Abstract
Objective:
Develop and evaluate a measure assessing helpful and harmful family/friends’ involvement in adults’ type 2 diabetes (T2D) self-management.
Methods:
Prior mixed-methods research, cognitive interviews, and expert input informed measure development. We administered the measure in two studies (N=392 and N=512) to evaluate its factor structure, internal consistency reliability, test-retest reliability, construct, criterion and predictive validity.
Results:
Analyses supported a two-factor solution: helpful and harmful involvement with internal consistency reliability α=.86 and .72, respectively. Three-month test-retest reliability was rho=0.64 for helpful and rho=0.61 for harmful (both p<0.001). Over 90% reported at least one instance of family/friend involvement in the past month. Associations with other measures of diabetes involvement were as anticipated (all p<.01). Helpful and harmful involvement were independently associated with diabetes self-efficacy, diet, blood glucose testing and medication adherence cross-sectionally, adjusted for demographics and diabetes characteristics [βs 0.13–0.39 helpful, −0.12–−0.33 harmful; all p<.05]. Harmful involvement independently predicted worse HbA1c (β=0.08, p=.03), and worsening HbA1c over three months (β=0.12, p=.04).
Conclusion:
The Family and Friend Involvement in Adults’ Diabetes (FIAD) is a reliable and valid measure assessing family/friend involvement in adults’ T2D.
Practice Implications:
FIAD use can inform interventions to improve social contexts in which adults manage diabetes.
1. Introduction
Successful self-management of type 2 diabetes (T2D) requires consistently taking prescribed medications, daily self-monitoring of blood glucose, and maintaining a healthful diet and regular physical activity. These daily activities often involve family members and close friends,[1, 2] who may provide instrumental support (e.g., assist with medication refills, help problem-solve in response to blood glucose readings),[3] and help to prioritize and support physical activity and healthful diet choices.[4–7] This received support makes adhering to the diabetes regimen easier,[3, 8–13] is associated with better self-care adherence[14] and self-efficacy,[15] and predicts better long-term glycemic control.[16]
However, qualitative and quantitative research indicates that family and friends can be involved in T2D in both helpful and harmful ways.[13, 17–20] Harmful involvement is multidimensional, consisting of “miscarried helping” and sabotaging.[3] Miscarried helping reflects an intent to be supportive (e.g., reminding the patient to avoid an unhealthy food), which can undermine patients’ self-efficacy, leading to interpersonal conflict[19] and, potentially, worse adherence due to reactance.[9, 17, 21, 22] This has been associated with maladaptive conflict resolution strategies[23] and may be interpreted by the receiver as social control.[24] Sabotaging/undermining occurs when patients’ self-care efforts are made more difficult by the behaviors or attitudes of others[3, 25] and is associated with worse adherence.[26] Harmful family/friend involvement, including both dimensions, has been associated cross-sectionally with worse glycemic control.[13]
Because helpful and harmful involvement are each common and often co-occur (are positively correlated),[9, 13, 17, 22, 25–27] examining both is critical for understanding the lived experience of adults with T2D.[25, 28] Observational research suggests interventions that successfully increase helpful involvement and decrease harmful involvement will be more effective in supporting diabetes self-management than those only increasing involvement.[11, 13] Failing to assess and address harmful involvement may be one reason for mixed and sometimes detrimental effects of family interventions adults with T2D.[3, 29, 30] Prior research has demonstrated the importance of including both types of involvement in the same models to isolate the unique contributions each type by adjusting for the frequency of involvement.[13]
There is need for a measure assessing patients’ experiences of helpful and harmful involvement that is flexible with regard to relationship types and living arrangements.[25, 31] A frequently used measure assessing both helpful and harmful aspects of family involvement is the Diabetes Family Behavior Checklist (DFBC).[9] This measure has demonstrated associations with self-care behaviors and glycemic control among adults with T2D.[13] However, it was originally designed for adolescents with type 1 diabetes[27] and several items pertain to parent-child relationships and/or presume the respondent lives with family. However, around a third of American households are nonfamily households, including adults who live alone.[32, 33] Out-of-home family support is also common; 78% of older adults in the U.S. have weekly contact with adult children living outside their home,[31] and up to 7 million Americans report receive support from long-distance family/friends.[31] Thus, a comprehensive operationalization of “family support” for T2D needs to look beyond traditional notions of a household unit and account for patients’ experiences with multiple others rather than a primary “caregiver.”[25] Finally, the DFBC was developed and validated among predominantly Caucasian patients,[9, 27] thus more inclusive items may be needed.[25]
Therefore, we drew upon prior qualitative and quantitative research on family/friend involvement in diabetes self-management among racially/ethnically and socioeconomically diverse adults with T2D to develop the Family and Friend Involvement in Adults’ Diabetes (FIAD) measure. We then administered this new measure in two studies among adults with T2D to evaluate the FIAD’s performance, including its factor structure, internal consistency reliability, test-retest reliability, convergent validity with other measures of involvement, and criterion and predictive validity with diabetes self-efficacy, self-care behaviors, and glycemic control.
2. Measure development
Item development was informed by patients’ quotes about family/friends’ involvement in T2D management from a series of prior qualitative/mixed-method studies.[3, 25, 34] Another prior quantitative study[13] examining associations between the DFBC and self-care and hemoglobin A1c (HbA1c) informed our decision to develop items to assess helpful and harmful involvement. We developed 18 new items and retained two DFBC items based on significant bivariate correlations with HbA1c in the prior study.[13] Goals for item development included (a) assessing received (i.e., experienced) support because it is more strongly associated with self-care adherence [14] and less conflated with need as compared to perceived (i.e., available if/when needed) support, (b) not presuming family/friends live with/near the adult with diabetes, and (c) avoiding words such as “nag” that may be perceived as either helpful or harmful by different respondents.[25, 28] These 20 items were included in a patient version and a parallel version for an important friend or family member. We generated several sets of Likert responses with a 5-point scale.
Next, the principal author (LSM) conducted iterative cognitive interviews by phone lasting 20–30 minutes with five adults with T2D and two family members of (other) adults with T2D. Respondents answered all questions aloud before the interviewer used retrospective probing[35] to identify problematic/unclear phrasing and ensure the interviewee’s initial thoughts fit into available response options (e.g., “How did you get to that answer?”). Interviewees were asked if any relevant family/friend involvement was not queried. Both items and response options were revised based on feedback during cognitive interviews, for a total of five iterations of the measure. The revised measure was reviewed by experts in family/friends’ involvement in diabetes (Acknowledgements) to ensure the items clearly assessed helpful and harmful involvement. Integration of this feedback resulted in 16 items, 9 assessing helpful involvement and 7 assessing harmful involvement, with response options on a scale from 1=“never in the past month” to 5=“twice or more each week” (Appendix). The final FIAD measure had a Flesch readability score of 93.6 (range 0–100 with higher score indicating easier readability) and Flesch-Kincaid grade level of 2.1.
