Abstract
The current study examines the continuity in comorbidity between substance use and internalizing mental health problems from adolescence to adulthood and investigates the general and specific predictors of comorbidity across development. Participants were drawn from the Seattle Social Development Project (N = 808), a gender-balanced, ethnically diverse longitudinal panel. Structural equation modeling was used to examine risk factors for comorbid substance use and internalizing problems in family and peer social environments; substance use- and mental health-specific social environments (family tobacco, alcohol, and marijuana use; family history of depression); and individual risk factors (behavioral disinhibition). Latent factors were created for comorbid substance use and mental health problems at ages 13–14 and comorbidity of substance abuse and dependence symptoms and mental health disorder symptoms at ages 30–33, and included indicators of anxiety, depression, alcohol, tobacco, and marijuana problems. Comorbid problems in adolescence predicted later comorbidity of disorders in adulthood. In addition, family tobacco environment and behavioral disinhibition predicted adolescent comorbidity, while family history of depression was associated with adult comorbidity. Finally, family and peer substance use in adolescence predicted substance use (alcohol, tobacco, and marijuana) both in adolescence and adulthood. The pattern of results suggests that comorbidity in adolescence continues into adulthood, and is predicted by both general and behavior-specific environmental experiences during adolescence. Findings clarify the etiology of comorbid internalizing and substance use problems, and suggest potential preventive intervention targets in adolescence to curb the development of comorbidity in adulthood.
Keywords: Comorbidity, dual diagnosis, substance use, internalizing disorders, etiology
Co-occurrence of substance use disorders with internalizing disorders is a form of comorbidity that holds particular clinical and public health importance. Among those diagnosed with at least one psychiatric disorder, comorbid diagnoses are associated with more severe and persistent illness among both adolescents (Costello, Mustillo, Erkanli, Keeler, & Angold, 2003) and adults (Kessler, 2004; Kessler, Chiu, Demler, Merikangas, & Walters, 2005; Najt, Fusar-Poli, & Brambilla, 2011). Patients with comorbid diagnoses tend to have a longer course of illness, greater functional impairment, utilize services at a higher rate (Graaf, Bijl, Smit, Vollebergh, & Spijker, 2002), and have often been exposed to significantly more environmental adversity (Kessler, 2004). Additionally, there is a lack of adequate integrated treatments specific to dually diagnosed patients, and pharmacological treatments for these patients pose additional risk (Kessler, 2004). Comorbidity of mental health problems with substance use disorder is also common enough to be the “rule rather the exception” among adults (Dell’Osso & Pini, 2012; Eaton, Rodriguez-Seijas, Carragher, & Krueger, 2015), with studies reporting that half of respondents with a substance use disorder also had a mental health disorder, and half of those with a mental health disorder also had a substance use disorder (Kessler et al., 2005). Prevalence of comorbid psychiatric diagnoses is similar among adolescents, with 40% of adolescents meeting criteria for more than one psychiatric illness (Merikangas et al., 2010). Given the severity of outcomes associated with comorbidity and its relative frequency, it is important to understand the predictors of comorbidity relative to single disorders and the developmental progression of comorbidity from adolescence to adulthood.
The risk and protective factors of comorbid psychiatric and substance use disorders are rarely explored (Dell’Osso & Pini, 2012; Swendsen & Merikangas, 2000), and long-term longitudinal studies in this area are rare, leading to a call for the study of the course and etiology of comorbidity (Krueger & Markon, 2006). Studies have established that anxiety and depression most often precede substance use disorders (Costello, Erkanli, Federman, & Angold, 1999; Costello et al., 2003), and that problems with substance use and mental health amongst adults often began in adolescence (Kessler, 2004; Kushner, Abrams, & Borchardt, 2000; Merikangas et al., 1998; Najt et al., 2011). Few studies, however, have explicitly examined the developmental progression of comorbidity (Costello et al., 2003). Further, although there are many risk factors that are common to both types of disorders (Green, Zebrak, Fothergill, Robertson, & Ensminger, 2012), few studies have tested whether these risk factors are also predictors of comorbidity (Armstrong & Costello, 2002; Green et al., 2012; Najt et al., 2011).
Existing studies of family, peer, and individual psychopathological risk factors for comorbid internalizing disorders and substance use suggest that there may be distinct etiologies for mental health, substance use problems, and their comorbidity. We are aware of three studies of comorbidity risk factors; among these, all found unique family and adolescent predictors of comorbidity, though there was no agreement as to which risk factors uniquely predict comorbidity. For example, Green and colleagues (2012) found that family influences were more closely related to depression, while early behavior problems were linked to substance use problems in adulthood. Similarly, Aseltine and colleagues (1998) found family environments to be associated with adolescent comorbidity, but also reported that peer support was related to depression uniquely and peer pressure was related to substance use uniquely (Aseltine et al., 1998). In another longitudinal cohort study, Salom and colleagues (2014) found that low maternal warmth was associated with comorbid mental health disorders and alcohol use disorders at age 21; maternal warmth uniquely predicted comorbidity of the two disorders compared to alcohol use disorders alone, and adolescent internalizing and drinking predicted comorbidity compared to mental health disorders alone (Salom et al., 2014). None of the studies examined the developmental timing of risk factors. The current study aims to address these gaps in understanding of the etiology of comorbid mental health and substance use disorders, by specifically examining the developmental progression of comorbidity, testing for common and unique risk factors in order to identify appropriate prevention and treatment targets.
The General-Specific Framework
Given the challenge of capturing the complexity of environmental contributions to comorbid outcomes, a framework that organizes the environment and outcomes into general and problem-specific components has been shown to be useful (Bailey, Hill, Meacham, Young, & Hawkins, 2011; Bailey et al., 2014; Epstein, Hill, Bailey, & Hawkins, 2013;Newcomb & McGee, 1991). General risk factors are theorized to predict a range of behavioral outcomes, including mental health and substance use, whereas specific predictors are linked more to a single behavioral outcome. For example, family warmth and positive involvement are likely to predict both better mental health and fewer substance using behaviors, whereas parent smoking is likely to only be associated with the likelihood of child smoking. Thus, environmental and personal risk and protective factors can be organized into those that are more general in nature and those that are specific to a disorder.
