Abstract
Objective:
To evaluate the impact of an academic detailing intervention delivered as part of a quality improvement project by a physician–pharmacist pair on (1) self-reported confidence in prescribing for older adults and (2) rates of potentially inappropriate medications (PIMs) prescribed to older adults by physician residents in a Veteran Affairs emergency department (ED).
Methods:
This quality improvement project at a single site utilized a questionnaire that assessed knowledge of Beers Criteria, self-perceived barriers to appropriate prescribing in older adults, and self-rated confidence in ability to prescribe in older adults which was administered to physician residents before and after academic detailing delivered during their emergency medicine rotation. PIM rates in the resident cohort who received the academic detailing were compared to residents who did not receive the intervention.
Results:
Sixty-three residents received the intervention between February 2013 and December 2014. At baseline, approximately 50% of the residents surveyed reported never hearing about nor using the Beers Criteria. A significantly greater proportion of residents agreed or strongly agreed in their abilities to identify drug–disease interactions and to prescribe the appropriate medication for the older adult after receiving the intervention. The resident cohort who received the educational intervention was less likely to prescribe a PIM when compared to the untrained resident cohort with a rate ratio of 0.73 (P < .0001).
Conclusion:
Academic detailing led by a physician–pharmacist pair resulted in improved confidence in physician residents’ ability to prescribe safely in an older adult ED population and was associated with a statistically significant decrease in PIM rates.
Keywords: potentially inappropriate medications, elderly, academic detailing
Introduction
Health-care providers with adequate geriatric training are essential to meet the health-care demands of an aging population. The Institute of Medicine reported that by 2030 the proportion of older adults will surpass the current infrastructure of geriatric-trained health-care professionals resulting in a health system at risk of failing to meet their health-care needs.1 The inability to produce health-care professionals with geriatric expertise has largely been the result of inconsistent geriatric training in both professional schools and postgraduate training.2,3 Lack of such training may result in prescribers not adequately exposed to the alterations of pharmacokinetic and pharmacodynamic medication parameters that increase the risk of adverse drug effects in the older adult.
Explicit criteria, such as the American Geriatrics Society Beers Criteria, exist to help guide prescribing by identifying potentially inappropriate medications (PIMs) in the older adult.4 The Beers Criteria identify medications that are high risk in older adults and have been used extensively in PIM research in various settings including the emergency department (ED).5–7 However, medication prescribing in older adults continues to be reported by recent physician graduates as an area of weakness.8–10 Specifically, in a survey administered to physician residents at a large teaching hospital, only 32% of respondents reported confidence in managing medications in an older adult population.10 Moreover, a large proportion of physician residents were unfamiliar with commonly used explicit criteria to identify PIMs and identified medication management and polypharmacy as important topics to learn.10
Physician residents frequently prescribe medications to older adults in the ED where PIMs are commonly used and are associated with poor outcomes. A significant proportion of older adults present to the ED already have been previously prescribed a PIM and approximately 6% to 14% of older adults are prescribed a PIM in the ED and discharged home.11–13 In a Veteran Affairs (VA) retrospective, cohort study, approximately 31% of older adults discharged from the ED were prescribed a suboptimal medication; of these 42% experienced ED representation, hospitalization, or death within the subsequent 90 days.14 Emergency medicine (EM) residents have tested poorly on geriatric EM competencies, specifically on the use of medications in the elderly with scores of 37.5%.15 Poor test scores by EM residents is an alarming finding, given they will provide care for a large proportion of older adults who are at an increased risk of drug-related problems.
In the past decade, several initiatives have been developed to create geriatric competencies in EM physicians but fall short on practical guidance to ensure safe medication prescribing. In 2008, the American College of Emergency Physicians called for the development of geriatric core competencies for the EM resident, which were subsequently released in 2010.16,17 These core competencies included medication management with 3 global recommendations on best practices in the ED but lacked specific recommendations to avoid medications that may increase harm. Additionally, geriatric ED guidelines were published in 2014 that included medication management highlighting the use of the American Geriatric Society Beers Criteria but offered little guidance on how to enhance prescribing practices in this population.18 Enhancing Quality of Prescribing Practices for Veterans Discharged from the Emergency Department (EQUiPPED) is one project that has aimed to decrease PIM prescribing in an older veteran population seen in the ED.19–23 The EQUiPPED intervention consisted of 3 main components: provider education through academic detailing, clinical decision support, and provider feedback on prescribing practices.19 EQUiPPED has been able to show a decrease in PIM rates by ED prescribers through education, clinical decision support, and prescribing feedback.19–23 The purpose of our article is to evaluate the impact of an academic detailing intervention on self-reported confidence in prescribing for older adults among physician residents rotating in the ED of an academic VA medical center and to compare pooled PIM rates from physician resident prescribers after receiving EQUiPPED academic detailing from a physician–pharmacist pair to a physician resident cohort prior to EQUiPPED who did not receive academic detailing. Because EQUiPPED targeted mostly ED staff providers, we were interested in examining the impact the intervention had specifically on physician residents, given they are still in postgraduate training and, due to their time in the ED, had less exposure to the intervention’s components. The association of PIMs use and morbidity in the older adult is well established in the literature; however, there is a lack of reports that describe physician residents and PIM use as well as interventions that impact prescribing in physician residents. Our site was the only site that delivered the EQUiPPED intervention to physician residents giving us the opportunity to examine this group separately.