3. Data and Methods
We included the new FIAD measure in two studies among adults with T2D. The first was a cross-sectional observational study which included the FIAD alongside other measures related to family involvement and extracted recent HbA1c from participants’ electronic medical record (EMR). The second was a longitudinal randomized controlled trial (RCT) which included quarterly surveys and HbA1c tests. Data were entered into REDCap (Research Electronic Data Capture)[36] for both studies. Vanderbilt University Institutional Review Board approved procedures for both studies prior to recruitment.
3.1. Procedures
3.1.1. Study 1 procedures
Participants were recruited from Vanderbilt University Medical Center via the Mid-South Clinical Data Research Network for an observational study which included completion of self-report measures and consent for EMR review. Recruitment occurred October 2017 through April 2018. Eligible participants were adults 18–80 years old with T2D (identified via EMR data with a validated phenotype algorithm[37]) who were receiving care for T2D at Vanderbilt (operationalized as having an outpatient visit at Vanderbilt within the prior 12 months and ≥two HbA1c values within the prior 18 months), had an email address in their EMR, and could read in English. Participants were excluded if they had conditions which likely alter family dynamics around the patients’ health (cancer treatment or pregnancy within prior 12 months), present a threat to health and longevity that might reduce the patient’s and clinician’s focus on diabetes (heart failure, end-stage renal disease, or hospice disposition), and/or impede the patient’s ability to respond to self-report measures (dementia, or schizophrenia). Participants were recruited via an email invitation which included a link to a REDCap survey to complete informed consent and the survey online and a phone number if they wished to complete via phone with a research assistant (RA). Participants received $20. For these analyses, we include the 392 participants who completed all FIAD items.
3.1.2. Study 2 procedures
Participants (N=512) were recruited May 2016 to December 2017 from Vanderbilt Adult Primary Care clinics (57%) and Federally Qualified Health Centers (43%) in Nashville, TN for an ongoing three-arm RCT evaluating mobile phone-delivered diabetes support interventions.[38] We used multiple recruitment methods including letters followed by a phone call, flyers at clinics, interest cards, referrals from clinic staff, and in-person contact. Eligible participants were ≥18 years old with T2D who were prescribed at daily diabetes medication and took their medication independently (i.e., not administered by a caregiver), could read English, and had a cell phone. Exclusion criteria included most recent HbA1c value <6.8% within the past 12 months, failing a cognitive impairment screen,[39] auditory limitations, inability to communicate orally, and/or inability to receive/send a text message as determined by trained RAs.
RAs met with interested patients privately at their clinic to verify eligibility, complete informed consent, administer survey instruments, and request an HbA1c test. Next, participants were randomized, and RAs called participants to explain the assigned condition. For these analyses, we use baseline data from all enrolled participants (N=512) and three-month follow-up data from participants assigned to the control condition who completed the follow-up assessment (n=227). Participants received $20 for completing the enrollment procedures plus $35 for completing the three-month survey and HbA1c test.
3.2. Measures
Each study included the FIAD items alongside different measures of interest. In both studies, participants reported characteristics including age, gender, race, ethnicity, education, income, marital status, and years since diabetes diagnosis. Diabetes medications were confirmed by EMR review. Cronbach’s α values are presented from the respective sample for each measure.
3.2.1. Study 1 measures
Participants completed several measures assessing family/friend involvement in their diabetes management. The Perceptions of Collaboration Questionnaire (PCQ)[40] measures collaborative problem solving and decision making which we adapted to reference the respondent’s “person most involved in your diabetes on a regular basis.” The PCQ assesses three aspects of respondents’ perceptions of collaborative coping: cognitive compensation which assesses the degree to which collaboration is needed to overcome cognitive deficits or decline (e.g., “I view working together as necessary because it is harder for me to do things by myself;” α=.80), interpersonal enjoyment which assesses the degree to which collaboration provides encouragement and closeness (e.g., “Solving everyday problems and making decisions together brings us closer together;” α=.63), and frequency of collaboration (e.g., “We always work together to deal with really important decisions or solve problems;” α=.78). Each subscale consisted of three items on 5-point response scales that were averaged to generate subscale scores ranging from 1–5.
Respondents also completed the Important Other Climate Questionnaire (IOCQ)[40] which assesses “autonomy support” defined as social support from family/friends which maintains support for the individual’s personal agency. We adapted the 6-item IOCQ to be specific to diabetes as the developers recommend[41] and to reference more than one important other to be consistent with the FIAD items (e.g., “My important others try to understand how I see my diabetes before suggesting any changes;” α=.88). Likert responses are averaged to create a scale score ranging from 1–5 with higher scores indicating more autonomy support.
Finally, we assessed participants’ perception of their family’s effectiveness in dealing with diabetes (“How effective is your family at dealing with troubles or issues related to your diabetes management?”) and their satisfaction (“How satisfied are you with your family members’ involvement in dealing with troubles or issues related to your diabetes management?”) from 1=“not at all” to 4=“Extremely.”
3.2.2. Study 2 measures
Diabetes self-efficacy was assessed with a 4-item version of the Perceived Diabetes Self-Management Scale (PDSMS-4)[42, 43] which includes self-ratings of competence to manage diabetes (e.g., “I’m generally able to accomplish my goals with respect to managing my diabetes;” α=0.68) on a 1=“strongly disagree” to 5=“strongly agree” scale. Summed scores range from 4 to 20 with higher scores indicating higher self-efficacy.[43]
We assessed diet with two, three-item subscales from the Personal Diabetes Questionnaire (PDQ).[44] The “Problem Eating Behavior” subscale asks how often the respondent overate, ate unplanned snacks, and made poor food choices (α=0.70). The “Use of Dietary Information for Decision Making” subscale asks how often the respondent uses information about calories, carbohydrates, and grams of fat to make food decisions (α=0.83). Respondents rate items across the past month with options from 1=“never” to 6=“one or more times per day.”
