriented subscales for analyses of mental health symptoms predicting sleep outcomes. For the 1.5- to 5-year-old form, three items (i.e., trouble sleeping, overtired, sleeps too little) from the affective problems subscale and two items (i.e., doesn’t want to sleep alone, has nightmares) from the anxiety problems subscale were removed. For the 6- to18-year old form, four items (i.e., tired, sleep too little, sleep too much, problems sleeping) were removed from the affective problems subscale.
Analysis Plan
First, descriptive statistics were conducted to determine demographics, sleep diagnoses and symptoms, and prevalence of mental health diagnoses and symptoms at initial sleep evaluation. Next, the unique effects of mental health symptom types in predicting sleep outcomes (insomnia severity as measured by the PISI, CSHQ subscales) were determined in separate analyses for preschool and school age youth. Separate analyses for age groups were run to best appreciate unique developmental differences and because of slight differences in measurement (i.e., CBCL DSM-oriented subscales) across groups. Raw scores for CBCL DSM-oriented subscales with sleep-related items removed were used to predict sleep outcomes. In predicting the PISI total score, multiple regression analyses were used with mental health symptom types (measured by CBCL subscales) as predictors. The relationship between CBCL subscales and sleep behaviors measured by CSHQ subscales were analyzed by estimating path models using Mplus Version 7.3. Path models were used so that multiple independent and dependent variables could be simultaneously evaluated. Separately for preschool and school age youth, a path model with five CBCL components (affective problems, anxiety problems, ADHD problems, and oppositional defiant problems for both age groups with the addition of pervasive developmental problems for preschoolers and conduct problems for school age youth) were regressed onto the CSHQ subscales. Suppressor effects were explored in models when predictors had significant directionality switches from bivariate analyses to multivariate path analyses. When appropriate, suppressor variables were removed from the corresponding model and results from simplified models are presented. Standardized path coefficients were interpreted as a measure of effect size for each relationship (i.e., ≤.1 = small effect, .3 = medium effect, and ≥.5 = large effect; Cohen, 1988).
Results
Descriptive Analyses
See Table 1 for demographics. Behavioral insomnia of childhood was the primary insomnia subtype for both the preschool and school age sample (91.4% and 72.3%, respectively) with 45% of preschoolers and 48% of school age youth having at least one comorbid sleep disorder (see Table 2). Descriptives for the PISI and CSHQ subscales are presented in Table 3.
Table 1.
Demographic information for preschool and school age sample.
| Demographics | Mean ± SD or # (%) | |
|---|---|---|
| Preschool | School Age | |
| N | 373 | 300 |
| Age | 3.72 ± 1.22 | 8.46 ± 1.4 |
| Gender | ||
| Female | 155 (41.6%) | 116 (38.7%) |
| Male | 218 (58.4%) | 184 (61.3%) |
| Race/Ethnicity | ||
| European American | 291 (78.0%) | 241 (80.3%) |
| Black/African-American | 36 (9.7%) | 31 (10.3%) |
| Multi-Racial | 36 (9.7%) | 16 (5.3%) |
| Hispanic/Latino | 6 (1.6%) | 6 (2.0%) |
| Asian/Asian-American | 4 (1.1%) | 5 (1.7%) |
| Other | 0 (0%) | 1 (.3%) |
| Income | ||
| under $19,000 | 91 (24.4%) | 68 (22.7%) |
| $20,000–$49,000 | 84 (22.5%) | 79 (26.3%) |
| $50,000–$74,000 | 53 (14.2%) | 37 (12.3%) |
| $75,000–$99,000 | 46 (12.2%) | 33 (11.0%) |
| $100,000–$149,000 | 52 (13.9%) | 31 (10.3%) |
| $150,000 or more | 30 (8.0%) | 31 (10.3%) |
| Declined to report | 17 (4.6%) | 21 (7.0%) |
Table 2.
Frequency of sleep diagnoses
| ICSD-2 Insomnia Diagnosis | ||
|---|---|---|
| Preschool | School Age | |
| Behavioral Insomnia of Childhood | ||
| Sleep Onset Association Subtype | 115 (30.8%) | 68 (22.7%) |
| Limit Setting Subtype | 69 (18.5%) | 71 (23.7%) |
| Combined Subtype | 157 (42.1%) | 78 (26.0%) |
| Psychophysiological Insomnia | 32 (8.6%) | 83 (27.7%) |
| Comorbid Sleep Disorders | ||
| Parasomnias | 117 (31.4%) | 133 (44.3%) |
| Sleep Related Breathing Disorders | 102 (27.3%) | 77 (25.7%) |
| Sleep Related Movement Disorders | 14 (3.8%) | 12 (4.0%) |
| Sleep Related Medical and Neurological Disorders | 1 (0.3%) | NA |
Table 3.