Methods
Setting
The Durham Veteran Affairs Medical Center (VAMC) is a tertiary care, teaching hospital affiliated with the Duke University School of Medicine. The Durham VAMC ED provides care for approximately 32 000 patient visits annually; of these, approximately 40% are 65 years and older.24 At the time of writing this article, ED care is provided by approximately 2 attending physicians, 3 advanced practice providers, and 6 to 8 physician residents at any one time. Additionally, the ED has a dedicated clinical pharmacy specialist (CPS). The EM CPS was physically present in the ED Monday through Friday from 0900 to 1730. Outside of these times, pharmacy support was limited to the centralized staff pharmacists whose primary responsibility was order processing. Following VA regulations, the EQUiPPED initiative was certified as a nonresearch quality improvement activity by the VA’s Acting Chief Consultant for Geriatrics in Office of Geriatrics and Extended Care and therefore did not require approval from an institutional review board.
Intervention
EQUiPPED is a multicomponent, quality improvement initiative that was implemented at the Atlanta VAMC (Birmingham/ Atlanta GRECC), the Durham VAMC (Durham GRECC), the Tennessee Valley Healthcare System Nashville Campus (Tennessee Valley GRECC), and later in the James J. Peters VAMC (Bronx GRECC) and the Birmingham VAMC (Birmingham/ Atlanta GRECC). The intervention was designed to be adaptable, with each site tailoring the individual project components to meet the needs of their specific VA ED. Internal medicine residents from Duke University complete a 4-week block of EM training at the Durham VAMC. Each month the Durham VA ED precepted approximately 3 internal medicine residents along with a first-year (intern) EM resident. The medical interns were in the first year of a 3-year EM residency program. Initial academic detailing was delivered to residents at the beginning of the EM rotation, either on the first day as a group or within the first week if there were scheduling conflicts. The initial academic detailing session consisted of didactic education comprised of a standardized lecture format that was developed by Durham EQUiPPED members highlighting core geriatric prescribing principles including physiologic changes in the elderly, changes in pharmacokinetic and dynamics, principles of adverse drug reactions (ADRs) in the older adult, a review of the 2012 American Geriatric Society Beers Criteria, and finally common examples of PIMs used in the EM setting with viable alternatives. The didactic session was facilitated by an EQUiPPED geriatrician–CPS pair. An EM attending filled the role of facilitator if the geriatrician was not available. Additionally, residents were oriented to clinical decision support tools that were designed to augment core geriatric principles through the use of prepopulated ordered sets.22 At the midpoint of the 1-month rotation, residents were provided with prescribing reports that included aggregate data on the individual resident, including patients and prescriptions, number of PIMs, and rate of PIMs on all prescriptions.21 To augment the academic detailing for the resident physicians at the Durham VAMC, additional interventions to decrease PIM prescribing were developed and implemented at various time points throughout the project. At the Durham VA, the components of the intervention were implemented in a rolling fashion. Academic detailing began in February 2013, clinical decision support was initially implemented in June 2013 with medication alert messages identifying the medication as a PIM at computerized order entry, and later disease-specific order sets were implemented in a rolling fashion starting July 2013 with the last order set live in November 2013. Lastly, computer cards that identified the most commonly prescribed PIMs were implemented in November 2013.