General Risk Factors
There are a number of risk factors that have been found to predict both mental health and substance use problems during adolescence and adulthood. In the present study, we focus on three domains of risk: a) family environment, b) peer environment, and c) individual risk. We chose these domains because their influence is salient during childhood and adolescence (Catalano, Kosterman, Hawkins, Newcomb, & Abbott, 1996), they are likely to be implicated in the development of comorbidity, and they are potential targets for preventive interventions.
Several risk factors in the family domain are "general" in nature. For example, poor family functioning, including low parent monitoring and warmth, and increased parent withdrawal are related to increased anxiety and depression in adolescence (Repetti, Taylor, & Seeman, 2002;Yap & Jorm, 2015; Yap, Pilkington, Ryan, & Jorm, 2014), which can have long-lasting effects into adulthood (Jones et al., 2016; Yap et al., 2014). Similarly, poor general family functioning has also been linked to substance use and dependence, both in adolescence (Hawkins, Catalano, & Miller, 1992) and adulthood (Stone, Becker, Huber, & Catalano, 2012). In a similar vein, peer networks have also been shown to be influential in mental health and substance use across development (Aseltine et al., 1998;Hawkins et al., 1992; Lee et al., 2012; Reynolds & Crea, 2015; Stone et al., 2012).
In the domain of individual risk, behavioral disinhibition, or the tendency toward impulsivity and sensation seeking, has been strongly associated with substance use across development (Iacono, Malone, & McGue, 2008; McGue, Iacono, Legrand, Malone, & Elkins, 2001). Negative affect in combination with disinhibition is thought to lead to externalizing problems, including substance use (Krueger & Markon, 2006); thus, disinhibition may be an individual characteristic driving comorbidity. Unlike family or peer influences, behavioral disinhibition is seen as a stable trait that is probably genetically determined (Iacono, Carlson, Taylor, Elkins, & McGue, 1999; Iacono et al., 2008) and that works in concert with environmental influence to affect risk behavior and mental health.
Specific Risk Factors
Risk factors specific to substance use in the family, peer, and individual domains include family substance use, peer substance use, and past history of using substances (Stone et al., 2012). Children of parents who use alcohol are more likely to use alcohol as adolescents and adults (Merline, Jager, & Schulenberg, 2008; Peterson, Hawkins, Abbott, & Catalano, 1994). Children of parents who smoke are more likely to smoke in adolescence (Avenevoli & Merikangas, 2003; Chassin et al., 2005; Epstein et al., 2013) and continue into adulthood (Epstein et al., 2013; Mays et al., 2014). Children of parents who use marijuana are more likely to use marijuana (Bailey, Hill, Oesterle, & Hawkins, 2006). Peer substance use has also been shown to be a strong predictor of substance use across development (Hawkins et al., 1992; Oxford, Oxford, Harachi, Catalano, & Abbott, 2001; Stone et al., 2012), though it is unknown how it is related to comorbidity. Finally, exposure to family mental health problems has been linked to mental health problems in adolescence (Mars et al., 2012; McCauley, Pavlidis, & Kendall, 2001) and adulthood (Mars et al., 2012; Weissman et al., 2006).
Specific substance use risk factors have a clear connection to the use of specific substances; some have been shown to cross domains—for example, substance-specific social environments can impact mental health functioning (Harter, 2000; Jones et al., 2016), and family mental health and peer functioning can influence substance use (Stone et al., 2012). These cross-domain risk factors are important to evaluate in the development of comorbidity, as they may have a specific role to play in fostering the development of comorbid mental health and substance use problems.
The Present Study
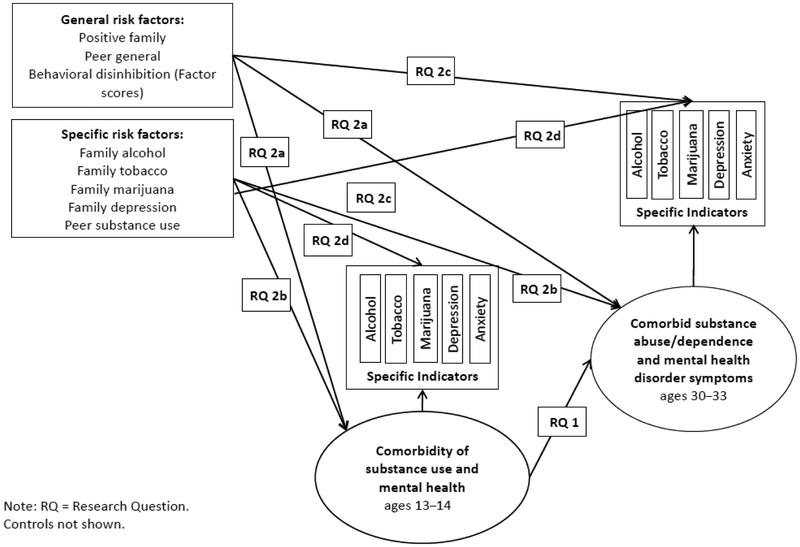
The present paper addresses gaps in the existing literature on comorbidity between mental health and substance use disorders by examining the etiology and developmental progression of comorbid substance use and mental health problems. Specifically, this work examines continuity in comorbidity from adolescence to adulthood and tests general and specific predictors of comorbidity in adolescence and adulthood. We model comorbidity as the shared variance in tobacco, marijuana, alcohol, anxiety, or depression problems in adolescence (ages 13–14) and in adulthood (ages 30–33). The escalation of issues from adolescence to adulthood was captured by modeling substance use and internalizing symptoms in adolescence, progressing to anxiety and depression disorder symptoms, and substance abuse or dependence symptoms in adulthood. Multivariate, quantitative approaches to modeling comorbidity have been proposed as a way to disentangle etiological pathways to comorbid conditions and to account for significant correlation between disorders (Krueger & Markon, 2006). That is, we can model the degree to which general and specific risk factors predict a given behavior over and above their role in predicting comorbidity. For example, it is possible that general family functioning, in addition to playing a role in predicting comorbidity between mental health and substance use, has an additional effect on depression symptoms. Figure 1 provides a conceptual model representing the following research questions:
Figure 1.
