Abstract
Although studies document an association between Attention-Deficit/Hyperactivity Disorder (ADHD) and social problems, little is known about mediating or moderating mechanisms underlying this association. We examined whether, among youth, emotion dysregulation (ED) mediates the negative association between ADHD and social skills, and whether this mediational process is moderated by symptoms of depression. A total of 171 youth with ADHD (76% male; Mage = 12.15, SD = 0.95) and their parents completed measures of ED, depression, and social skills. Results indicated that, after controlling for oppositional defiant disorder, the negative association between ADHD and social skills was mediated by ED. Further, this indirect effect was relevant for youth with non-clinical and subclinical levels of depression but not for those with clinical levels of depression. These findings underscore the importance of ED in the association between ADHD and social functioning among youth and suggest a need for additional research to understand how and when ED impacts such functioning.
Keywords: ADHD, social skills, emotion dysregulation, emotion regulation, depression
Considering the areas of impairment commonly associated with Attention-Deficit/Hyperactivity Disorder (ADHD), impairments in the social domain are among the most pervasive and persistent (Hoza, 2007). Compared to youth without ADHD, those with the disorder have more difficulties in their interpersonal relationships (Cunningham & Barkley, 1979; Hoza, 2007), including being less well-liked and more often rejected by peers (e.g., Guevremont & Dumas 1994; Hoza et al., 2005) and experiencing higher levels of family conflict (Biederman, Faraone, & Monuteaux, 2002). Moreover, social problems among individuals with ADHD persist throughout adolescence and into adulthood (Bagwell et al., 2001; Barkley, 2008), likely contributing to long-term negative outcomes. These impairments underscore the importance of better understanding factors that influence and sustain social problems among youth with ADHD so as to inform the development of targeted intervention programs.
Among the factors that contribute to social problems among youth with ADHD, emotion dysregulation (ED) has been a recent target of theoretical and empirical attention (e.g., Barkley, 2010; Bunford, Evans, & Langberg, 2014; Maegden & Carlson, 2000; Melnick & Hinshaw, 2000; Musser et al., 2011, 2013; Nigg et al., 2004; Seymour et al., 2012, 2014). ED, when associated with ADHD, involves two deficits. First, an inhibitory deficit that manifests in socially inappropriate behavioral responses associated with a strong emotional reaction to a stimulus; and second, a self-regulatory deficit that manifests in an inability to (1) self-soothe physiologic arousal induced by strong emotion, (2) refocus attention, and (3) organize the self for coordinated action in the service of a goal (Barkley, 2010)1. Indeed, findings of empirical studies indicate that, relative to typical peers, youth with ADHD exhibit behaviors consistent with ED (e.g., Scime & Norvilitis, 2006; Sjöwall, et al., 2012). In turn, ED is associated with social problems among youth with ADHD (Bunford et al., 2014; Maegden & Carlson, 2000; Melnick & Hinshaw, 2000), including peer rejection (Henker & Whalen, 1989; Landau & Moore, 1991) and social skills deficits (Kats-Gold et al., 2007; Singh et al., 1998). Thus, prior findings indicate that the social problems experienced by youth with ADHD may be partly attributable to ED.
Yet, research to date has been primarily focused on the direct association between ADHD and social problems. Mediating (i.e., mechanisms through which ADHD is negatively associated with social problems) and moderating (i.e., when the mediational relationships are relevant) mechanisms underlying this association have generally been untested. Examining these mechanisms is timely, especially with regard to obtaining an enhanced understanding of the etiology of social problems associated with ADHD as well as the development of targeted interventions (e.g., Kazdin & Nock, 2003). In the present study, we aimed to examine two questions: first, whether ADHD is associated with increased ED, which in turn is associated with poorer social skills; second, whether the negative direct and indirect association between ADHD and social skills is moderated by important comorbid symptoms, such as of depression.
Emotion Dysregulation as a Mediator
To determine whether ED may mediate the association between ADHD and social problems, it must be established first, that ED is associated with ADHD and second, that among youth with ADHD, ED is associated with social problems. Regarding an association between ED and ADHD, findings of experimental studies indicate that youth with ADHD are less likely to display constructive emotional coping2 or perceive themselves as able to regulate emotions (Scime & Norvilitis, 2006) and more likely to exhibit behavioral signs of negative or frustrated emotions (Melnick & Hinshaw, 2000; Walcott & Landau, 2004) than typically developing peers.
With regard to an association between ED and social problems among youth with ADHD, there is evidence that deficient emotion recognition is associated with social skills deficits3 (Singh et al., 1998) and manifestations of ED, such as low frustration tolerance, over-excitability to emotions, and slow return to emotional baseline (Barkley, 2010; Martel & Nigg, 2006) likely contribute to peer perceptions of youth with ADHD as disruptive, overly-exuberant, or annoying (Henker & Whalen, 1989; Landau & Moore, 1991). Among youth with ADHD, the association between ED and social problems may be particularly pertinent as children develop into young adolescents. First, impairments associated with ADHD persist and may worsen during this developmental period (Wolraich et al., 2005). Second, although young adolescents are expected to develop increasingly sophisticated emotion regulation skills, adults’ expectations for self-regulation often exceed the capabilities of many youth to effectively regulate their emotions (Steinberg, 2005), creating a gap between adult expectations and youth development. This gap may be particularly relevant and impairing for youth with a psychopathology, including ADHD. Indeed, our recent research indicates that, depending on the way in which ED is indexed, 4–35% of young adolescents with ADHD exhibit some manifestation of ED (Bunford et al., 2014). Further, among young adolescents with ADHD, three aspects of ED are associated with social skills impairment, above and beyond the contributions of co-morbid oppositional defiant disorder (ODD; Bunford et al., 2014). These include emotional inflexibility and slow return to emotional baseline; a low threshold for emotional excitability, impatience, and socially inappropriate behaviors; and difficulty in behavioral control in the face of strong emotions. Thus, the hitherto reviewed findings indicate that ED is associated with ADHD; that, among youth with the disorder, ED is associated with social problems; and that these associations may be particularly relevant for children as they mature into their adolescent years. Therefore, ED is a viable candidate for a mediator between ADHD and social skills impairment. Accordingly, we propose the following hypothesis: Hypothesis 1: ED will mediate the negative association between ADHD and social skills among youth.
Depression as a Moderator
Our second aim was to examine whether the negative direct and indirect (through ED) association between ADHD and social skills is moderated by depression. To determine whether depression may moderate the direct association between ADHD and social problems, it must be established that ADHD and depression co-occur and that, among youth with ADHD, different levels of depression correspond to different levels of social problems. With regard to the co-occurrence of symptoms of ADHD and depression, it has been estimated as high as 75% and prior research indicates that 20–30% of youth with ADHD have co-morbid major depressive disorder (MDD) (Daviss et al., 2009; Elia et al., 2008; Chronis-Tuscano et al., 2010).
Regarding different levels of depression corresponding to different levels of social problems, findings indicate that among the internalizing disorders that co-occur with ADHD, MDD is more often associated with problems in functioning than others. For example, some results indicate that symptoms of depression, but not anxiety, exacerbate the association between symptoms of ADHD and social problems (Becker, Langberg, Evans, Girio-Herrera, & Vaughn, 2014). In addition, among youth with ADHD, MDD is associated with more severe impairments and poorer developmental outcomes than those associated with either disorder alone (Daviss, 2008). As a result, youth with ADHD and co-morbid MDD experience more psychosocial and family problems than youth with ADHD alone and the co-occurrence of symptoms of ADHD and depression necessitates more intensive interventions (e.g., McQuade et al., 2011). These findings indicate that depression is a viable candidate for a moderator of the direct association between ADHD and social problems.
