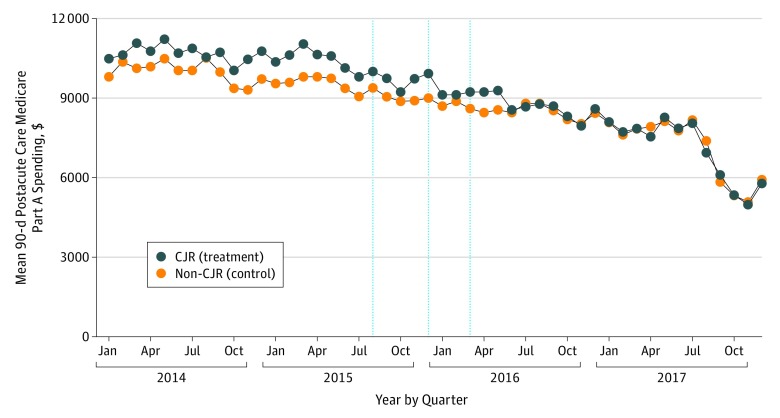
Figure. Medicare Spending on Postacute Care in the 90 Days After Discharge per Episode.
Unadjusted, 90-day postacute care spending among episodes with index admissions at Comprehensive Care for Joint Replacement (CJR) hospitals and non-CJR hospitals. All Medicare Severity Diagnosis Related Group 470 and 469 episodes were included. Data points denote the month of the index admission; thus, the last data point shown is 3 months before the end of data availability. The first vertical line indicates the initial CJR announcement by the Centers for Medicare & Medicaid (CMS), the second vertical line indicates the release of the CMS final rule, and the third vertical line was the start of the CJR model.