Conceptual model of hypothesized structural pathways between risk factors, comorbidity, and specific indicators.
To what extent does comorbidity between alcohol use, tobacco use, marijuana use, depression, and anxiety in adolescence lead to comorbidity in these problems in adulthood?
To what extent do general and problem-specific risk factors in adolescence predict comorbidity in adolescence and adulthood?
Method
Sample
Data were drawn from the Seattle Social Development Project (SSDP), a community-based sample of 808 participants in Seattle, Washington. SSDP is a longitudinal study of the development of prosocial and antisocial behaviors that was established in 1985. All fifth graders and their parents from 18 schools across Seattle were recruited to participate in the study (N=1,053), and 77% enrolled (N = 808). Additional information about the sampling procedures and study design can be found elsewhere (Hawkins et al., 2003). The sample is gender balanced (49% female) and ethnically diverse, (47% identify as Caucasian, 26% African American, 22% Asian American, and 5% Native American). Over half (52%) of the participants were low income as determined by enrollment in the National School Lunch/School Breakfast program at least 1 year between fifth and seventh grade. Participants have been interviewed at ages 10, 11, 12, 13, 14, 15, 16, and 18, 21, 24, 27, 30, and 33. Structured interviews were conducted in person during the earlier waves of the study; other interviews have been done over the phone or online. Respondents’ parents completed paper surveys when participants were age 10–16, and teachers completed paper surveys at ages 10–14. Retention rates averaged 90% through age 33. The final analysis sample included 765 participants; Native Americans (N = 43) were not included in the present analyses due to their small sample size. The institutional review board at the University of Washington approved all study procedures.
Measures
Substance use and mental health indicators in adolescence (ages 13–14).
Past-month alcohol, cigarette, and marijuana use were self-reported at ages 13 and 14. Alcohol and tobacco use frequency were coded as 0 = no use, 1 = used one time, or 3 = used two or more times. Marijuana use was coded as 0 = no use or 1 = any use. The maximum frequency for each substance at age 13 or 14 was used and represented problematic use at this point in development.
Adolescent anxiety and depression scores were based on the teacher report form of the Child Behavior Checklist (CBCL; Achenbach, 1991; Lengua, Sadowski, Friedrich, & Fisher, 2001). The specific items used to measure anxiety (7 items) and depression (10 items) were based on scaling and validation work by Lengua and colleagues (2001). Items were summed and recoded as 0 = no symptoms, 1 = 1–2 symptoms, and 3 = 3 or more symptoms to create a categorical index. The maximum score across ages 13 and 14 was used in analyses.
Substance use and mental health indicators in adulthood (ages 30–33).
At ages 30 and 33, participants completed the Diagnostic Interview Schedule (Robins, Helzer, Croughan, Williams, & Spitzer, 1981), which yielded Diagnostic and Statistical Manual, Fourth Edition (DSM-IV; American Psychiatric Association, 1994) past-year symptom counts for alcohol abuse or dependence, nicotine dependence, marijuana abuse or dependence, major depressive episode, and generalized anxiety disorder. For each disorder, the maximum number of criteria endorsed across ages 30 and 33 was used. Consistent with previous work (Bailey et al., 2011), the number of substance use criteria was truncated at 4+, and the number of anxiety and depression criteria was truncated at 6+ because few respondents reported higher numbers of criteria.
General risk factors.
Items for the general and substance-specific environment scales were developed based on the social development model (SDM; Catalano et al., 1996) and created specifically for the SSDP. Detailed information is available on these measures elsewhere (a measurement appendix can be found here: Bailey et al., 2011; Epstein et al., 2013; Lee et al., 2012). A positive family environment scale included youth reports of family management, involvement, bonding, and conflict (reverse coded) measured prospectively at ages 10–12. Items were averaged within each year, then averaged across ages 10–12 to create a scale of positive family environment (α = .80). A peer general environment scale included prospectively reported perceptions of peer antisocial behavior at ages 10–12. For each of their three best friends, respondents were asked, “Does this friend get in trouble with the teacher?” Responses for each friend were averaged within each year, and then averaged across years to create a scale of general peer environment (α = .65).
A measure of behavioral disinhibition (BD) was only available starting at age 14. Items included, “How many times have you done what feels good no matter what,” with response options “never” = 1, “I’ve done it but not in the past year” = 2, “less than once a month” = 3, “about once a month” = 4, “2 or 3 times in a month” = 5, or “once a week or more” = 6. In order to capture the BD as a stable trait, we sought to capture its stability across the early life course by creating a two-level latent variable. Items within time created a first-order latent factor for each age (five items ages 10–16; three items at ages 18, 21, 24, and 27), with significant loadings ranging from .44 to .89 (p < 0.01); a second-order latent factor then captured the stable variance in BD items over time, with significant loadings ranging from .74 to .87 (p < 0.001). Reliability of items within in each time point was sufficient, Cronbach’s alpha of standardized scores ranged from .63 – .79. Factor scores of the second order BD latent factor were saved and included in the model.
Specific risk factors.
The alcohol, tobacco and marijuana family environment (ages 10–12) scales were prospectively measured and included items on parent and sibling alcohol, tobacco and marijuana use; parent attitudes towards each substance; and involvement of the respondent in the parents’ alcohol and tobacco use (i.e., getting or opening an alcoholic drink or getting or lighting cigarettes for a parent). Items were averaged within year, then across ages to create a family alcohol environment scale (α = .72), and a family tobacco environment scale (α = .66), and a family marijuana environmental scale (same as the other two, excepting items regarding handling of marijuana products; α = .45). Family depression was measured retrospectively as a count of the total number of family members (mother, father, sibling, or other family members) with a history of depression (range 0 to 4), retrospectively reported by the respondent at age 24.