Knowledge Measure
A previously published questionnaire (Appendix A) was adapted to assess physician resident prescribing behaviors and confidence of prescribing in an older adult population prior to the educational intervention.25 The questionnaire was in a paper format, and residents were allowed 5 to 10 minutes to complete it prior to the education after which the questionnaires were collected by the EQUiPPED geriatric–CPS pair. The questionnaire included 3 items: (1) a statement for residents to rate how often they use the Beers Criteria to guide medication prescribing for older adults in an ED environment (5-point Likert scale; 1 = often use, 2 = sometimes use, 3 = rarely use, 4 = know of but never use, 5 = never heard of); (2) residents’ confidence of their ability to prescribe appropriate medications in 5 domains (4-point Likert scale; 1 = strongly agree, 2 = agree, 3 = disagree, 4 = strongly disagree); and (3) a 9-item scale rating of identified barriers to appropriate geriatric prescribing (4-point Likert scale; strongly agree, agree, disagree, strongly disagree). During the final week of rotation, the questionnaire was readministered to determine whether the educational intervention improved self-perceived confidence in prescribing habits and the frequent use of the Beers Criteria in older adults provided care in the ED.
PIM Rates
To assess the impact of the educational intervention, new PIMs prescribed by residents who received the intervention were compared to new PIMs prescribed by a resident cohort who did not receive the educational intervention and rotated through the ED from July 1, 2011, to February 28, 2013, prior to the onset of EQUiPPED. New medications were defined as PIMs and were adapted from table 2 in the American Geriatrics Society 2012 Beers Criteria Update that lists medications to avoid in all older adults.4 Medications were categorized as an ED discharge medication if the medication was released and the ordering clinic location was from the ED and the provider was a resident during their EM rotation. We included all ED discharge medications to patients aged 65 years and older discharged from the Durham VAMC EM prescribed by both the trained and untrained residents, and medications administered in the ED were not included.
Analysis
Questionnaire data were analyzed to determine whether there was a difference in the aggregate between pre- and postintervention for the distribution of the responses. Since these were ordinal categorical variables, the Mantel-Haenszel row mean score test was used. Monthly PIM rates (dependent variable) were defined as new PIMs over total discharge medications prescribed to patients aged 65 or older. Poisson regression was used to evaluate the PIMs prescribing rates between the untrained period (starting July 1, 2011, and ending February 28, 2013) and the trained period (starting February 1, 2013, and ending December 31, 2014). The total number of prescriptions served as the offset term in the model and the link was specified as log linear, and the model was found not to be overdispersed. In addition, to illustrate the “nearest neighbor” estimate of PIM rate over time, a LOESS curve was generated by using a smoothing parameter of 0.5. Analyses were conducted with SAS version 9.4 (SAS Institute, Cary, North Carolina).
Results
The educational intervention was delivered to 63 internal medicine residents from February 2013 to December 2014. Of these, n = 50 (79%) completed the preintervention questionnaire and n = 29 (46%) completed the posttest questionnaire. Figure 1 shows the baseline responses of self-perceived barriers to appropriate prescribing. A large proportion of participants agreed or strongly agreed that potential drug interactions, n = 43 (86%); the patient taking multiple medications, n = 48 (96%); and lack of acceptable alternatives, n = 38 (76%), were barriers to appropriate prescribing. Approximately 50% (n = 42) of the residents surveyed reported never hearing about (16.7%) or never using (35.7%) the Beers Criteria. Of the respondents who reported use (n = 20), the large majority reported it as rarely used or sometimes used, 65% and 30%, respectively.
Figure 1.
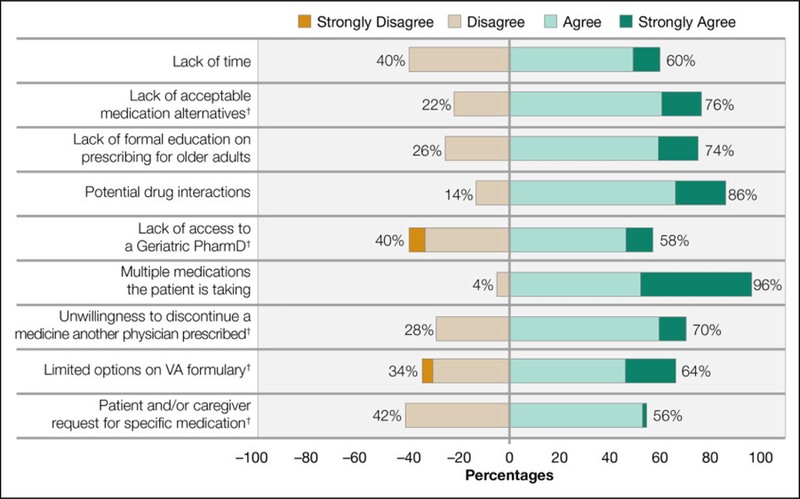
Reported barriers to appropriate prescribing by physician residents in the emergency department.