Descriptive information for parent-report sleep outcome measures.
| Preschool Youth | Mean | SD | Min | Max |
|---|---|---|---|---|
| Pediatric Insomnia Severity Index | 17.46 | 5.6 | 4 | 30 |
| Child Sleep Habits Questionnaire | ||||
| Total Score | 61.3 | 8.14 | 41 | 84 |
| Bedtime Resistance Subscale | 11.77 | 3.34 | 6 | 18 |
| Sleep Onset Delay Subscale | 2.26 | 0.79 | 1 | 3 |
| Sleep Duration Subscale | 6.85 | 1.67 | 3 | 9 |
| Sleep Anxiety Subscale | 7.62 | 2.2 | 4 | 12 |
| Night Wakings Subscale | 6.9 | 1.51 | 3 | 9 |
| Parasomnias Subscale | 12.11 | 2.8 | 7 | 21 |
| Sleep Disordered Breathing Subscale | 4.01 | 1.44 | 3 | 9 |
| Daytime Sleepiness Subscale | 13.88 | 3.39 | 8 | 24 |
| School Age Youth | Mean | SD | Min | Max |
| Pediatric Insomnia Severity Index | 17.21 | 5.6 | 3 | 30 |
| Child Sleep Habits Questionnaire | ||||
| Total Score | 59.88 | 8.64 | 36 | 84 |
| Bedtime Resistance Subscale | 10.53 | 3.08 | 6 | 18 |
| Sleep Onset Delay Subscale | 2.26 | 0.83 | 1 | 3 |
| Sleep Duration Subscale | 6.62 | 1.84 | 3 | 9 |
| Sleep Anxiety Subscale | 7.49 | 2.32 | 4 | 12 |
| Night Wakings Subscale | 6.35 | 1.68 | 3 | 9 |
| Parasomnias Subscale | 11.28 | 2.55 | 7 | 20 |
| Sleep Disordered Breathing Subscale | 3.76 | 1.29 | 3 | 9 |
| Daytime Sleepiness Subscale | 15.26 | 3.99 | 8 | 24 |
Prevalence of Mental Health Symptoms
Table 4 presents the frequency and percentages of parent-reported mental health disorders and clinical elevations (i.e., T-score ≥ 70) on the CBCL DSM-oriented subscales for each group. Rates of any CBCL clinical elevation were statistically different, yet clinically similar, across age groups (69.2% for preschoolers, 77.3% for school age youth; χ2(1) = 5.6, p = .02, r=.09). However, preschoolers had notably lower parent-reports of a mental health diagnosis (34.9% vs. 77.3%; χ2(1) = 100.38, p < .001, r=.39). Behavior disorders, ADHD, and adjustment disorder were the most common parent-reported diagnoses for preschoolers; ADHD, anxiety, and behavior disorders were most common for school age youth. In regards to CBCL symptomatology, affective problems, oppositional defiant problems, and attention-deficit/hyperactivity problems were most commonly clinically elevated for preschoolers; affective problems, oppositional defiant and/or conduct problems, and anxiety problems were most commonly elevated for school age youth. The frequency of affective problem elevations for both age groups may be inflated by the sleep-related items (e.g., sleep problems, sleeps less/more) that load onto this subscale. These items were removed in subsequent analyses to remove content overlap between predictor and outcome variables.
Table 4.
Frequency and prevalence of parent-reported mental health diagnoses and clinical elevations on the CBCL DSM-oriented subscales for preschool and school age youth.
| Preschool Age Children | School Age Children | ||||
|---|---|---|---|---|---|
| Psychopathology Symptom/Diagnosis | Parent-Report Diagnosis | Clinical CBCL Elevation | Parent-Report Diagnosis | Clinical CBCL Elevation | |
| Any Disorder/Elevation | 130 (34.9%) | 258 (69.2%) | 221 (73.7%) | 232 (77.3%) | |
| Anxiety & Related Disorders | 26 (7.0%) | 92 (24.7%) | 94 (31.3%) | 108 (36.0%) | |
| Depression/Mood Disorders | 1 (0.03%) | 203 (54.4%) | 26 (8.7%) | 172 (57.3%) | |
| ADHD | 39 (10.5%) | 107 (28.7%) | 150 (50.0%) | 94 (31.3%) | |
| Behavior Disorders | 40 (10.7%) | 115 (30.8%) | 42 (14.0%) | 119 (39.7%) | |
| Pervasive Dev. Disorders | 19 (5.1%) | 103 (27.6%) | 25 (8.3%) | NA | |
| Adjustment Disorder | 27 (7.2%) | NA | 30 (10.0%) | NA | |
| Other* | 2 (.05%) | NA | 6 (2.0%) | NA | |
| # of Disorders/Elevations | |||||
| Zero | 259 (69.4%) | 115 (30.8%) | 84 (28.0%) | 68 (22.7%) | |
| One | 80 (21.4%) | 91 (24.4%) | 111 (37.0%) | 62 (20.7%) | |
| Two | 27 (7.2%) | 56 (15.0%) | 57 (19.0%) | 65 (21.7%) | |
| More than Two | 7 (1.9%) | 111 (29.8%) | 48 (16.0%) | 105 (35.0%) | |
Note.