A peer substance use measure (ages 10–13) consisted of target youth’s prospective reports as to whether each of their three best friends used alcohol or marijuana. The number of friends who used each substance was averaged across ages.
Analysis
Structural equation models were estimated using Mplus version 7.11 (Muthén & Muthén, 2008). All substance use and mental health problem indicators were specified as ordered categorical, and the Weighted Least Squares Means Variances (WLSMV) estimator was used with THETA parameterization. Missing data were accounted for with Full Information Maximum Likelihood estimation. We created two comorbidity latent factors in adolescence and adulthood using confirmatory factor analysis; these variables will be referred to as the shorthand “comorbidity” when referred to in the text.
Research question 1 (RQ1) focused on the path linking comorbidity in adolescence to comorbidity in adulthood. Relevant paths for research question 2 (RQ2) included a) pathways between the general risk factors (positive family environment, peer general environment, and behavioral disinhibition) and the comorbidity latent variables in adolescence (ages 13–14) and adulthood (ages 30–33); b) pathways between general risk factors and each of the specific indicators of depression, anxiety, and problem use of tobacco, alcohol and marijuana in adolescence and adulthood; c) pathways from specific risk factors (family depression, family tobacco, alcohol, and marijuana use, and peer substance use) to comorbidity at both time points; and d) pathways between specific risk factors and corresponding specific indicators at both time points (e.g., family alcohol environment to alcohol residual). Control variables included gender, race, and socioeconomic status based on eligibility for free or reduced-price school lunch when participants were in Grades 5, 6, and 7 (ages 10–12). Controls were correlated with endogenous variables and regressed on the latent comorbidity factors.
Results
Structural Equation Models
Correlations among model variables and descriptive statistics are reported in Table 1. Confirmatory factor analysis was used to construct the two latent comorbidity variables to model the shared variance amongst indicators of anxiety, depression, alcohol, tobacco, and marijuana use in adolescence (ages 13–14) and adulthood (ages 30–33), connected by a regression path. All indicators significantly loaded onto each comorbidity factor (see Table 2 for coefficients). Within each age, residuals of depression and anxiety were allowed to correlate, which significantly improved fit (χ2(2) = 118, p < .001). Given previous findings documenting significant continuity in substance use and mental health across development, we tested whether adding additional paths between residuals from adolescence to adulthood (e.g., smoking in adolescence to tobacco disorder in adulthood) would improve fit. Significant correlations between smoking in adolescence and adulthood, and anxiety at both time points, were retained, which also significantly improved fit (χ2(2) = 21, p < .001). The fit of the final measurement model was good: χ2(30) = 76, p < 0.001, CFI = .97, TLI = .96, RMSEA = .05.
Table 1.
Descriptive Statistics and Correlations Between Predictors at Ages 10–12 and Outcomes at Ages 13–14 and 30–33
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Marijuana symptoms 30–33 | - | |||||||||||||||||
| 2 | Alcohol symptoms 30–33 | 0.26 | - | ||||||||||||||||
| 3 | Tobacco symptoms 30–33 | 0.23 | 0.37 | - | |||||||||||||||
| 4 | Depression symptoms 30–33 | 0.18 | 0.19 | 0.26 | - | ||||||||||||||
| 5 | Anxiety symptoms 30–33 | 0.16 | 0.16 | 0.24 | 0.56 | - | |||||||||||||
| 6 | Depression 13–14 | 0.08 | 0.14 | 0.21 | 0.16 | 0.18 | - | ||||||||||||
| 7 | Anxiety 13–14 | −0.01 | 0.1 | 0.08 | 0.11 | 0.17 | 0.49 | - | |||||||||||
| 8 | Alcohol 13–14 | 0.1 | 0.1 | 0.12 | 0.06 | 0.07 | 0.19 | 0.1 | - | ||||||||||
| 9 | Tobacco 13–14 | 0.05 | 0.08 | 0.28 | 0.14 | 0.15 | 0.26 | 0.14 | 0.4 | - | |||||||||
| 10 | Marijuana 13–14 | 0.11 | 0.04 | 0.14 | 0.13 | 0.15 | 0.22 | 0.14 | 0.4 | 0.74 | - | ||||||||
| 11 | Positive family | −0.06 | −0.04 | −0.02 | −0.06 | −0.1 | −0.09 | −0.09 | −0.06 | −0.17 | −0.05 | - | |||||||
| 12 | Peer general | 0.1 | 0.11 | 0.16 | 0.02 | 0.05 | 0.16 | 0.06 | 0.18 | 0.1 | 0.1 | −0.2 | - | ||||||
| 13 | Family alcohol | 0.03 | 0.09 | 0.02 | −0.07 | 0.01 | 0.01 | 0.07 | 0.07 | 0.03 | −0.03 | 0.03 | −0.04 | - | |||||
| 14 | Family tobacco | 0.06 | 0.08 | 0.16 | 0.04 | 0.05 | 0.15 | 0.07 | 0.12 | 0.22 | 0.15 | −0.02 | −0.03 | 0.28 | - | ||||
| 15 | Family marijuana | 0.1 | 0.09 | 0.07 | 0.02 | 0.04 | 0.12 | 0.13 | 0.09 | 0.14 | 0.18 | −0.12 | 0.13 | 0.3 | 0.36 | - | |||
| 16 | Family depression | 0.12 | 0.09 | 0.18 | 0.29 | 0.32 | 0.11 | 0.09 | 0.1 | 0.25 | 0.06 | 0 | −0.02 | 0.07 | 0.03 | 0.09 | - | ||
| 17 | Behavioral disinhibition | 0.21 | 0.32 | 0.29 | 0.06 | 0.13 | 0.16 | 0.07 | 0.25 | 0.29 | 0.15 | −0.1 | 0.22 | 0.14 | 0.07 | 0.1 | 0.12 | - | |
| 18 | Peer substance use | 0.01 | 0.11 | 0.08 | 0.07 | 0.1 | 0.18 | 0.12 | 0.31 | 0.37 | 0.29 | −0.19 | 0.29 | 0.04 | 0.11 | 0.18 | 0.08 | 0.16 | - |
| Mean | 0.36 | 0.86 | 1.16 | 1.05 | 2.48 | 0.73 | 0.64 | 0.56 | 0.21 | 0.07 | 0 | 0.01 | −0.01 | 0.01 | 0.01 | 1 | 0 | 0.19 | |
| Standard deviation | 1.02 | 1.36 | 1.44 | 1.93 | 1.98 | 0.82 | 0.83 | 0.81 | 0.53 | 0.26 | 0.69 | 0.64 | 0.69 | 0.73 | 0.74 | 1.1 | 0.92 | 0.32 |
Note: Correlations significant at p < 0.05 are bolded.