†Incorrect survey selection by n = 1 respondent, values will not add to 100%.
Abbreviations: PharmD, doctor of pharmacy; VA, Veteran affairs.
Figure 2 shows the pre- and postintervention questionnaire responses on physician resident–rated confidence in appropriate prescribing behaviors in the older adult. A significantly greater proportion of residents agreed and strongly agreed in their confidence to identify drug–disease interactions (pre- 80% and post-100%; P = .0053) and in their ability to prescribe the appropriate medication for the older adult (90% vs 100%; P = .025) after receiving the educational intervention. Additionally, residents before receiving the education intervention were more likely to strongly disagree or disagree with routine use of the Beers Criteria when prescribing in the ED for older adults (86%). After the educational intervention, residents were significantly more likely to agree or strongly agree that they routinely consulted with the Beers Criteria when prescribing medications in the ED for older adults (14% vs 66%; P < .0001).
Figure 2.
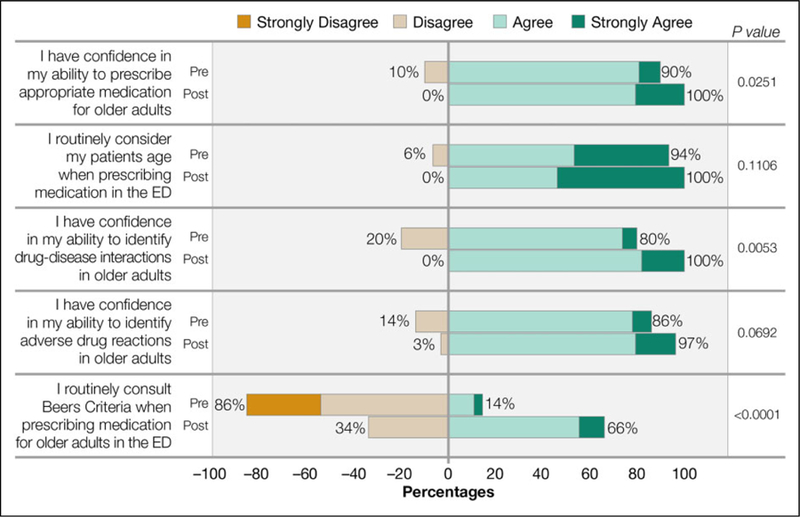
Pre- and postintervention questionnaire for resident confidence in prescribing for older adults.
Abbreviations: ED, emergency department.
PIM Rates
From July 2012 to February 2013, n = 67 physician residents who did not receive the educational intervention prescribed a total of 6082 medications to 2500 adults over 65 years of age treated and released from the ED; 510 of these medications were identified as PIMs. A total of 4966 medications were prescribed to 3162 adults over 65 years of age treated and released from the ED by n = 63 internal medicine residents who received the education intervention; 286 of these medications were identified as PIMs.
Figure 3 shows the monthly PIM rates for both the untrained and trained resident cohorts from July 2011 to December 2014. The Poisson regression model shows the resident cohort who received the educational intervention were less likely to prescribe a PIM when compared to the untrained resident cohort (rate ratio = 0.73, 95% confidence interval = 0.632–0.850; P < .0001). Table 1 shows the most common PIMs prescribed by physician residents with similar PIMs prescribed in the cohort who received the intervention and the cohort who did not. Although the types of PIMs were similar in each group, physician residents who received the intervention were less likely to prescribe cyclobenzaprine, naproxen, and ibuprofen when compared to the untrained cohort.
Figure 3.
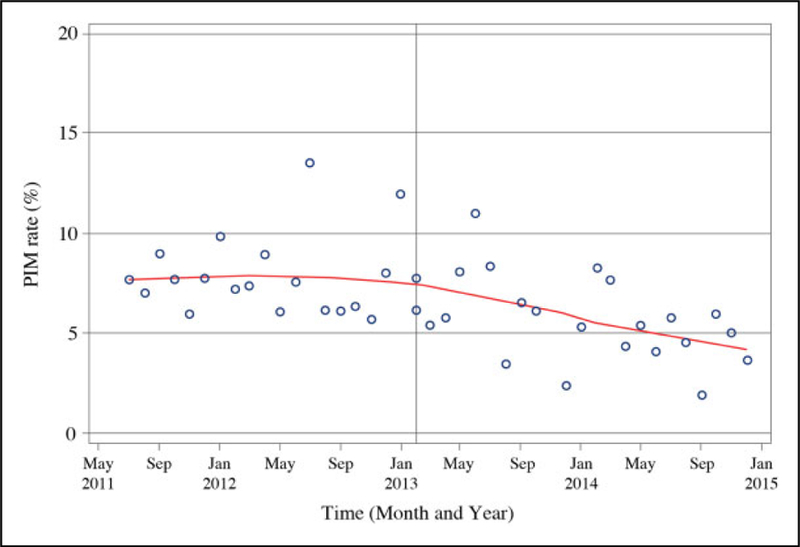
Potentially inappropriate medication (PIM) rates by month. Loess regression curve generated from PIM rates. The solid line at the February 2013 timepoint indicates when the EQUiPPED academic detailing started.