We used the International Physical Activity Questionnaire–Short Form[45] to obtain MET-minutes per week. We assessed diabetes medication adherence and blood glucose testing with the respective subscales of the Summary of Diabetes Self-Care Activities.[46] The blood glucose testing subscale consists of two items (α=0.88) and we asked the medication adherence questions separately for each prescribed diabetes medication and then averaged responses across medications.[47]
RAs obtained HbA1c results from the participants’ EMR if taken within three weeks of study enrollment. Otherwise, RAs either requested a blood-drawn HbA1c test be completed at the clinic or asked the participant to complete a mail-in kit, depending on clinic preference. The kits use the dried blood-spot method which has been validated against venipuncture.[48, 49]1
3.3. Analyses
First, we conducted an exploratory factor analysis (EFA) using FIAD data from Study 1, followed by a confirmatory factor analysis (CFA) using FIAD data from Study 2[50] with IBM SPSS statistics version 24 Amos add-on. For the EFA, we used principal component analysis with a varimax rotation with Kaiser normalization, retaining items with factor loadings >.32. For the CFA, we assessed model fit with multiple indices and associated thresholds [comparative fit index, CFI≥0.90; root mean square error of approximation, RMSEA≤0.06 with confidence interval (CI) 0.00–0.08; and standardized root mean square residual, SRMR<0.08].[50]
Other analyses were conducted with Stata version 14.2. FIAD item responses were averaged to generate index scores for helpful and harmful involvement, each ranging from 1–5 with higher scores indicating more frequent helpful or harmful involvement. We examined internal consistency reliability with Cronbach’s α and summary statistics for the FIAD scores in both samples. Because of significant skew and kurtosis of the FIAD scores, we used nonparametric tests and robust standard errors (type HC3)[51] which are robust to normality assumption violations.[52] We examined three-month test-retest reliability of the FIAD scores using Spearman’s rho and intraclass correlation coefficients (ICC) to assess the strength of correlation between the two measurement times and paired Wilcoxon rank-sign tests to assess systematic changes between the times.
We examined bivariate and partial associations between the FIAD scores and other measures of family involvement to establish convergent validity (Study 1) and with self-efficacy and self-care behaviors cross-sectionally to establish criterion and predictive validity (Study 2). To obtain a more normal HbA1c distribution, we combined study samples for analyses examining the cross-sectional relationship between the FIAD scores and HbA1c.
A suppression effect would be indicated if partial associations for both FIAD scores were larger than bivariate associations, indicating that suppressing shared variance (conceptualized as degree of involvement) allows for examination of the unique contributions of each type of involvement.[13] This is reciprocal or “cooperative” suppression in which the two independent variables mutually suppress irrelevant variance in each other.[53] Construct validity would be indicated by FIAD helpful involvement being positively associated with all three PCQ subscales, the IOCQ, and with perceived effectiveness and satisfaction and FIAD harmful involvement being negatively associated with the interpersonal enjoyment and frequency of collaboration subscales of the PCQ (but not with the cognitive compensation subscale), the IOCQ, and with perceived effectiveness and satisfaction. Criterion validity would be indicated if helpful and harmful FIAD scores were associated respectively with better and worse self-efficacy, self-care, and HbA1c in fully adjusted cross-sectional regression models.
Finally, we examined predictive validity by evaluating change in diabetes self-efficacy, self-care behaviors, and HbA1c – that is, predicting the three-month outcome adjusted for the baseline value of the outcome, in fully adjusted models. All fully adjusted models included a priori covariates: age in years, gender, race (non-Hispanic White, non-Hispanic Black, other), education in years, diabetes duration in years, income, and insulin status (prescribed insulin, not prescribed insulin).
3.3.1. Missing data
Each summary score was calculated for participants responding to at least two-thirds of the respective items. No FIAD scores were missing in either sample. Seven variables used in multivariate regression analyses had missing data (≤2.5% missing for any one variable except 9.3% missing for income). Because casewise deletion can bias estimates, we used multiple imputation using chained equations with predictive mean matching to impute m=10 data sets for regression models.
4. Results
Participant characteristics for each study sample are shown in Table 1. Notably, the samples varied with respect to race/ethnicity, socioeconomic status, prescribed diabetes medications, and HbA1c value distributions.
Table 1.
Participant Characteristics.
| Study 1 (N=392) |
Study 2 (N=512) |
|
|---|---|---|
| Age, years (Mean ± SD) | 57.5±12.2 | 56.0±9.5 |
| Female (%) | 50.6% | 54.1% |
| Married/Partnered (%) | 65.7% | 42.4% |
| Race/Ethnicity (%) | ||
| Non-Hispanic White | 76.5% | 46.3% |
| Non-Hispanic Black | 15.3% | 39.4% |
| Hispanic | 2.3% | 6.0% |
| Other, including multiracial | 5.9% | 6.0% |
| Education, years (Mean ± SD) | 15.8±2.6 | 14.1±3.1 |
| Less than high school degree or GED (%) | 0.8% | 41.7% |
| Income, USD (%) | ||
| < $15,000 | 7.5% | 32.2% |
| $15,000 - $34,999 | 14.6% | 28.8% |
| $35,000 - $54,999 | 17.6% | 14.5% |
| ≥$55,000 | 60.3% | 24.5% |
| Insurance Status (%) | Not collected | |
| Uninsured | 23.2% | |
| Public insurance only | 25.4% | |
| Private insurance | 51.4% | |
| Diabetes duration, years (Mean ± SD) | 9.7±8.0 | 11.1±7.9 |
| Prescribed diabetes medication regimen (%) | ||
| None | 2.6% | 0.0% |
| Orals or non-insulin injectables only | 77.5% | 51.2% |
| Insulin | 19.9% | 48.8% |
| Hemoglobin A1c, % (Mean ± SD)a | 7.2±1.5% | 8.6±1.8% |
| HbAlc ≥7.0% (%) | 49.7% | 84.8% |
| Family and Friend Involvement in Adults’ Diabetes | ||
| Helpful involvement | 1.9±0.9 | 2.0±0.9 |
| Harmful involvement | 1.6±0.6 | 1.7±0.6 |
Study 1 HbA1c tests were completed median −9 [−77, 34] days from survey date; 74% were within 90 days and 99% within 365 days.
Study 2 HbA1c tests were completed median 0 [0,0] days from survey date; 99% were within 30 days. Three-month follow-up HbA1c tests were completed median 91 [79, 100] days post-baseline; 94% were completed 90 ± 30 days from baseline survey.
