Abstract
Background:
Vitamin B12 deficiency is believed to be widespread in Indian population. However, more data is needed to fuel a meaningful debate on preventive and therapeutic strategies.
Aims and Objectives:
Objective of the current study is to evaluate status of vitamin B12 levels in people from a tier 3 city and among people living in an urban area with or without diabetes.
Settings and Design:
Retrospective, cross-sectional study.
Methodology:
Data captured in electronic medical records (EMR) of an endocrine practice and from a diagnostic laboratory was analysed.
Statistical Analysis Used:
Statistical analysis was done using open source software “Jamovi”.
Results:
Prevalence of vitamin B12 deficiency (Vitamin B12 levels <200 pg/ml) in tier 3 city was 47.19% (n = 267). From an urban endocrine practice, database of 11913 patients was searched for reports of vitamin B12 levels. Prevalence of vitamin B12 deficiency was 37.76% in people with pre-diabetes (n = 92), 31.23% in people with endocrine problems other than diabetes and pre-diabetes (n = 285) and 18.25% in people with diabetes (n = 378). Tier 3 city population had significantly lower vitamin B12 levels than people living in an urban area and attending an endocrine clinic. Vitamin B12 levels were significantly higher in people with diabetes as compared to people with other endocrine problems.
Conclusion:
Prevalence of vitamin B12 deficiency is 47% in north Indian population. People with diabetes have higher vitamin B12 levels than general population though still have high prevalence of deficiency. This data shows that Vitamin B12 deficiency is widespread in Indian population.
Keywords: Diabetes, electronic medical records, North India, vitamin B12 deficiency
INTRODUCTION
Vitamin B12 is an essential vitamin with largely non vegetarian source.[1,2] Indian population, with largely vegetarian food habit, is more prone to harbour deficiency of vitamin B12.[2,3] But data documenting vitamin B12 status in India in general population as well as in people with diabetes is limited. Documentation of more data from different parts of country may spark well-informed debate on replacement strategies and also on food fortification. This study fills this lacuna in literature and presents prevalence of vitamin B12 deficiency in general population of a tier 3 city of Haryana.
Assessment of this deficiency would be even more important in people with diabetes. Microvascular complications of diabetes have a time dependent component apart from being correlated with glycemic control.[4] In India, we are encountering people with new onset diabetes at much younger ages now.[5] These people would be spending increasingly more life with diabetes and would be more prone to complications of diabetes, including diabetic neuropathy. Diagnosis of diabetic neuropathy is made clinically and is one of exclusion. It is prudent to look for any potentially reversible factor contributing to neuropathy such as vitamin B12 deficiency.[6] Moreover, in literature, vitamin B12 deficiency has been shown to be aggravated by metformin, cornerstone of pharmacotherapy for diabetes mellitus type 2. This study also presents data from a fairly large endocrine practice from urban India to assess prevalence of vitamin B12 deficiency in people attending the clinic for diabetes or any other endocrine related problem.
METHODOLOGY
Retrospective, cross-sectional data from electronic medical records was extracted from software “Healthvriksh EMR, version 1 (Kalpavriksh Healthcare, Delhi, India)”. Two datasets were extracted and evaluated. First dataset included people attending endocrinology OPD and with a record of serum level of vitamin B12. This dataset was segregated for people with diabetes, pre-diabetes and other endocrine problems. First reading of vitamin B12 was taken in case of multiple reports. Second dataset was extracted from camps conducted in a tier 3 city. This city ’Jind’ is situated in state of Haryana of north India with population of 191145.[7] These camps were conducted as part of routine commercial activity by KV Labs (diagnostic arm of Kalpavriksh Healthcare) and were targeted at general population. All samples from these camps were analysed on Cobasintegra 411 (Roche diagnostics) using electrochemiluminescence assay. These camps were conducted between September 2016 and August 2018. In both the databases, records with vitamin B12 levels more than the upper detectable limit (2000 pg/ml) of assay were excluded as they are indicative of active supplementation. Statistical analysis was done using open source software “Jamovi” (Version 0.9).[8] Normalcy of data was assessed and further analysis was done using non-parametric tests.[8]
RESULTS
Records of 11,913 patients were searched in EMR database with date bounds of 8th May, 2015 (the day of operationalisation of EMR) till 14th December, 2018. This search revealed a record of vitamin B12 levels in 378 people with diabetes, 92 people with pre-diabetes and 285 people who attended endocrine OPD for reasons other than diabetes or pre-diabetes. Another dataset of 267 people was retrieved from records of ’KV Labs’ (diagnostic arm of Kalpavriksh Healthcare). KV Labs conducts camps for preventive health checkup involving urine and blood investigations, at a tier 3 city (Jind, Haryana) on regular basis.