Table 2.
Standardized Factor Loadings for Latent Comorbidity Variables
| β | S.E. | p | |
|---|---|---|---|
| Comorbidity ages 13–14 | |||
| Depression | 0.55 | 0.05 | 0.01 |
| Anxiety | 0.31 | 0.06 | 0.01 |
| Alcohol | 0.56 | 0.05 | 0.01 |
| Tobacco | 0.70 | 0.06 | 0.01 |
| Marijuana | 0.87 | 0.05 | 0.01 |
| Comorbidity ages 30–33 | |||
| Depression symptoms | 0.47 | 0.07 | 0.01 |
| Anxiety symptoms | 0.38 | 0.06 | 0.01 |
| Marijuana symptoms | 0.61 | 0.08 | 0.01 |
| Alcohol symptoms | 0.48 | 0.06 | 0.01 |
| Tobacco symptoms | 0.61 | 0.06 | 0.01 |
Next, we added general and problem-specific predictors and the paths described in the Analysis section and the conceptual model in Figure 1. Results of the full estimated model including all the paths tested in RQ 1 and 2 are shown in Table 3, including continuity between adolescent and adult comorbidity (RQ1) and residuals regressed onto general and specific predictors (RQ2). Fit of the final model was adequate (χ2(110) = 350, p < .001, CFI = .95, TLI = .88, RMSEA = .04). The adolescent comorbidity factor had higher loadings on substance use than mental health, whereas the loadings on the adult comorbidity factor were more even.
Table 3.
Model Results: Standardized Betas, Standard Errors, and Significance of Structural Paths
| Predictor | Outcome age 13–14 |
B | S.E. | p | Outcome ages 30–33 |
β | S.E. | p |
|---|---|---|---|---|---|---|---|---|
| Research question 1: Continuity in comorbidity | ||||||||
| Comorbidity 13–14 → | Comorbidity 30–33 | 0.28 | 0.10 | 0.01 | ||||
| Research question 2a: General risk factors → comorbidity | ||||||||
| Positive family environment→ | Comorbidity | −0.09 | 0.05 | 0.11 | Comorbidity | 0.01 | 0.06 | 0.92 |
| Peer general environment→ | Comorbidity | −0.03 | 0.06 | 0.60 | Comorbidity | 0.09 | 0.07 | 0.16 |
| Behavioral disinhibition→ | Comorbidity | 0.21 | 0.07 | 0.01 | Comorbidity | −0.15 | 0.11 | 0.15 |
| Research question 2b: Specific risk factors → comorbidity | ||||||||
| Family depression→ | Comorbidity | 0.06 | 0.07 | 0.41 | Comorbidity | 0.17 | 0.06 | 0.01 |
| Family alcohol environment→ | Comorbidity | −0.09 | 0.07 | 0.23 | Comorbidity | −0.04 | 0.07 | 0.58 |
| Family tobacco environment→ | Comorbidity | 0.15 | 0.06 | 0.01 | Comorbidity | 0.03 | 0.07 | 0.70 |
| Family marijuana environment→ | Comorbidity | 0.01 | 0.06 | 0.87 | Comorbidity | −0.07 | 0.06 | 0.23 |
| Peer substance use→ | Comorbidity | 0.12 | 0.09 | 0.20 | Comorbidity | 0.14 | 0.10 | 0.14 |
| Research question 2c: General risk factors → specific indicators | ||||||||
| Positive family environment→ | Anxiety | −0.12 | 0.04 | 0.01 | Anxiety symptoms | −0.11 | 0.04 | 0.01 |
| Peer general environment→ | Depression | 0.19 | 0.05 | 0.01 | Depression symptoms | n.s. | ||
| Peer general environment→ | Tobacco use | −0.13 | 0.06 | 0.03 | Tobacco depend. symptoms | n.s. | ||
| Behavioral disinhibition→ | Alcohol use | n.s. | Alcohol abuse/depend. symptoms | 0.43 | 0.06 | 0.01 | ||
| Behavioral disinhibition→ | Tobacco use | n.s. | Tobacco depend. symptoms | 0.40 | 0.06 | 0.01 | ||
| Behavioral disinhibition→ | Marijuana use | n.s. | Marijuana abuse/depend. symptoms | 0.38 | 0.08 | 0.01 | ||
| Research question 2d: Specific risk factors → specific indicators | ||||||||
| Family depression→ | Anxiety | 0.09 | 0.05 | 0.07 | Anxiety symptoms | 0.30 | 0.04 | 0.01 |
| Family depression→ | Depression | 0.06 | 0.05 | 0.28 | Depression symptoms | 0.28 | 0.05 | 0.01 |
| Peer substance use→ | Alcohol use | 0.25 | 0.06 | 0.01 | Alcohol abuse/depend. symptoms | −0.14 | 0.07 | 0.04 |
| Family alcohol environment→ | Alcohol use | 0.03 | 0.05 | 0.55 | Alcohol abuse/depend. symptoms | 0.14 | 0.05 | 0.01 |
| Peer substance use→ | Tobacco use | 0.32 | 0.07 | 0.01 | Tobacco depend. symptoms | −0.13 | 0.07 | 0.05 |
| Family tobacco environment→ | Tobacco use | 0.00 | 0.06 | 0.99 | Tobacco depend. symptoms | 0.11 | 0.05 | 0.03 |
| Peer substance use→ | Marijuana use | 0.23 | 0.10 | 0.01 | Marijuana abuse/depend. symptoms | −0.19 | 0.09 | 0.03 |
| Family marijuana environment→ | Marijuana use | 0.01 | 0.06 | 0.84 | Marijuana abuse/depend. symptoms | 0.16 | 0.06 | 0.01 |
Note: p values < 0.05 are in boldface. Standardized estimates reported. Controls and correlations among exogenous variables not shown; depend = dependence; n.s. = not significant. Nonsignificant general and specific pathways to specific indicators were removed from the final model for identifiability.