4.1. FIAD Factor Structure & Internal Consistency
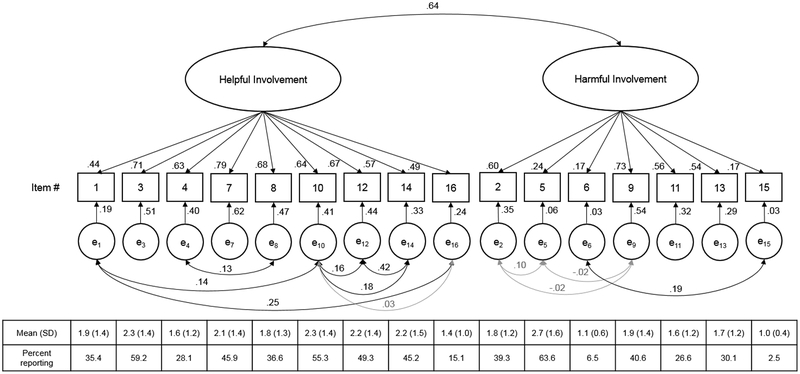
We applied a two-factor solution to determine if items loaded as expected an EFA (Table 2). Eigenvalues for two factors were 5.6 and 2.0, explaining 46.9% of the variance. The helpful FIAD items each had a factor loading >.5 on Factor 1; three also had factor loadings >.4 on Factor 2 (Table 2). Because of the way these items are worded and their higher factor loadings on Factor 1, they remained indicators of helpful involvement in the CFA. The harmful FIAD items each had a factor loading >.32 on Factor 2; items regarding criticism/arguing had higher factor loadings compared to items regarding undermining/sabotaging. We evaluated the 9 helpful and 7 harmful items in a CFA using data from Study 2 (Figure 1). Correlated error terms were determined a priori based on potential for shared sources of variation aside from the factors of interest (e.g., referencing the same self-care behavior).[54] Each fit statistic indicated good fit: CFI=.94, RMSEA=.054 [.046, .063], SRMR=.046. All helpful involvement item loadings were ≥.40. As in the EFA, loadings for items assessing undermining/sabotaging were lower than those assessing criticism/arguing. In Study 1 and 2, respectively, internal consistency reliability was Cronbach’s α=0.86 and 0.87 for the 9-item helpful involvement score and α=0.72 and 0.63 for the 7-item harmful involvement score. Therefore, we maintained all harmful items in a single summary score.2
Table 2.
Principal component exploratory factor analysis (Study 1).
| Item | Mean (SD) | Percent reportinga | Factor 1 | Factor 2 |
|---|---|---|---|---|
| Helpful involvement | Harmful involvement | |||
| Helpful items | ||||
| 1. exercise with you or ask you to exercise with them | 2.1 (1.4) | 42.7 | .616 | |
| 3. gently talk with you about taking care of your diabetes | 2.1 (1.3) | 54.7 | .611 | .453 |
| 4. help you decide if changes should be made based on your blood sugar testing | 1.6 (1.1) | 29.2 | .562 | .459 |
| 7. ask how they can help you with your diabetes | 1.9 (1.2) | 45.4 | .746 | |
| 8. suggest things that might help you take your diabetes medicine | 1.7 (1.2) | 33.8 | .603 | .417 |
| 10. praise you for eating healthy foods or following your exercise routine | 2.3 (1.4) | 57.7 | .741 | |
| 12. help you choose healthy foods, for example, by reading food labels | 2.2 (1.4) | 50.7 | .782 | |
| 14. prepare or plan healthy foods to help with your recommended diet | 2.2 (1.4) | 50.6 | .764 | |
| 16. take on one of your responsibilities, so you can have time to exercise | 1.4 (0.9) | 21.5 | .632 | |
| Harmful items | ||||
| 2. point out in front of others when you are eating unhealthy foods | 1.7 (1.1) | 33.6 | .608 | |
| 5. bring foods around that you shouldn’t be eating | 2.7 (1.4) | 69.4 | .472 | |
| 6. tell you diabetes is your problem to deal with on your own | 1.2 (0.7) | 7.8 | .364 | |
| 9. argue with you about your food choices or your health | 1.6 (1.1) | 32.9 | .702 | |
| 11. criticize you for not testing your blood sugar | 1.4 (1.0) | 21.3 | .763 | |
| 13. criticize you for not exercising | 1.7 (1.1) | 36.4 | .709 | |
| 15. suggest you don’t need to take your diabetes medicine | 1.1 (0.4) | 4.6 | .367 | |
Includes participants scoring the item > 1 “never in the past month” SD = standard deviation; blank factor loading values were <.32
Figure 1. Confirmatory factor analysis (Study 2).
Standardized factor loadings are shown on the paths from the latent variable to each indicator (item), all p<.001; squared multiple correlations are shown on the paths from each indicator to each error term, all p<.001. Curved arrows depict correlations between error terms that were not constrained to zero based on hypothesized shared error variance for certain items (correlations non-significant at p<.05 are grayed). Mean (standard deviations) and percent reporting a score > 1 = “never in the past month” for each item are shown across the bottom.
4.2. Scale Characteristics
FIAD scores were similar across study samples (Table 1) and nearly all (91.6% and 92.5%) participants reported experiencing at least one of the items in the past month. In both samples, the FIAD helpful and harmful scores were moderately, positively correlated (rho=0.40 and 0.44, p<.001), both were right skewed (p<.001), and harmful involvement had significant kurtosis (p<.001).
4.3. Test-retest reliability
Test-retest reliability for the control condition participants in Study 2 was rho=0.64 for helpful and rho=0.61 for harmful (ps<0.001) and ICCs were 0.65 [95% CI .58, .72] for helpful and 0.60 [95% CI .52, .68] for harmful. There were no significant differences between scores at baseline and the three-month follow-up on either (paired Wilcoxon sign-rank for helpful z=1.04, p=0.298; harmful z=0.75, p=0.452).
4.4. Construct & Criterion Validity
Table 3 shows pairwise and partial associations between the FIAD scores and other measures of family/friend involvement as well as outcomes (diabetes self-efficacy, self-care behaviors, and HbA1c). Relationships were stronger when both FIAD scores were included (partial correlations) as hypothesized, except for associations with HbA1c. The FIAD scores correlated in expected (and opposite) directions with measures of collaborative coping, autonomy support, and patients’ perceptions of effectiveness of and satisfaction with support received. Table 4 shows results of fully adjusted cross-sectional models. Standardized independent associations with FIAD scores were strongest for diabetes self-efficacy, diet (both PDQ subscales) and medication adherence, explaining 7–11% of the variance in each above the a priori covariates. Due to lack of evidence for a suppression effect on HbA1c, we evaluated the effects of helpful and harmful involvement on HbA1c separate models adjusted for covariates. There was a significant independent association between harmful involvement and higher HbA1c (Table 2) but not between helpful involvement and HbA1c.
Table 3.
