Abstract
Background
Hospitalised patients are often not able to correctly identify members of their physician team. Identifying physicians is a critical component of developing the patient–physician relationship and visual aids have been shown to improve physician identification and overall patient satisfaction.
Objectives
The aim of this quality improvement study was to assess the impact of implementation of a physician facecard on the ability of patients to identify their attending physician and other members of the physician team, as well as to evaluate current use of patient whiteboards for physician team identification.
Methods
We prospectively studied 149 patients admitted to the medicine teaching service, who were randomised to receive a physician facecard or usual care. Patients were surveyed to determine their ability to identify physician team members. Observational data was also collected regarding use of patient whiteboards. Additionally, all hospitalists were surveyed to assess their perception of these visual aids.
Results
Patients who received the facecard were more likely to recall the name of the attending physician as compared with the control group (63% vs 32%, p<0.01). Additionally, 68% of patients with the attending name correctly listed on their whiteboard were able to correctly identify the attending physician (p<0.01). Ninety per cent of patients who both received a facecard and had their whiteboard correctly filled out were able to identify the attending physician. Eighty per cent of hospitalists surveyed agreed that use of the facecard added value and 90% disagreed that routine use of the facecard was burdensome.
Conclusion
The use of physician facecards improves the ability of hospitalised patients to identify their attending physicians, and the combined use of facecards and whiteboards may provide additive benefits.
Keywords: facecard, whiteboard, communication, quality improvement
Introduction
More often than not, hospitalised patients are not able to correctly identify the members of their physician team.1 2 This has been attributed to a multitude of factors including the size of academic inpatient medical teams, providers neglecting to properly introduce themselves, frequent hand-offs leading to changes in team members, lack of continuity between outpatient and inpatient care teams and the innate fast-paced environment of inpatient medicine. Being able to identify the members of the physician team, and their respective roles, is a critical component of developing and maintaining the patient–physician relationship with hospitalised patients. Furthermore, all hospitalised patients receive the Centres for Medicare and Medicaid Services (CMS) Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey following discharge which has three questions devoted specifically to communication, a subject that is directly influenced by patient’s interaction and satisfaction with their physician team. It has been shown that patient satisfaction and perception of communication improves when they are able to identify members of their physician team.3 Interventions targeted at improving patient satisfaction have become increasingly popular, particularly as CMS are incorporating patient satisfaction scores into reimbursement.
Strategies targeted at improving patients’ ability to identify their inpatient physicians are diverse and have included formal communication curricula for attending physicians and housestaff,4–6 visual aids including physician facecards5–10 and whiteboards,9 11–14 financial incentives,6 specified rounding styles15 and even social media campaigns that have reaffirmed the importance of healthcare provider introductions in proper patient-centred care.16 These interventions vary in both their methodology and cost of implementation. The literature is heterogeneous with regard to the effectiveness of visual aids; however, the use of physician facecards has been shown to improve the ability of patients to correctly identify the members of their physician team, as well as improve overall satisfaction and HCAHPS scores5 6 17 in some instances. Similarly, the use of whiteboards to display the names of the treatment team, nurses, support staff and treatment goals has been shown to be overwhelmingly welcomed by patients and to lead to improvements in identification of team members as well as overall satisfaction with care.11 12 14 18
Patient–physician communication was identified as the area of focus for quality improvement at our academic medical centre, which serves as the tertiary referral centre for the region. Physician facecards were developed for use within the hospitalist group in the years prior to this study; however, utilisation was not mandated and was variable. Additionally, all patient rooms are equipped with whiteboards with spaces for physician names, team name and daily goals. There has been no standardised policy or procedure in place governing regular use of the whiteboards, with practices varying greatly depending on floor, as well as individual physician and nursing team practices.
The aim of this quality improvement study was to assess the impact of implementation of a physician facecard on the ability of patients to correctly identify their attending physician, as well as evaluate current use of patient whiteboards and compare the effectiveness of this visual aid to the facecard. Lastly, we assessed hospitalist perception of these visual aids.