Distribution of overall data is shown in Figure 1. Normalcy of data was assessed using Shapiro Wilk test and Shapiro Wilk ’P’ was <0.001 suggestive of non-normal distribution of data. Non parametric tests were used for further analysis of data.
Figure 1.
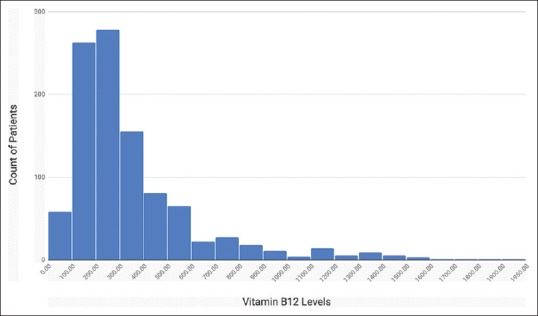
Distribution of vitamin B12 levels in total population
Descriptive details of data are shown in Table 1. Proportion of people with low vitamin B12 levels was calculated to assess prevalence of deficiency in different subgroups of population. Vitamin B12 level of <200 pg/ml (150 pmol/L) is universally considered to be threshold of deficiency.[9] Overall, in entire study population of 1022 people, 321 (31.40%) people had vitamin B12 deficiency. Emerging consensus is that people with vitamin B12 levels between 200 and 300 pg/ml may have relative deficiency and need to be evaluated further with measurement of serum methylmalonic acid or homocysteine concentrations.[10] With this definition, 74.90% of people would be potentially deficient in vitamin B12 among general population in a tier 3 city.
Table 1.
Vitamin B12 status in different population
| Diabetes | Endocrine | Prediabetes | T3 City | Total | |
|---|---|---|---|---|---|
| n (M:F) | 378 (218:160) | 285 (95:190) | 92 (41:51) | 267 (170:97) | 1022 (524:498) |
| Age (years) (SD) | 50.31 (12.39) | 37.85 (12.99) | 43.05 (12.97) | 48.81 (12.02) | |
| Mean Vitamin B12 Levels (SD) (pg/ml) | 431.10 (314.12) | 330.01 (252.91) | 316.89 (247.72) | 274.59 (224.77) | 351.74 (277.47) |
| Median Vitamin B12 Levels (pg/ml) | 331.40 | 253.90 | 222.70 | 213.80 | 266.00 |
| 25th Centile Vitamin B12 levels (pg/ml) | 222.25 | 183.80 | 184.18 | 154.65 | 187.70 |
| 75th Centile Vitamin B12 Levels (pg/ml) | 528.00 | 390.00 | 360.40 | 301.30 | 415.75 |
| n with <300 pg/ml (%) | 163 (43.12) | 178 (62.46) | 58 (63.04) | 200 (74.90) | 599 (58.61) |
| n with <200 pg/ml(%) | 69 (18.25) | 89 (31.23) | 37 (37.76) | 126 (47.19) | 321 (31.40) |
In total population, women had statistically higher median vitamin B12 levels of 286.20 pg/ml (25th percentile 199.13; 75th percentile 459.67) as compared to men (vitamin B12 (pg/ml) median 243.80;25th percentile 172.70;75th percentile 369.25) (P < 0.001). This difference was largely contributed by T3 city population and diabetes group.
All four populations were further compared vis-a-vis vitamin B12 levels observed. Distribution of data is shown in Figure 2 for different population. Kruskal Wallis ANOVA was applied and it revealed significant difference among groups (P < 0.001). Dwass-Steel-Critchlow-Fligner pairwise comparison was further applied and results are shown in Table 2.
Figure 2.