Abbreviations: PIM, potentially inappropriate medications; EQUiPPED, Enhancing Quality of Prescribing Practices for Veterans Discharged from the Emergency Department.
Table 1.
Most Common Potentially Inappropriate Medications (PIMs) Prescribed by Physician Residents.
| PIMa | Untrained Residents (Denominator = 6082 Total Prescriptions), % (n) | Trained Residents (Denominator = 4966 Total Prescriptions), % (n) | Rate Ratio (95% CI) | P Value |
|---|---|---|---|---|
| Cyclobenzaprine | 2.33 (142) | 0.97 (48) | 0.414 (0.300–0.573) | <.0001 |
| Naproxen | 1.59 (97) | 0.36 (18) | 0.227 (0.138–0.375) | <.0001 |
| Ibuprofen | 1.40 (85) | 0.32 (16) | 0.231 (0.135–0.393) | <.0001 |
| Hydroxyzine | 0.38 (23) | 0.28 (14) | 0.746 (0.384–1.40) | 0.38 |
| Diphenhydramine | 0.39 (24) | 0.22 (11) | 0.561 (0.275–1.15) | 0.107 |
| Methocarbamol | 0.38 (23) | 0.22 (11) | 0.586 (0.286–1.20) | 0.140 |
Abbreviation: CI, confidence interval.
PIM/total medications.
Discussion
This report describes the impact of the EQUiPPED intervention on physician residents at a VA ED and on physician residents’ confidence in their ability to prescribe medications in an older adult ED population and routine use of Beers criteria. The educational intervention had the largest impact on the residents’ confidence in their abilities to identify drug–disease interactions, selecting the appropriate medication, and routine consultation of the Beers Criteria when prescribing in the ED for older adults. Additionally, residents who received the educational intervention prescribed a lower rate of PIMs compared to a cohort who did not receive the intervention. Our findings reinforce the importance of focused education in resident prescribers on the avoidance of PIMs using explicit criteria and that an improvement in residents’ self-rated confidence in geriatric prescribing is associated with a lower rate of PIMs.
Educational interventions that impact prescribing practices have been delivered in other therapeutic topics to physician residents such as pain management26; however, our report is unique in demonstrating the use of academic detailing to decrease PIM prescribing in an ED environment. Curricula comprised of geriatric medicine principles delivered to EM residents may include a component related to pharmacodynamics of aging; however, there is little previous literature regarding the specific details of the medication components or the impact of educational interventions on the quality of prescribing. In 1 study, 29 EM residents received a geriatric curriculum over 1 year comprised of didactic lectures and simulations that included principles of medication management.27 Geriatric knowledge increased; however, data were not included regarding the impact of the curriculum on medication prescribing behavior. In another study, EM residents who attended a lecture focused on geriatric competencies and completed a didactic test showed an improvement related to knowledge; however, no prescribing data were available.15 Our data show that focused education on prescribing habits not only increases confidence but also shows an impact on prescribing rates.