Methods
This study was completed between November 2017 and April 2018 at the University of Vermont Medical Center in Burlington, Vermont, a tertiary care hospital. A total of 149 patients and 18 internal medicine hospitalists were enrolled in this study.
Intervention
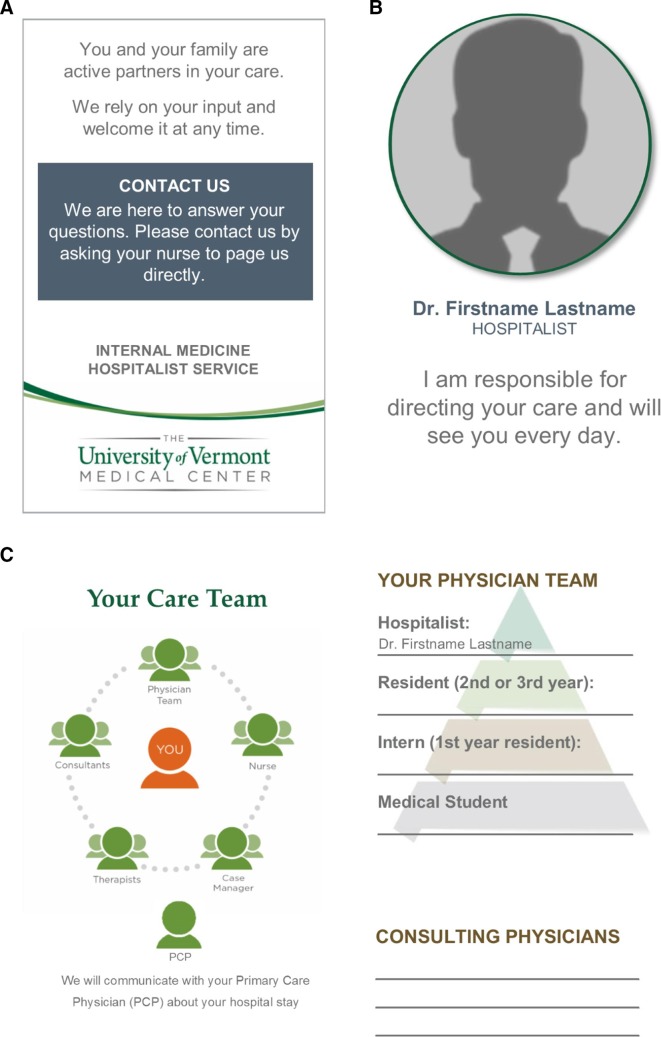
The physician facecard is a bifold card depicting the attending physician’s face and title on the front (figure 1). Inside the card is an illustration of the components of the care team, including physicians, nurses, case managers and consultants, among others. The back of the card contained instructions about how to contact the physician team should questions arise.
Figure 1.
Initial facecard design that was used during the study. The facecard is a bifold card with the top panel representing the back (A) and front (B) of the card, with the bottom panel representing the inside (C). The front includes the name and photo of the attending physician.
The facecard was initially developed by the internal medicine hospital department in conjunction with the hospital marketing department as a means to help with physician identification and to aid in explanation of the many members of the care team. A standardised template was created that was easily customisable to allow for change in name and photo for each attending physician. The facecards were internally produced with a cost to the hospitalist group of only US$1.48 for every 150 cards. Initially, there was no formal introductory process and use was voluntary among hospitalists. Baseline use was variable as was discovered in the hospitalist survey below.
Hospitalist survey
Prior to the study, hospitalists who attend on the teaching services were surveyed to assess their perception of patients’ ability to recognise members of the physician team, as well as hospitalist attitudes towards use of the physician facecards. Questions were formatted using a 3–4 point Likert-type scale (ie, never, sometimes, usually, always) and 0–1 for yes/no questions. The survey was collected anonymously via REDCap electronic data capture tools hosted at our institution.19 Free text elements were available in order to provide feedback regarding facecard use and opportunities for improvement in design.