Other refers to any diagnosis of Reactive Attachment Disorder, Psychotic Disorder, or Tourette’s Disorder. In regards to correspondence with CBCL DSM-oriented subscales: Anxiety & Related Disorders = Anxiety Problems, Depression & Mood Disorders = Affective Problems, ADHD = Attention Deficit/Hyperactivity Problems, Behavior Disorders = Oppositional Defiant Problems and/or Conduct Problems, Pervasive Dev. Disorders = Pervasive Developmental Problems.
Mental Health Symptoms Predicting Sleep Outcomes
Pediatric Insomnia Severity Index.
Using multiple regression, CBCL subscales accounted for a significant amount of variance (12.1%) in predicting insomnia severity in preschoolers, F(5, 367) = 10.12, p < .001. Affective (β = .22, p = .001) and ADHD problems (β = .18, p = .009) were the only psychopathology domains uniquely associated with insomnia severity.
In school age youth, CBCL subscales accounted for 8.4% of the variance in insomnia severity, F(5, 293) = 5.34, p < .001. Conduct (β = .19, p = .04) and anxiety problems (β = .15, p = .03) were the only psychopathology domains uniquely associated with insomnia severity.
Children’s Sleep Habits Questionnaire.
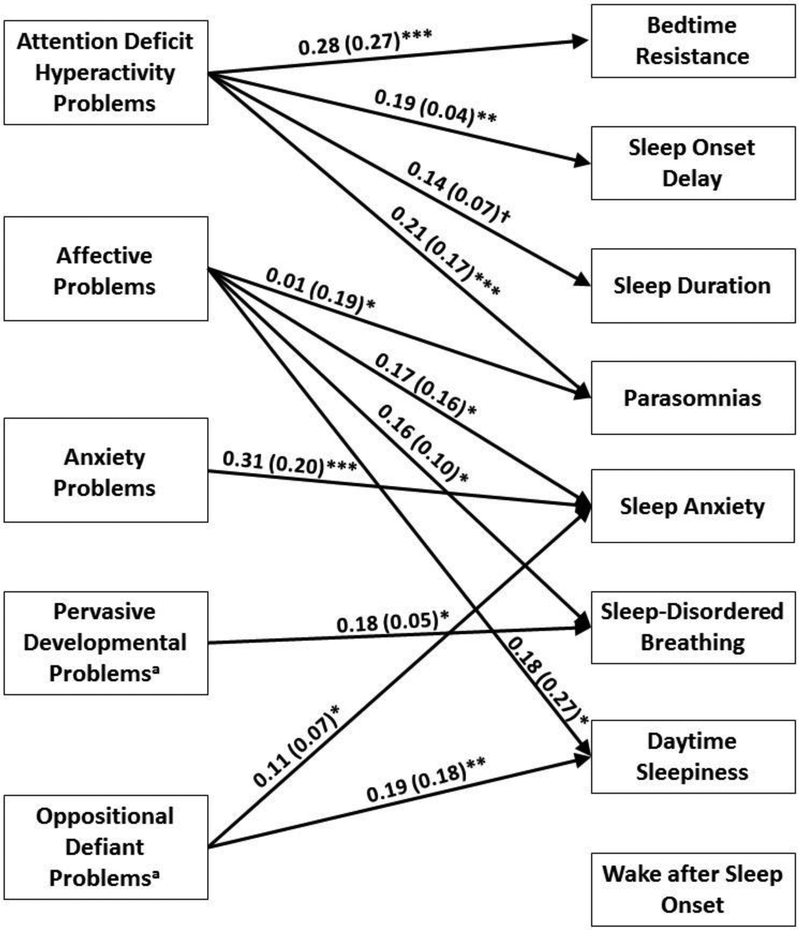
Results from a path model in which the five CBCL DSM-oriented subscales were regressed on CSHQ subscales are presented in Figure 1 for preschoolers and Figure 2 for school age youth. In the preschool model, after controlling for other mental health symptoms, ADHD problems were significantly positively associated with greater bedtime resistance, sleep onset delay, and parasomnias and marginally significantly related (p = .055) to shorter sleep duration. Affective problems were positively associated with greater sleep anxiety, parasomnias, sleep disordered breathing, and daytime sleepiness; oppositional defiant problems with greater sleep anxiety and daytime sleepiness; anxiety problems with greater sleep anxiety; and pervasive developmental problems with greater sleep-disordered breathing. Two directionality switches from bivariate correlations (see Table 5) to multivariate path analyses were present in the preschool models, thus suppressor effects were explored. In the path models, pervasive developmental problems were negatively associated with sleep anxiety and oppositional defiant problems was negatively associated with bedtime resistance despite significant positive bivariate correlations. Follow-up analyses examining suppressor effects found that pervasive developmental problems were nonsignificant when anxiety problems were not included in the path model and oppositional defiant problems were nonsignificant when ADHD was removed. Given these considerations, these negative findings in the path model should not be interpreted, at least until replicated in future research.