Approximately 50% of the residents surveyed reported never hearing about or never using the Beers Criteria, which is an alarming finding given that residents will prescribe medications for many older adults. Our results, however, show that focused education for residents delivered at the beginning of the rotation with targeted feedback on prescribing practices throughout is not only feasible but can also have a significant impact on prescribing behaviors. Clinical teaching can be challenging in a highly dynamic environment treating patients with a high acuity of severe illness. This point is reinforced with data that suggest medical residents’ prescribing behaviors are not influenced by practicing under the supervision of an attending physician.28 Additionally, studies have shown that a large proportion of physicians are unaware of PIMs and explicit criteria to guide prescribing.25 Our educational intervention offers a model to overcome the above-identified barriers by providing targeted education to increase confidence and impact prescribing behaviors in residents. A study showed similar results by identifying gaps in prescribing medications in chronic pain and found that educational interventions increased knowledge and confidence resulting in increased confidence in prescribing in that area in the medical resident.29
Academic detailing is a useful quality improvement strategy to improve prescribing practices. This educational practice involves an experience detailer who provides individualized feedback on the prescriber’s clinical practice through direct education. A Cochrane review in 2007 showed academic detailing alone or as part of a multifaceted intervention improved prescribing practices.30 Our described academic detailing approach was similar to other published models that have focused on inappropriate prescribing in an older adult population with the exception of using an innovative geriatrician–CPS pair as the detailers. The majority of these studies were conducted within a nursing home population and utilized an academic detailing intervention that consisted of both individualized and group detailing sessions along with distributed educational materials.31–34 Academic detailing models have been described with a pharmacist and physician as detailers but not providing detailing sessions as a pair.35–37
Our study has considerations and limitations that should be noted. First, while all physician residents received academic detailing, those residents who received the academic detailing later in the project were exposed to components of the intervention that residents may not have been exposed to early on. Second, although our results showed a decline in the number of PIMs prescribed, our study did not seek to demonstrate whether the reduction in PIMs had an impact on other meaningful clinical outcomes. There are robust data from previous trials that have linked PIMs to meaningful clinical outcomes such as predictors of ADRs,38 reduced hospital length of stay,39 and reduced hospitalizations.40 Third, our impact to improve confidence was assessed over a short period time, and therefore, further research needs to elucidate whether or not our findings are sustained over a longer period of time to determine whether improvement of prescribing patterns hold. Fourth, given the initial quality improvement design of this project, we were unable to control for confounding variables that could have impacted the PIM rates after the physician residents received education. Finally, fewer physician residents completed the questionnaire after receiving the academic detailing compared to those completing the questionnaire prior to academic detailing. This could have resulted in residents who did not have improved confidence to not complete the questionnaire.
Conclusion
The results of this report demonstrate that academic detailing in physician residents delivered by a physician–pharmacist pair was associated with a decrease in PIM prescribing practices. These improvements were associated with an increase in physician residents’ knowledge and confidence related to geriatric prescribing and the Beers Criteria. Early targeting of medical residents at the beginning of their ED rotation is feasible and serves as model for other residency programs.
Acknowledgments
The authors would like to acknowledge Sherman Lee for editorial support.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding was provided by the Department of Veterans Affairs Office of Geriatrics and Extended Care T-21 initiative (G508-1 and G521-5). This work was also supported in part by the Center of Innovation for Health Services Research in Primary Care (CIN 13-410) at the Durham VA Health Care System. Dr Vaughan is supported by a Rehabilitation R&D CDA-2 award from the Department of Veterans Affairs 1 IK2 RX000747-01. Dr Hastings is supported by the Duke Claude D. Pepper Older Americans Independence Center NIA grant (P30AG028716).
Appendix A. Resident Questionnaire
Thank you for participating in our educational session. Please respond to the following questions regarding appropriate medication prescribing in older adults. For the purposes of this survey, an older adult refers to patients 65 years and older. Your results will be kept confidential and will not be used to influence any evaluation of your clinical performance.
With respect to your CURRENT clinical practice, please indicate how often you use the Beers Criteria to guide medication prescribing in your older adult emergency department (ED) patients.
| Often Use | Sometimes Use | Rarely Use | Know of but Never Use | Never Heard of |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
With respect to your CURRENT clinical practice, please indicate the extent to which you agree or disagree with the following statements.
| Strongly Disagree | Strongly Agree | Agree | Disagree | |
|---|---|---|---|---|
| I have confidence in my ability to prescribe appropriate medications for older adults | 1 | 2 | 3 | 4 |
| I routinely consider my patient’s age when prescribing medications in the ED | 1 | 2 | 3 | 4 |
| I have confidence in my ability to identify drug–disease interactions in older adults | 1 | 2 | 3 | 4 |
| I have confidence in my ability to identify adverse drug reactions in older adults | 1 | 2 | 3 | 4 |
| I routinely consult Beers Criteria when prescribing medications for older adults in the ED | 1 | 2 | 3 | 4 |
Please indicate the extent to which you agree or disagree that the following are BARRIERS to appropriate prescribing in older adults.
| Strongly Disagree | Strongly Agree | Agree | Disagree | |
|---|---|---|---|---|
| Lack of time | 1 | 2 | 3 | 4 |
| Lack of acceptable medication alternatives | 1 | 2 | 3 | 4 |
| Lack of formal education on prescribing for older adults | 1 | 2 | 3 | 4 |
| Potential drug interactions | 1 | 2 | 3 | 4 |
| Lack of access to a geriatric PharmD | 1 | 2 | 3 | 4 |
| Multiple medications the patient is taking | 1 | 2 | 3 | 4 |
| Unwillingness to discontinue a medicine another physician prescribed | 1 | 2 | 3 | 4 |
| Patient and/or caregiver request for specific medication | 1 | 2 | 3 | 4 |
Thank you!