To determine whether depression may moderate the negative indirect association between ADHD and social problems through ED, it must be established that ED and depression co-occur and that, among youth with ADHD, the effect of ED on social problems varies as a function of depression. Prior findings indicate that ED is associated with, and predates the development of, depression in youth (e.g., Durbin & Shafir 2008; Feng et al., 2009; Tortella-Feliu et al., 2010). Recently, Seymour et al. (2012; 2014) examined whether ED mediates the association between ADHD and symptoms of depression among youth with and without ADHD in a cross-sectional study of youth aged 10–14 years and whether ED mediates the association between symptoms of ADHD and symptoms of depression in a longitudinal study among youth 9–12 years. Seymour et al.’s findings indicate that, relative to those without, youth with ADHD experienced heightened rates of both ED and symptoms of depression (Seymour et al., 2012). In addition, ED mediated the association between ADHD and symptoms of depression (Seymour et al., 2012; 2014), above and beyond ODD (Seymour et al., 2014). Thus, given that ED has been shown to predate the development of depression and mediate the association between ADHD and depression, it is reasonable to conceptualize depression not as a mediator of the association between ADHD and ED but, rather, as a moderator of this relationship. Nevertheless, it remains unclear whether, among youth with ADHD, the effect of ED on social problems varies as a function of depression.
In addition, the nature of the proposed interactions are unclear, as no investigators have examined whether the direct or indirect (through ED) association between ADHD and social skills impairment is moderated by depression. As per one perspective on the relationship among multiple risk factors and associated outcomes, one risk factor confers disadvantages, and this negative effect is especially potent among individuals who are at high levels of another risk factor (Wang et al., 2009). Per this model, the detrimental effect of both ADHD and ED would be more potent for youth with high rather than low levels of depression. A different perspective, however, indicates that if an individual is significantly impaired due to one risk factor, another risk factor will not incrementally contribute to further impairment. Per this conceptualization, the detrimental effect of both ADHD and ED would be more potent for youth with low rather than high levels of depression. We thus propose the following exploratory hypothesis: Hypothesis 2: Depression will moderate the negative direct and indirect association between ADHD and social skills. These direct and indirect associations may either be significant among youth with low depression but weaker among those with high depression, or be significant among youth with high depression but weaker among those with low depression.
The Present Study
In sum, the present study links hitherto largely disconnected bodies of research to examine mechanisms through which ADHD is associated with social skills impairment. Particularly, our overarching purpose was to examine the way in which ADHD, ED, and depression are associated with social skills impairment. To this end, our specific goals were twofold. First, we aimed to examine whether ED mediates the negative association between ADHD and social skills. Second, we aimed to test whether this relationship is moderated by depression. In line with our first aim, our first hypothesis is that ED will mediate the negative association between ADHD and social skills among youth. Our second hypothesis is that depression will moderate the negative direct and indirect association between ADHD and social skills. Our second hypothesis implies a “moderated mediation” model wherein the mediational mechanism responsible for the association between the predictor and the outcome depends on levels of the moderator (Hayes, 2013). Testing this model, we address questions about both how ADHD is associated with social skills impairment (i.e., mediation) and when such mediational relationship is most potent (i.e., moderation).
In all analyses, per prior findings, we investigated mediation and moderated mediation using three indices of ED, emotional inflexibility and slow return to emotional baseline (ERICA Self-Awareness subscale); a low threshold for emotional excitability, impatience, and socially inappropriate behaviors (ERICA Emotional Control subscale); and behavioral control in the face of strong emotions (DERS Impulse subscale). Given prior findings indicating that ODD is correlated both with ADHD and with ED (see Barkley, 2010, for a review), we included ODD as a control variable in all analyses. Of note, our analyses are based on cross-sectional data.
Method
The data analyzed in this study were collected in the context of a randomized controlled trial. Participants’ parents completed measures of ADHD symptoms during baseline assessments, prior to being assigned to treatment condition and participants and their parents completed rating scales of social skills, ED, and depression at post-treatment.
Participants.
Participants were 171 youth (76% males) who were recruited at two sites and from seven public middle schools. One-third of the participants were randomized to a community care condition and the other two-thirds were randomly assigned to one of two treatment conditions. Participants were between the ages of 10 and 14 years (Mage = 12.15, SD = 0.95) and the majority were Caucasian (77.2%), followed by African American (11.6%), biracial (9.4%), and other ethnicities (1.8%). Inclusionary criteria were: (a) attendance at one of the participating middle schools; (b) meeting diagnostic criteria for at least one subtype of ADHD, (c) demonstrating academic or social impairment and (d) an IQ of 80 or above on a shortened test of cognitive ability (i.e., Wechsler Intelligence Scale for Children, Fourth Edition, [Wechsler, 2003]); and (e) not meeting diagnostic criteria for pervasive developmental, bipolar, or obsessive-compulsive disorder, psychosis, or substance dependence other than tobacco.
Diagnoses were established using the Children’s Interview for Psychiatric Syndromes (P-ChIPS), a semi-structured diagnostic interview administered to the child’s parent(s). For ADHD specifically, in addition to the P-ChIPS, parent- and teacher-reported symptoms were collected using the Disruptive Behavior Disorders Rating Scale (DBD) and functional impairment was measured using the Impairment Rating Scale (IRS). Symptoms were considered present if endorsed by either a parent or teacher, with subtype determinations made based on parent endorsement of at least four of the necessary six symptoms. Final ADHD diagnosis decisions were made by unanimous agreement between two psychologists. For a summary of participants’ psychiatric diagnoses, estimated IQ, and family income across grade levels, see Table 1.
Table 1.
Demographic Characteristics of the Sample
| Variable | 5th | 6th | 7th | 8th |
|---|---|---|---|---|
| Grade (%) | 1 | 30 | 40 | 30 |
| ADHD-I (N) | 1 | 20 | 31 | 37 |
| ADHD-C (N) | 0 | 31 | 39 | 15 |
| MDD | 0 | 1 | 4 | 3 |
| ODD | MDD | Any Anxiety | ||
| Comorbidity (%) | 95 | 18 | 27 | |
| M | SD | Min | Max | |
| IQ (WISC-IV) | 96.08 | 12.65 | 81 | 137 |
| M | SD | Min | Max | |
| Family Income ($) | 58,611 | 49,587 | 5,000 | 225,000 |
| M | SD | Min | Max | |
| Mother Education (years) | 14.02 | 2.29 | 8 | 18 |
| M | SD | Min | Max | |
| Father Education (years) | 13.66 | 2.49 | 8 | 18 |
Note: Our sample was representative of youth with ADHD in terms of comorbidity status, such as ODD (Biederman, Newcorn, & Sprich, 1991), any mood disorder (Biederman, et al., 1992), and any anxiety disorder (Wilens, et al., 2002). Our sample was representative of our state census with regard to household income and parental education (United States Census Bureau of 2011).
ADHD-I = Attention-Deficit/Hyperactivity Disorder, Inattentive Subtype; ADHD-HI = Attention-Deficit/Hyperactivity Disorder, Hyperactive-Impulsive Subtype; ADHD-C = Attention-Deficit/Hyperactivity Disorder, Combined Subtype; ODD = Oppositional Defiant Disorder (measured by the PChIPS); MDD = Major Depressive Disorder (measured by the RADS-2); Any Anxiety = (any anxiety disorder measured by the PChIPS); WISC-IV = Wechsler Intelligence Scale for Children, Fourth Edition.
No significant main or interaction effects were obtained on IQ or income across the 4 groups.
Procedures.
Recruitment flyers were mailed to all families with children attending participating middle schools during two consecutive school years. Primary caregivers (79% mothers) who responded to the flyers participated in a telephone screen to determine the likelihood of child eligibility. Parents and their children were scheduled to complete informed consent/assent procedures, followed by an evaluation if the parent reported either that the child had a prior diagnosis of ADHD or endorsed four or more symptoms of inattention. Families were involved in the study for one academic year, during which interventions took place, and six months afterward, for a follow-up phase.
Measures.
Measures used in this study were those employed in diagnostic decisions (i.e., P-ChIPS, DBD, and IRS) and two self-report questionnaires of ED, a self-report questionnaire of depression, and a parent- and self-report questionnaire of social skills.