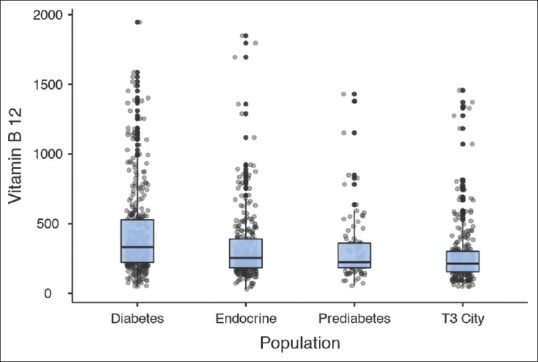
Distribution of vitamin B12 levels in 4 different populations
Table 2.
Dwass-Steel-Critchlow-Fligner pairwise comparison between different study population for vitamin B12 levels
| Comparator 1 | Comparator 2 | Wilcoxon statistic | P |
|---|---|---|---|
| Diabetes | Endocrine | −7.35 | <0.001 |
| Diabetes | Prediabetes | −5.88 | <0.001 |
| Diabetes | T3 City | −12.33 | <0.001 |
| Endocrine | Prediabetes | −1.21 | 0.393 |
| Endocrine | T3 City | −5.73 | <0.001 |
| Prediabetes | T3 City | −2.81 | 0.047 |
T3 City: tier 3 city (Jind, Haryana)
DISCUSSION
Dietary source of vitamin B12 largely consists of non vegetarian food. This may be more relevant in people from India as large majority of Indian population is vegetarian by food habits.[3] However, population based data reflecting exact scenario of vitamin B12 levels in Indian population is still evolving. Different studies reporting a deficiency ranging from 16% to 77% are summarised in Table 3.[11,12,13,14] In pregnancy, deficiency of vitamin B12 has been estimated to have prevalence of 43% to 74%.[15] Estimate by Shobha et al. seems to be lower than experienced in all other studies and authors attributed it to studied population being largely non-vegetarian by food habits.[12] Current study estimate of prevalence of vitamin B12 deficiency at 47.19% agrees with the current understanding of overall status of Indian population [Table 3]. Overall, presence of this large prevalence of vitamin B12 deficiency calls for debate on prudence of expensive testing before supplementing in susceptible populations.
Table 3.
Summary of Indian studies documenting Vitamin B12 status
| Study | Setting and population | Vitamin B12 levels (median) (pg/ml) | Prevalence of deficiency (%) |
|---|---|---|---|
| Refsum et al, 2001, AJCN[11] | 63 subjects from urban area | 216.86 | 46 |
| Shobha et al, 2011, IJMR[12] | 175 elderly urban subjects from south India | 414.74 | 16 |
| Naik et al, 2018, BJN[13] | 46 males and 73 females from urban area | Males: 198.56 Females: 222.28 |
Males: 77 Females: 50 |
| Yajnik et al, 2006, JAPI[14] | 441 males from rural, slums and urban areas | 149.09 | 67 |
This is also in gross contrast with very low prevalence of vitamin B12 deficiency in western population. Analysis of data from the National Health and Nutrition Examination Survey, 1999-2006 by Reinstaller et al. revealed that prevalence of vitamin B12 deficiency (defined as Vitamin B12 <200 pg/ml (148 pmol/l)) in general population in United States of America is 3.3%.[16] Underlying cause of vitamin B12 deficiency in western population is considered to be intrinsic factor deficiency and hence malabsorption of oral vitamin B12.[17,18] This leads to uniform guidelines of treating vitamin B12 deficiency with injectable preparations or very high doses of oral methylcobalamin in western literature. While deficiency is India seems largely due to diet being deficient in vitamin B12.[3,14] This difference in underlying mechanism of vitamin B12 deficiency may have therapeutic implications in Indian population where oral supplementation with low doses of methylcobalamin may suffice and thus injectable or oral high dose therapy may not be required.
In western population, people with diabetes have been shown to have lower prevalence of vitamin B12 deficiency as compared to general population (2.2% vs. 3.3% respectively).[16] From India, Refsum et al., showed slightly higher prevalence of vitamin B12 deficiency in 41 people with diabetes at 54% as compared to 46% in 63 people without diabetes.[11] In current study, people with diabetes had lower prevalence of vitamin B12 deficiency than people without diabetes, similar to study by Reinstaller et al.[16] There can be two possible explanations that can be responsible either in combination or independently. Firstly, people with diabetes are more likely to be in constant touch with healthcare system and are more likely to be supplemented.[16] We reported previously that 44% of people with diabetes were prescribed vitamin supplements during their routine diabetes care.[19] Secondly, people without diabetes might seek attention later due to long latent period of manifestations of vitamin B12 deficiency. Our effort to document exogenous supplementation was not successful due to non-centralized nature of healthcare system in India and over-the-counter availability of vitamin B12 preparations.