RQ1: Continuity in Comorbidity from Adolescence to Adulthood
Comorbidity showed continuity across development; adolescent comorbidity significantly predicted comorbidity in adulthood, with a standardized coefficient of .28. Before predictors were added, the standardized coefficient of this association was .36, suggesting that there was strong continuity in comorbidity from adolescence to adulthood above the role of the predictors.
RQ2: General and Specific Predictors of Comorbidity and Specific Effects
General and specific predictors of comorbidity.
After accounting for demographic controls and continuity in comorbidity, only behavioral disinhibition (general) and family tobacco environment (specific) predicted comorbidity at ages 13–14. Only family history of depression predicted comorbidity in adulthood.
Predictors of specific effects (residuals).
Examining associations with residual, or unique, variance in the indicators of comorbidity allowed us to test whether predictors were related to aspects of each indicator that were uncorrelated with the other indicators (see Table 3). With regard to adolescent substance use and internalizing problems in adolescence, positive family functioning in adolescence predicted unique variance in anxiety, and peer substance use predicted the residuals of all three substance use indicators—alcohol, tobacco, and marijuana. Peer general functioning predicted unique variance in tobacco use and depression symptoms but was in the opposite direction from expected for tobacco; because we do see a positive zero-order correlation as expected (Table 1), we interpreted this finding as a suppressor effect.
Many specific risk factors from the childhood context predicted unique variance in substance use and mental health indicators in adulthood. Family history of depression predicted residual variance in adult anxiety and depression symptoms, and positive family functioning predicted unique variance in anxiety symptoms in adulthood. Adolescent family alcohol environment predicted unique variance in alcohol symptoms, family tobacco environment predicted unique variance in adult tobacco symptoms, and family marijuana environment predicted unique variance in adult marijuana symptoms. Finally, behavioral disinhibition predicted unique variance in each of the three adult substance use disorder indicators. Peer substance use demonstrated some negative effects on adult-specific indicators, which are likely suppressor effects due to their positive zero-order correlations.
Discussion
This study sought to advance understanding of the etiology and developmental progression of comorbid substance use and mental health problems. The model used latent variables to partition variance in mental health and substance use problems into what is common (comorbid) and what is unique, and determined the extent to which general and problem-specific risk factors predicted the common and unique variance. Results show significant continuity from comorbid substance use and mental health at ages 13–14 to comorbid substance abuse and dependence symptoms and internalizing mental health disorder symptoms at ages 30–33, and that the significant general and specific predictors of comorbidity varied by age.
Beyond continuity, we found that adolescent and adult comorbidity did not share predictors. Only BD and family tobacco environment were related to adolescent comorbidity; only family history of mental health was predictive of comorbidity in adulthood. This pattern of findings is consistent with the hypothesis that environmental effects may be especially important in adolescence, and genetic effects may be more salient in adulthood (Pagan et al., 2006). Further, some predictors were associated with comorbidity early on (e.g., BD), but predicted specific behaviors later on. This may be developmentally bound or related to the difference in how we constructed comorbidity to account for development. For example, it is possible that BD is more related to substance use, which drove the comorbidity in adolescence and continued to predict substance use disorders in adulthood. Future research might investigate whether adolescent comorbidity mediates the effect of BD on comorbidity in adulthood.
The finding of continuity in comorbidity across development is an important contribution to the understanding of comorbidity etiology. While there is a significant gap in development not included on our study, we found that comorbidity in substance use and internalizing problems in adolescence was a risk factor for later comorbidity in mental health disorder symptoms and symptoms of substance use dependence. The implication is that adolescent comorbid symptoms may escalate to disorder in adulthood if left untreated, and suggests that screening and early intervention with adolescents with comorbid problems may reduce comorbidity in adulthood, potentially reducing severity of illness (Graaf et al., 2002; Kessler, 2004).
By specifying the general and specific influences of peer and family environments, we have identified a number of potential targets for interventions that differ by developmental period. There may be multiple benefits to targeting adolescents who show characteristics of behavioral disinhibition for early intervention, as it is likely to influence the development of adolescent comorbidity and substance use in adulthood, which may also interrupt the continuity of comorbidity to adulthood. Intervening in the specific social environments of family depression and family substance use early in development may not exert an influence until adulthood, while intervening specifically to address family depression might also prevent adult comorbidity.
Limitations
Some limitations are important to note when interpreting the results. First, retrospective self-reports of family history of depression may be biased by one’s current mental health state, and are a reflection of respondents’ perception of their family’s mental health status. Second, teacher reports of internalizing processes capture behavior that appears to be internalizing, but may not reflect the internal state of the adolescent at the time. There is also potential for method variance bias, as we use a combination of self- and teacher reports. Future studies need to replicate the continuity in comorbidity over a shorter developmental period—it is possible that adolescent predictors such as BD, and family environments may be associated with comorbidity in late adolescence or young adulthood, with potential for intervention targets. Finally, future studies replicating these results in different geographic and ethnic contexts are warranted.