Children’s Interview for Psychiatric Syndromes - Parent Version
(P-ChIPS; Weller, Weller, Rooney, & Fristad, 1999). The P-ChIPS is a semi-structured parent interview of 20 Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (APA, 2000) mental health disorders in youth ages 6–18 years. Adequate psychometric properties have been reported for the P-ChIPS, including moderate agreement among the P-ChIPS and clinician diagnoses (ĸ = 0.49) and average sensitivity of 87% and specificity of 76% (Fristad et al., 1998; Weller, Weller, Fristad, Rooney, & Schecter, 2000).
Disruptive Behavior Disorder Rating Scale
(DBD; Pelham, Gnagy, Greenslade, & Milich, 1992). The DBD Rating Scale is a measure of parent- and teacher-rated DSM-IV symptoms of ADHD, ODD, and conduct disorder (CD). The DBD consists of 45 items rated on a 4-point scale (0 = not at all present, 3 = very much present), with higher scores indicative of more severe symptoms. Scores for the entire scale range from 0 to 135, for the ADHD subscale from 0 to 54, for the ODD subscale from 0 to 24, and for the CD subscale from 0 to 84. The reliability and validity of the DBD is well-established (Pelham et al., 1992). In the present study, parents and teachers completed the DBD for diagnostic purposes.
Impairment Rating Scale
(IRS; Fabiano et al., 2006). The IRS is a parent- and teacher-report measure of areas of functioning in which children with ADHD are typically impaired. The parent version measures seven (relationship with peers, siblings, and parents; academic progress; self-esteem; family functioning; and overall impairment) and the teacher version measures six (relationship with peers and teacher, academic progress, self-esteem, classroom functioning, and overall impairment) domains. Raters rate youth on a continuum (0 = no problem/definitely does not need treatment, 6 = extreme problem/definitely needs treatment). As each item represents a unique domain, scores range from 0 to 6 per domain. Prior findings indicate excellent test-retest reliability and convergent and discriminant validity for the IRS (Fabiano et al., 2006) and that IRS scores discriminate between children whose parent- and teacher-rated ADHD symptoms are consistent with a DSM-IV diagnosis of ADHD and those whose ratings are not (Fabiano et al., 2006). In the present study, parents and teachers completed the IRS for diagnostic purposes. We used the IRS as a measure of impairment to inform diagnoses and used the recommended cutoff score of three or greater to establish impairment (see Fabiano et al., 2006).
Difficulties in Emotion Regulation Scale
(DERS; Gratz & Roemer, 2004). The DERS is a self-report measure of ED with 36-items rated on a 5-point scale (1 = almost never, 5 = almost always). Higher scores indicate greater ED. Subscales of the DERS are Nonacceptance of Emotional Responses (Nonacceptance), Difficulties Engaging in Goal-Directed Behavior (Goals), Impulse Control Difficulties (Impulse), Lack of Emotional Awareness (Awareness), Limited Access to Emotion Regulation Strategies (Strategies), and Lack of Emotional Clarity (Clarity). Scores for the total DERS range from 36 to 180. Good internal consistency and test–retest reliability, and adequate construct and predictive validity for the DERS have been demonstrated with multiple adolescent samples (e.g., Vasilev et al., 2009; Weinberg & Klonsky, 2009). In addition, robust correlations between the DERS and psychological problems reflecting ED (Weinberg & Klonsky, 2009) and physiological indices of ED (Vasilev et al., 2009) have been found. In the present study, the DERS demonstrated excellent internal consistency (α = .913). Per prior findings (Bunford et al., 2014) implicating the Impulse subscale in social skills impairment associated with ADHD, only this subscale were used in the analyses for this study.
Emotion Regulation Index for Children and Adolescents
(ERICA; MacDermott, Gullone, & Allen, 2010). The ERICA is a self-report measure of ED consisting of 16 items rated on a 5-point scale (1 = strongly disagree, 5 = strongly agree). Higher scores indicate better emotion regulation. Subscales of the ERICA are Emotional Control (Emotional Control), Emotional Self-Awareness (Self-Awareness), and Situational Responsiveness (Situational Responsiveness). Scores for the total ERICA range from 16 to 80. Good internal consistency, test-retest reliability, and convergent and construct validity for the ERICA has been demonstrated in a sample of 9–16 year olds (MacDermott et al., 2010). In the present study, the ERICA demonstrated good internal consistency (α = .801). Per prior findings (Bunford et al., 2014) implicating the Self-Awareness and Emotional Control subscales in social skills impairment associated with ADHD, these two subscales were used in the analyses for this study.
Reynolds Adolescent Depression Scale, Second Edition
(RADS-2; Reynolds, 2002). The RADS-2 is a self-report measure of depressive symptomatology that was developed specifically for use with adolescents, and consists of 30, 4-point Likert-type response format items (1 = almost never, 4 = most of the time). The RADS-2 is a measure of four dimensions of adolescent depression: dysphoric mood, anhedonia/negative affect, negative self-evaluation, and somatic complaints. Higher scores indicate more severe depressive symptoms. The RADS-2 demonstrated high internal consistency for the total depression scale (.93) and moderately high test-retest reliability for the subscales, ranging from .77 to .84 (Reynolds, 2002).
Social Skills Improvement System-RS
(SSIS-RS; Elliott & Gresham, 2008). The SSIS-RS is a teacher-, parent- and self-report measure of two domains of social functioning: social skills and problem behaviors. The Social Skills subscale is comprised of 46 items, with scores ranging from 0 to 138. The Problem Behaviors subscale is comprised of 29 items, with scores ranging from 0 to 87. Items are rated on a 4-point scale (0 = never, 3 = almost always). Norms and standardization sample information reveal acceptable subscale reliabilities and test-retest indices for the parent- and self-report forms (Gresham, Elliott, Vance, & Cook, 2011). For the present study, the SSIS-RS was completed by parents and by youth and only scores on the Social Skills subscale were used. Higher scores indicate better social skills.
Data preparation.
Eight participants failed to respond to one item each on our rating scale measures of ED. Mean-imputing based on participants’ average score on the subscale to which the item belongs was conducted. There was no pattern to missing data.
Preliminary analyses.
To examine whether being randomized to one of the three treatment conditions (i.e., a community care and two treatment conditions) had an effect on ED, depression, or social skills, a multivariate analysis of variance (MANOVA) was conducted to compare participants across groups on measures of ED (on each ED factor and the total score) as well as on depression and parent- and self-rated social skills. The omnibus test of condition was nonsignificant, F(12, 171) = 1.074, p = .386. To examine whether key demographic variables including gender and grade level, or diagnoses commonly comorbid with ADHD, including CD, or any anxiety disorder had an effect on ED, a MANOVA was conducted to compare participants across groups on measures of ED (on each ED factor and the total score). The omnibus tests of gender F(10, 171) = 1.781, p = .075, grade, F(10, 171) = 1.128, p = .346, CD, F(10, 171) = .749, p = .663, or any anxiety disorder, F(10, 171) = .647, p = .755 were all nonsignificant.
Although we used the continuous measure of social skills on the SSIS-RS in our analyses, descriptively, 10% and 9% of the sample exhibited well-below average and 35% and 13% exhibited below average parent- and self-rated social skills, respectively. We tested all models with both parent- and self-rated social skills. We present findings on models with parent-rated social skills; these were largely replicated with self-report social skills (data on models with self-rated social skills are available at ONLINE SUPPLEMENT). See Table 2 for bivariate correlations among all study variables.
Table 2.