Correlations of FIAD helpful and harmful involvement scores with other measures of family involvement and outcomes of interest.
| Pairwise rho | Partially adjusted | |||||
|---|---|---|---|---|---|---|
| Outcome | Mean ± SD | Range | Helpful | Harmful | Helpful | Harmful |
| Study 1 (N=392) | ||||||
| Cognitive Compensation (PCQ) | 3.3 ± 1.1 | 1 – 5 | .35*** | .14** | .32*** | −.04 |
| Interpersonal Enjoyment (PCQ) | 3.6 ± 0.9 | 1 – 5 | .36*** | .00 | .39*** | −.21*** |
| Frequency of Collaboration (PCQ) | 3.6 ± 1.1 | 1 – 5 | .34*** | .04 | .36*** | −.16** |
| Autonomy Support (IOCQ) 1 | 3.5 ± 0.9 | 1 – 5 | .36*** | −.12* | .44*** | −.27*** |
| Effectiveness | 2.5 ± 1.0 | 1 – 4 | .46*** | −.05 | .48*** | −.24*** |
| Satisfaction | 2.9 ± 0.9 | 1 – 4 | .30*** | −.20*** | .41*** | −.32*** |
| Study 2 (N=512) | ||||||
| Diabetes Self-Efficacy (PDSMS) | 13.9 ± 3.6 | 4 – 20 | .05 | −.20*** | .18*** | −.30*** |
| Problem Eating Behavior (PDQ) | 3.3 ± 1.1 | 1 – 6 | −.02 | .25*** | −.15** | .29*** |
| Use of Dietary Information for Decision Making (PDQ) | 3.0 ± 1.7 | 1 – 6 | .21*** | −.06 | .32*** | −.22*** |
| Physical Activity (MET-minutes per week, IPAQ) | 2274 ± 2778 | 0 – 15084 | .10* | −.03 | .13* | −.09 |
| Blood Glucose Testing (SDSCA) | 3.6 ± 2.8 | 0 – 7 | .12** | −.05 | .17*** | −.14** |
| Medication Adherence (SDSCA) | 6.4 ± 1.2 | 0 – 7 | .07 | −.19*** | .16*** | −.29*** |
| Study 1 & 2, N=904 | ||||||
| Glycemic Control (HbA1c, %) | 8.0 ± 1.8 | 4.8 – 16.1 | .03 | .16*** | −.07 | .12* |
p < .05,
p < .01,
p < .001.
FIAD = Family and Friend Involvement in Adults’ Diabetes; IOCQ = Important Other(s) Climate Questionnaire; IPAQ = International Physical Activity Questionnaire (short form); PCQ = Perceptions of Collaboration Questionnaire; PDQ = Personal Diabetes Questionnaire; PDSMS = Perceived Diabetes Self-Management Scale; SDSCA = Summary of Diabetes Self-care Activities
Table 4.
Criterion validity: Adjusted associations between FIAD helpful and harmful involvement scores and diabetes self-efficacy, adherence to self-care behaviors and glycemic control.
| Study 2, N=512 | β | P | Incremental R2 (%) |
|---|---|---|---|
| Diabetes Self-Efficacy (PDSMS) | |||
| Helpful | .15 | .002 | 1.9** |
| Harmful | −.25 | <.001 | 5.9*** |
| Problem Eating Behavior (PDQ) | |||
| Helpful | −.18 | .001 | 2.4*** |
| Harmful | .32 | <.001 | 7.7*** |
| Use of Dietary Information for Decision Making (PDQ) | |||
| Helpful | .31 | <.001 | 7.3*** |
| Harmful | −.20 | <.001 | 3.0*** |
| Physical Activity (MET-minutes per week, IPAQ) | |||
| Helpful | .13 | .025 | 1.0* |
| Harmful | −.12 | .058 | 0.8* |
| Blood Glucose Testing (SDSCA) | |||
| Helpful | .20 | <.001 | 3.3*** |
| Harmful | −.15 | .004 | 1.7** |
| Medication Adherence (SDSCA) | |||
| Helpful | .18 | .001 | 2 3** |
| Harmful | −.26 | <.001 | 5.0*** |
| Study 1 & 2, N=904 | |||
| Hemoglobin A1c (HbA1c, %) | |||
| Helpful | −.04 | .323 | 0.1 |
| Harmful | .08 | .026 | 0.6* |
p < .05,
p < .01,
p < .001.
FIAD = Family and Friend Involvement in Adults’ Diabetes; IPAQ = International Physical Activity Questionnaire (short form); PDQ = Personal Diabetes Questionnaire; PDSMS = Perceived Diabetes Self-Management Scale, 4 item version; SDSCA = Summary of Diabetes Self-care Activities
β = standardized regression coefficients; p = probability value; Incremental R2 = percent of variance in outcome variable uniquely explained by the predictor variable, controlling for the other predictor variables in the model. Fully adjusted models include covariates: age, gender, race, education, income, diabetes duration, and insulin status.
4.5. Predictive Validity
In fully adjusted predictive models (not shown in Tables), helpful involvement independently predicted increased blood glucose testing from enrollment to three-month follow-up (β=0.17, p=.011), whereas harmful involvement independently predicted worsening HbA1c from enrollment to three-month follow-up (β=0.12, p=.046). Neither helpful nor harmful involvement predicted change in self-efficacy, diet, physical activity, or medication adherence.
5. Discussion and Conclusion
5.1. Discussion
The FIAD is a reliable and valid brief measure of helpful and harmful family/friend involvement that was developed for and evaluated among adults with T2D. Over 90% of respondents endorsed at least one of the FIAD items and both the helpful and harmful scores were independently associated with T2D-related self-efficacy and self-care behaviors, pointing to the measure’s sensitivity and construct validity. We also found good internal consistency reliability and three-month test-retest reliability was adequate and reasonable given changing social dynamics over time. Furthermore, FIAD scores demonstrated convergent validity with other measures of family/friend involvement, including perceived effectiveness of and satisfaction with the involvement received. Cross-sectionally, helpful family and friend involvement was independently associated with greater diabetes self-efficacy, better dietary behaviors, more physical activity, more frequent blood glucose testing and better medication adherence, while harmful involvement was independently associated with less diabetes self-efficacy, worse dietary behaviors, less frequent blood glucose testing and worse medication adherence. Furthermore, more harmful involvement was associated worse glycemic control cross-sectionally and with worsening glycemic control over three months.
This study is the first, to our knowledge, to find a longitudinal association between harmful family/friend involvement and worsening glycemic control. Family/friends may engage in more harmful involvement when patients have worse glycemic control, and/or experiencing harmful involvement may have a stronger influence on patients than experiencing helpful involvement. Although both directions of causation are plausible,[1] our finding provides support for the latter.
We did not find, however, that helpful involvement was associated, either cross-sectionally or longitudinally, with better glycemic control. Furthermore, we found little evidence of associations between FIAD scores and changes in self-care adherence over three months (except for helpful involvement predicting increased blood glucose testing). Prior research has also found harmful involvement to be more associated with glycemic control than helpful involvement cross-sectionally,[3, 13] but Nicklette et al. assessed how much adults with T2D could “count on my family or friends to help and support me a lot with…[various regimen activities]” and found more perceived support was associated with improved outcomes over time. Therefore, this finding appears consistent with research on received support (helpful and harmful) for T2D, but not with the literature on perceived support (availability of supports if/when needed) which may play a distinct role.