Conclusions and Prevention Implications
Findings from the current study offer novel approaches to the study and prevention of comorbidity of mental health and substance use problems. Comorbidity shares some risk factors with those specific to mental health and substance use problems, but also has unique predictors. Results suggest that comorbidity has different risk factors in different developmental time periods, and that prevention interventions should be tailored accordingly. Early intervention with behaviorally disinhibited youth has the potential to curb comorbidity in adolescence and may curb comorbidity in adulthood as well.
Acknowledgments
Funding: This research was supported by grants (R01DA024411, R01DA003721, and R01DA09679) from the National Institute on Drug Abuse (NIDA). The funding organization had no role in the design and conduct of the study; collection, analysis, or preparation of data; or preparation, review, or approval of the manuscript. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of NIDA.
This research was supported by grants from the National Institute on Drug Abuse [R01DA024411, R01DA003721, and R01DA09679]. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
Ethical Approval: All procedures in this study were approved by and in accordance with the ethical standards of the University of Washington institutional review board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
References
- Achenbach TM (1991). Manual for the Child Behavior Checklist/4-18 and 1991 profile. Department of Psychiatry, University of Vermont; Burlington, VT. [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Armstrong TD, & Costello EJ (2002). Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. Journal of Consulting and Clinical Psychology, 70, 1224–1239. [DOI] [PubMed] [Google Scholar]
- Aseltine RH, Gore S, & Colten ME (1998). The co-occurrence of depression and substance abuse in late adolescence. Development and Psychopathology, 10, 549–570. [DOI] [PubMed] [Google Scholar]
- Avenevoli S, & Merikangas KR (2003). Familial influences on adolescent smoking. Addiction, 98, 1–20. [DOI] [PubMed] [Google Scholar]
- Bailey JA, Hill KG, Meacham MC, Young SE, & Hawkins JD (2011). Strategies for characterizing complex phenotypes and environments: General and specific family environmental predictors of young adult tobacco dependence, alcohol use disorder, and co-occurring problems. Drug and Alcohol Dependence, 118, 444–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey JA, Hill KG, Oesterle S, & Hawkins JD (2006). Linking substance use and problem behavior across three generations. Journal of Abnormal Child Psychology, 34, 273–292. [DOI] [PubMed] [Google Scholar]
- Bailey JA, Samek DR, Keyes MA, Hill KG, Hicks BM, McGue M, … Hawkins JD (2014). General and substance-specific predictors of young adult nicotine dependence, alcohol use disorder, and problem behavior: Replication in two samples. Drug and Alcohol Dependence, 138, 161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano RF, Kosterman R, Hawkins JD, Newcomb MD, & Abbott RD (1996). Modeling the etiology of adolescent substance use: A test of the social development model. Journal of Drug Issues, 26, 429–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Presson CC, Rose J, Sherman SJ, Davis MJ, & Gonzalez JL (2005). Parenting style and smoking-specific parenting practices as predictors of adolescent smoking onset. Journal of Pediatric Psychology, 30, 333–344. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Erkanli A, Federman E, & Angold A (1999). Development of psychiatric comorbidity with substance abuse in adolescents: Effects of timing and sex. Journal of Clinical Child Psychology, 28, 298–311. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, & Angold A (2003). Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry, 60, 837–844. [DOI] [PubMed] [Google Scholar]
- Dell’Osso L, & Pini S (2012). What did we learn from research on comorbidity in psychiatry? Advantages and limitations in the forthcoming DSM-V era. Clinical Practice and Epidemiology in Mental Health, 8, 180–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Rodriguez-Seijas C, Carragher N, & Krueger RF (2015). Transdiagnostic factors of psychopathology and substance use disorders: A review. Social Psychiatry and Psychiatric Epidemiology, 50, 171–182. [DOI] [PubMed] [Google Scholar]
- Epstein M, Hill KG, Bailey JA, & Hawkins JD (2013). The effect of general and drug-specific family environments on comorbid and drug-specific problem behavior: A longitudinal examination. Developmental Psychology, 49, 1151–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graaf R. d., Bijl RV, Smit F, Vollebergh WAM, & Spijker J (2002). Risk factors for 12-month comorbidity of mood, anxiety, and substance use disorders: Findings from the Netherlands mental health survey and incidence study. The American Journal of Psychiatry, 159, 620–629. [DOI] [PubMed] [Google Scholar]
- Green KM, Zebrak KA, Fothergill KE, Robertson JA, & Ensminger ME (2012). Childhood and adolescent risk factors for comorbid depression and substance use disorders in adulthood. Addictive Behaviors, 37, 1240–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harter SL (2000). Psychosocial adjustment of adult children of alcoholics: A review of the recent empirical literature. Clinical Psychology Review, 20, 311–337. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, & Miller JY (1992). Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin, 112, 64–105. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Smith BH, Hill KG, Kosterman R, Catalano RF, & Abbott RD (2003). Understanding and preventing crime and violence: Findings from the Seattle Social Development Project In Thornberry TP, & Krohn MD (Eds.), Taking stock of delinquency: An overview of findings from contemporary longitudinal studies (pp. 255–312). New York, NY: Kluwer Academic/Plenum. [Google Scholar]
- Iacono WG, Carlson SR, Taylor J, Elkins IJ, & McGue M (1999). Behavioral disinhibition and the development of substance-use disorders: Findings from the Minnesota Twin Family Study. Development and Psychopathology, 11, 869–900. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Malone SM, & McGue M (2008). Behavioral disinhibition and the development of early-onset addiction: Common and specific influences. Annual Review of Clinical Psychology, 4, 325–348. [DOI] [PubMed] [Google Scholar]