Metformin has been argued to aggravate vitamin B12 deficiency in people with diabetes. In study by Reinstaller et al., prevalence at 5.8%, in people with diabetes and taking metformin was more than general population.[16] In Indian population, Raizada et al. reported no difference between vitamin B12 levels in people with diabetes taking metformin or without it.[20] Serum Vitamin B12 levels were 267.7 ± 194.4 pmol/l in metformin group and 275.1 ± 197.2 pmol/l in the no metformin group (P = 0.78).[20] In current study, almost all patients enrolled with diabetes were on metformin and therefore no comparison could be done to delineate effect of metformin. Discrepancy between Indian and western literature may be due to huge difference in prevalence of vitamin B12 deficiency among general population.
Current study also looks at vitamin B12 status of people attending endocrine clinic with diagnosis other than diabetes. This group has significantly higher vitamin B12 levels as compared to tier 3 city population reflecting possibility of supplementation due to contact with healthcare. Another possible explanation may be different food habits of these two populations. Current endocrine practice is situated in a highly urbanised area of national capital territory. Food habits of people residing in this area may be different from those of people living in tier 3 city. But, at the same time, this group has significantly lower vitamin B12 levels as compared to people with diabetes from same clinical practice. This raises the possibility of higher supplementation in people with diabetes. We analysed pre-diabetes as a separate group to assess potential impact of diabetes pathophysiology on vitamin B12 status; but levels were statistically similar in people with pre-diabetes and other endocrine problems.
An argument has been made in literature to consider people with vitamin B12 levels between 200 pg/ml and 300 pg/ml as borderline deficient.[10,16] If these recommendations are considered, then upto 74% of people in India would be potentially deficient for vitamin B12.
STRENGTHS AND LIMITATIONS
This is the largest study from Indian population reporting vitamin B12 status. Data from general population of tier 3 city is likely to be representative of north Indian population at large. However, a few limitations of this study must be mentioned. Data presented here does not exclude people who might have already taken supplements including vitamin B12. But, same limitation has been faced by other researchers worldwide. People attending endocrine practice might have got their vitamin B12 levels evaluated from different laboratories and therefore, using different machines. Current data collected from tier 3 city may underestimate prevalence of vitamin B12 deficiency as it is a retrospective collection of data of people who themselves sought lab testing, so these people may be more health conscious than general population.
CONCLUSION
Prevalence of vitamin B12 deficiency is at least 47% in Indian population and only 26% population may be vitamin B12 sufficient, if people with levels between 200-300 pg/ml are considered borderline deficient. People with diabetes are likely to have higher levels of vitamin B12 presumably due to higher chances of being prescribed with vitamin B12 supplements. In Indian context and in light of this data, it may be prudent to either supplement vitamin B12 in people with neuropathic symptoms or at least rule out vitamin B12 deficiency by testing for it.
With this data, a debate on food fortification for vitamin B12 may be worthwhile in India.[9]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Vitamin B12 Deficiency | National Health Portal Of India. [Last accessed on 2018 Dec 18]. Available from: https://www.nhp.gov.in/disease/bl od-lymphatic/vitamin-b12-deficiency .
- 2.Sasidharan PK. B12 deficiency in India? Arch Med Health Sci. 2017;5:261. doi: 10.4103/amhs.amhs_121_17. [Google Scholar]
- 3.Vecchio MG, Paramesh EC, Paramesh H, Loganes C, Ballali S, Gafare CE, et al. Types of food and nutrient intake in India: A literature review. Indian J Pediatr. 2014;81(Suppl 1):17–22. doi: 10.1007/s12098-014-1465-9. [DOI] [PubMed] [Google Scholar]
- 4.Valencia WM, Florez H. How to prevent the microvascular complications of type 2 diabetes beyond glucose control. BMJ. 2017;356:i6505. doi: 10.1136/bmj.i6505. [DOI] [PubMed] [Google Scholar]
- 5.Singla R, Garg A, Singla S, Gupta Y. Temporal change in profile of association between diabetes, obesity, and age of onset in Urban India: A brief report and review of literature. Indian J Endocrinol Metab. 2018;22:429–32. doi: 10.4103/ijem.IJEM_601_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Diabetes Association. 10. Microvascularcomplications and foot care: Diabetes Care. 2018;41(Suppl 1):S105–18. doi: 10.2337/dc18-S010. [DOI] [PubMed] [Google Scholar]
- 7.ORGI. Census of India: C.D. Block Wise Primary Census Abstract Data (PCA) [Last accessed on 2018 Dec 23]. Available from: http://censusindia.gov.in/pca/cdb_ ca_census/Houselisting housing-HARYANA.html .