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Institute of Medicine. Retooling for an Aging America: Building the Healthcare Workforce Washington, DC: Institute of Medicine; 2008. [Google Scholar]
- 2.Education in Geriatric Medicine. AGS education committee and public policy advisory group (PPAG). J Am Geriatr Soc 2001; 49(2):223–224. [PubMed] [Google Scholar]
- 3.Keller I, Makipaa A, Kalenscher T, et al. Global Survey on Geriatrics in the Medical Curriculum Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 4.The American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American geriatrics society updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2015;63(11):2227–2246. [DOI] [PubMed] [Google Scholar]
- 5.Caterino JM, Emond JA, Camargo CA Jr. Inappropriate medication administration to the acutely ill elderly: a nationwide emergency department study, 1992–2000. J Am Geriatr Soc 2004; 52(11):1847–1855. [DOI] [PubMed] [Google Scholar]
- 6.Koyama A, Steinman M, Ensrud K, et al. Long-term cognitive and functional effects of potentially inappropriate medications in older women. J Gerontol A Biol Sci Med Sci 2014;69(4):423–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thorpe JM, Thorpe CT, Kennelty KA, et al. The impact of family caregivers on potentially inappropriate medication use in noninstitutionalized older adults with dementia. Am J Geriatr Pharmacother 2012;10(4):230–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coombes ID, Mitchell CA, Stowasser DA. Safe medication practice: attitudes of medical students about to begin their intern year. Med Educ 2008;42(4):427–431. [DOI] [PubMed] [Google Scholar]
- 9.Illing JC, Morrow GM, Rothwell nee Kergon CR, et al. Perceptions of UK medical graduates’ preparedness for practice: a multi-centre qualitative study reflecting the importance of learning on the job. BMC Med Educ 2013;13:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kostas T, Zimmerman K, Salow M, et al. Improving medication management competency of clinical trainees in geriatrics. J Am Geriatr Soc 2014;62(8):1568–1574. [DOI] [PubMed] [Google Scholar]
- 11.Chin MH, Wang LC, Jin L, et al. Appropriateness of medication selection for older persons in an urban academic emergency department. Acad Emerg Med 1999;6(12):1232–1242. [DOI] [PubMed] [Google Scholar]
- 12.Hustey FM, Wallis N, Miller J. Inappropriate prescribing in an older ED population. Am J Emerg Med 2007;25(7):804–807. [DOI] [PubMed] [Google Scholar]
- 13.Meurer WJ, Potti TA, Kerber KA, et al. Potentially inappropriate medication utilization in the emergency department visits by older adults: analysis from a nationally representative sample. Acad Emerg Med 2010;17(3):231–237. [DOI] [PubMed] [Google Scholar]
- 14.Hastings SN, Schmader KE, Sloane RJ, et al. Quality of pharmacotherapy and outcomes for older veterans discharged from the emergency department. J Am Geriatr Soc 2008;56(5):875–880. [DOI] [PubMed] [Google Scholar]
- 15.Hogan TM, Hansoti B, Chan SB. Assessing knowledge base on geriatric competencies for emergency medicine residents. West J Emerg Med 2014;15(4):409–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leipzig RM, Granville L, Simpson D, et al. The Future of Geriatric Care in Our Nation’s Emergency Departments: Impact and Implications Dallas, TX: American College of Emergency Physicians; 2008. [Google Scholar]
- 17.Hogan TM, Losman ED, Carpenter CR, et al. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med 2010;17(3):316–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geriatric Emergency Department Guidelines. Ann Emerg Med 2014;63(5):e7–e25. [DOI] [PubMed] [Google Scholar]
- 19.Stevens M, Hastings SN, Powers J, et al. Enhancing the quality of prescribing practices for older veterans discharged from the emergency department: preliminary results from EQUiPPED, a novel multi-component interdisciplinary quality improvement initiative. J Am Geriatr Soc 2015;63(5):1025–1029. [DOI] [PubMed] [Google Scholar]
- 20.Hastings SN, Vaughan CP, Stevens M, et al. Invited commentary—research and operations: joining forces to improve care for veterans. N C Med J 2015;76(5):315–319. [DOI] [PubMed] [Google Scholar]