Study population
Prior to each data collection period, attending hospitalists were randomly selected to be part of the interventional group (use of facecard) or control group (no use of facecard). Patients were eligible for enrollment if they were admitted to one of the inpatient internal medicine teaching services. Hospitalists were enrolled if they were scheduled to attend on the inpatient service during one of the data collection periods. Patients were screened by their primary attending and excluded if they met one of the following criteria: cognitive impairment, non-English speaking, prisoners or wards of the state, minors under the age of 18 and any individual circumstance where the primary attending believed that study participation would be inappropriate or burdensome to the patient (ie, pending procedure or comfort directed care).
Patient interviews
Screened patients were approached by the study team (one internal medicine attending (Gardner) and one resident physician (Wahlberg)) after they had been admitted for at least 1 day. Consent was obtained and a brief interview was conducted to assess their ability to (1) identify the attending physician, (2) identify any other members of the physician team (resident, intern, medical student) and their roles and (3) assess their satisfaction with receiving a physician facecard (or desire to receive one in a subsequent admission if they were part of the control group).
Additional observational data was collected regarding the use of visual communication aids in the room, specifically, whether the attending, resident(s) and team name were written on the patient’s whiteboard.
Analysis
Data was recorded without patient identifiers during patient interviews and the hospitalist survey results were compiled using REDCap. We used unpaired t-tests to compare observational data regarding use of whiteboards and patient satisfaction with the facecard. Similarly, unpaired t-tests were used to compare patients’ ability to identify their attending physician and other members of the physician team based on receipt of a facecard. A contingency table was created to explore a relationship between whiteboard use and receipt of a facecard. This was analysed by calculating a χ2 statistic and using Fisher’s exact test. A logistical regression analysis was performed using the MedCalc statistics package to determine the effect of receipt of facecard and whiteboard use on ability to identify the attending physician.
Patient and public involvement
The initial decision to implement the facecard and subsequently develop a study to better understand its utility was driven by a renewed focus on improving communication and ultimately the patient experience, a hospital and department-wide commitment inspired directly by patient feedback garnered from post-hospitalisation surveys. Patients and patient’s families, in the form of hospital Patient-Family Advisors, were involved throughout the study. The final question of the patient interview was devoted to understanding the patient’s perspective of the benefit, or lack thereof, of receiving a facecard. Patients who were in the control arm of the study and did not receive a facecard were shown a facecard and provided with an explanation of its purpose and then asked for feedback about whether or not a visual aid like the facecard would be beneficial in future hospital encounters. Following the study, the investigators met with Patient-Family Advisors to explain the results of the study and seek feedback during the facecard redesign process.
Results
Visual aids
Facecard
One hundred and forty-nine patients were enrolled in the study, with 80 in the intervention (facecard) arm and 69 in the control arm. Among patients randomised to the intervention arm, 78% received a facecard (table 1). No patients in the control arm received a facecard.
Table 1.
Prevalence of facecard and whiteboard use
| Control group, (N=69) n (%) | Intervention group, (N=80) n (%) | |
| Received facecard | 0 (0) | 62 (78) |
| Attending physician’s name written on whiteboard | 37 (54) | 31 (39) |
| Resident(s) name(s) written on whiteboard | 10 (14) | 12 (15) |
| Team name written on whiteboard | 15 (22) | 12 (15) |
There were no statistically significant differences between the baseline use of whiteboards among the control and intervention groups.
Patients who received the facecard were significantly more likely to be able to recall the name of their attending physician as compared with the control group (63% vs 32%, p<0.01, table 2). Patients who received a facecard were able to identify another member of the physician team 43% of the time, compared with 32% in the control group (p=0.18).
Table 2.
