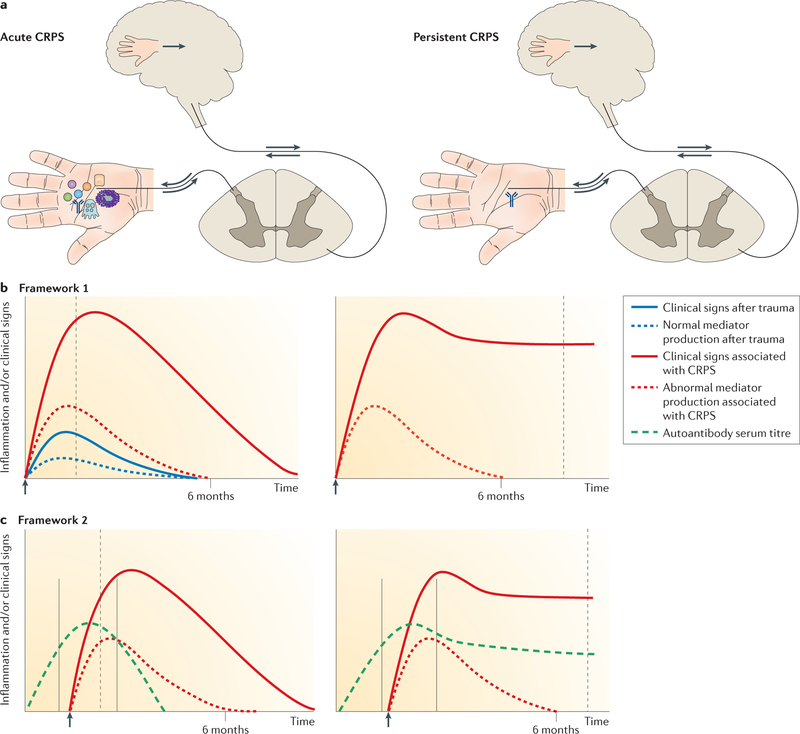
Figure 1. Hypothetical conceptual frameworks for CRPS.
a | Schematic representations of acute and persistent complex regional pain syndrome (CRPS). Proximally pointing arrows indicate signalling in response to distal excitation, and distally pointing arrows indicate descending signals leading to neuropeptide secretion and neurogenic inflammation. The depicted events correspond to the time points indicated by dashed grey lines in the graphs. b | Framework 1: augmented (neuro) immune activation. After injury (arrow), inflammatory mediators are produced by mast cells, sensory nerves, keratinocytes and osteocytes (represented by symbols in part a). In acute CRPS, mediator production is temporarily increased, triggering augmented post-traumatic clinical signs and primary afferent sensitization and leading to segmental spinal cord dorsal horn sensitization and sometimes a shift in the cortical representation of the affected limb with abnormal limb perception. Mediators and clinical signs normalize by about 6 months. In persistent CRPS, local production of inflammatory mediators at the affected limb normalizes and CNS changes now drive the clinical picture. In this framework, CRPS-associated autoantibodies might contribute to some clinical signs, such as sweating, but do not explain the main symptoms of pain and hypersensitivity. c | Framework 2: autoantibodies. If distal limb trauma is sustained during a time window of vulnerability characterized by high autoantibody production (solid grey lines), an enhanced trauma-induced inflammatory response renders these antibodies locally pathogenic, resulting in augmented post-traumatic signs. Autoantibodies might bind to neurons, causing afferent sensitization through changes in the transduction or transmission properties of these cells, or to perineural cells, which then release pronociceptive molecules (not shown). These autoantibodies are noninflammatory; that is, they neither activate complement nor attract immune cells. Acute CRPS resolves after cessation of autoantibody production. A small group of patients develops persistent CRPS, in which autoantibody production continues at a reduced rate that is still sufficient to sustain the clinical phenotype.