Figure 1.
Estimated path model for CBCL DSM-oriented subscale raw scores predicting CSHQ subscales for preschool youth. Standardized parameter estimates are reported outside parentheses; unstandardized parameter estimates are reported inside parentheses. Nonsignificant paths (p > .05) are not shown. aPervasive developmental problems and oppositional defiant problems were found to be suppressor variables in predicting sleep anxiety and bedtime resistance, respectively, thus paths are not shown. †p < .10; *p < .05; **p < .01; ***p < .001.
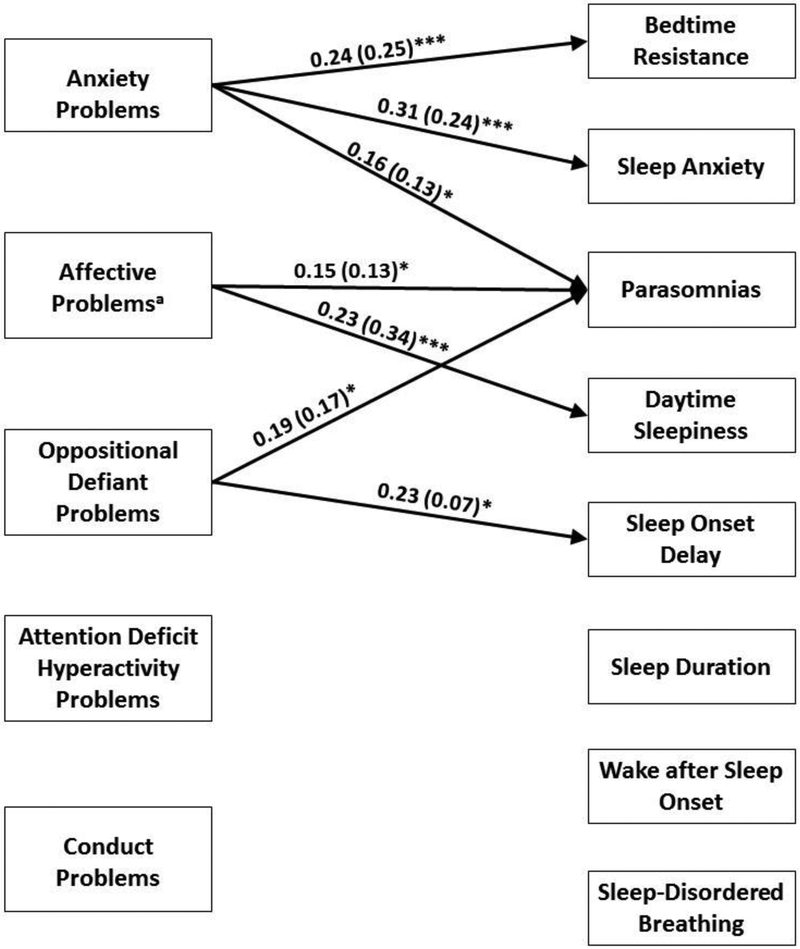
Figure 2.
Estimated path model for CBCL DSM-oriented subscale raw scores predicting CSHQ subscales for school age youth. Standardized parameter estimates are reported outside parentheses; unstandardized parameter estimates are reported inside parentheses. Nonsignificant paths (p > .05) are not shown. aAffective problems was found to be a suppressor variable in predicting sleep anxiety thus path is not shown *p < .05; ***p < .001.
Table 5.