- 8.jamovi - Stats. Open. Now. [Last accessed on 2018 Dec 18]. Available from: https://www.jamovi.org .
- 9.de Benoist B. Conclusions of a WHO technical consultation on folateand vitamin B12 deficiencies. Food Nutr Bull. 2008;29(Suppl 2):S238–44. doi: 10.1177/15648265080292S129. [DOI] [PubMed] [Google Scholar]
- 10.Mazokopakis EE, Starakis IK. Recommendations for diagnosis and management of metformin-induced vitamin B12 (Cbl) deficiency. Diabetes Res Clin Pract. 2012;97:359–67. doi: 10.1016/j.diabres.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Refsum H, Yajnik CS, Gadkari M, Schneede J, Vollset SE, Orning L, et al. Hyperhomocysteinemia and elevated methylmalonic acid indicate a high prevalence of cobalamin deficiency in Asian Indians. Am J Clin Nutr. 2001;74:233–41. doi: 10.1093/ajcn/74.2.233. [DOI] [PubMed] [Google Scholar]
- 12.Shobha V, Tarey SD, Singh RG, Shetty P, Unni US, Srinivasan K, et al. Vitamin B12 deficiency & levels of metabolites in an apparently normal urban south Indian elderly population. Indian J Med Res. 2011;134:432–9. [PMC free article] [PubMed] [Google Scholar]
- 13.Naik S, Mahalle N, Bhide V. Identification of vitamin B12 deficiency in vegetarian Indians. Br J Nutr. 2018;119:629–35. doi: 10.1017/S0007114518000090. [DOI] [PubMed] [Google Scholar]
- 14.Yajnik CS, Deshpande SS, Lubree HG, Naik SS, Bhat DS, Uradey BS, et al. Vitamin B12 deficiency and hyperhomocysteinemia in rural and urban Indians. J Assoc Physicians India. 2006;54:775–82. [PubMed] [Google Scholar]
- 15.Yajnik C, Deshmukh U, Katre P, Limaye T. Vitamin B12. Taylor & Francis Group; 2017. 6. Vitamin B12 deficiency in developing and newly industrialising countries; pp. 131–50. doi: 10.1201/9781315119540-7. [Google Scholar]
- 16.Reinstatler L, Qi YP, Williamson RS, Garn JV, Oakley GP., Jr Association of biochemical B12 deficiency with metformin therapy and vitamin B12 supplements: The National Health and Nutrition Examination Survey, 1999-2006. Diabetes Care. 2012;35:327–33. doi: 10.2337/dc11-1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stabler SP. Clinical practice. Vitamin B12 deficiency. N Engl J Med. 2013;368:149–60. doi: 10.1056/NEJMcp1113996. [DOI] [PubMed] [Google Scholar]
- 18.Website NHS. Vitamin B12 or folate deficiency anaemia. [Last accessed on 2018 Dec 23]. Available from: https://www.nhs.uk/conditions/vit min-b12-or-folate deficiencyanaemia/
- 19.Singla R, Bindra J, Singla A, Gupta Y, Kalra S. Drug prescription patterns and cost analysis of diabetes therapy in India: Audit of an endocrine practice. Indian J Endocr Metab (in press) doi: 10.4103/ijem.IJEM_646_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raizada N, Jyotsna VP, Sreenivas V, Tandon N. Serum Vitamin B12 levels in type 2 diabetes patients on metformin compared to those never on metformin: A cross-sectional study. Indian J Endocrinol Metab. 2017;21:424–8. doi: 10.4103/ijem.IJEM_529_16. [DOI] [PMC free article] [PubMed] [Google Scholar]