Bivariate Correlations Among Main Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 ADHD | - | ||||||||||||||
| 2. ODD | .593† | - | |||||||||||||
| 3. DERS Total | −.002 | .125 | - | ||||||||||||
| 4. ERICA Total | .207** | −.011 | −.261** | - | |||||||||||
| DERS | |||||||||||||||
| 5. Nonacceptance | −.019 | .051 | .749† | −.047 | - | ||||||||||
| 6. Goals | .026 | .078 | .735† | −.060 | .474† | - | |||||||||
| 7. Impulse | .063 | .161* | .824† | −.201** | .552† | .575† | - | ||||||||
| 8. Awareness | −.015 | .023 | .455† | −.237** | .108 | .203** | .191* | - | |||||||
| 9. Strategies | .022 | .153* | .910† | −.226** | .696† | .625† | .751† | .219** | - | ||||||
| 10. Clarity | −.151* | .023 | .667† | −.482† | .326† | .324† | .434† | .455† | .567† | - | |||||
| ERICA | |||||||||||||||
| 11. Emotional Control | .249** | .054 | −.157* | .848† | .016 | .012 | −.145 | −.183* | −.105 | −.382† | - | ||||
| 12. Self-Awareness | .058 | −.124 | −.359† | .752† | −.157* | −.226** | −.205** | −.221** | −.364† | −.467† | .368† | - | |||
| 13. Situational Responsiveness | .104 | .005 | −.099 | .660† | .008 | .066 | −.119 | −.143 | −.084 | −.238** | .296† | .514† | - | ||
| 14. RADS-2: Depression | .021 | .128 | .573† | −.216** | .459† | .432† | .428† | .097 | .623† | .403† | −.032 | −.439† | −.106 | - | |
| 15. SSIS-RS: Parent Social Skills | −.415† | −.565† | −.025 | −.017 | −.021 | .028 | −.039 | .020 | −.066 | −.008 | −.181* | .183* | .101 | −.152* | - |
| 16. SSIS-RS: Self Social Skills | −.073 | −.112 | −.363† | .242** | −.111 | −.274† | −.467† | −.120 | −.355† | −.223** | −.012 | .413† | .330† | −.417† | .250** |
Note:
p < .05,
p < .01,
p < .001.
Analytic plan.
To test for mediation, we used a bootstrapping method with 1,000 bootstrap resamples (Hayes, 2013)4. For all significant simple mediational models, we tested the indirect effects of the alternative model (i.e., wherein the roles of the independent and mediator variables were reversed). For all models, tests of the alternative models were non-significant, indicating that only the models in the hypothesized direction were supported. We used PROCESS (Hayes, 2013) to test for moderated mediation. In all analyses, the ADHD variable corresponded to the total ADHD score as measured by the DBD. With regard to depression, a T score<61 falls within the normal range, T scores between 61–64 fall within the mild clinical depression range, T scores between 65–69 fall within the moderate clinical depression range, and T score>70 indicates severe clinical depression on the RADS-2. We conceptualized the normal range as non-clinical, the mild and moderate ranges as subclinical, and the clinical range as clinical. In all analyses, we controlled for ODD, by including it as a covariate in the models5. We included ODD in our analyses as a dimensional variable, as measured by the DBD. Of note, below we do not present data on effect sizes corresponding to the individual paths in our models and our results are presented as unstandardized regression coefficients, due to these modes of presentation being beyond the current state of the science when testing simple mediation with covariates or moderated mediation with covariates (Hayes, 2013).
Results
Hypothesis 1: ED Will Mediate the Negative Association between ADHD and Social Skills
To test whether ADHD is negatively associated with social skills through ED, we tested one, multiple-mediational model with ERICA Self-Awareness, ERICA Emotional Control and DERS Impulse as parallel mediators. Bootstrapping results of the omnibus effect supported our model (R2 = .384, F(5, 171) = 20.176, p < .001) and indicated that, jointly, ADHD and ERICA Self-Awareness, ERICA Emotional Control and DERS Impulse account for 38% of the variance in social skills. This effect was due to mediation by ERICA Self-Awareness (point estimate = .069; SE = .039; 95% CIs [.011, .175]) and Emotional Control (point estimate = −.072; SE = .040; 95% CIs [−.180, .015]). No mediation by DERS Impulse (point estimate = .001; SE = .014; 95% CIs [−.023, .039]) was observed. These findings suggest that ERICA Self-Awareness and Emotional Control are, but DERS Impulse is not a mediator of the negative association between ADHD and social skills.
A follow-up test of simple mediation with ERICA Self-Awareness as the mediator further supported our model (R2 = .352, F[2, 171] = 30.749, p < .001, point estimate = .045; SE = .029; 95% CIs [.004, .135]) and indicated that, jointly, ADHD and ERICA Self-Awareness account for 35% of the variance in social skills. As hypothesized, the relationship between ADHD and ERICA Self-Awareness was negative (b = −.073, p = .017) and between ERICA Self-Awareness and social skills was positive (b = .614, p = .033). When controlling for ERICA Self-Awareness, the relationship between ADHD and social skills was only marginally significant (b = −.220, p = .056), further supporting the role of ERICA Self-Awareness as a mediator. A follow-up test of simple mediation with ERICA Emotional Control as the mediator was nonsignificant (point estimate = −.066; SE = .044; 95% CIs [−.169, .001]).
Exploratory Analysis: Does Depression Mediate the Negative Association between ADHD and Social Skills?
As previously noted, although prior evidence indicates that ED predates the development of depression and mediates the association between ADHD and depression, it is unclear whether depression is best conceptualized as a moderator of the direct and indirect (through ED) association between ADHD and social skills. Indeed, ED and depression were correlated in our sample (see Table 2). To examine whether, in line with our proposed hypothesis, depression is best conceptualized as a moderator and not a mediator, we conducted an exploratory analysis to examine whether depression mediates the negative association between ADHD and social skills. Bootstrapping results did not support this model (point estimate = .013; SE = .017; 95% CIs [−.007, .066]), indicating that depression does not mediate the negative association between ADHD and social skills.
Thus, per our mediation results, we conclude that some aspects of ED mediate the negative association between ADHD social skills but depression does not. We thus chose to retain our proposed hypothesis, per which it may be that ADHD is associated with social skills through ED and that this process operates differently at distinct levels of depression.
Hypothesis 2: Depression Will Moderate the Negative Direct and Indirect Association between ADHD and Social Skills
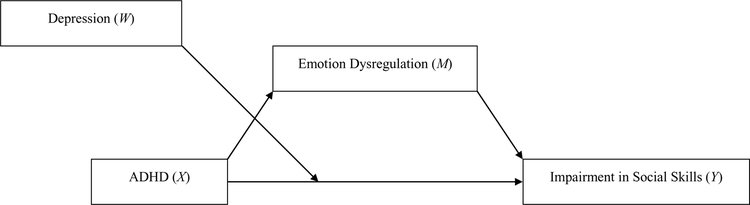
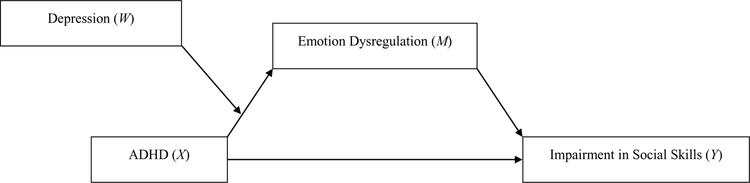
To test this research question, we examined moderated mediation models with ADHD as the predictor, social skills as the outcome, ED mediating the negative association between ADHD and social skills, and depression moderating the mediational model. To this end, we evaluated whether depression moderates (1) the path between ADHD and social skills (i.e., direct path) (Figure 1) and (2) the path between ADHD and ED (i.e., indirect path) (Figure 2).
Figure 1.
Depression moderates the direct path between ADHD and impairment in social skills, with ED mediating the association between ADHD and impairment in social skills.
Figure 2.
Depression moderates the indirect path between ADHD and impairment in social skills, with ED mediating the association between ADHD and impairment in social skills.
Hypothesis 2a: Depression will moderate the negative direct association between ADHD and social skills.
A test of the omnibus effect supported our hypothesized model with ERICA Self-Awareness, ERICA Emotional Control, and DERS Impulse as parallel mediators (R2 = .414, F(7, 171) = 15.856, p < .001) and indicated that, jointly, ADHD, ERICA Self-Awareness, ERICA Emotional Control, DERS Impulse and depression account for 41% of the variance in social skills. This effect was driven by depression moderating the negative direct effect of ADHD on parent-rated social skills with ERICA Self-Awareness (point estimate = .073; SE = .044; 95% CIs [.009, .208]) and Emotional Control (point estimate = −.088; SE = .050; 95% CIs [−.214, −.014]) as mediators of this association. Depression did not moderate the negative direct effect of ADHD on social skills with DERS Impulse (point estimate = −.006; SE = .018; 95% CIs [−.060, .017]) as a mediator of this association.