Effect of facecard and whiteboard on patients’ ability to identify attending physician and team roles
| Facecard | |||
| Control group, (N=69) n (%) | Intervention group, (N=80) n (%) | P value | |
| Patient correctly identifies attending physician | 22 (32) | 50 (63) | <0.01 |
| Patient correctly identifies resident | 22 (32) | 34 (43) | 0.18 |
| Whiteboard | |||
| Name not on board, (N=81) n (%) | Name written on board, (N=68) n (%) | P value | |
| Patient correctly identifies attending physician | 26 (32) | 46 (68) | <0.01 |
Of all study patients who received a facecard, 89% reported the card being ‘helpful’. Among the control patients who did not receive a facecard, 87% thought that the concept of a physician facecard would be ‘helpful’ during a future admission.
Whiteboards
In total, the attending name was written on the whiteboard 46% of the time (54% control, 39% intervention. p=0.069, table 1). The resident(s) name and team name were recorded 15% (14% control, 15% intervention. p=0.76) and 18% of the time, respectively (22% control, 15% intervention. p=0.29). Among the 68 study patients who had the attending name recorded on the whiteboard, 68% were able to correctly identify the attending as compared with 32% in the control group (p<0.01, table 2). Furthermore, when examining the 72 patients who both received a physician facecard and had the attending name listed on the whiteboard there was a 90% success rate of correctly identifying the attending physician (table 3). Using χ2 and Fisher’s exact test to analyse a contingency table of whiteboard use and receipt of facecard suggested no association between the two variables (p=0.06)
Table 3.
Effect of facecard and whiteboard on patients’ ability to identify attending physician
| Name on whiteboard | No name on whiteboard | Total | |
| Received facecard n (%) | 28 (39) | 22 (31) | 50 (70) |
| No facecard n (%) | 18 (25) | 4 (6) | 22 (31) |
| Total n (%) | 46 (54) | 26 (37) |
The 72 patients included were the subset of patients from the study who correctly identified the attending physician.
A logistical regression analysis was performed to further evaluate the independent effects of facecard and whiteboard use on ability to identify the attending physician, which demonstrated increased odds of identifying the attending physician with the receipt of both the facecard (OR 7.4, 95% CI 3.0 to 18.0. p<0.0001) and the whiteboard (OR 8.7, 95% CI 3.6 to 21.3. p<0.0001).
Hospitalist survey
Of the 18 attending hospitalists who were surveyed prior to the study, 16 (89%) responded. On average, hospitalists think that patients only ‘sometimes’ have a good understanding of the attending physician’s role on the team, with similar results for resident and medical student roles (table 4).
Table 4.
Hospitalist survey regarding use of facecard prior to the study
| Response (frequency) | |
| Do you think your patients have a good understanding of your role on the team? | Never (0) Sometimes (5) Usually (11) Always (0) |
| Do you think your patients have a good understanding of the resident's role on the team? | Never (1) Sometimes (8) Usually (7) Always (0) |
| Do you think your patients have a good understanding of the medical student's role on the team? | Never (0) Sometimes (11) Usually (5) Always (0) |
| Do you use the facecard while attending on the inpatient Medicine services? | Never (6) Sometimes (5) Always (5) |
| If improvements were made to the facecard, would you be more likely to begin using it? (among those who answered ‘no’ to previous question) | No (2) Yes (4) |
| Do you feel that use of the facecard improves the communication between the patient and the physician care team? | No (2) Yes (8) |
| Do you feel that use of the facecard adds a significant amount of time to the patient encounter? | No (9) Yes (1) |
Baseline usage of the physician facecard was variable, average use was reported as ‘sometimes’. Reasons for not using the facecard included but were not limited to: ‘Never getting in the habit of using it’, ‘forgot about it’ and ‘I don’t like them’. Of those who were not regularly using the card, 70% stated that they would be more likely to use the card if improvements were made.
Importantly, 80% of hospitalists believed that use of the facecard improved communication between patients and the physician care team. Furthermore, only 10% perceived that use of the facecard imparted a significant amount of time or burden to the patient encounter.