- Jones TM, Hill KG, Epstein M, Lee JO, Hawkins JD, & Catalano RF (2016). Understanding the interplay of individual and social-developmental factors in the progression of substance use and mental health from childhood to adulthood. Development and Psychopathology special issue: Longitudinal Transactional Models of Development and Psychopathology, 28, 721–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC (2004). The epidemiology of dual diagnosis. Biological Psychiatry, 56, 730–737. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, & Markon KE (2006). Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology, 2, 111–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, & Borchardt C (2000). The relationship between anxiety disorders and alcohol use disorders: A review of major perspectives and findings. Clinical Psychology Review, 20, 149–171. [DOI] [PubMed] [Google Scholar]
- Lee JO, Hill KG, Guttmannova K, Bailey JA, Hartigan LA, Hawkins JD, & Catalano RF (2012). The effects of general and alcohol-specific peer factors in adolescence on trajectories of alcohol abuse disorder symptoms from 21 to 33 years. Drug and Alcohol Dependence, 121, 213–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lengua LJ, Sadowski CA, Friedrich WN, & Fisher J (2001). Rationally and empirically derived dimensions of children's symptomatology: Expert ratings and confirmatory factor analyses of the CBCL. Journal of Consulting and Clinical Psychology, 69, 683–698. [PubMed] [Google Scholar]
- Mars B, Collishaw S, Smith D, Thapar A, Potter R, Sellers R, … Thapar A (2012). Offspring of parents with recurrent depression: Which features of parent depression index risk for offspring psychopathology? Journal of Affective Disorders, 136, 44–53. [DOI] [PubMed] [Google Scholar]
- Mays D, Gilman SE, Rende R, Luta G, Tercyak KP, & Niaura RS (2014). Parental smoking exposure and adolescent smoking trajectories. Pediatrics, 133, 983–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley E, Pavlidis K, & Kendall K (2001). Developmental precursors of depression: The child and the social environment. The Depressed Child and Adolescent, 2, 46–78. [Google Scholar]
- McGue M, Iacono WG, Legrand LN, Malone S, & Elkins I (2001). Origins and consequences of age at first drink. Associations with substance-use disorders, disinhibitory behavior and psychopathology, and p3 amplitude. Alcoholism: Clinical & Experimental Research, 25, 1156–1165. [PubMed] [Google Scholar]
- Merikangas KR, He J.-p., Burstein M, Swanson SA, Avenevoli S, Cui L, … Swendsen J (2010). Lifetime prevalence of mental disorders in us adolescents: Results from the National Comorbidity Survey replication-Adolescent Supplement (NCS-A). Journal of the Academy of Child & Adolescent Psychiatry, 49, 980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar-Gaziola S, … Kessler RC (1998). Comorbidity of substance use disorders with mood and anxiety disorders: Results of the International Consortium in Psychiatric Epidemiology. Addictive Behaviors, 23, 893–907. [DOI] [PubMed] [Google Scholar]
- Merline A, Jager J, & Schulenberg JE (2008). Adolescent risk factors for adult alcohol use and abuse: Stability and change of predictive value across early and middle adulthood. Addiction, 103, 84–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2008). Mplus user's guide (4th ed.). Los Angeles: Muthén & Muthén. [Google Scholar]
- Najt P, Fusar-Poli P, & Brambilla P (2011). Co-occurring mental and substance abuse disorders: A review on the potential predictors and clinical outcomes. Psychiatry Research, 186, 159–164. [DOI] [PubMed] [Google Scholar]
- Newcomb MD, & McGee L (1991). Influence of sensation seeking on general deviance and specific problem behaviors from adolescence to young adulthood. Journal of Personality and Social Psychology, 61, 614–628. [DOI] [PubMed] [Google Scholar]
- Oxford M, Oxford ML, Harachi TW, Catalano RF, & Abbott RD (2001). Preadolescent predictors of substance initiation: A test of both the direct and mediated effect of family social control factors on deviant peer associations and substance initiation. American Journal of Drug and Alcohol Abuse, 27, 599–616. [DOI] [PubMed] [Google Scholar]
- Pagan JL, Rose RJ, Viken RJ, Pulkkinen L, Kaprio J, & Dick DM (2006). Genetic and environmental influences on stages of alcohol use across adolescence and into young adulthood. Behavior Genetics, 36, 483–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson PL, Hawkins JD, Abbott RD, & Catalano RF (1994). Disentangling the effects of parental drinking, family management, and parental alcohol norms on current drinking by black and white adolescents. Journal of Research on Adolescence, 4, 203–227. [Google Scholar]
- Repetti RL, Taylor SE, & Seeman TE (2002). Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin, 128, 330–366. [PubMed] [Google Scholar]
- Reynolds AD, & Crea TM (2015). Peer influence processes for youth delinquency and depression. Journal of Adolescence, 43, 83–95. [DOI] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan J, Williams JBW, & Spitzer RL (1981). NIMH Diagnostic Interview Schedule: Version III (May 1981). Rockville, MD: National Institute of Mental Health. [Google Scholar]
- Salom CL, Williams GM, Najman JM, & Alati R (2014). Familial factors associated with development of alcohol and mental health comorbidity. Addiction, 110, 248–257. [DOI] [PubMed] [Google Scholar]
- Stone AL, Becker LG, Huber AM, & Catalano RF (2012). Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive Behaviors, 37, 747–775. [DOI] [PubMed] [Google Scholar]
- Swendsen JD, & Merikangas KR (2000). The comorbidity of depression and substance use disorders. Clinical Psychology Review, 20, 173–189. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, & Verdeli H (2006). Offspring of depressed parents: 20 years later. The American Journal of Psychiatry, 163, 1001–1008. [DOI] [PubMed] [Google Scholar]
- Yap MBH, & Jorm AF (2015). Parental factors associated with childhood anxiety, depression, and internalizing problems: A systematic review and meta-analysis. Journal of Affective Disorders, 175, 424–440. [DOI] [PubMed] [Google Scholar]
- Yap MBH, Pilkington PD, Ryan SM, & Jorm AF (2014). Parental factors associated with depression and anxiety in young people: A systematic review and meta-analysis. Journal of Affective Disorders, 156, 8–23. [DOI] [PubMed] [Google Scholar]