A follow-up test of moderated mediation with ERICA Self-Awareness as a single mediator indicated that the association between ADHD and social skills depends on the degree to which youth exhibit symptoms of depression (R2 = .378, F[3, 165] = 20.001, p < .001) and indicated that, jointly, ADHD, ERICA Self-Awareness, and depression account for 38% of the variance in social skills. Specifically, at non-clinical levels of depression, ADHD was negatively associated with social skills. At subclinical (p = .770) and clinical (p = .196) levels of depression, the negative association between ADHD and social skills diminished (see Table 3).
Table 3.
Conditional direct effect(s) of ADHD on Impairment in Parent-Rated Social Skills with ED as the Mediator and Depression Moderating the Direct Path
| ERICA Self Awareness | ||||
|---|---|---|---|---|
| Variable | Coeffa | SE | t | p |
| ERICA Self-Awareness | .7046 | .315 | 2.237 | .027 |
| ADHD | −1.502 | .449 | −3.349 | .001 |
| RADS | −.720 | .235 | −3.349 | .003 |
| ODD | −1.286 | .230 | −5.595 | .000 |
| Interaction | .029 | .010 | 2.962 | .004 |
| ERICA Emotional Control | ||||
| Coeffa | SE | t | p | |
| ERICA Emotional Control | −.3255 | .171 | −1.900 | .059 |
| ADHD | −1.112 | .440 | −2.528 | .012 |
| RADS | −.674 | .226 | −2.853 | .005 |
| ODD | −1.437 | .228 | −6.299 | <.001 |
| Interaction | .022 | .009 | 2.343 | .020 |
Coeff = Unstandardized regression coefficient.
A T score<61 falls within the normal range, T scores between 61–64 fall within the mild clinical depression range, T scores between 65–69 fall within the moderate clinical depression range, and T score>70 indicates severe clinical depression.
RADS = Very Low (non-clinical range): 10th percentile, Low (non-clinical range): 25th percentile, Moderate (non-clinical range): 50th percentile, High (subclinical range): 75th percentile, Very High (clinical range): 90th percentile
Similarly, a follow-up test of moderated mediation with ERICA Emotional Control as a single mediator indicated that the association between ADHD and social skills depends on the degree to which youth exhibit symptoms of depression (R2 = .372, F[3, 165] = 19.575, p < .001) and indicated that, jointly, ADHD, ERICA Emotional Control, and depression account for 37% of the variance in social skills. Specifically, at non-clinical levels of depression, ADHD was negatively associated with social skills. At subclinical (p = .847) and clinical (p = .202) levels of depression, the negative association between ADHD and social skills diminished (see Table 3).
Hypothesis 2b: Depression will moderate the negative indirect association between ADHD and social skills through ED.
A test of the omnibus effect supported our hypothesized model with ERICA Self-Awareness, ERICA Emotional Control, and DERS Impulse as parallel mediators (R2 = .375, F(5, 171) = 19.079, p < .001) and indicated that, jointly, ADHD, ERICA Self-Awareness, ERICA Emotional Control, DERS Impulse, and depression account for 38% of the variance in social skills. Depression moderated the negative indirect effect of ADHD on parent-rated social skills through ERICA Self-Awareness (b = .925, p = .003) and Emotional Control (b = −.519, p = .006) but not DERS Impulse (b = .165, p = .368).
Follow-up tests of moderated mediation with ERICA Self Awareness and Emotional Control as single mediators indicated that Self-Awareness was a mediator at non-clinical but not at sub-clinical or at clinical levels of depression (R2 = .341, F(3, 171) = 28.811, p < .001) (see Table 4) and Emotional Control was a mediator at non-clinical and sub-clinical but not at clinical levels of depression (R2 = .340, F(3, 171) = 28.664, p < .001) (see Table 4). In these models, jointly, ADHD, ERICA Self-Awareness and depression and ADHD and ERICA Emotional Control, and depression account for 34 and 34% of the variance in social skills, respectively.
Table 4.
Conditional indirect effect(s) of ADHD on Impairment in Social Skills at values of Depression scores with ED as the Mediator
| ERICA Self-Awareness | |||||
|---|---|---|---|---|---|
| Variable | Coeffa | SE | t | p | |
| ADHD | .372 | .107 | 3.490 | .000 | |
| RADS | .018 | .058 | .302 | .763 | |
| ODD | −.141 | .056 | −2.533 | .012 | |
| Interaction | −.007 | .002 | −3.011 | .003 | |
| Effects of ADHD on ERICA Self-Awareness at Depressionb Levels | |||||
| RADS | Effect | SE | BootLLCI | BootULCI | |
| ERICA Self-Awareness | Very Low: 34 | .082 | .044 | .012 | .186 |
| Low: 37 | .069 | .038 | .009 | .157 | |
| Moderate: 43 | .043 | .027 | .005 | .119 | |
| High: 51 | .009 | .022 | −.027 | .069 | |
| Very High: 61 | −.034 | .035 | −.132 | .016 | |
| ERICA Emotional Control | |||||
| Coeffa | SE | t | p | ||
| ADHD | .392 | .197 | 1.996 | .048 | |
| RADS | .104 | .107 | .974 | .331 | |
| ODD | −.159 | .103 | −1.553 | .122 | |
| Interaction | −.005 | 004 | −1.069 | .287 | |
| Effects of ADHD on ERICA Emotional Control at Depressionb Levels | |||||
| RADS | Effect | SE | BootLLCI | BootULCI | |
| ERICA Emotional Control | Very Low: 34 | −.085 | .053 | −.219 | −.006 |
| Low: 37 | −.080 | .049 | −.199 | −.005 | |
| Moderate: 43 | −.070 | .041 | −.174 | −.006 | |
| High: 51 | −.057 | .035 | −.159 | −.008 | |
| Very High: 61 | −.040 | .037 | −.174 | .006 | |
Coeff = Unstandardized regression coefficient.
A T score<61 falls within the normal range, T scores between 61–64 fall within the mild clinical depression range, T scores between 65–69 fall within the moderate clinical depression range, and T score>70 indicates severe clinical depression.
RADS = Very Low (non-clinical range): 10th percentile, Low (non-clinical range): 25th percentile, Moderate (non-clinical range): 50th percentile, High (subclinical range): 75th percentile, Very High (clinical range): 90th percentile
Discussion
The first purpose of this study was to examine whether three aspects of ED mediate the negative association between ADHD and social skills in a sample of youth. In addition, we formulated and examined a moderated mediation model wherein depressive symptoms were hypothesized to moderate both the direct and the indirect effect of ADHD on social skills. To support our conceptualization of depression as a moderator, we also explored whether depression mediates the negative association between ADHD and social skills.
In all analyses pertaining to ED, per prior findings, we investigated mediation and moderated mediation using three indices of ED. These included: emotional inflexibility and slow return to emotional baseline (ERICA Self-Awareness); a low threshold for emotional excitability, impatience, and socially inappropriate behaviors (ERICA Emotional Control); and behavioral control in the face of strong emotions (DERS Impulse). Our findings indicated that, ERICA Self-Awareness mediates the negative association between ADHD and social skills. Our findings further indicated that ERICA Emotional control mediates the negative association between ADHD and social skills, but only in the presence of ERICA Self-Awareness. Further, moderated mediation analyses indicated that the mediational role of these manifestations of ED depend on youths’ level of depression. Specifically, at non-clinical levels of depression, ERICA Self-Awareness is a mediator of the negative association between ADHD and social skills. However, at subclinical and clinical levels of depression, ADHD is not associated with social skills and the negative effect of ADHD on social skills through ERICA Self-Awareness diminishes. Similarly, at non-clinical and subclinical levels of depression, ERICA Emotional Control is a mediator of the negative association between ADHD and social skills. However, at clinical levels of depression, ADHD is not associated with social skills and the negative effect of ADHD on social skills through ERICA Emotional Control diminishes. Thus, ED, as measured by youths’ self-report on the ERICA Self-Awareness and Emotional Control subscales, mediates the negative association between ADHD and social skills at non-clinical and subclinical levels of depression but does not at clinical levels of depression. These findings clarify the contribution of ADHD symptoms and ED to social skills as well as the effect of depression on these relationships. Furthermore, these full models account for between 34 and 41 percent of the variance in social skills. Thus, they appear to include some of the important constructs related to the social impairment of these youth.