Discussion
The use of a physician facecard was able to significantly improve patients’ ability to identify their attending physician. Similarly, while patient whiteboards were not designed as a specific intervention in this study, it was found that they also portend a significant improvement in identification of providers. Perhaps the most interesting finding is a suggested ‘additive’ benefit with use of both visual aids, where 90% of patients who both received a facecard and had their whiteboard correctly filled out were able to correctly identify their attending physician by name.
Though use of the facecard was mandated for those randomised to the intervention group, patients in this cohort only reported receiving a facecard 78% of the time. While it is possible that this is partially accountable by patients forgetting that they had received a card, it is more likely reflective of real-life practice and other studies have shown similar rates of use.10 It should also be noted that baseline use of the whiteboards was low (attending name recorded 46% of the time), particularly with regard to the recording of residents (15%) and team (18%) names. Prior studies have shown similar baseline usage rates9 11 and have demonstrated significant improvement in adherence following simple education. Regular use then resulted in a significant improvement in ability of patients to identify their providers, a testament to the low-cost, high-reward value of visual aids.
Although our study demonstrated a benefit from use of visual aids, the intervention group was still only able to correctly identify the attending physician 63% of the time. Prior studies are quite variable with regard to the effectiveness of facecards, some reporting marginal benefit (21%) and others near perfect (89%).7 10 The heterogeneity may be due in part to small sample sizes, as well as the countless other factors involved in patient care that influence the ability to remember the name of a provider.
Our survey of participating hospitalists showed that physicians believe that patients only ‘sometimes’ understand who they are or what their specific role is on the treatment team, which is similar to the 48% of all study patients who could correctly identify the attending physician. There was a favourable perception of the facecard and its potential to improve patient communication. Importantly, physicians did not perceive that routine use of the facecard imparted a significant time burden to their workday, which is a common sentiment in other studies as well.8 14
There are several limitations to our study. First, some of the eligibility criteria for patient enrollment involved subjective decision-making by attending physicians such as excluding patients based on baseline cognitive impairment or the belief that participation would be too burdensome and therefore could have inserted a degree of selection bias. As there was variable baseline use of the facecard prior to the study, some physicians were much more accustomed to routine use of the card which could have impacted its effectiveness. Importantly, however, there were eight different attending physicians accounting for the 28/31 patients who correctly identified their attending after both receiving a facecard and having the name written on the whiteboard, suggesting that this effect was not the result of just a few very effective physicians. One cannot discount the role of the Hawthorne effect in this study, as physicians in the control group may have been more likely to spend more time introducing themselves or updating the whiteboard when they previously would not have done so. Rounding style was not controlled during this study, with routine use of hallway rounding, bedside rounding and card-flipping rounds throughout the different inpatient teams. As hallway rounding and bedside rounding are thought to lead to improvements in communication and patient care,15 it is possible that variability in rounding style confounded the data. HCAHPS scores were not an outcome of this study, but we acknowledge that this could be an important measure to investigate in the future to fully assess the impact of visual aids. Lastly, our exclusion criteria were deliberately few with the goal of generalising our study population to include as many of the general medicine patients as possible, and as a consequence there are some factors, such as length of stay, that could certainly have an impact on a patient’s ability to identify members of their treatment team irrespective of receipt of a facecard. One would expect that the likelihood of identifying members of the treatment team to increase with length of stay and number of encounters with the same providers.
