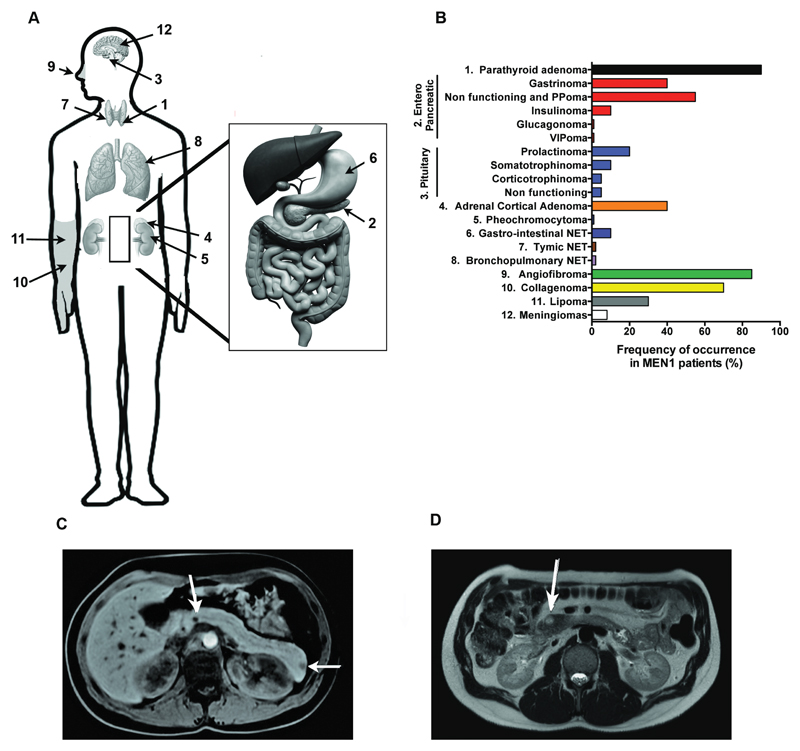
Figure 2.
Distribution of endocrine and non-endocrine tumours in MEN1 patients. (A) MEN1 patients may develop: endocrine tumours involving the parathyroids (labelled number 1), pancreas (2), pituitary (3), adrenal cortex (4) and medulla (5), gastro-intestinal tract (6), thymus (7) and bronchial tree (8); and non-endocrine tumours such as facial angiofibromas (9), collagenomas (10), lipomas (11) and meningiomas (12). (B) Frequencies of MEN1-associated tumours. The most frequently occurring endocrine tumours in MEN1 patients are: parathyroid adenomas, which occur in >95% of patients; pancreatic neuroendocrine tumours (PNETs), which occur in 50-70% of patients, with ~40% of patients having gastrinomas, ~10% having insulinomas, <1% having glucagonomas, <1% having VIPomas, and ~20-50% having PPomas or non-functioning tumours; anterior pituitary tumours, which occur in 20-40% of patients, with ~20% having prolactinomas, ~10% having somatotrophinomas, <5% having corticotrophinomas, and ~5% having non-functioning tumours; and adrenal tumours, which occur in 20-40% of patients, with ~40% having cortical adenomas that are usually non-secreting, but may occasional secrete glucocorticoids, or aldosterone causing Cushing’s or Conn’s syndrome, respectively, and <1% having pheochromocytoma tumours arising from the medulla. The most frequently occurring non-endocrine tumours in MEN1 patients are angiofibromas, collagenomas, and lipomas, which are reported to occur in 0-85%, 0-70%, and ~30% of patients, respectively. (C) Magnetic Resonance Imaging (MRI) sagittal section of multiple PNETs (indicated by white arrows) in an MEN1 patient. (D) MRI sagittal section of a non-MEN1 PNET (the tumour is indicated by a white arrow).