DERS Impulse did not mediate the negative association between ADHD and social skills in any of our models. It may be that the ERICA subscales, but not the DERS subscale, mediated the effect of ADHD on social skills because the item content of the ERICA Self-Awareness (e.g., return to emotional baseline and emotional flexibility/adaptability to change in environmental demands) and of the Emotional Control (e.g., low threshold for emotional excitability) subscales are more distinct from our measure of ADHD symptoms and social skills than those of the DERS subscale (e.g., impulsive behavioral responses to strong emotion). Furthermore, these specific ERICA subscales may better capture the ED that is most often exhibited by youth with ADHD than the other ERICA or DERS subscales. Excitability, difficulty adapting to changes in context, and a slow return to emotional baseline are behaviors targeted by these ERICA subscales and are consistent with clinical descriptions of youth with ADHD (e.g., Barkley, 2010; Henker & Whalen, 1989; Landau & Moore, 1991; Melnick & Hinshaw, 2000; Walcott & Landau, 2004) and theories of ED associated with ADHD (e.g., Barkley, 2010; Martel & Nigg, 2006).
One explanatory hypothesis for our findings on the moderating role of depression pertains to characteristics of depression that overshadow the negative effects of ED on social skills among youth with ADHD. This conceptualization is in line with prior findings indicating that, among youth with ADHD, depression exacerbates social problems (Becker et al., 2013; Daviss, 2008) and necessitates more intensive interventions (e.g., McQuade et al., 2011). It may be that among youth who experience clinical depression, depression accounts for enough variance in social skills impairment that the variance attributable to ADHD or to ED becomes trivial. Conversely, it may be that among youth who experience non-clinical or subclinical depression (in the present sample, 155 participants fell in the normal range, 7 in the mild clinical depression range, 5 in the moderate clinical depression range, and 6 in the severe clinical depression range), ADHD and ADHD through ED account for detectable variance in social skills impairment. This effect may be partly due to overlap between symptoms of depression, which, by definition, is a mood disorder, and ED, which pertains to deficits in regulating emotions. Indeed, some research provides evidence for a ‘nonspecific ED factor’ that is common across internalizing and externalizing disorders (Silk et al., 2003). Youth with depression exhibit poor emotional understanding, low self-efficacy to regulate emotions, and difficulties expressing and coping with anger (Zeman, et al., 2006). This overlap between depression and ED may result in depression overshadowing the effects of ED on social skills impairment at clinical levels but not at the non-clinical or subclinical levels.
The overlap between ED and depression is a worthwhile focus of future study. In our sample, correlations between the ED subscales and our measure of depression ranged from .03 to .62 in our sample. Thus, there are certainly unique aspects to each construct. ED, when associated with ADHD, involves problems both in the positive incentive approach and negative withdrawal systems (Martel & Nigg, 2006), and manifest in exuberant positive affect and fearful and angry negative affect (Nigg et al., 2004). As further evidence of the distinction between ED and depression, our data indicate that although aspects of ED were correlated with depression, unlike ED, depression did not mediate the negative association between ADHD and social skills. Understanding the way in which ED manifests in youth with ADHD as well as youth with depression and youth with comorbid ADHD and depression is an important line of research and one that may lead to some important advances in expanding our treatments to address some of the complicated presentations of these youth.
Limitations
There are limitations to this study that warrant consideration. First, although we mathematically established mediation, experimental and prospective designs are needed to establish causation (Shadish, Cook, & Campbell, 2002). Nonetheless, given that we reversed our models, our findings are encouraging and indicate further studies should be undertaken to replicate and extend our results. In addition, because doing so is beyond the current state of the science (A. Hayes, personal communication, March 12, 2014; Hayes, 2013), we were unable to estimate the statistical power needed for our analyses or to provide standardized coefficients or effect size estimates individual paths. Still, we could determine that ADHD, ED, and depression, jointly, accounted for about one-third or more of the variance in social skills, underscoring the importance of these variables with regard to the outcome. Second, with regard to the generalizability of our findings, it is important to keep in mind that our sample is characterized by relatively low variability in depression. Third, there are inherent limitations to youth’s self-report. Youth with ADHD tend to over- and under-report the deficits they experience in diverse areas of performance (Owens et al., 2011). However, with regard to ED, given increased cognitive maturity in adolescence and the largely internal nature of emotions, self-report may be an appropriate measurement method for this age group (Walden et al. 2003). With regard to depression, there is reason to believe that youth with ADHD and depression are less likely to exhibit biased self-perceptions than youth with ADHD and without depression (Hoza et al., 2010). Nevertheless, youth may have limited insight into some aspects of ED they exhibit yet such insight may be critical to understanding the associations between ED and social problems, and ultimately, to improving youth’s functioning. In addition, the present findings are limited to social skills as an index of social impairment. Investigators may wish to replicate and expand these findings to other areas of social functioning. These limitations emphasize the need for prospective designs as well as for a multi-method, multi-informant approach to measurement.
Future Directions
It appears that emotional inflexibility and slow return to baseline as well as a low threshold for emotional excitability, impatience, and socially inappropriate behaviors play a unique role in youth’s social skills impairment. We anticipate that a model that adequately explains the relationships among ADHD, ED, and social functioning is actually far more complex than the models we tested. Thus, there is a need to improve our definitions and measurement of these constructs as well as increase our understanding of the way in which these manifest and interact to compromise functioning among youth with ADHD over time.
Interventions that target ED may be beneficial additions to interventions targeting the social impairment of youth with ADHD. Prior evidence indicates that mindfulness meditation may improve emotion regulation (Teasdale, Segal, & Williams, 1995). In addition, dialectical behavior therapy (DBT) is a comprehensive and effective treatment for ED (Linehan, Bohus, & Lynch, 2007) that has been adapted for youth with internalizing and externalizing disorders (e.g., Goldstein et al., 2007). Researchers have tested mindfulness meditation and DBT with adults and adolescents with ADHD, although these investigators focused on symptom change and not improvements in functioning (Hesslinger et al., 2002; Zylowska et al., 2007). Although these studies are with methodological limitations, findings indicate that integrating mindfulness-meditation and DBT with psychosocial treatments for the social impairment associated with ADHD may enhance their impact.
Conclusions
Youth with ADHD often experience social impairment. Empirical evidence indicates that such impairment is related, in part, to ED. Our own research to date has shown that, among youth with ADHD, the association between ED and impairment in social skills is specific to (and holds above and beyond the contribution of ODD) emotional inflexibility and slow return to baseline; a low threshold for emotional excitability, impatience, and socially inappropriate behaviors; and difficulty in behavioral control when experiencing strong emotions (Bunford et al., 2014). Our present findings indicate that the contribution of emotional inflexibility and slow return to baseline as well as of a low threshold for emotional excitability, impatience, and socially inappropriate behaviors to impairment in social skills of youth with ADHD depends on the degree to which these youth exhibit symptoms of depression. ADHD and ED both contribute to impairment in social skills at non-clinical and subclinical levels of depression. The contribution of ADHD and ED to impairment in social skills appears to diminish for youth who report clinical levels of depression.
Supplementary Material
Author Notes and Disclosures
During the preparation of this article, the first author was supported in parts by the Elizabeth Munsterberg Koppitz Dissertation Fellowship, awarded by the American Psychological Foundation. The second and fourth authors were supported in parts by a grant from the National Institute of Mental Health (5ROIMH082864) and the second author by grants from the Department of Education, Institute of Educational Sciences (R324C08006; R324A120272). The contents of this article do not necessarily represent the views of the American Psychological Foundation, National Institutes of Health or Institute for Education Sciences and do not imply endorsement by the federal government.