It is unclear why FIAD scores were not associated with changes in more self-care behaviors given the association with worsening glycemic control. This could be due to use of self-report measures of self-care behaviors (e.g., recall and social desirability bias). Using daily diaries, Stephens et al.[22] found diet-specific spousal involvement affected patients’ subsequent dietary behaviors. Harmful family/friend involvement may affect patients’ HbA1c through pathways other than less self-care, such as increased diabetes distress[55, 56] and reduced motivation to cope with diabetes-related problems.[57] Finally, the suppression effect identified in our prior work[13] and replicated here suggests the overall ratio of helpful and harmful involvement may matter more than the frequency of family/friend involvement for self-care behaviors, underlining the importance of targeting both types in interventions to improve social support for T2D.
Additional limitations of our approach include the potential for selection bias in the studies used to examine the measures’ psychometric properties and assessing test-retest reliability at three-months for a measure which asks the respondent about their experiences in the prior 30 days. Strengths include our step-wise and multi-stakeholder approach to measure development, attention to racial and socioeconomic diversity, use of both an EFA and CFA, and using relatively large samples to examine the psychometric properties of the measures.
5.2. Practice Implications
Findings underline the importance of examining both helpful and harmful aspects of family/friend involvement, using a measure appropriate for adults’ diverse social and living situations, and examining potential suppression effects for each outcome prior to analyses to determine whether the FIAD scores should be analyzed together or separately. Evidence that associations are stronger and in hypothesized directions when both scores are included indicates including both in subsequent models. Because the FIAD was designed to be relevant to adults with T2D, we anticipate it may be sensitive to interventions seeking to improve their diabetes self-management support, but future research assessing sensitivity to intervention effects is needed. Attempts to engage family/friends or increase “social support” may be ineffective or detrimental without attention to patients’ experiences of harmful involvement.
Highlights.
Supportive social environments theoretically improve diabetes self-management
Measures relevant to adults needed to assess helpful & harmful social involvement
We developed a measure applicable to diverse adults agnostic to living situation
Helpful & harmful scores were independently divergently associated with self-management
Harmful involvement was independently associated with worsening HbA1c over 3 months
Acknowledgements:
Experts providing feedback on the measure during the development stage included Barbara Anderson, Shari Barkin, Tom Elasy, Sarah Jaser, Shelagh Mulvaney, and Chandra Osborn. This research was supported by the National Institute of Health via NIH/NIDDK R01-DK100694, NIH/NIDDK R03-DK113329 and Dr. Mayberry’s Mentored Career Development Award NIH/NIDDK K01-DK106306. This study was also supported by the National Institutes of Health National Center for Advancing Translational Sciences UL1 TR000445 through the use of REDCap and Secondary use of clinical data: The Vanderbilt Approach.
Appendix. Family and Friend Involvement in Adults’ Diabetes (FIAD)
The following questions are about certain things your friends or family members may or may not do to try to help you take care of your diabetes. Just think about the people closest to you in your everyday life – it doesn’t matter if they live with you. For each item, respond according to how often your friends or family members have done the behavior in the past month.
| How often do your friends or family members… | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. exercise with you or ask you to exercise with them? | ○ | ○ | ○ | ○ | ○ |
| 2. point out in front of others when you are eating unhealthy foods, like at a party or get together? | ○ | ○ | ○ | ○ | ○ |
| 3. gently talk with you about taking care of your diabetes? | ○ | ○ | ○ | ○ | ○ |
| 4. help you decide if changes should be made based on your blood sugar testing results? | ○ | ○ | ○ | ○ | ○ |
| 5. bring foods around that you shouldn’t be eating? | ○ | ○ | ○ | ○ | ○ |
| 6. tell you diabetes is your problem to deal with on your own? | ○ | ○ | ○ | ○ | ○ |
| 7. ask how they can help you with your diabetes? | ○ | ○ | ○ | ○ | ○ |
| 8. suggest things that might help you take your diabetes medicine when you are supposed to? | ○ | ○ | ○ | ○ | ○ |
| 9. argue with you about your food choices or your health? | ○ | ○ | ○ | ○ | ○ |
| 10. praise you for eating healthy foods or following your exercise routine? | ○ | ○ | ○ | ○ | ○ |
| 11. criticize you for not testing your blood sugar? | ○ | ○ | ○ | ○ | ○ |
| 12. help you choose healthy foods, by reading food labels or helping you choose from a menu? | ○ | ○ | ○ | ○ | ○ |
| 13. criticize you for not exercising? | ○ | ○ | ○ | ○ | ○ |
| 14. prepare or plan healthy foods to help with your recommended diet? | ○ | ○ | ○ | ○ | ○ |
| 15. suggest you don’t need to take your diabetes medicine? | ○ | ○ | ○ | ○ | ○ |
| 16. take on one of your responsibilities, so you can have time to exercise? | ○ | ○ | ○ | ○ | ○ |
Scoring & Analysis:
Helpful involvement score; Average items 1, 3, 4, 7, 8, 10, 12, 14, 16 for summary score ranging 1–5
Harmful involvement score; Average items 2, 5, 6, 9, 11, 13, 15 for summary score ranging 1–5
Any score with fewer than two-thirds of associated items answered should be given a missing value. Scales may perform better (direction and magnitude of associations) when including both in the same model (i.e., including both as predictors), this may depend on outcome.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing Interests Statements:
The authors have no competing interests to declare.
We ran sensitivity analyses to determine if adjusting for HbA1c test type in cross-sectional analyses and change in HbA1c test type in longitudinal analyses changed regression coefficients or p values. They did not, so, for simplicity, we present results of models without the HbA1c test type adjustment.
Excluding items 5, 6, and 15 due to low factor loadings and infrequent reporting on items 6 and 15 weakened associations between the FIAD harmful involvement score and outcomes of interest in subsequent analyses, which reinforced our decision to retain them in a total harmful involvement score.
