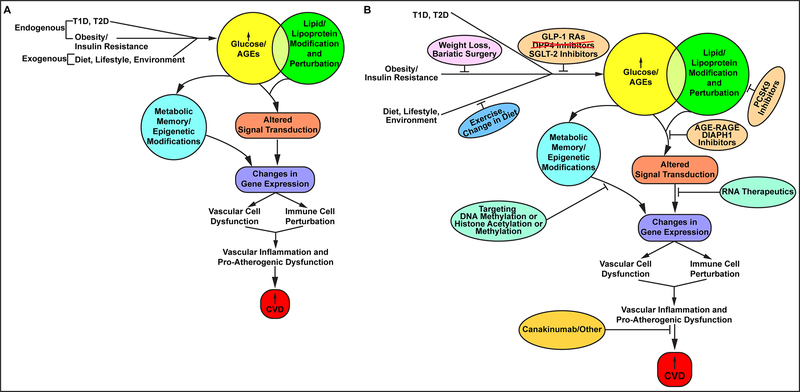
Figure 1. Pathobiological mechanisms and therapeutic targets for diabetes and CVD.
(A). Examples of proposed mechanisms of diabetes and CVD. Both endogenous and exogenous forces may converge to increase glucose levels, one consequence of which is the formation nonenzymatically glycated proteins or lipids, called AGEs, or advanced glycation endproducts – factors that have been linked mechanistically to the pathogenesis of CVD. Independently, lipid abnormalities in obesity and diabetes pose independent risk for CVD. Further, these two pathways may converge, as glycation of lipids and lipoproteins has been shown in multiple basic science experiments to regulate factors that aggravate CVD risk. Once ignited, the actions of glucose, AGEs and lipids modulate signaling pathways and factors that regulate gene expression, including microRNAs and lncRNAs. The consequences of these changes in gene expression may be vast, affecting the functions of both vascular cells and immune cells. Indeed, increased “vascular inflammation” occurs in diabetes and leads to the upregulation of factors that augment CVD risk. In addition, long-term epidemiologic studies have underscored that in both T1D and T2D, the effects of hyperglycemia may be long-lived, leading to epigenetic changes that may affect gene expression patterns and CVD risk for many years. Finally, fundamental changes in body mass and reductions in physical activity may portend increased obesity, insulin resistance, and if left unchecked, T2D. (B) Emerging therapeutic strategies in diabetes and metabolic dysfunction to combat CVD. Recent results from CVOTs demonstrated unexpected cardiovascular benefit from the use of newer classes of agents targeting hyperglycemia, namely, the GLP-1 RAs and the SGLT-2 inhibitors. However, the DPP4 inhibitors have not been shown to exert the same degree of benefits in CVD, but may be associated with higher rates of heart failure. Further, some of the members of these classes of agents have been associated with some risks, such as increased mycotic infections, increased retinopathy and risk of amputations, for unclear reasons. For maximally treated with statins subjects or in subjects with statin intolerance, studies have begun to show that the new series of antibodies targeting PCSK9 may exert equivalent benefit in CVD in non-diabetic and diabetic subjects. Recent discoveries on the roles of miRNAs and lncRNAs in diabetic complications in preclinical models may lead to broader testing and use of ASOs and GapmeRs for diabetes and CVD. The recent success of canakinumab, as illustrated in the CANTOS trial, solidified for the first time in a large clinical trial the benefits of targeting inflammation for CVD. In the CANTOS trial, it was shown that diabetic subjects and non-diabetic subjects benefitted from this approach. It is to be noted that there was an increased risk of serious infection in the canakinumab-treated group vs. the placebo. If and how this may affect overall utility for diabetic subjects remains to be determined. In the field of cancer, novel approaches to targeting DNA methylation and histone methylation and acetylation are gaining traction; given the evidence of “metabolic memory” in diabetic complications, such approaches may well soon be tested in diabetes and CVD. Lifestyle interventions, although tantalizing, have long proved to be difficult to achieve and sustain. Recent work has suggested that bariatric surgery may exert possible CVD benefits on account of weight loss, but, as well, to other to-be-elucidated factors (such as changes in gut hormones, as an example). Finally, novel approaches to disease modification, such as antagonism of the RAGE/DIAPH1 signaling pathway, have shown benefit in preclinical models of inflammation and diabetes. Work is ongoing to test these concepts. Note that this review was meant to illustrate but some of recently emerging targets for diabetes and CVD. Given the scope of the epidemics of obesity and diabetes, such efforts are both timely and, potentially, life-saving.