Bivariate correlations between Child’s Sleep Habits Questionnaire (CSHQ) subscales and Child Behavior Checklist (CBCL) subscale raw scores (excluding sleep-related items) for preschool and school age youth.
| Affective | Anxiety | PDD | ADHD | ODD | Affective | Anxiety | ADHD | ODD | CD | |
|---|---|---|---|---|---|---|---|---|---|---|
| .236*** | .216*** | .216*** | .334*** | .193*** | 0.091 | .264*** | 0.065 | 0.095 | 0.013 | |
| .166*** | .106* | .158** | .210*** | .123* | .198*** | .164** | .199*** | .269*** | .177** | |
| .137** | 0.035 | .115* | .168*** | .121* | .141* | 0.093 | .210*** | .189*** | .190*** | |
| .261*** | .312*** | .146** | .196*** | .201*** | 0.006 | .285*** | −0.025 | −0.010 | −0.11* | |
| 0.094 | 0.086 | 0.025 | 0.065 | 0.017 | 0.066 | 0.097 | 0.002 | 0.007 | −0.016 | |
| .243*** | .184*** | .165*** | .289*** | .253*** | .288*** | .305*** | .254*** | .283*** | .154*** | |
| .222*** | 0.094 | .217*** | .137** | .132* | 0.105 | 0.081 | 0.062 | 0.036 | 0.020 | |
| .232*** | .160** | .147** | .117* | .213*** | .298*** | .234*** | .134* | .219*** | .126* |
p < .05,
p < .01,
p < .001
After controlling for other mental health symptoms in the school age model, anxiety problems were positively associated with greater bedtime resistance, sleep anxiety, and parasomnias and oppositional defiant problems were positively associated with greater sleep onset delay and parasomnias. Affective problems were positively associated with greater parasomnias and daytime sleepiness but, contrary to the bivariate correlation, were negatively associated with sleep anxiety. Follow-up analyses examining suppressor effects found that affective problems were no longer associated with sleep anxiety when anxiety was removed from the model, suggesting this finding should not be interpreted.
Discussion
This study demonstrates that prior mental health diagnoses and mental health symptoms are highly prevalent in preschool and school age youth presenting to insomnia evaluation. Over a third of preschoolers and nearly three-quarters of school age youth presented with a diagnosed mental health disorder, per parent report. These rates are far higher than those reported in community samples with prevalence estimates of 12% for school age youth (Polanczyk, Salum, Sugaya, Caye, & Rohde, 2015) and between 14–26% for preschoolers (Egger & Angold, 2006). Even more youth in our sample had at least one clinical elevation on the CBCL DSM-oriented subscales (69% of preschoolers and 77% of school age youth). Notably, parent-report of a mental health diagnosis was significantly lower in the preschool group whereas CBCL elevations were more similar to those of school age youth. This may be an indication that preschoolers presenting to insomnia evaluation have undiagnosed disorders despite clear mental health symptom elevations.
In considering interrelations of psychopathologies and sleep, symptoms of ADHD and affective problems were most consistently associated with sleep problems in preschoolers whereas symptoms of anxiety, affective, and behavioral problems were most consistently associated with sleep problems in school age youth. It is important to acknowledge that youth in these age groups presented with different insomnia subtypes as per ICSD-2 criteria (i.e., school age youth with higher rates of psychophysiological insomnia; 27.7% versus 8.6%) and also demonstrated varying patterns of mental health symptoms which are related to sleep disruptions. This highlights the importance of considering development in the assessment and treatment of behavioral insomnia.
Although associated with most types of sleep disruption, no mental health symptoms in either age group were associated with night wakings as measured by the CSHQ. One possible explanation is that mental health symptoms may be more clearly related to sleep onset problems (e.g., bedtime resistance, difficulty falling asleep, nighttime fears) or of daytime sequela of poor sleep (e.g., daytime sleepiness) but are less likely to be associated with sleep maintenance difficulties. It is possible that sleep maintenance problems are more reflective of issues of sleep quality or of medical sleep concerns (e.g., OSA). However, this null finding may reflect limitations of parental reports of sleep problems and, specifically, the possibility that parents are unaware of or underestimate the number of night wakings in their children (Owens, Spirito, McGuinn, & Nobile, 2000; Van Dyk, Thompson, & Nelson, 2016). Research using more objective measures of night wakings (e.g., actigraphy) is needed to confirm this lack of relationship.
Notably, many mental health symptoms were associated with parasomnias including ADHD and affective problems in preschool youth and anxiety, affective, and oppositional defiant problems in school age youth. These results are consistent with prior studies in youth finding relationships between ADHD and restlessness (Cortese et al., 2005); anxiety and night terrors, sleep talking, restlessness, bruxism, and body rocking (Laberge, Tremblay, Vitaro, & Montplaisir, 2000); and anxiety and depressive symptoms with nightmares (Jansen et al., 2011). It is possible that sleep disruption resulting from parasomnias may impact daytime behavior (e.g., increased inattentiveness) and mood (e.g., poor emotion regulation) or that shared etiological factors (e.g., dopaminergic deficits in both ADHD and restlessness) explain the association between parasomnias and mental health symptoms in youth (Cortese et al., 2005). Future research is needed to more closely examine mechanisms of this relationship.