References
- [1].Fisher L, Chesla CA, Bartz RJ, Gilliss C, Skaff MA, Sabogal F, Kanter RA, Lutz CP, The family and type 2 diabetes: a framework for intervention, Diabetes Educ 24 (1998) 599–607. https://doi.org/0.1177/014572179802400504 [DOI] [PubMed] [Google Scholar]
- [2].Young-Hyman D, De Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M, Psychosocial care for people with diabetes: a position statement of the American Diabetes Association, Diabetes Care 39 (2016) 2126–2140. 10.2337/dc16-2053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Mayberry LS, Osborn CY, Family support, medication adherence, and glycemic control among adults with type 2 diabetes, Diabetes Care 35 (2012) 1239–1245. 10.2337/dc11-2103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Barrera M, Toobert DJ, Angell KL, Glasgow RE, Mackinnon DP, Social support and social-ecological resources as mediators of lifestyle intervention effects for type 2 diabetes, J Health Psychol 11 (2006) 483–495. 10.1177/1359105306063321 [DOI] [PubMed] [Google Scholar]
- [5].De Vries Mcclintock HF, Wiebe DJ, O’donnell AJ, Morales KH, Small DS, Bogner HR, Neighborhood social environment and patterns of adherence to oral hypoglycemic agents among patients with type 2 diabetes mellitus, Fam Community Health 38 (2015) 169–179. 10.1097/FCH.0000000000000069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Soto SC, Louie SY, Cherrington AL, Parada H, Horton LA, Ayala GX, An ecological perspective on diabetes self-care support, self-management behaviors, and hemoglobin A1C Among Latinos, Diabetes Educ 41 (2015) 214–223. 10.1177/0145721715569078 [DOI] [PubMed] [Google Scholar]
- [7].Nicolucci A, Kovacs Burns K, Holt R, Comaschi M, Hermanns N, Ishii H, Kokoszka A, Pouwer F, Skovlund S, Stuckey H, Diabetes Attitudes, Wishes and Needs second study (DAWN2™): Cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes, Diabetic Med 30 (2013) 767–777. 10.1111/dme.12245 [DOI] [PubMed] [Google Scholar]
- [8].Garay-Sevilla ME, Nava LE, Malacara JM, Huerta R, Diaz De Leon J, Mena A, Fajardo ME, Adherence to treatment and social support in patients with non-insulin dependent diabetes mellitus, J Diabetes Complications 9 (1995) 81–6. https://doi.org/105687279400021F [DOI] [PubMed] [Google Scholar]
- [9].Glasgow RE, Toobert DJ, Social environment and regimen adherence among type II diabetic patients, Diabetes Care 11 (1988) 377–386. 10.1016/1056-8727(94)00021-F [DOI] [PubMed] [Google Scholar]
- [10].Tang TS, Brown MB, Funnell MM, Anderson RM, Social support, quality of life, and self-care behaviors among African Americans with type 2 diabetes, Diabetes Educ 34 (2008) 266–76. 10.1177/0145721708315680 [DOI] [PubMed] [Google Scholar]
- [11].Rosland AM, Heisler M, Piette JD, The impact of family behaviors and communication patterns on chronic illness outcomes: a systematic review, J Behav Med 35 (2012) 221–39. 10.1007/s10865-011-9354-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Choi SE, Diet-specific family support and glucose control among Korean immigrants with type 2 diabetes, Diabetes Educ 35 (2009) 978–985. 10.1177/0145721709349220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Mayberry LS, Osborn CY, Family involvement is helpful and harmful to patients’ self-care and glycemic control, Pat Educ Couns 97 (2014) 418–425. 10.1016/j.pec.2014.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Dimatteo MR, Social support and patient adherence to medical treatment: A meta-analysis, Health Psychol 23 (2004) 207–218. 10.1037/0278-6133.23.2.207 [DOI] [PubMed] [Google Scholar]
- [15].Johnson MD, Anderson JR, Walker A, Wilcox A, Lewis VL, Robbins DC, Common dyadic coping is indirectly related to dietary and exercise adherence via patient and partner diabetes efficacy, J Fam Psychol 27 (2013) 722–730. 10.1037/a0034006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Nicklett EJ, Heisler MEM, Spencer MS, Rosland AM, Direct social support and long-term health among middle-aged and older adults with type 2 diabetes mellitus, J Gerontol B Psychol Sci Soc Sci 68 (2013) 933–943. 10.1093/geronb/gbt100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Mayberry LS, Osborn CY, Family support, medication adherence, and glycemic control among adults with type 2 diabetes, Diabetes Care 35 (2012) 1239–45. 10.2337/dc11-2103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Rosland AM, Heisler M, Choi H-J, Silveira MJ, Piette JD, Family influences on self-management among functionally independent adults with diabetes or heart failure: do family members hinder as much as they help?, Chronic Illn 6 (2010) 22–33. 10.1177/1742395309354608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Harris MA, The family’s involvement in diabetes care and the problem of miscarried helping, Business Briefing: European Endocrine Review Reference Section (2006) 1–3. 10.17925/USE.2006.00.1.2g [DOI] [Google Scholar]
- [20].Wen LK, Shepherd MD, Parchman ML, Family support, diet, and exercise among older Mexican Americans with type 2 diabetes, Diabetes Educ 30 (2004) 980–993. 10.1177/014572170403000619 [DOI] [PubMed] [Google Scholar]
- [21].Wen LK, Parchman ML, Shepherd MD, Family support and diet barriers among older Hispanic adults with type 2 diabetes, Fam Med 36(2004) 423–430. [PubMed] [Google Scholar]
- [22].Stephens M.a.P., Franks MM, Rook KS, Iida M, Hemphill RC, Salem JK, Spouses’ attempts to regulate day-to-day dietary adherence among patients with type 2 diabetes, Health Psychol 32 (2013) 1029–1037. 10.1037/a0030018 [DOI] [PubMed] [Google Scholar]
- [23].Tanaka R, Trief PM, Scales K, Weinstock RS, “Miscarried helping” in adults with Type 2 diabetes: Helping for Health Inventory—Couples, Fam Syst Health 35 (2017) 409–419. 10.1037/fsh0000289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].August KJ, Rook KS, Parris Stephens MA, Franks MM, Are spouses of chronically ill partners burdened by exerting health-related social control?, J Health Psychol 16 (2011) 1109–1119. 10.1177/1359105311401670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Mayberry LS, Harper KJ, Osborn CY, Family behaviors and type 2 diabetes: What to target and how to address in interventions for adults with low socioeconomic status, Chronic Illn 12 (2016) 199–215. 10.1177/1742395316644303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Henry SL, Rook KS, Stephens MA, Franks MM, Spousal undermining of older diabetic patients’ disease management, J Health Psychol 18 (2013) 1550–1561. 10.1177/1359105312465913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Schafer LC, Mccaul KD, Glasgow RE, Supportive and nonsupportive family behaviors - relationships to adherence and metabolic control in persons with type-I diabetes, Diabetes Care 9 (1986) 179–185. 10.2337/diacare.9.2.179 [DOI] [PubMed] [Google Scholar]
- [28].Vongmany J, Luckett T, Lam L, Phillips J, Family behaviours that have an impact on the self-management activities of adults living with Type 2 diabetes: a systematic review and meta-synthesis, Diabetic Med 35 (2018) 184–194. 10.1111/dme.13547 [DOI] [PubMed] [Google Scholar]
- [29].Baig AA, Benitez A, Quinn MT, Burnet DL, Family interventions to improve diabetes outcomes for adults, Ann N Y Acad Sci 1353 (2015) 89–112. 10.1111/nyas.12844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Torenholt R, Schwennesen N, Willaing I, Lost in translation—the role of family in interventions among adults with diabetes: a systematic review, Diabetic Med 31 (2014) 15–23. 10.1111/dme.12290. [DOI] [PubMed] [Google Scholar]
- [31].Piette JD, Rosland AM, Silveira M, Kabeto M, Langa KM, The case for involving adult children outside of the household in the self-management support of older adults with chronic illnesses, Chronic Illn 6 (2010) 34–45. 10.1177/1742395309347804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Vespa J, Lewis JM, Kreider RM , America’s families and living arrangements: 2012, Current Population Reports 20 (2013) P570 https://www.census.gov/prod/2013pubs/p20-570.pdf. (Accessed June 7, 2017). [Google Scholar]
- [33].US Department of Health and Human Services Administration on Aging. 2017 Profile of Older Americans, 2017. https://www.acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/2017OlderAmericansProfile.pdf. (Accessed June 4, 2017).