We wish to thank Andrew F. Hayes and Eric A. Youngstrom for their valuable assistance and feedback during the preparation of this manuscript.
Footnotes
Currently, many different and at times conflicting definitions of emotion regulation are accepted in the field. As such, there is often limited theoretical and empirical agreement on conceptualizations of the construct. We adopt Barkley’s definition of ED as this definition is most specific to ADHD.
Constructive emotional coping includes, for example, an inability to continue a task in the wake of frustration, an inability to seek help from parents when frustrated, extreme levels of negative affect, poor problem solving, and an extreme focus on negative aspects of a task.
As measured by teacher ratings of cooperation, assertiveness, and self-control and by peer-ratings of desirability as play- or study-partners.
The macros provide a 95% confidence interval around the indirect effect. When zero is not in the 95% confidence interval (i.e., both numbers fall on the same side of 0), it can be concluded that the indirect effect is significantly different from zero at p < .05 (two tailed).
When controlling for gender and age in our analyses, by including gender and age as covariates in the models, neither emerged as a significant covariate (gender ps ranging from .304 to .810; age ps ranging from .146 to .603).Thus, the models on which we report data do not include gender or age as a covariate.
References
- Bagwell CL, Molina BS, Pelham WE Jr. & Hoza B (2001). Attention deficit hyperactivity disorder and problems in peer relations: Predictions from childhood to adolescence. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 1285–92. [DOI] [PubMed] [Google Scholar]
- Barkley RA (2010). Deficient emotional self-regulation: A core component of attention-deficit/hyperactivity disorder. Journal of ADHD and Related Disorders, 1, 5–37. [Google Scholar]
- Barkley RA (2008). Challenges in diagnosing adults with ADHD. The Journal of clinical psychiatry, 69(12), e36–e36. [DOI] [PubMed] [Google Scholar]
- Becker SP, Langberg JM, Evans SW, Girio-Herrera E, & Vaughn AJ (2014). Differentiating anxiety and depression in relation to the social functioning of young adolescents with ADHD. Journal of Clinical Child and Adolescent Psychology. DOI: 10.1080/15374416.2014.930689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Keenan K, Benjamin J, Krifcher B, Moore C, … & Tsuang M,T. (1992). Further evidence for family-genetic risk factors in attention deficit hyperactivity disorder: Patterns of comorbidity in probands and relatives in psychiatrically and pediatrically referred samples. Archives of General Psychiatry, 49, 728–738. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Monuteaux MC (2002). Differential effect of environmental adversity by gender: Rutter’s index of adversity in a group of boys and girls with and without ADHD. American Journal of Psychiatry, 159, 1556–1562. [DOI] [PubMed] [Google Scholar]
- Biederman J, Newcorn J, & Sprich S (1991). Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. American Journal of Psychiatry, 148, 564–577. [DOI] [PubMed] [Google Scholar]
- Bunford N, Evans SW, & Langberg JM (2014). Emotion Dysregulation Is Associated With Social Impairment Among Young Adolescents With ADHD. Journal of Attention Disorders, DOI: 1087054714527793. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Molina BS, Pelham WE, Applegate B, Dahlke A, Overmyer M, & Lahey BB (2010). Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Archives of general psychiatry, 67(10), 1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham CE, & Barkley RA (1979). The interactions of normal and hyperactive children with their mothers during free play and structured tasks. Child Development, 50, 217–224. [PubMed] [Google Scholar]
- Daviss W (2008). A review of co-morbid depression in pediatric ADHD: Etiologies, phenomenology, and treatment. Journal of Child and Adolescent Psychopharmacology, 18(6), 565–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daviss W, Diler R, & Birmaher B (2009). Associations of lifetime depression with trauma exposure, other environmental adversities, and impairment in adolescents with ADHD. Journal of Abnormal Child Psychology: An official publication of the International Society for Research in Child and Adolescent Psychopathology, 37(6), 857–871. [DOI] [PubMed] [Google Scholar]
- Durbin C, & Shafir D (2008). Emotion regulation and risk for depression In Abela JRZ & Hankin HL (Eds.), Handbook of depression in children and adolescents (pp. 149–176). New York: Guilford. [Google Scholar]
- Elia J, Ambrosini P, & Berrettini W (2008). ADHD characteristics: I. Concurrent co-morbidity patterns in children & adolescents. Child and Adolescent Psychiatry and Mental Health, 2, [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott SN, & Gresham FM (2008). SSIS-RS intervention guide. Minneapolis, MN: NCS Pearson. [Google Scholar]
- Fabiano GA, Pelham WE, Waschbusch DA, Gnagy EM, Lahey BB, Chronis AM et al. (2006). A practical measure of impairment: Psychometric properties of the impairment rating scale in samples of children with attention deficit hyperactivity disorder and two school-based samples. Journal of Clinical Child and Adolescent Psychology, 35, 369–385. [DOI] [PubMed] [Google Scholar]
- Feng X, Keenan K, Hipwell A, Henneberger A, Rischall M, Butch J, et al. (2009). Longitudinal associations between emotion regulation and depression in preadolescent girls: Moderation by the caregiving environment. Developmental Psychology, 45(3), 798–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fristad MA, Teare M, Weller EB, Weller RA, & Salmon P (1998). Study III: Development and concurrent validity of the Children’s Interview for Psychiatric Syndromes—parent version (P-ChIPS). Journal of Child and Adolescent Psychopharmacology, 8(4), 221–226. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, Axelson DA, Birmaher B &. Brent DA. (2007). Dialectical behavior therapy for adolescents with bipolar disorder: A 1-year open trial. American Academy of Child and Adolescent Psychiatry, 46, 820–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. [Google Scholar]
- Gresham FM, Elliott SN, Vance MJ, & Cook CR (2011). Comparability of the Social Skills Rating System to the Social Skills Improvement System: Content and psychometric comparisons across elementary and secondary age levels. School Psychology Quarterly, 26, 27–44. [Google Scholar]
- Guevremont DC, & Dumas MC (1994). Peer relationship problems and disruptive behavior disorders. Journal of Emotional and Behavior Disorders, 2, 164–172. [Google Scholar]
- Hayes AF (2013). Introduction to Mediation, Moderation, and Conditional Process Analysis. New York: Guilford Press. [Google Scholar]
- Henker B, & Whalen CK (1989). Hyperactivity and attention deficits. American Psychologist, 44, 216–223. [DOI] [PubMed] [Google Scholar]
- Hesslinger B, Tebartz van Elst L, Nyberg E, Dykierek P, Richter H, Berner M, & Ebert D (2002). Psychotherapy of attention deficit hyperactivity disorder in adults: A pilot study using a structured skills training program. European Archives of Psychiatry and Clinical Neuroscience, 252, 177–184. [DOI] [PubMed] [Google Scholar]
- Hoza B (2007). Peer functioning in children with ADHD. Ambulatory Pediatrics, 7(1 Suppl.), 101–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoza B, Mrug S, Gerdes AC, Hinshaw SP, Bukowski WM, Gold JA, … & Arnold LE. (2005). What aspects of peer relationships are impaired in children with attention-deficit/hyperactivity disorder?. Journal of Consulting and Clinical Psychology, 73(3), 411–423. [DOI] [PubMed] [Google Scholar]
- Hoza B, Murray-Close D, Arnold LE, Hinshaw SP, Hechtman L, & MTA Cooperative Group. (2010). Time-dependent changes in positively biased self-perceptions of children with ADHD: A developmental psychopathology perspective. Development and psychopathology, 22(2), 375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kats-Gold I, Besser A, & Priel B (2007). The role of simple emotion recognition skills among school aged boys at risk of ADHD. Journal of Abnormal Child Psychology, 35(3), 363–378. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, & Nock MK (2003). Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. Journal Of Child Psychology And Psychiatry, 44, 1116–1129. [DOI] [PubMed] [Google Scholar]
