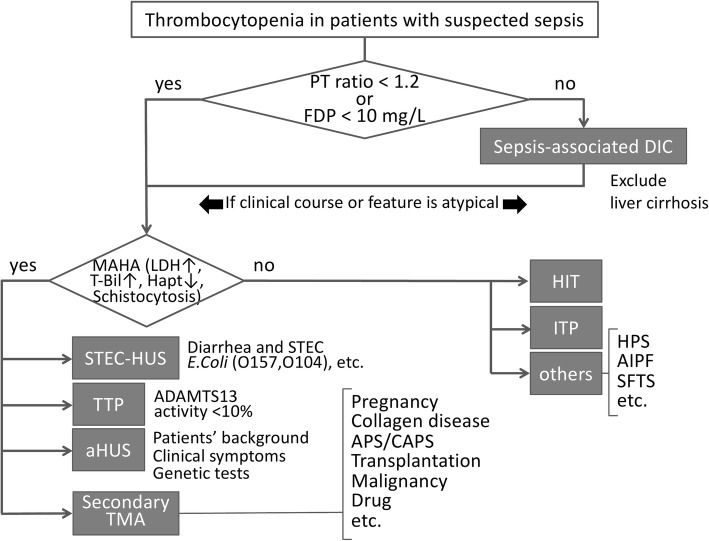
Fig. 1.
An algorithm to differentiate sepsis-associated DIC from other diseases with thrombocytopenia. Both the prothrombin time (PT) ratio and the level of fibrin/fibrinogen degradation products are elevated in sepsis-associated DIC (disseminated intravascular coagulation). If either marker is within the normal range, other diseases can be suspected. If microangiopathic hemolytic anemia (MAHA) is recognized, Escherichia coli (STEC)-hemolytic uremic syndrome (HUS) will be discriminated by performing a stool culture or polymerase chain reaction (PCR) assay first. If it is not, thrombotic thrombocytopenic purpura (TTP), atypical HUS (aHUS), or secondary thrombotic microangiopathy are suspicious, and the early initiation of plasma exchange is recommended unless a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13 (ADAMTS13) level is confirmed. TTP is diagnosed by the identification of a low ADAMTS13 activity (< 10%). If plasma exchange is ineffective, refractory TTP, aHUS, or other disease is suspicious and the use of either rituximab or eculizumab will be considered. In those cases, the laboratory findings and clinical symptoms such as acute kidney injury and gastrointestinal or neurological damage will be carefully examined; if these findings suggest aHUS, the patient’s age and medical and family histories can be helpful for a diagnosis. Similarly, the possibility of secondary TMAs can be considered. If the presence of MAHA is not recognized, the possibility of other diseases such as heparin-induced thrombocytopenia (HIT), immune thrombocytopenia purpura (ITP), hemophagocytic syndrome (HPS), acute infectious purpura fulminans (AIPF), severe fever and thrombocytopenia syndrome (SFTS), and thrombocytopenia, anasarca, fever, reticulin fibrosis, and organomegaly (TAFRO) syndrome would be considered