- [34].Mayberry LS, Berg CA, Harper KJ, Osborn CY, The design, usability, and feasibility of a family-focused diabetes self-care support mHealth intervention for diverse, low-income adults with type 2 diabetes, J Diab Res 2016 (2016) 7586385 10.1155/2016/7586385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Willis GB, Cognitive interviewing: A “how to” guide. Guide provided for the short course, “Reducing survey error through resarch on the cognitive and decision processes in surveys” offered at the 1999 meeting of the American Statistical Assocation, in: Rachael A Caspar JTL, and Willis Gordon B (Ed.) 1999. [Google Scholar]
- [36].Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG, Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support, J Biomed Inform 42 (2009) 377–381. 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Kirby JC, Speltz P, Rasmussen LV, Basford M, Gottesman O, Peissig PL, Pacheco JA, Tromp G, Pathak J, Carrell DS, PheKB: a catalog and workflow for creating electronic phenotype algorithms for transportability, J Am Med Inform Assoc 23 (2016) 1046–1052. 10.1093/jamia/ocv202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Nelson LA, Wallston KA, Kripalani S, Greevy RA Jr, Elasy TA, Bergner EM, Gentry CK, Mayberry LS, Mobile phone support for diabetes self-care among diverse adults: Protocol for a three-arm randomized controlled trial, JMIR Res Protoc 7 (2018) e92 10.2196/resprot.9443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC, Six-item screener to identify cognitive impairment among potential subjects for clinical research, Med Care 40 (2002) 771–781. 10.1097/01.MLR.0000024610.33213.C8 [DOI] [PubMed] [Google Scholar]
- [40].Berg CA, Schindler I, Smith TW, Skinner M, Beveridge RM, Perceptions of the cognitive compensation and interpersonal enjoyment functions of collaboration among middle-aged and older married couples, Psychol Aging 26 (2011) 167 10.1037/a0021124. [DOI] [PubMed] [Google Scholar]
- [41].Williams GC, Lynch MF, Mcgregor HA, Ryan RM, Sharp D, Deci EL, Validation of the” Important Other” Climate Questionnaire: Assessing autonomy support for health-related change, Fam Sys Health 24 (2006) 179–194. 10.1037/1091-7527.24.2.179 [DOI] [Google Scholar]
- [42].Wallston KA, Rothman RL, Cherrington A, Psychometric properties of the Perceived Diabetes Self-Management Scale (PDSMS), J Behav Med 30 (2007) 395–401. 10.1007/s10865-007-9110-y [DOI] [PubMed] [Google Scholar]
- [43].Wild MG, Ostini R, Harrington M, Cavanaugh KL, Wallston KA, Validation of the shortened Perceived Medical Condition Self-Management Scale in patients with chronic disease, Psychol Assess 30 (2018)1300–1307. 10.1037/pas0000572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Akohoue SA, Wallston KA, Schlundt DG, Rothman RL, Psychometric evaluation of the short version of the Personal Diabetes Questionnaire to assess dietary behaviors and exercise in patients with type 2 diabetes, Eating Behaviors 26 (2017) 182–188. 10.1016/j.eatbeh.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, International physical activity questionnaire: 12-country reliability and validity, Med Sci Sports Exerc 35 (2003) 1381–1395. 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- [46].Toobert DJ, Hampson SE, Glasgow RE, The Summary of Diabetes Self-Care Activities measure: Results from 7 studies and a revised scale, Diabetes Care 23(2000) 943–950. 10.2337/diacare.23.7.943 [DOI] [PubMed] [Google Scholar]
- [47].Mayberry LS, Gonzalez JS, Wallston KA, Kripalani S, Osborn CY, The ARMS-D out performs the SDSCA, but both are reliable, valid, and predict glycemic control, Diabetes Res Clin Prac 102 (2013) 96–104. 10.1016/j.diabres.2013.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Fokkema MR, Bakker AJ, De Boer F, Kooistra J, De Vries S, Wolthuis A, HbA1c measurements from dried blood spots: Validation and patient satisfaction, Clin Chem Lab Med 47 (2009) 1259–1264. 10.1515/CCLM.2009.274. [DOI] [PubMed] [Google Scholar]
- [49].Jones TG, Warber KD, Roberts BD, Analysis of hemoglobin a1c from dried blood spot samples with the Tina-quant®II Immunoturbidimetric method, J Diabetes Sci Technol 4 (2010) 244–249. 10.1177/193229681000400203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Kline RB, Principles and practice of structural equation modeling, Guilford publications, 2015. [Google Scholar]
- [51].Hayes AF, Cai L, Using heteroskedasticity-consistent standard error estimators in OLS regression: An introduction and software implementation, Behav Res Method 39 (2007) 709–722. 10.3758/BF03192961 [DOI] [PubMed] [Google Scholar]
- [52].Kitchen CM, Nonparametric versus parametric tests of location in biomedical research, Am J Opthamol 147 (2009) 571–572. 10.1016/j.ajo.2008.06.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Conger AJ, A revised definition for suppressor variables: A guide to their identification and interpretation, Educ Psychol Meas 34 (1974) 35–46. 10.1177/001316447403400105 [DOI] [Google Scholar]
- [54].Cole DA, Ciesla JA, Steiger JH, The insidious effects of failing to include design-driven correlated residuals in latent-variable covariance structure analysis, Psychol Methods 12 (2007) 381396 10.1037/1082-989X.12.4.381 [DOI] [PubMed] [Google Scholar]
- [55].Baek RN, Tanenbaum ML, Gonzalez JS, Diabetes burden and diabetes distress: the buffering effect of social support, Ann Behav Med 48 (2014) 145–155. 10.1007/s12160-013-9585-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Schiøtz M, Bøgelund M, Almdal T, Jensen B, Willaing I, Social support and self-management behaviour among patients with type 2 diabetes, Diabet Med 29 (2012) 654–661. 10.1111/j.1464-5491.2011.03485.x [DOI] [PubMed] [Google Scholar]
- [57].Karlsen B, Idsoe T, Hanestad B, Murberg T, Bru E, Perceptions of support, diabetes-related coping and psychological well-being in adults with type 1 and type 2 diabetes, Psychol Health Med 9 (2004) 53–70. 10.1080/135485003100016377 [DOI] [Google Scholar]