Interestingly, despite prior studies finding a relationship between ADHD and disrupted sleep in children (Cortese, Faraone, Konofal, & Lecendreux, 2009), we found ADHD symptoms to be independently associated with sleep problems in preschool-aged children but not school aged children. There are several possible reasons for this differential finding across developmental groups. First, it should be noted that although the CBCL ADHD scale is DSM-based, it does not capture all ADHD symptoms and does not separate inattentive and hyperactive-impulsive symptoms which are themselves differentially related to sleep problems and daytime dysfunction (Mayes et al., 2009). Second, our sample is unique in that children were referred for insomnia, not mental health difficulties, and the heterogeneity of our sample including a wide range of psychological and medical comorbidities (and possible medications) may have impacted findings. Third, children with ADHD frequently experience comorbid mental health problems, and comorbid symptoms have been identified as important contributors to the sleep problems experienced by children with ADHD (e.g., Becker, Cusick, Sidol, Epstein, & Tamm, 2017; Moreau, Rouleau, & Morin, 2014). In our preschool sample, both ADHD and ODD symptoms had unique associations to sleep behavior. This is despite high rates of comorbidity. Specifically, 68% of preschoolers in our sample with a clinical elevation of ADHD also had a clinical elevation of ODD, which is consistent with rates of ADHD/ODD comorbidity found in clinical samples of youth (Wilens et al., 2002). In contrast, ADHD symptoms were not associated with sleep problems in our school age sample. Although speculative in the absence of longitudinal data, it is possible that co-occurring symptoms become more strongly associated with sleep problems across development. Future research in longitudinal samples should further explore the links between ADHD and sleep disruption within the context of comorbidity, focusing on specific symptoms or possible mechanisms which may explain differences across development.
Clinical Implications
Results support the notion that mental health symptoms should be assessed within the context of pediatric insomnia evaluation. Further, appropriate referrals or treatment should be provided to target these symptoms. Currently, evidenced-based treatments of pediatric insomnia specifically designed to be implemented in youth with psychological comorbidity are lacking and needed. A recent review explored the feasibility of using behavioral sleep interventions originally developed for typically developing youth in children with neurodevelopmental disorders, including ADHD and Autism Spectrum Disorder (Rigney et al., 2018). Studies reviewed indicated that components of behavioral treatments for insomnia (e.g., psychoeducation, healthy sleep practices, graduated extinction, bedtime fading) were effective. This suggests that effective behavioral sleep treatments can be developed and implemented specifically for these special populations. Further, considering the high rates of mental health problems in youth presenting for insomnia assessment, behavioral sleep medicine providers should consider the potential impact of specific psychiatric symptoms on insomnia conceptualization and treatment. Although these constructs are related at intake into treatment, further research is needed to examine how psychological comorbidity could exacerbate sleep-related behaviors and/or interfere with behavioral sleep treatments.
As previously noted, preschoolers had far fewer mental health diagnoses than the school age group despite similar levels of distress being reported on the CBCL by parents. Relatively low rates of diagnosis in preschoolers could be because (1) children at this age may have not yet been referred for evaluation, and (2) even if evaluated, many professionals are reluctant to diagnose a mental health disorder at such an early age. Although they have not received diagnoses, parents are viewing their children’s symptoms as problematic yet may not be receiving services to target these concerns. Behavioral sleep medicine providers may be uniquely poised to identify these problems in preschoolers and provide adequate follow-up care or referrals.
Limitations and Future Directions
Despite several study advantages, including a large, representative sample size; use of standardized measures; and ability to examine developmental differences in the relationship between sleep and mental health, limitations should be noted. First, although statistically and clinically meaningful, effect sizes were small. This suggests that mental health problems are just one factor predicting disrupted sleep. A multifactorial approach to understanding sleep problems in youth is needed. For example, future research should examine medical comorbidities and medication use (particularly psychotropic medications) in addition to mental health comorbidities. Second, both assessment of mental health diagnoses/symptoms and sleep problems relied on parent report. It is possible that findings are at least partially accounted for by shared method variance and/or reporter bias. Further related to measurement, the preliminary validation of the CSHQ and PISI for youth under 2.5 years is a limitation. Future research utilizing multiple reporters (e.g., children, teachers), different methodologies (e.g., questionnaire, actigraphy), and measures specifically validated in younger samples is needed to confirm relationships between sleep and mental health problems in youth presenting to insomnia treatment. Third, although our methodology includes a more comprehensive sample than has been evaluated in prior research, our decision to include those with a primary insomnia diagnosis does exclude some youth presenting to behavioral sleep medicine clinics (e.g., those with a primary diagnosis of parasomnia) and thus findings cannot be generalized to these individuals. Next, the cross-sectional nature of this study prevents conclusions regarding the directionality of associations. It is possible that sleep problems precede mental health symptoms or that bidirectional relationships exist. Finally, direct comparison of mental health symptoms between age groups is limited by the use of two different versions of the CBCL. This was appropriate for each age group, but it is possible the differences in measurement could account for discrepancies in findings.