This study demonstrates that the use of visual aids, including physician facecards and patient whiteboards, serve to improve patients’ ability to identify their attending physicians. However, we recognise that the baseline utilisation of both the facecards and whiteboards is low, which leaves room for significant improvement. We suspect that the reason for low baseline whiteboard usage is lack of a standardised protocol across the many different patient floors that the inpatient medicine teams utilise. For example, on some floors, nursing updates the treatment team on the board regularly and on other floors the whiteboard is designated for other nursing communication and displaying the treatment team is not prioritised. This lack of whiteboard standardisation often leads to inconsistent use. Another contributing factor to variable use is the rounding style of the physician team, as teams who bedside round as large group may often delegate one member of the team to update the whiteboard while another is leading the conversation at the bedside. Regardless, this is an area that is ripe for improvement, and we plan to begin a quality improvement initiative to increase use through education of the physician teams about the benefits of whiteboard use. Of note, a new medical ward will be opening in our hospital within the next year that will feature a computerised tablet at the bedside that will automatically load the names and photos of members of the treatment team in real time, serving as an automated way to deliver the information that a facecard and whiteboard would otherwise provide. This technology does not seem to be widespread at this time, but should be an area for future study.
As part of our ongoing quality improvement initiative focusing on communication, we sought to make improvements to the facecard based on suggestions from attending physicians in the survey, direct feedback from patients following the study interviews, meetings with the hospitalist Patient Experience Committee and Patient-Family Advisors. A specific example of improvement includes dedicating space in the card to identify each member of the physician team by name including residents, interns and medical students, as our data clearly show that the current iteration was not successful in helping patients identify these crucial members of their care team (figure 2). We have shared the findings of this study with attending and resident physicians in the department of medicine with the goal of encouraging use, as our survey of hospitalists showed that there was willingness to increase use of the cards if improvements were made. Since the facecards are currently utilised only by attending hospitalists at our institution, there is very minimal time and labour needed to create new cards, which is a challenge that has been mentioned by other groups who utilise these cards for residents and other members of the treatment team that often change on a weekly basis.
Figure 2.
Revised facecard design. The facecard was redesigned after obtaining feedback from patients, Patient-Family Advisors and physicians. The top panel represents the back (A) and front (B) of the card, with the bottom panel representing the inside (C).
This study demonstrates that whiteboards and facecards are low cost (less than US$0.01 per card), high-yield interventions that can help improve patient’s ability to identify their attending physician. Importantly, the use of physician facecards is regarded as helpful by physicians and not perceived to impose extra time or undue burden to the patient encounter. In addition to the demonstrated benefits of facecards in this study, it is our hope that the true sustainability from this intervention will come from a change in culture with renewed focus on introductions and explanation of team structure that will persist beyond the use of a visual aid and ultimately lead to improvement in the patient experience.
Acknowledgments
We would like to thank Alan Howard of the Larner College of Medicine at the University of Vermont Medical Center for his guidance with the statistical analysis, as well as Dr Allen Repp for his expert guidance and feedback. We would also like to thank the University of Vermont Medical Center Patient-Family Advisors for their thoughtful feedback and guidance throughout the study.
Footnotes
Contributors: ZG and SL were responsible for the conception and initial design of the study and study materials, with KW helping to finalise the study materials and IRB protocol. Data collection was performed by KW and ZG. Data analysis was primarily performed by KW with guidance from ZG. KW is the primary author of the manuscript, but ZG and SL were involved in the revision and approval process.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The University of Vermont Medical Center Institutional Review Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are available upon reasonable request.
References
- 1. Arora V, Gangireddy S, Mehrotra A, et al. . Ability of hospitalized patients to identify their in-hospital physicians. Arch Intern Med 2009;169:199–201. 10.1001/archinternmed.2008.565 [DOI] [PubMed] [Google Scholar]
- 2. O'Leary KJ, Kulkarni N, Landler MP, et al. . Hospitalized patients' understanding of their plan of care. Mayo Clin Proc 2010;85:47–52. 10.4065/mcp.2009.0232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Francis JJ, Pankratz VS, Huddleston JM. Patient satisfaction associated with correct identification of physician's Photographs. Mayo Clin Proc 2001;76:604–8. 10.1016/S0025-6196(11)62411-7 [DOI] [PubMed] [Google Scholar]
- 4. Boissy A, Windover AK, Bokar D, et al. . Communication skills training for physicians improves patient satisfaction. J Gen Intern Med 2016;31:755–61. 10.1007/s11606-016-3597-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Horton DJ, Yarbrough PM, Wanner N, et al. . Improving physician communication with patients as measured by HCAHPS using a standardized communication model. Am J Med Qual 2017;32:617–24. 10.1177/1062860616689592 [DOI] [PubMed] [Google Scholar]
- 6. Dutta SFF, Behel J. How we improved Hospitalist-Patient communication. NEJM catalyst, 2016. April 6 Available: https://catalyst.nejm.org/how-we-improved-hospitalist-patient-communication/ [Accessed 8 Jul 2018].
