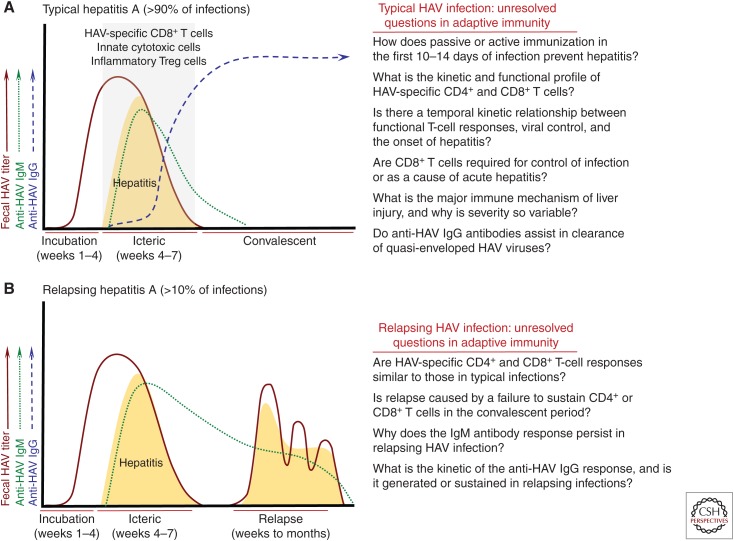
Figure 1.
Adaptive immunity in hepatitis A virus (HAV) infection. (A) Typical hepatitis A. The majority (>90%) of acute HAV infections are characterized by an incubation phase of 3–4 weeks followed by an icteric phase of 2–4 weeks (see Shin and Jeong 2018). Hepatitis, which is thought to be immune mediated, is highly variable in severity. It ranges from clinically inapparent in young children to more severe in older children and adults. Serum anti-HAV IgM antibodies appear within a few days of the onset of hepatitis and generally become undetectable within 4 months. Anti-HAV IgG antibody titers increase in the late symptomatic phase and remain detectable for life. HAV-specific CD8+ T cells have been detected in blood and liver of patients during the icteric phase (Vallbracht et al. 1986, 1989; Fleischer and Vallbracht 1991; Schulte et al. 2011), and probably decline in frequency with resolution of the infection (Schulte et al. 2011). Recent studies have also described expansion of innate cytotoxic cells and T regulatory (Treg) cells that have converted to an inflammatory phenotype in individuals with symptomatic infections (Choi et al. 2018b; Kim et al. 2018). CD4+ and CD8+ T-cell frequency and function have been described in too few studies to superimpose kinetic curves on the profile of resolving HAV infections. Key unanswered questions about adaptive immune responses in acute hepatitis A are shown to the right. (B) Relapsing hepatitis A. Approximately 5%–10% of acute HAV infections relapse about 1–4 months after apparent resolution of symptoms and virus replication. Very little is known about adaptive immune responses in this uncommon but fascinating atypical form of the infection. Anti-HAV IgM responses persist through the relapse phase, and therefore are sustained for a longer period of time when compared with typical infections that do not relapse. Little is known about the anti-HAV IgM response or the nature of T-cell immunity during the primary or relapsing phases of infection. It is likely that failure to develop or sustain a virus-specific humoral or cellular immune response facilitates relapse of infection. It is important to emphasize that even relapsing infections eventually resolve, and persistence of HAV has not been described under conditions that lead to chronic hepatitis E virus (HEV) infection.