Conclusions
Youth presenting to insomnia treatment have high rates of mental health diagnoses and symptoms and these symptoms are associated with sleep disruption. Symptoms of psychopathology should be regularly assessed in behavioral sleep medicine clinics and providers should consider how these symptoms may exacerbate sleep problems and/or interfere with treatment. Clinicians should be targeting mental health symptoms in their treatment or making referrals to appropriate providers to address mental health problems.
References
- Achenbach TM, Dumenci L, & Rescorla LA (2003). DSM-oriented and empirically based approaches to constructing scales from the same item pools. Journal of Clinical Child and Adolescent Psychology, 32(3), 328–340. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Aikens JE, Vanable PA, Tadimeti L, Caruana-Montaldo B, & Mendelson WB (1999). Differential Rates of Psychopathology Symptoms in Periodic Limb Movement Disorder, Obstructive Sleep Apnea, Psychophysiological Insomnia, and Insomnia with Psychiatric Disorder. Sleep, 22(6), 775–780. [DOI] [PubMed] [Google Scholar]
- American Academy of Sleep Medicine. (2005). International Classification of Sleep Disorders: Diagnostic and Coding Manual (2nd ed., Vol. 2). Westchester, IL: American Academy of Sleep Medicine. [Google Scholar]
- American Academy of Sleep Medicine. (2014). International Classification of Sleep Disorders: Diagnostic and Coding Manual (3rd ed.). Darien, IL: American Academy of Sleep Medicine. [Google Scholar]
- Becker SP, Cusick CN, Sidol CA, Epstein JN, & Tamm L (2017). The impact of comorbid mental health symptoms and sex on sleep functioning in children with ADHD. European Child & Adolescent Psychiatry, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byars K, Apiwattanasawee P, Leejakpai A, Tangchityongsiva S, & Simakajornboom N (2011). Behavioral sleep disturbances in children clinically referred for evaluation of obstructive sleep apnea. Sleep Medicine, 12(2), 163–169. [DOI] [PubMed] [Google Scholar]
- Byars K, & Simon S (2014). Practice patterns and insomnia treatment outcomes from an evidence-based pediatric behavioral sleep medicine clinic. Clinical Practice in Pediatric Psychology, 2(3), 337. [Google Scholar]
- Byars KC, Simon SL, Peugh J, & Beebe DW (2017). Validation of a Brief Insomnia Severity Measure in Youth Clinically Referred for Sleep Evaluation. Journal of Pediatric Psychology, 42(4), 466–475. [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. Hilsdale. NJ: Lawrence Earlbaum Associates, 2. [Google Scholar]
- Cortese S, Faraone SV, Konofal E, & Lecendreux M (2009). Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. Journal of the American Academy of Child & Adolescent Psychiatry, 48(9), 894–908. [DOI] [PubMed] [Google Scholar]
- Cortese S, Konofal E, Lecendreux M, Arnulf I, Mouren M-C, Darra F, & Bernardina BD (2005). Restless Legs Syndrome and Attention-Deficit/Hyperactivity Disorder: a Review of the Literature. Sleep, 28(8), 1007–1013. [DOI] [PubMed] [Google Scholar]
- Dahl RE, & Harvey AG (2007). Sleep in Children and Adolescents with Behavioral and Emotional Disorders. Sleep Medicine Clinics, 2(3), 501–511. [Google Scholar]
- Dezee KJ, Hatzigeorgiou C, Kristo D, & Jackson JL (2005). Prevalence of and screening for mental disorders in a sleep clinic. Journal of Clinical Sleep Medicine, 1(2), 136–142. [PubMed] [Google Scholar]
- Ebesutani C, Bernstein A, Nakamura BJ, Chorpita BF, Higa-McMillan CK, & Weisz JR (2010). Concurrent Validity of the Child Behavior Checklist DSM-Oriented Scales: Correspondence with DSM Diagnoses and Comparison to Syndrome Scales. Journal of Psychopathology and Behavioral Assessment, 32(3), 373–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger HL, & Angold A (2006). Common emotional and behavioral disorders in preschool children: presentation, nosology, and epidemiology. Journal of Child Psychology and Psychiatry, 47(3–4), 313–337. [DOI] [PubMed] [Google Scholar]
- Ivanenko A, Barnes ME, Crabtree VM, & Gozal D (2004). Psychiatric symptoms in children with insomnia referred to a pediatric sleep medicine center. Sleep Medicine, 5(3), 253–259. [DOI] [PubMed] [Google Scholar]