- 7. Arora VM, Schaninger C, D'Arcy M, et al. . Improving inpatients' identification of their doctors: use of face cards. Jt Comm J Qual Patient Saf 2009;35:613–9. 10.1016/S1553-7250(09)35086-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gottenborg ELS, Mourad M, Morduchowicz S, et al. . Face Cards Improve Patient Perception of Physician Communication [abstract]. J Hosp Med 2014;9(Suppl 2). [Google Scholar]
- 9. Goyal AA, Tur K, Mann J, et al. . Do bedside visual tools improve patient and caregiver satisfaction? A systematic review of the literature. J Hosp Med 2017;12:930–6. 10.12788/jhm.2871 [DOI] [PubMed] [Google Scholar]
- 10. Simons Y, Caprio T, Furiasse N, et al. . The impact of facecards on patients' knowledge, satisfaction, trust, and agreement with hospital physicians: a pilot study. J Hosp Med 2014;9:137–41. 10.1002/jhm.2100 [DOI] [PubMed] [Google Scholar]
- 11. Cholli P, Meyer EC, David M, et al. . Family perspectives on Whiteboard use and recommendations for improved practices. Hosp Pediatr 2016;6:426–30. 10.1542/hpeds.2015-0182 [DOI] [PubMed] [Google Scholar]
- 12. Maniaci MJ, Heckman MG, Dawson NL. Increasing a patient's ability to identify his or her attending physician using a patient room display. Arch Intern Med 2010;170:1084–5. 10.1001/archinternmed.2010.158 [DOI] [PubMed] [Google Scholar]
- 13. Sehgal NL, Green A, Vidyarthi AR, et al. . Patient whiteboards as a communication tool in the hospital setting: a survey of practices and recommendations. J Hosp Med 2010;5:234–9. 10.1002/jhm.638 [DOI] [PubMed] [Google Scholar]
- 14. Tan M, Hooper Evans K, Braddock CH, et al. . Patient whiteboards to improve patient-centred care in the hospital. Postgrad Med J 2013;89:604–9. 10.1136/postgradmedj-2012-131296 [DOI] [PubMed] [Google Scholar]
- 15. Shoeb M, Khanna R, Fang M, et al. . Internal medicine rounding practices and the accreditation Council for graduate medical education core competencies. J Hosp Med 2014;9:239–43. 10.1002/jhm.2164 [DOI] [PubMed] [Google Scholar]
- 16. Granger K. Healthcare staff must properly introduce themselves to patients. BMJ 2013;347:f5833 10.1136/bmj.f5833 [DOI] [PubMed] [Google Scholar]
- 17. O'Leary KJ, Darling TA, Rauworth J, et al. . Impact of hospitalist communication-skills training on Patient-satisfaction scores. J Hosp Med 2013;8:315–20. 10.1002/jhm.2041 [DOI] [PubMed] [Google Scholar]
- 18. Singh S, Fletcher KE, Pandl GJ, et al. . It's the writing on the wall: Whiteboards improve inpatient satisfaction with provider communication. Am J Med Qual 2011;26:127–31. 10.1177/1062860610376088 [DOI] [PubMed] [Google Scholar]
- 19. Harris PA, Taylor R, Thielke R, et al. . Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]