- 21.Moss J, Bryan W, Wilkerson LM, et al. Impact of clinical pharmacy specialists on the design and implementation of a quality improvement initiative to decrease inappropriate medications in a veterans affairs emergency department. J Manag Care Spec Pharm 2016;22(1):74–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vandenberg AE, Vaughan CP, Stevens M, et al. Improving geriatric prescribing in the ED: a qualitative study of facilitators and barriers to clinical decision support tool use. Int J Qual Health Care 2016;29(1):117–123. [DOI] [PubMed] [Google Scholar]
- 23.Vandenberg A, Stevens M, Echt K, et al. Implementation of a medication management program across 5 VA emergency departments. Fed Pract 2016;33(4):29–32. [PMC free article] [PubMed] [Google Scholar]
- 24.Kessler C, Chen J, Dill C, et al. State of affairs of emergency medicine in the Veterans Health Administration. Am J Emerg Med 2010;28(8):947–951. [DOI] [PubMed] [Google Scholar]
- 25.Ramaswamy R, Maio V, Diamond JJ, et al. Potentially inappropriate prescribing in elderly: assessing doctor knowledge, confidence, and barriers. J Eval Clin Pract 2011;17(6):1153–1159. [DOI] [PubMed] [Google Scholar]
- 26.Ury WA, Rahn M, Tolentino V, et al. Can a pain management and palliative care curriculum improve the opioid prescribing practices of medical residents? J Gen Intern Med 2002;17(8): 625–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Biese KJ, Roberts E, LaMantia M, et al. Effect of a geriatric curriculum on emergency medicine resident attitudes, knowledge, and decision-making. Acad Emerg Med 2011;18 suppl 2: S92–S96. [DOI] [PubMed] [Google Scholar]
- 28.Ryskina KL, Dine CJ, Kim EJ, et al. Effect of attending practice style on generic medication prescribing by residents in the clinic setting: an observational study. J Gen Intern Med 2015;30(9): 1286–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fox AD, Kunins HV, Starrels JL. Which skills are associated with residents’ sense of preparedness to manage chronic pain? J Opioid Manag 2012;8(5):328–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Brien MA, Rogers S, Jamtvedt G, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database of Syst Rev 2007;(4):CD000409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Avorn J, Soumerai SB, Everitt DE, et al. A randomized trial of a program to reduce the use of psychoactive drugs in nursing homes. N Engl J Med 1992;327(3):168–173. [DOI] [PubMed] [Google Scholar]
- 32.Crotty M, Whitehead C, Rowett D, et al. An outreach intervention to implement evidence based practice in residential care: a randomized controlled trial. BMC Health Serv Res 2004;4(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schmidt I, Claesson CB, Westerholm B, et al. The impact of regular multidisciplinary team interventions on psychotropic prescribing in Swedish nursing homes. J Am Geriatr Soc 1998; 46(1):77–82. [DOI] [PubMed] [Google Scholar]
- 34.van Eijk MEC, Avorn J, Porsius AJ, et al. Reducing prescribing of highly anticholinergic antidepressants for elderly people: randomized trial of group vs individual academic detailing. BMJ 2001; 322(7287):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Solomon DH, Van Houten L, Glynn RJ, et al. Academic detailing to improve use of broad-spectrum antibiotics at an academic medical center. Arch Intern Med 2001;161(15):1897–1902. [DOI] [PubMed] [Google Scholar]
- 36.Kisuule F, Wright S, Barreto J, et al. Improving antibiotic utilization among hospitalists: a pilot academic detailing project with a public health approach. J Hosp Med 2008;3(1): 64–70. [DOI] [PubMed] [Google Scholar]
- 37.Majumdar SR, Guirguis LM, Toth EL, et al. Controlled trial of a multifaceted intervention for improving quality of care for rural patients with type 2 diabetes. Diabetes Care 2003;26(11): 3061–3066. [DOI] [PubMed] [Google Scholar]
- 38.Chang CM, Liu PY, Yang YH, et al. Use of the Beers criteria to predict adverse drug reactions among first-visit elderly outpatients. Pharmacotherapy 2005;25(6):831–838. [DOI] [PubMed] [Google Scholar]
- 39.Corbi G, Gambassi G, Pagano G, et al. Impact of an innovative educational strategy on medication appropriate use and length of stay in elderly patients. Medicine (Baltimore) 2015;94(24):e918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pitkala KH, Juola AL, Kautiainen H, et al. Education to reduce potentially harmful medication use among residents of assisted living facilities: a randomized controlled trial. J Am Med Dir Assoc 2014;15(12):892–898. [DOI] [PubMed] [Google Scholar]