- Landau S, & Moore LA (1991). Social skill deficits in children with attention-deficit hyperactivity disorder. School Psychology Review, 20, 235–251. [Google Scholar]
- Linehan MM, Bohus M, & Lynch TR (2007). Dialectical behavior therapy for pervasive emotion dysregulation: Theoretical and practical underpinnings In Gross JJ (Ed). Handbook of Emotion Regulation. New York, NY: Guilford Press. [Google Scholar]
- MacDermott ST, Gullone E, Allen JS, King NJ, & Tonge B (2010). The emotion regulation index for children and adolescents (ERICA): a psychometric investigation. Journal of Psychopathology and Behavioral Assessment, 32(3), 301–314. [Google Scholar]
- Maedgen JW, & Carlson CL (2000). Social functioning and emotional regulation in the attention deficit hyperactivity disorder subtypes. Journal of Clinical Child Psychology, 29, 30–42. [DOI] [PubMed] [Google Scholar]
- Martel MM, & Nigg JT (2006). Child ADHD and personality/temperament traits of reactive and effortful control, resiliency, and emotionality. The Journal of Child Psychology and Psychiatry, 47, 1175–1183. [DOI] [PubMed] [Google Scholar]
- McQuade JD, Hoza B, Waschbusch DA, Murray-Close D, & Owens JS (2011). Changes in self-perceptions in children with ADHD: a longitudinal study of depressive symptoms and attributional style. Behavior Therapy, 42(2), 170–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnick SM & Hinshaw SP (2000). Emotion regulation and parenting in AD/HD and comparison boys: Linkages with social behaviors and peer preference. Journal of Abnormal Child Psychology, 28, 73–86. [DOI] [PubMed] [Google Scholar]
- Musser ED, Galloway-Long HS, Frick PJ, & Nigg JT (2013). Emotion Regulation and Heterogeneity in Attention-Deficit/Hyperactivity Disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 52(2), 163–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musser ED, Backs RW, Schmitt CF, Ablow JC, Measelle JR, & Nigg JT (2011). Emotion regulation via the autonomic nervous system in children with Attention Deficit/Hyperactivity Disorder (ADHD). Journal of Abnormal Child Psychology, 39(6), 841–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT, Goldsmith HH, & Sachek J (2004). Temperament and attention-deficit/hyperactivity disorder: the development of a multiple pathway model. Journal of Clinical Child and Adolescent Psychology, 33, 42–53. [DOI] [PubMed] [Google Scholar]
- Owens JS, Sadler JM, Bunford N, Vaughn A, Schultz B, Evans SW, & Langberg J (November, 2011). Self-Perceptions of Competence in Adolescents with ADHD. Symposium presented at the annual meeting of the Association for Behavioral and Cognitive Therapies, Toronto, Canada. [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, & Milich R (1992). Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 31(2), 210–218. [DOI] [PubMed] [Google Scholar]
- Reynolds WM (2002). Reynolds adolescent depression scale, second edition John Wiley & Sons, Inc. [Google Scholar]
- Seymour KE, Chronis-Tuscano A, Halldorsdottir T, Stupica B, Owens K, & Sacks T (2012). Emotion regulation mediates the relationship between ADHD and depressive symptoms in youth. Journal of abnormal child psychology, 40(4), 595–606. [DOI] [PubMed] [Google Scholar]
- Seymour KE, Chronis-Tuscano A, Iwamoto DK, Kurdziel G, & MacPherson L (2014). Emotion regulation mediates the association between ADHD and depressive symptoms in a community sample of youth. Journal of Abnormal Psychology, 42(4), 611–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scime M, & Norvilitis J (2006). Task performance and response to frustration in children with attention deficit hyperactivity disorder. Psychology in the Schools, 43(3), 377–386. [Google Scholar]
- Shadish WR, Cook TD, & Campbell DT (2002). Experimental and quasi-experimental designs for generalized causal inference. Boston, MA: Houghton Mifflin and Company. [Google Scholar]
- Silk JS, Steinberg L, & Morris AS (2003). Adolescents’ emotion regulation in daily life: Links to depressive symptoms and problem behavior. Child Development, 74, 1869–1880. [DOI] [PubMed] [Google Scholar]
- Singh SD, Ellis CR, Winton AS, Singh NN, Leung JP, & Oswald DP (1998). Recognition of facial expressions of emotion by children with attention-deficit hyperactivity disorder. Behavior Modification, 22(2), 128–142. [DOI] [PubMed] [Google Scholar]
- Sjöwall D, Roth L, Lindqvist S, & Thorell LB (2012). Multiple deficits in ADHD: Executive dysfunction, delay aversion, reaction time variability, and emotional deficits. Journal of Child Psychology and Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L (2005). Cognitive and affective development in adolescence. Trends in Cognitive Science, 9, 69–74. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Segal ZV, & Williams MG (1995). How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness training) help? Behaviour Research and Therapy, 33, 25–39. [DOI] [PubMed] [Google Scholar]
- Tortella-Feliu M, Balle M, & Sesé A (2010). Relationships between negative affectivity, emotion regulation, anxiety, and depressive symptoms in adolescents as examined through structural equation modeling. Journal of Anxiety Disorders, 24(7), 686–693. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. (2011). State & County QuickFacts. Retrieved from http://quickfacts.census.gov/qfd/states/39000.html
- Vasilev CA, Crowell SE, Beauchaine TP, Mead HK, & Gatzke-Kopp LM (2009). Correspondence between physiological and self-report measures of emotion dysregulation: A longitudinal investigation of youth with and without psychopathology. Journal of Child Psychology and Psychiatry, 50, 1357–1364. [DOI] [PubMed] [Google Scholar]
- Walcott C, & Landau S (2004). The Relation Between Disinhibition and Emotion Regulation in Boys with Attention Deficit Hyperactivity Disorder. Journal of Clinical Child and Adolescent Psychology, 33(4), 772–782. [DOI] [PubMed] [Google Scholar]
- Walden TA, Harris VS, & Catron TF (2003). How I feel: a self-report measure of emotional arousal and regulation for children. Psychological Assessment, 15(3), 399–412. [DOI] [PubMed] [Google Scholar]
- Wang Y, Zhang W, Peng J, Mo B, & Xiong S (2009). The relations of attachment, self-concept, and deliberate self-harm in college students. Psychological Exploration, 5, 56–61. [Google Scholar]
- Wechsler D (2003). Wechsler intelligence scale for children–Fourth Edition (WISC-IV). San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Weinberg A, & Klonsky ED (2009). Measurement of emotion dysregulation in adolescents. Psychological Assessment, 21, 616–621. [DOI] [PubMed] [Google Scholar]
- Weller EB, Weller RA, Rooney MT & Fristad MA. (1999). Parent Form - Children’s Interview for Psychiatric Syndromes (P-ChIPS). Arlington, VA: American Psychiatric Press, Inc. [Google Scholar]
- Weller EB, Weller RA, Fristad MA, Rooney MT, & Schecter J (2000). Children’s Interview for Psychiatric Syndromes (ChIPS). Journal of the American Academy of Child and Adolescent Psychiatry, 39, 76–84. [DOI] [PubMed] [Google Scholar]
- Wilens E, Biederman J, Brown S, Tanguay S, Monuteaux M, Blake C, & Spencer T (2002) Psychiatric comorbidity and functioning in clinically referred preschool children and schoolage youths with ADHD. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 262–268. [DOI] [PubMed] [Google Scholar]
- Wolraich ML, Wibbelsman CJ, Brown TE, Evans SW, Gotlieb EM, Knight JR, … & Wilens T. (2005). Attention-deficit/hyperactivity disorder among adolescents: a review of the diagnosis, treatment, and clinical implications. Pediatrics, 115(6), 1734–1746. [DOI] [PubMed] [Google Scholar]
- Zeman J, Cassano M, Perry-Parrish C, & Sheri S (2006). Emotion regulation in children and adolescents. Journal of Developmental and Behavioral Pediatrics, 27, 155–168. [DOI] [PubMed] [Google Scholar]
- Zylowska L, Ackerman DL, Yang MH, Futrell JL, Horton NL, Hale TS, Pataki C, & Smalley SL (2008). Mindfulness meditation training in adults and adolescents with ADHD: A feasibility study. Journal of Attention Disorders, 11, 737–746. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.