- Ivanenko A, Crabtree VM, Obrien LM, & Gozal D (2006). Sleep complaints and psychiatric symptoms in children evaluated at a pediatric mental health clinic. Journal of Clinical Sleep Medicine, 2(1), 42–48. [PubMed] [Google Scholar]
- Jansen PW, Saridjan NS, Hofman A, Jaddoe VWV, Verhulst FC, & Tiemeier H (2011). Does Disturbed Sleeping Precede Symptoms of Anxiety or Depression in Toddlers? The Generation R Study. Psychosomatic Medicine, 73(3), 242–249. [DOI] [PubMed] [Google Scholar]
- Laberge L, Tremblay RE, Vitaro F, & Montplaisir J (2000). Development of Parasomnias From Childhood to Early Adolescence. Pediatrics, 106(1), 67–74. [DOI] [PubMed] [Google Scholar]
- Lewandowski AS, Toliver-Sokol M, & Palermo TM (2011). Evidence-based review of subjective pediatric sleep measures. Journal of Pediatric Psychology, 36(7), 780–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayes SD, Calhoun SL, Bixler EO, Vgontzas AN, Mahr F, Hillwig-Garcia J, … Parvin M (2009). ADHD Subtypes and Comorbid Anxiety, Depression, and Oppositional-Defiant Disorder: Differences in Sleep Problems. Journal of Pediatric Psychology, 34(3), 328–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreau V, Rouleau N, & Morin CM (2014). Sleep of children with attention deficit hyperactivity disorder: actigraphic and parental reports. Behavioral Sleep Medicine, 12(1), 69–83. [DOI] [PubMed] [Google Scholar]
- Nakamura BJ, Ebesutani C, Bernstein A, & Chorpita BF (2009). A psychometric analysis of the child behavior checklist DSM-oriented scales. Journal of Psychopathology and Behavioral Assessment, 31(3), 178–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens J, Opipari L, Nobile C, & Spirito A (1998). Sleep and daytime behavior in children with obstructive sleep apnea and behavioral sleep disorders. Pediatrics, 102(5), 1178–1184. [DOI] [PubMed] [Google Scholar]
- Owens JA, Spirito A, & McGuinn M (2000). The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep, 23(8), 1043–1052. [PubMed] [Google Scholar]
- Owens JA, Spirito A, McGuinn M, & Nobile C (2000). Sleep habits and sleep disturbance in elementary school-aged children. Journal of Developmental and Behavioral Pediatrics, 21(1), 27–36. [DOI] [PubMed] [Google Scholar]
- Polanczyk GV, Salum GA, Sugaya LS, Caye A, & Rohde LA (2015). Annual Research Review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. Journal of Child Psychology and Psychiatry, 56(3), 345–365. [DOI] [PubMed] [Google Scholar]
- Reigstad B, Jørgensen K, Sund AM, & Wichstrøm L (2010). Prevalences and correlates of sleep problems among adolescents in specialty mental health services and in the community: What differs? Nordic Journal of Psychiatry, 64(3), 172–180. [DOI] [PubMed] [Google Scholar]
- Rescorla LA (2005). Assessment of young children using the Achenbach System of Empirically Based Assessment (ASEBA). Developmental Disabilities Research Reviews, 11(3), 226–237. [DOI] [PubMed] [Google Scholar]
- Rigney G, Ali NS, Corkum P, Brown CA, Constantin E, Godbout R, … Weiss SK (2018). A Systematic Review to Explore the Feasibility of a Behavioural Sleep Intervention for Insomnia in Children with Neurodevelopmental Disorders: A Transdiagnostic Approach. Sleep Medicine Reviews. [DOI] [PubMed] [Google Scholar]
- Van Dyk TR, Thompson RW, & Nelson TD (2016). Daily Bidirectional Relationships Between Sleep and Mental Health Symptoms in Youth With Emotional and Behavioral Problems. Journal of Pediatric Psychology, 41(9), 983–992. [DOI] [PubMed] [Google Scholar]
- Velten-Schurian K, Hautzinger M, Poets CF, & Schlarb AA (2010). Association between sleep patterns and daytime functioning in children with insomnia: the contribution of parent-reported frequency of night waking and wake time after sleep onset. Sleep Medicine, 11(3), 281–288. [DOI] [PubMed] [Google Scholar]
- Wilens TE, Biederman J, Brown S, Tanguay S, Monuteaux MC, Blake C, & Spencer TJ (2002). Psychiatric comorbidity and functioning in clinically referred preschool children and school-age youths with ADHD. Journal of the American Academy of Child & Adolescent Psychiatry, 41(3), 262–268. [DOI] [PubMed] [Google Scholar]